Adherence to Three Mediterranean Dietary Indexes and All-Cause, Cardiovascular, and Cancer Mortality in an Older Mediterranean Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Dietary Intake and MedDiet Indexes
2.3. Assessment of Mortality
2.4. Other Variables
2.5. Statistical Analysis
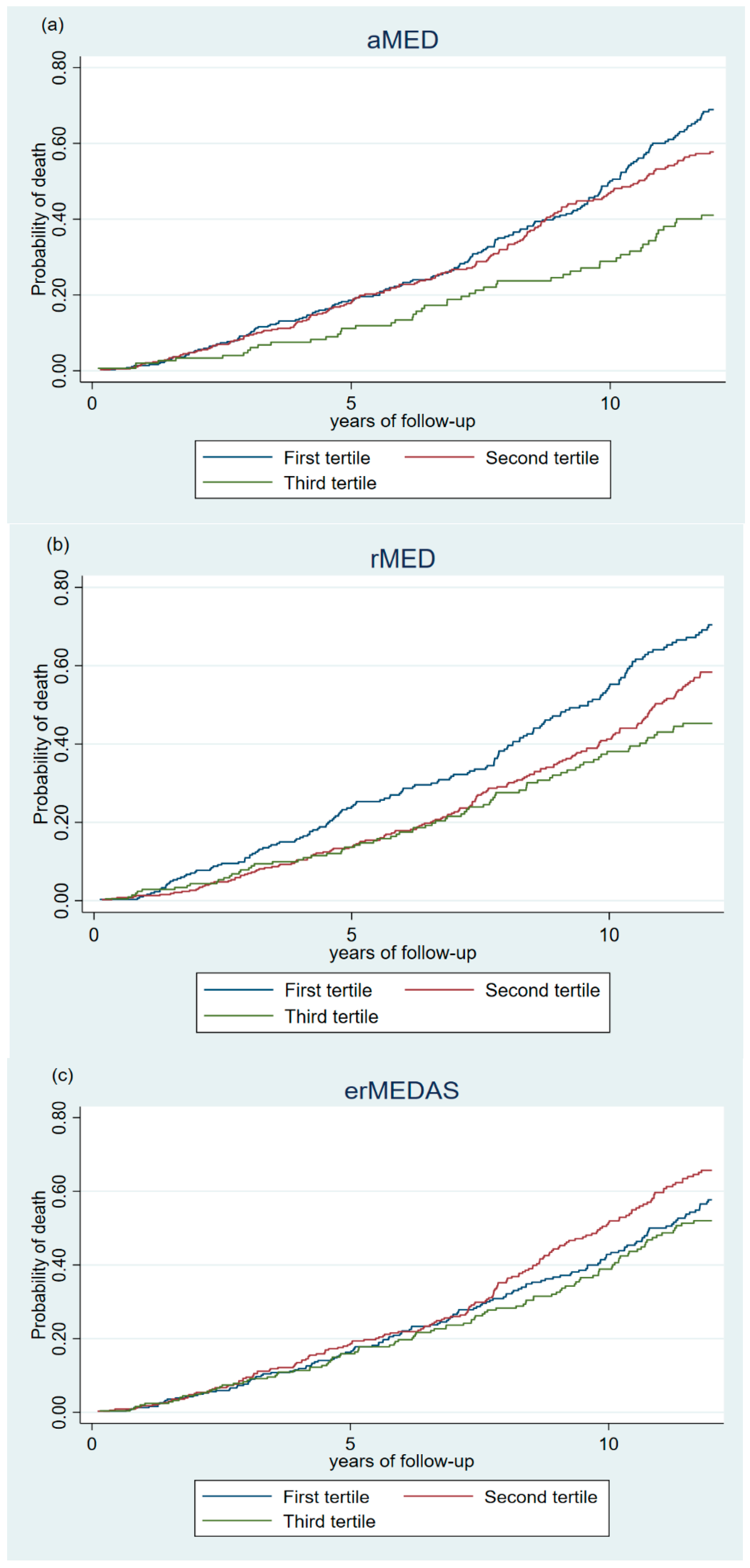
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MedDiet | Mediterranean diet |
| CVD | Cardiovascular disease |
| FFQ | Food-frequency questionnaires |
| aMED | Alternate Mediterranean Diet Score |
| rMED | Relative Mediterranean Diet Score |
| erMEDAS | 17-item energy-restricted Mediterranean Diet Adherence Screener |
| HR | Hazard ratios |
| CI | Confidence intervals |
| MDS | Mediterranean Diet Scale |
| NHS | Nurses’ Health Study |
| NFCCR | Newfoundland Familial Colorectal Cancer Registry |
| EPIC | The European Prospective Investigation into Cancer and Nutrition |
| EUREYE | The European Eye Study |
| VNS | Valencia Nutrition Survey |
| PREDIMED-Plus | PREvención con DIeta MEDiterránea-Plus |
| ICD-10 | International Classification of Diseases version 10 |
| SD | Standard deviations |
| NHANES | National Health and Nutrition Examination Survey |
| HPFS | Health Professionals Follow-Up Study |
| SCHS | Singapore Chinese Health Study |
| MEDAS | 14-point Mediterranean Diet Adherence Screener |
| NIH-AARP | The National Institutes of Health-American Association of Retired Persons |
| WHI OS | Women’s Health Initiative Observational Study |
References
- Knoops, K.T.B.; de Groot, L.C.P.G.M.; Kromhout, D.; Perrin, A.E.; Moreiras-Varela, O.; Menotti, A.; Van Staveren, W.A. Mediterranean Diet, Lifestyle Factors, and 10-Year Mortality in Elderly European Men and Women: The HALE Project. J. Am. Med. Assoc. 2004, 292, 1433–1439. [Google Scholar] [CrossRef]
- Grosso, G.; Marventano, S.; Yang, J.; Micek, A.; Pajak, A.; Scalfi, L.; Galvano, F.; Kales, S.N. A Comprehensive Meta-Analysis on Evidence of Mediterranean Diet and Cardiovascular Disease: Are Individual Components Equal? Crit. Rev. Food Sci. Nutr. 2017, 57, 3218–3232. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Dietary Patterns, Mediterranean Diet, and Cardiovascular Disease. Curr. Opin. Lipidol. 2014, 25, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Adherence to Mediterranean Diet and Risk of Cancer: An Updated Systematic Review and Meta-Analysis of Observational Studies. Cancer Med. 2015, 4, 1933–1947. [Google Scholar] [CrossRef] [PubMed]
- Morze, J.; Danielewicz, A.; Przybyłowicz, K.; Zeng, H.; Hoffmann, G.; Schwingshackl, L. An Updated Systematic Review and Meta-Analysis on Adherence to Mediterranean Diet and Risk of Cancer. Eur. J. Nutr. 2021, 60, 1561–1586. [Google Scholar] [CrossRef]
- Furbatto, M.; Lelli, D.; Antonelli Incalzi, R.; Pedone, C. Mediterranean Diet in Older Adults: Cardiovascular Outcomes and Mortality from Observational and Interventional Studies—A Systematic Review and Meta-Analysis. Nutrients 2024, 16, 3947. [Google Scholar] [CrossRef]
