Adherence to the Provegetarian Food Patterns and Incidence of All-Cause Mortality in a Mediterranean Population: The SUN Cohort
Highlights
- Greater adherence to a provegetarian dietary pattern, which emphasizes plant-based food without completely excluding animal products, was significantly associated with a 32% lower risk of total mortality.
- A plant-based food dietary pattern, characterized by a high consumption of refined grains, French fries, sugar-sweetened beverages, fruit juices and pastries, although plant-based, was not associated with a reduced mortality.
- Promoting a healthy plant-based dietary pattern should be a public health priority to improve population health and reduce mortality from all causes.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Dietary Assessment
2.3. Outcome Assessment
2.4. Assessment of Other Variables
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PVG | Provegetarian |
| hPVG | Healthful provegetarian |
| uPVG | Unhealthful provegetarian |
| SUN | Seguimiento Universidad de Navarra |
References
- Wang, P.; Song, M.; Eliassen, A.H.; Wang, M.; Fung, T.T.; Clinton, S.K.; Rimm, E.B.; Hu, F.B.; Willett, W.C.; Tabung, F.K.; et al. Optimal Dietary Patterns for Prevention of Chronic Disease. Nat. Med. 2023, 29, 719–728. [Google Scholar] [CrossRef]
- Shan, Z.; Wang, F.; Li, Y.; Baden, M.Y.; Bhupathiraju, S.N.; Wang, D.D.; Sun, Q.; Rexrode, K.M.; Rimm, E.B.; Qi, L.; et al. Healthy Eating Patterns and Risk of Total and Cause-Specific Mortality. JAMA Intern. Med. 2023, 183, 142–153. [Google Scholar] [CrossRef]
- Neuenschwander, M.; Stadelmaier, J.; Eble, J.; Grummich, K.; Szczerba, E.; Kiesswetter, E.; Schlesinger, S.; Schwingshackl, L. Substitution of Animal-Based with Plant-Based Foods on Cardiometabolic Health and All-Cause Mortality: A Systematic Review and Meta-Analysis of Prospective Studies. BMC Med. 2023, 21, 404. [Google Scholar] [CrossRef] [PubMed]
- Acevedo Cantero, P.; Ortega Santos, C.P.; López-Ejeda, N. Vegetarian Diets in Spain: Temporal Evolution through National Health Surveys and Their Association with Healthy Lifestyles. Endocrinol. Diabetes Nutr. 2023, 70, 1–8. [Google Scholar] [CrossRef]
- Janssen, M.; Busch, C.; Rödiger, M.; Hamm, U. Motives of Consumers Following a Vegan Diet and Their Attitudes towards Animal Agriculture. Appetite 2016, 105, 643–651. [Google Scholar] [CrossRef]
- Nelson, M.E.; Hamm, M.W.; Hu, F.B.; Abrams, S.A.; Griffin, T.S. Alignment of Healthy Dietary Patterns and Environmental Sustainability: A Systematic Review. Adv. Nutr. 2016, 7, 1005–1025. [Google Scholar] [CrossRef]
- Springmann, M.; Wiebe, K.; Mason-D’Croz, D.; Sulser, T.B.; Rayner, M.; Scarborough, P. Health and Nutritional Aspects of Sustainable Diet Strategies and Their Association with Environmental Impacts: A Global Modelling Analysis with Country-Level Detail. Lancet Planet. Health 2018, 2, E451–E461. [Google Scholar] [CrossRef]
- Clarys, P.; Deliens, T.; Huybrechts, I.; Deriemaeker, P.; Vanaelst, B.; De Keyzer, W.; Hebbelinck, M.; Mullie, P. Comparison of Nutritional Quality of the Vegan, Vegetarian, Semi-Vegetarian, Pesco-Vegetarian and Omnivorous Diet. Nutrients 2014, 6, 1318–1332. [Google Scholar] [CrossRef] [PubMed]
- Key, T.J.; Appleby, P.N.; Spencer, E.A.; Travis, R.C.; Roddam, A.W.; Allen, N.E. Mortality in British Vegetarians: Results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford). Am. J. Clin. Nutr. 2009, 89, 1613S–1619S. [Google Scholar] [CrossRef]
- Orlich, M.J.; Singh, P.N.; Sabaté, J.; Jaceldo-Siegl, K.; Fan, J.; Knutsen, S.; Beeson, W.L.; Fraser, G.E. Vegetarian Dietary Patterns and Mortality in Adventist Health Study 2. JAMA Intern. Med. 2013, 173, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- Blackie, K.; Bobe, G.; Takata, Y. Vegetarian Diets and Risk of All-Cause Mortality in a Population-Based Prospective Study in the United States. J. Health Popul. Nutr. 2023, 42, 130. [Google Scholar] [CrossRef]
- Chang-Claude, J.; Hermann, S.; Eilber, U.; Steindorf, K. Lifestyle Determinants and Mortality in German Vegetarians and Health-Conscious Persons: Results of a 21-Year Follow-Up. Cancer Epidemiol. Biomark. Prev. 2005, 14, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Petermann-Rocha, F.; Parra-Soto, S.; Gray, S.; Anderson, J.; Welsh, P.; Gill, J.; Sattar, N.; Ho, F.K.; Celis-Morales, C.; Pell, J.P. Vegetarians, Fish, Poultry, and Meat-Eaters: Who Has Higher Risk of Cardiovascular Disease and Mortality? A Prospective Study Biobank. Eur. Heart J. 2021, 42, 1136–1143. [Google Scholar] [CrossRef]