- Martínez-González, M.Á.; Hershey, M.S.; Zazpe, I.; Trichopoulou, A. Transferability of the Mediterranean Diet to Non-Mediterranean Countries. What Is and What Is Not the Mediterranean Diet. Nutrients 2017, 9, 1226. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean Diet Pyramid: A Cultural Model for Healthy Eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Vassilakou, T.; Lipworth, L.; Trichopoulos, D. Diet and Overall Survival in Elderly People. BMJ 1995, 311, 1457–1460. [Google Scholar] [CrossRef]
- Hutchins-Wiese, H.L.; Bales, C.W.; Porter Starr, K.N. Mediterranean Diet Scoring Systems: Understanding the Evolution and Applications for Mediterranean and Non-Mediterranean Countries. Br. J. Nutr. 2022, 128, 1371–1392. [Google Scholar] [CrossRef]
- Fung, T.T.; McCullough, M.L.; Newby, P.K.; Manson, J.E.; Meigs, J.B.; Rifai, N.; Willett, W.C.; Hu, F.B. Diet-Quality Scores and Plasma Concentrations of Markers of Inflammation and Endothelial Dysfunction. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [CrossRef][Green Version]
- Buckland, G.; González, C.A.; Agudo, A.; Vilardell, M.; Berenguer, A.; Amiano, P.; Ardanaz, E.; Arriola, L.; Barricarte, A.; Basterretxea, M.; et al. Adherence to the Mediterranean Diet and Risk of Coronary Heart Disease in the Spanish EPIC Cohort Study. Am. J. Epidemiol. 2009, 170, 1518–1529. [Google Scholar] [CrossRef]
- Schröder, H.; Zomeño, M.D.; Martínez-González, M.A.; Salas-Salvadó, J.; Corella, D.; Vioque, J.; Romaguera, D.; Martínez, J.A.; Tinahones, F.J.; Miranda, J.L.; et al. Validity of the Energy-Restricted Mediterranean Diet Adherence Screener. Clin. Nutr. 2021, 40, 4971–4979. [Google Scholar] [CrossRef]
- Jacobs, S.; Harmon, B.E.; Ollberding, N.J.; Wilkens, L.R.; Monroe, K.R.; Kolonel, L.N.; Marchand, L.L.; Boushey, C.J.; Maskarinec, G. Among 4 Diet Quality Indexes, Only the Alternate Mediterranean Diet Score Is Associated with Better Colorectal Cancer Survival and Only in African American Women in the Multiethnic Cohort. J. Nutr. 2016, 146, 1746–1755. [Google Scholar] [CrossRef]
- Zaslavsky, O.; Zelber-Sagi, S.; Shikany, J.M.; Orchard, T.; Wallace, R.; Snetselaar, L.; Tinker, L. Anatomy of the Mediterranean Diet and Mortality among Older Women with Frailty. J. Nutr. Gerontol. Geriatr. 2018, 37, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Harmon, B.E.; Boushey, C.J.; Shvetsov, Y.B.; Ettienne, R.; Reedy, J.; Wilkens, L.R.; Le Marchand, L.; Henderson, B.E.; Kolonel, L.N. Associations of Key Diet-Quality Indexes with Mortality in the Multiethnic Cohort: The Dietary Patterns Methods Project. Am. J. Clin. Nutr. 2015, 101, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Sharma, I.; Roebothan, B.; Zhu, Y.; Woodrow, J.; Parfrey, P.S.; McLaughlin, J.R.; Wang, P.P. Hypothesis and Data-Driven Dietary Patterns and Colorectal Cancer Survival: Findings from Newfoundland and Labrador Colorectal Cancer Cohort. Nutr. J. 2018, 17, 55. [Google Scholar] [CrossRef]
- Fung, T.T.; Kashambwa, R.; Sato, K.; Chiuve, S.E.; Fuchs, C.S.; Wu, K.; Giovannucci, E.; Ogino, S.; Hu, F.B.; Meyerhardt, J.A. Post Diagnosis Diet Quality and Colorectal Cancer Survival in Women. PLoS ONE 2014, 9, e115377. [Google Scholar] [CrossRef]
- Fung, T.T.; Rexrode, K.M.; Mantzoros, C.S.; Manson, J.E.; Willett, W.C.; Hu, F.B. Mediterranean Diet and Incidence of and Mortality from Coronary Heart Disease and Stroke in Women. Circulation 2010, 119, 1093–1100. [Google Scholar] [CrossRef]
- Shvetsov, Y.B.; Harmon, B.E.; Ettienne, R.; Wilkens, L.R.; Le Marchand, L.; Kolonel, L.N.; Boushey, C.J. The Influence of Energy Standardisation on the Alternate Mediterranean Diet Score and Its Association with Mortality in the Multiethnic Cohort. Br. J. Nutr. 2016, 116, 1592–1601. [Google Scholar] [CrossRef]
- Buckland, G.; Agudo, A.; Travier, N.; Huerta, J.M.; Cirera, L.; Tormo, M.J.; Navarro, C.; Dolores Chirlaque, M.; Moreno-Iribas, C.; Ardanaz, E.; et al. Adherence to the Mediterranean Diet Reduces Mortality in the Spanish Cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Spain). Br. J. Nutr. 2011, 106, 1581–1591. [Google Scholar] [CrossRef]
- Knoops, K.T.B.; de Groot, L.C.; Fidanza, F.; Alberti-Fidanza, A.; Kromhout, D.; van Staveren, W.A. Comparison of Three Different Dietary Scores in Relation to 10-Year Mortality in Elderly European Subjects: The HALE Project. Eur. J. Clin. Nutr. 2006, 60, 746–755. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; De Curtis, A.; Persichillo, M.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; Iacoviello, L. Impact of Combined Healthy Lifestyle Factors on Survival in an Adult General Population and in High-Risk Groups: Prospective Results from the Moli-Sani Study. J. Intern. Med. 2019, 286, 207–220. [Google Scholar] [CrossRef]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; Gialluisi, A.; Persichillo, M.; Cerletti, C.; Donati, M.B.; De Gaetano, G.; Iacoviello, L. Mediterranean Diet and Mortality in the Elderly: A Prospective Cohort Study and a Meta-Analysis. Br. J. Nutr. 2018, 120, 841–854. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, S.A.; Bates, C.J.; Mishra, G.D. Diet Quality Is Associated with All-Cause Mortality in Adults Aged 65 Years and Older. J. Nutr. 2012, 142, 320–325. [Google Scholar] [CrossRef]
- Augood, C.; Fletcher, A.; Bentham, G.; Chakravarthy, U.; de Jong, P.T.V.M.; Rahu, M.; Seland, J.; Soubrane, G.; Tomazzoli, L.; Topouzis, F.; et al. Methods for a Population-Based Study of the Prevalence of and Risk Factors for Age-Related Maculopathy and Macular Degeneration in Elderly European Populations: The EUREYE Study. Ophthalmic Epidemiol. 2004, 11, 117–129. [Google Scholar] [CrossRef]
- Quiles, J.; Vioque, J. Prevalence of Obesity in the Valencian Community. Med. Clin. 1998, 110, 319. [Google Scholar]
- Vioque, J.; González, L. Validity of a Food Frequency Questionnaire (Preliminary Results). Eur. J. Cancer Prev. 1991, 1, 19–20. [Google Scholar] [CrossRef]
- Vioque, J.; Weinbrenner, T.; Asensio, L.; Castelló, A.; Young, I.S.; Fletcher, A. Plasma Concentrations of Carotenoids and Vitamin C Are Better Correlated with Dietary Intake in Normal Weight than Overweight and Obese Elderly Subjects. Br. J. Nutr. 2007, 97, 977–986. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture, Agricultural Research Service, USDA Nutrient Data Laboratory. USDA National Nutrient Database for Standard Reference; U.S. Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Nutrient Data Laboratory: Beltsville, MA, USA, 2008. [Google Scholar]
- Palma, I.; Farran, A.; Cantós, D. Tablas de Composición de Alimentos Por Medidas Caseras de Consumo Habitual En España, 1st ed.; Centre D´Ensenyament Superior de Nutrició i Dietètica (CESNID), Mc Graw-Hill Interamericana: Madrid, Spain, 2008. [Google Scholar]
- Martínez-González, M.A.; Buil-Cosiales, P.; Corella, D.; Bulló, M.; Fitó, M.; Vioque, J.; Romaguera, D.; Alfredo Martínez, J.; Wärnberg, J.; López-Miranda, J.; et al. Cohort Profile: Design and Methods of the PREDIMED-Plus Randomized Trial. Int. J. Epidemiol. 2019, 48, 387–388. [Google Scholar] [CrossRef]
- Lean, M.E.; Han, T.S.; Morrison, C.E. Waist Circumference as a Measure for Indicating Need for Weight Management. BMJ 1995, 311, 158. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean Diet and Health Status: An Updated Meta-Analysis and a Proposal for a Literature-Based Adherence Score. Public. Health Nutr. 2013, 17, 2769–2782. [Google Scholar] [CrossRef]
- Wang, Y.; Fan, H.; Ren, Z.; Liu, X.; Niu, X. Sleep Disorder, Mediterranean Diet, and All-Cause and Cause-Specific Mortality: A Prospective Cohort Study. BMC Public Health 2023, 23, 904. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Mattei, J.; Fung, T.T.; Li, Y.; Pan, A.; Willett, W.C.; Rimm, E.B.; Hu, F.B. Association of Changes in Diet Quality with Total and Cause-Specific Mortality. N. Engl. J. Med. 2017, 377, 143–153. [Google Scholar] [CrossRef]
- Hashemian, M.; Farvid, M.S.; Poustchi, H.; Murphy, G.; Etemadi, A.; Hekmatdoost, A.; Kamangar, F.; Sheikh, M.; Pourshams, A.; Sepanlou, S.G.; et al. The Application of Six Dietary Scores to a Middle Eastern Population: A Comparative Analysis of Mortality in a Prospective Study. Eur. J. Epidemiol. 2019, 34, 371–382. [Google Scholar] [CrossRef]
- Neelakantan, N.; Koh, W.P.; Yuan, J.M.; van Dam, R.M. Diet-Quality Indexes Are Associated with a Lower Risk of Cardiovascular, Respiratory, and All-Cause Mortality among Chinese Adults. J. Nutr. 2018, 148, 1323–1332. [Google Scholar] [CrossRef]
- Cárdenas-Fuentes, G.; Subirana, I.; Martinez-Gonzalez, M.A.; Salas-Salvadó, J.; Corella, D.; Estruch, R.; Fíto, M.; Muñoz-Bravo, C.; Fiol, M.; Lapetra, J.; et al. Multiple Approaches to Associations of Physical Activity and Adherence to the Mediterranean Diet with All-Cause Mortality in Older Adults: The PREvención Con DIeta MEDiterránea Study. Eur. J. Nutr. 2019, 58, 1569–1578. [Google Scholar] [CrossRef]
- Reedy, J.; Krebs-Smith, S.M.; Miller, P.E.; Liese, A.D.; Kahle, L.L.; Park, Y.; Subar, A.F. Higher Diet Quality Is Associated with Decreased Risk of All-Cause, Cardiovascular Disease, and Cancer Mortality among Older Adults. J. Nutr. 2014, 144, 881–889. [Google Scholar] [CrossRef]
- George, S.M.; Ballard-Barbash, R.; Manson, J.A.E.; Reedy, J.; Shikany, J.M.; Subar, A.F.; Tinker, L.F.; Vitolins, M.; Neuhouser, M.L. Comparing Indices of Diet Quality with Chronic Disease Mortality Risk in Postmenopausal Women in the Women’s Health Initiative Observational Study: Evidence to Inform National Dietary Guidance. Am. J. Epidemiol. 2014, 180, 616–625. [Google Scholar] [CrossRef]
- Lemming, E.W.; Byberg, L.; Wolk, A.; Michaëlsson, K. A Comparison between Two Healthy Diet Scores, the Modified Mediterranean Diet Score and the Healthy Nordic Food Index, in Relation to All-Cause and Cause-Specific Mortality. Br. J. Nutr. 2018, 119, 836–846. [Google Scholar] [CrossRef]
- World Cancer Research Fund & American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective; American Institute for Cancer Research (AICR): Washington, DC, USA, 2007; ISBN 9780972252225. [Google Scholar]
- Verberne, L.; Bach-Faig, A.; Buckland, G.; Serra-Majem, L. Association Between the Mediterranean Diet and Cancer Risk: A Review of Observational Studies. Nutr. Cancer 2010, 62, 860–870. [Google Scholar] [CrossRef]
- Kiani, A.K.; Medori, M.C.; Bonetti, G.; Aquilanti, B.; Velluti, V.; Matera, G.; Iaconelli, A.; Stuppia, L.; Connelly, S.T.; Herbst, K.L.; et al. Modern Vision of the Mediterranean Diet. J. Prev. Med. Hyg. 2022, 63, E36–E43. [Google Scholar] [CrossRef]
- Ditano-Vázquez, P.; Torres-Peña, J.D.; Galeano-Valle, F.; Pérez-Caballero, A.I.; Demelo-Rodríguez, P.; Lopez-Miranda, J.; Katsiki, N.; Delgado-Lista, J.; Alvarez-Sala-Walther, L.A. The Fluid Aspect of the Mediterranean Diet in the Prevention and Management of Cardiovascular Disease and Diabetes: The Role of Polyphenol Content in Moderate Consumption of Wine and Olive Oil. Nutrients 2019, 11, 2833. [Google Scholar] [CrossRef]
- Antoniazzi, L.; Arroyo-Olivares, R.; Bittencourt, M.S.; Tada, M.T.; Lima, I.; Jannes, C.E.; Krieger, J.E.; Pereira, A.C.; Quintana-Navarro, G.; Muñiz-Grijalvo, O.; et al. Adherence to a Mediterranean Diet, Dyslipidemia and Inflammation in Familial Hypercholesterolemia. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2014–2022. [Google Scholar] [CrossRef]
- Gärtner, C.; Stahl, W.; Sies, H. Lycopene is more bioavailable from tomato paste than from fresh tomatoes. Am. J. Clin. Nutr. 1997, 66, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, N.; Steppel, M.T.; Kampman, E.; De Groot, L.C.; Boshuizen, H.C.; Soedamah-Muthu, S.S.; Kromhout, D.; Feskens, E.J. Stability of Dietary Patterns Assessed with Reduced Rank Regression; The Zutphen Elderly Study. Nutr. J. 2014, 13, 30. [Google Scholar] [CrossRef]
- Newby, P.K.; Weismayer, C.; Akesson, A.; Tucker, K.L.; Wolk, A. Long-Term Stability of Food Patterns Identified by Use of Factor Analysis among Swedish Women. J. Nutr. 2006, 136, 626–633. [Google Scholar] [CrossRef] [PubMed]
| Total | aMED | rMED | erMEDAS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | p-Value 1 | T1 | T2 | T3 | p-Value 1 | T1 | T2 | T3 | p-Value 1 | ||
| N (%) | 903 (100) | 365 (40.4) | 387 (42.9) | 151 (16.7) | 308 (34.1) | 384 (42.5) | 211 (23.4) | 312 (34.6) | 340 (37.7) | 251 (27.8) | |||
| Score, mean (SD) | 1.6 (0.6) | 3.4 (0.5) | 5.5 (0.7) | 5.8 (1.3) | 9.0 (0.8) | 11.8 (1.1) | 3.3 (0.8) | 5.4 (0.5) | 8.1 (1.2) | ||||
| Score, range | 0.0–2.0 | 3.0–4.0 | 5.0–8.0 | 0.0–7.0 | 8.0–10.0 | 11.0–16.0 | 1.0–4.0 | 5.0–6.0 | 7.0–12.0 | ||||
| Study, n (%) | |||||||||||||
| EUREYE | 597 (66.1) | 235 (64.4) | 252 (65.1) | 110 (72.9) | 0.156 | 195 (63.3) | 261 (68.0) | 141 (66.8) | 0.424 | 224 (71.8) | 218 (64.1) | 155 (61.8) | 0.027 |
| VNS | 306 (33.9) | 130 (35.6) | 135 (34.9) | 41 (27.2) | 113 (36.7) | 123 (32.0) | 70 (33.2) | 88 (28.2) | 122 (35.9) | 96 (38.3) | |||
| Sex, n (%) | |||||||||||||
| Men | 392 (43.4) | 160 (43.8) | 170 (43.9) | 62 (41.1) | 0.815 | 110 (35.7) | 182 (47.4) | 100 (47.4) | 0.004 | 154 (49.4) | 157 (46.2) | 81 (32.3) | <0.001 |
| Women | 511 (56.6) | 205 (56.2) | 217 (56.1) | 89 (58.9) | 198 (64.3) | 202 (52.6) | 111 (52.6) | 158 (50.6) | 183 (53.8) | 170 (67.7) | |||
| Age, n (%) | |||||||||||||
| 65–74 years | 567 (62.8) | 223 (61.1) | 245 (63.3) | 99 (65.6) | 0.610 | 172 (55.8) | 247 (64.3) | 148 (70.1) | 0.003 | 197 (63.1) | 216 (63.5) | 154 (61.4) | 0.853 |
| ≥75 years | 336 (37.2) | 142 (38.9) | 142 (36.7) | 52 (34.4) | 136 (44.2) | 137 (35.7) | 63 (29.9) | 115 (36.9) | 124 (36.5) | 97 (38.7) | |||
| Educational level, n (%) | |||||||||||||
| <Primary school | 588 (65.1) | 240 (65.8) | 264 (68.2) | 84 (55.6) | 0.021 | 198 (64.3) | 251 (65.4) | 139 (65.9) | 0.924 | 201 (64.4) | 225 (66.2) | 162 (64.5) | 0.873 |
| ≥Primary school | 315 (34.9) | 125 (34.3) | 123 (31.8) | 67 (44.4) | 110 (35.7) | 133 (34.6) | 72 (34.1) | 111 (35.6) | 115 (33.8) | 89 (35.5) | |||
| Waist circumference (cm) 2, n (%) | |||||||||||||
| I | 97 (10.9) | 36 (10.0) | 40 (10.5) | 21 (14.0) | 0.624 | 27 (9.0) | 47 (12.3) | 23 (11.0) | 0.551 | 29 (9.4) | 46 (13.8) | 22 (8.9) | 0.109 |
| II | 204 (22.9) | 88 (24.5) | 83 (21.7) | 33 (22.0) | 64 (21.3) | 90 (23.6) | 50 (23.8) | 82 (26.5) | 69 (20.7) | 53 (21.4) | |||
| III | 590 (66.2) | 235 (65.5) | 259 (67.8) | 96 (64.0) | 209 (69.7) | 244 (64.0) | 137 (65.2) | 199 (64.2) | 218 (65.5) | 173 (69.8) | |||
| Smoking status, n (%) | |||||||||||||
| Never | 574 (63.7) | 230 (63.4) | 243 (62.8) | 101 (66.9) | 0.696 | 207 (67.4) | 240 (62.7) | 127 (60.2) | 0.129 | 186 (59.8) | 208 (61.4) | 180 (71.7) | 0.017 |
| Ex-smoker | 206 (22.9) | 79 (21.8) | 93 (24.0) | 34 (22.5) | 62 (20.2) | 84 (21.9) | 60 (28.4) | 73 (23.5) | 84 (24.8) | 49 (19.5) | |||
| Current | 121 (13.4) | 54 (14.9) | 51 (13.2) | 16 (10.6) | 38 (12.4) | 59 (15.4) | 24 (11.4) | 52 (16.7) | 47 (13.9) | 22 (8.8) | |||
| Diabetes 3, n (%) | |||||||||||||
| Yes | 175 (19.4) | 58 (15.9) | 85 (22.0) | 32 (21.2) | 0.094 | 52 (16.9) | 78 (20.3) | 45 (21.3) | 0.388 | 28 (9.0) | 71 (20.9) | 76 (30.3) | <0.001 |
| No | 727 (80.6) | 306 (84.1) | 302 (78.0) | 119 (78.8) | 255 (83.1) | 306 (79.7) | 166 (78.7) | 283 (91.0) | 269 (79.1) | 175 (69.7) | |||
| High cholesterol 3, n (%) | |||||||||||||
| Yes | 181 (20.2) | 57 (15.8) | 81 (21.1) | 43 (28.7) | 0.003 | 48 (15.7) | 78 (20.5) | 55 (26.2) | 0.002 | 55 (17.7) | 62 (18.5) | 64 (25.6) | 0.042 |
| No | 715 (79.8) | 305 (84.3) | 303 (78.9) | 107 (71.3) | 257 (84.3) | 303 (79.5) | 155 (73.8) | 256 (82.3) | 273 (81.5) | 186 (74.4) | |||
| Hypertension 3, n (%) | |||||||||||||
| Yes | 359 (40.1) | 142 (39.3) | 163 (42.5) | 54 (36.0) | 0.364 | 121 (39.8) | 159 (41.7) | 79 (37.6) | 0.615 | 129 (41.8) | 121 (36.0) | 109 (43.6) | 0.138 |
| No | 536 (59.9) | 219 (60.7) | 221 (57.6) | 96 (64.0) | 183 (60.2) | 222 (58.3) | 131 (62.4) | 180 (58.3) | 215 (64.0) | 141 (56.4) | |||
| TV watching, h/d, mean, SD | 3.8 (2.0) | 3.8 (1.9) | 3.9 (2.1) | 3.4 (1.6) | 0.001 | 3.8 (2.0) | 3.9 (2.1) | 3.8 (1.8) | 0.151 | 3.9 (1.9) | 3.8 (2.0) | 3.7 (1.9) | 0.585 |
| Sleeping time, h/d mean, SD | 7.8 (2.0) | 7.9 (2.1) | 7.8 (2.0) | 7.6 (1.9) | 0.587 | 8.0 (2.1) | 7.8 (2.0) | 7.5 (1.9) | 0.141 | 8.0 (2.0) | 7.9 (2.1) | 7.5 (1.9) | 0.418 |
| T1 | T2 | T3 | p-Value 2 | p-Trend 3 | Per Two-Point Increase | |
|---|---|---|---|---|---|---|
| aMED | ||||||
| All-cause (n, %) | 365 (40.4) | 387 (42.9) | 151 (16.7) | |||
| Deaths, n | 182 | 170 | 51 | |||
| Person-years | 3423.7 | 3676.6 | 1549.7 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 0.88 (0.71–1.08) | 0.61 (0.45–0.84) | 0.002 | 0.001 | 0.81 (0.71–0.92) |
| Multivariable 1 | Ref | 0.87 (0.70–1.08) | 0.70 (0.51–0.96) | 0.026 | 0.008 | 0.83 (0.73–0.95) |
| CVD (n, %) | 256 (38.8) | 286 (43.3) | 118 (17.9) | |||
| Deaths, n | 73 | 69 | 18 | |||
| Person-years | 2689.0 | 3045.6 | 1327.4 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 0.82 (0.60–1.15) | 0.49 (0.29–0.82) | 0.007 | 0.007 | 0.75 (0.61–0.93) |
| Multivariable 1 | Ref | 0.83 (0.59–1.18) | 0.60 (0.35–1.02) | 0.060 | 0.037 | 0.79 (0.64–0.99) |
| Cancer (n, %) | 218 (36.9) | 259 (43.9) | 113 (19.2) | |||
| Deaths, n | 35 | 42 | 13 | |||
| Person-years | 2419.5 | 2844.4 | 1271.4 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 1.03 (0.66–1.61) | 0.70 (0.37–1.32) | 0.273 | 0.118 | 0.80 (0.61–1.06) |
| Multivariable 1 | Ref | 1.08 (0.68–1.71) | 0.86 (0.45–1.64) | 0.642 | 0.392 | 0.88 (0.66–1.18) |
| rMED | ||||||
| All-cause (n, %) | 308 (34.1) | 384 (42.5) | 211 (23.4) | |||
| Deaths, n | 156 | 170 | 77 | |||
| Person-years | 2799.3 | 3757.5 | 2093.2 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 0.80 (0.64–1.00) | 0.70 (0.53–0.92) | 0.012 | 0.006 | 0.90 (0.83–0.97) |
| Multivariable 1 | Ref | 0.82 (0.65–1.03) | 0.76 (0.57–1.01) | 0.057 | 0.028 | 0.91 (0.84–0.99) |
| CVD (n, %) | 216 (32.7) | 278 (42.1) | 166 (25.2) | |||
| Deaths, n | 64 | 64 | 32 | |||
| Person-years | 2247.9 | 3004.9 | 1809.2 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 0.75 (0.53–1.06) | 0.69 (0.45–1.06) | 0.099 | 0.048 | 0.88 (0.78–1.00) |
| Multivariable 1 | Ref | 0.79 (0.55–1.13) | 0.79 (0.51–1.23) | 0.292 | 0.180 | 0.91 (0.80–1.04) |
| Cancer (n, %) | 187 (31.7) | 255 (43.2) | 148 (25.1) | |||
| Deaths, n | 35 | 41 | 14 | |||
| Person-years | 2012.5 | 2816.0 | 1706.8 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 0.82 (0.52–1.28) | 0.50 (0.27–0.94) | 0.030 | 0.025 | 0.83 (0.70–0.98) |
| Multivariable 1 | Ref | 0.85 (0.53–1.36) | 0.55 (0.29–1.04) | 0.066 | 0.082 | 0.85 (0.72–1.02) |
| erMEDAS | ||||||
| All-cause (n, %) | 312 (34.6) | 340 (37.7) | 251 (27.8) | |||
| Deaths, n | 137 | 164 | 102 | |||
| Person-years | 3007.4 | 3190.3 | 2452.2 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 1.19 (0.95–1.49) | 1.00 (0.77–1.30) | 0.992 | 0.977 | 1.00 (0.91–1.10) |
| Multivariable 1 | Ref | 1.07 (0.85–1.36) | 0.86 (0.65–1.13) | 0.280 | 0.257 | 0.94 (0.85–1.04) |
| CVD (n, %) | 224 (33.9) | 245 (37.1) | 191 (28.9) | |||
| Deaths, n | 49 | 69 | 42 | |||
| Person-years | 2423.1 | 2596.1 | 2042.7 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 1.40 (0.97–2.02) | 1.04 (0.68–1.59) | 0.845 | 0.915 | 0.99 (0.85–1.16) |
| Multivariable 1 | Ref | 1.25 (0.85–1.84) | 0.84 (0.53–1.31) | 0.436 | 0.242 | 0.91 (0.77–1.07) |
| Cancer (n, %) | 206 (34.9) | 210 (35.6) | 174 (29.5) | |||
| Deaths, n | 31 | 34 | 25 | |||
| Person-years | 2266.2 | 2310.4 | 1958.7 | |||
| HR (95% CI) | ||||||
| Age- and sex-adjusted | Ref | 1.18 (0.72–1.92) | 1.11 (0.65–1.91) | 0.693 | 0.040 | 1.02 (0.83–1.26) |
| Multivariable 1 | Ref | 1.16 (0.70–1.91) | 1.07 (0.61–1.87) | 0.818 | 0.982 | 1.00 (0.80–1.25) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ojeda-Belokon, C.; González-Palacios, S.; Compañ-Gabucio, L.M.; Oncina-Cánovas, A.; García-de-la-Hera, M.; Vioque, J.; Torres-Collado, L. Adherence to Three Mediterranean Dietary Indexes and All-Cause, Cardiovascular, and Cancer Mortality in an Older Mediterranean Population. Nutrients 2025, 17, 2956. https://doi.org/10.3390/nu17182956
Ojeda-Belokon C, González-Palacios S, Compañ-Gabucio LM, Oncina-Cánovas A, García-de-la-Hera M, Vioque J, Torres-Collado L. Adherence to Three Mediterranean Dietary Indexes and All-Cause, Cardiovascular, and Cancer Mortality in an Older Mediterranean Population. Nutrients. 2025; 17(18):2956. https://doi.org/10.3390/nu17182956
Chicago/Turabian StyleOjeda-Belokon, Carolina, Sandra González-Palacios, Laura María Compañ-Gabucio, Alejandro Oncina-Cánovas, Manuela García-de-la-Hera, Jesús Vioque, and Laura Torres-Collado. 2025. "Adherence to Three Mediterranean Dietary Indexes and All-Cause, Cardiovascular, and Cancer Mortality in an Older Mediterranean Population" Nutrients 17, no. 18: 2956. https://doi.org/10.3390/nu17182956
APA StyleOjeda-Belokon, C., González-Palacios, S., Compañ-Gabucio, L. M., Oncina-Cánovas, A., García-de-la-Hera, M., Vioque, J., & Torres-Collado, L. (2025). Adherence to Three Mediterranean Dietary Indexes and All-Cause, Cardiovascular, and Cancer Mortality in an Older Mediterranean Population. Nutrients, 17(18), 2956. https://doi.org/10.3390/nu17182956