- Mihrshahi, S.; Ding, D.; Gale, J.; Allman-Farinelli, M.; Banks, E.; Bauman, A.E. Vegetarian Diet and All-Cause Mortality: Evidence from a Large Population-Based Australian Cohort—The 45 and Up Study. Prev. Med. 2017, 97, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Appleby, P.N.; Crowe, F.L.; Bradbury, K.E.; Travis, R.C.; Key, T.J. Mortality in Vegetarians and Comparable Nonvegetarians in the United Kingdom. Am. J. Clin. Nutr. 2016, 103, 218–230. [Google Scholar] [CrossRef]
- Abris, G.P.; Shavlik, D.J.; Mathew, R.O.; Butler, F.M.; Oh, J.; Sirirat, R.; Sveen, L.E.; Fraser, G.E. Cause-Specific and All-Cause Mortalities in Vegetarian Compared with Those in Nonvegetarian Participants from the Adventist Health Study-2 Cohort. Am. J. Clin. Nutr. 2024, 120, 907–917. [Google Scholar] [CrossRef]
- Key, T.J.; Fraser, G.E.; Thorogood, M.; Appleby, P.N.; Beral, V.; Reeves, G.; Burr, M.L.; Chang-Claude, J.; Frentzel-Beyme, R.; Kuzma, J.W.; et al. Mortality in Vegetarians and Nonvegetarians: Detailed Findings from a Collaborative Analysis of 5 Prospective Studies. Am. J. Clin. Nutr. 1999, 70, 516S–524S. [Google Scholar] [CrossRef]
- Satija, A.; Bhupathiraju, S.N.; Rimm, E.B.; Spiegelman, D.; Chiuve, S.E.; Borgi, L.; Willett, W.C.; Manson, J.A.E.; Sun, Q.; Hu, F.B. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLoS Med. 2016, 13, e1002039. [Google Scholar] [CrossRef]
- Bhandari, B.; Liu, Z.; Lin, S.; Macniven, R.; Akombi-Inyang, B.; Hall, J.; Feng, X.; Schutte, A.E.; Xu, X. Long-Term Consumption of 10 Food Groups and Cardiovascular Mortality: A Systematic Review and Dose Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2023, 14, 55–63. [Google Scholar] [CrossRef]
- Benisi-Kohansal, S.; Saneei, P.; Salehi-Marzijarani, M.; Larijani, B.; Esmaillzadeh, A. Whole-Grain Intake and Mortality from All Causes, Cardiovascular Disease, and Cancer: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2016, 7, 1052–1065. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Liang, H.; Yang, H.; Zhang, X.; Ding, X.; Zhang, R.; Mao, Y.; Liu, Z.; Kan, Q.; Sun, T. Association between Intake of Sweetened Beverages with All-Cause and Cause-Specific Mortality: A Systematic Review and Meta-Analysis. J. Public Health 2022, 44, 516–526. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Sánchez-Tainta, A.; Corella, D.; Salas-Salvadó, J.; Ros, E.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; Lamuela-Raventós, R.M.; Schröder, H.; et al. A Provegetarian Food Pattern and Reduction in Total Mortality in the Prevención Con Dieta Mediterránea (PREDIMED) Study. Am. J. Clin. Nutr. 2014, 100, 320S–328S. [Google Scholar] [CrossRef]
- Li, H.; Zeng, X.; Wang, Y.; Zhang, Z.; Zhu, Y.; Li, X.; Hu, A.; Zhao, Q.; Yang, W. A Prospective Study of Healthful and Unhealthful Plant-Based Diet and Risk of Overall and Cause-Specific Mortality. Eur. J. Nutr. 2022, 61, 387–398. [Google Scholar] [CrossRef]
- Zhou, L.; Zhang, R.; Yang, H.; Zhang, S.; Zhang, Y.; Li, H.; Chen, Y.; Maimaitiyiming, M.; Lin, J.; Ma, Y.; et al. Association of Plant-Based Diets with Total and Cause-Specific Mortality across Socioeconomic Deprivation Level: A Large Prospective Cohort. Eur. J. Nutr. 2024, 63, 835–846. [Google Scholar] [CrossRef]
- Wang, D.D.; Li, Y.; Nguyen, X.M.T.; Song, R.J.; Ho, Y.L.; Hu, F.B.; Willett, W.C.; Wilson, P.; Cho, K.; Gaziano, J.M.; et al. Degree of Adherence to Plant-Based Diet and Total and Cause-Specific Mortality: Prospective Cohort Study in the Million Veteran Program. Public Health Nutr. 2023, 26, 381–392. [Google Scholar] [CrossRef]
- Mo, Q.; Wu, J.; Lu, Y.; Zhang, X. Plant-Based Diets and Total and Cause-Specific Mortality: A Meta-Analysis of Prospective Studies. Front. Nutr. 2025, 12, 1518519. [Google Scholar] [CrossRef] [PubMed]
- Carlos, S.; De La Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Razquin, C.; Rico-Campà, A.; Martínez-González, M.A.; Ruiz-Canela, M. Mediterranean Diet and Health Outcomes in the SUN Cohort. Nutrients 2018, 10, 439. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C. Nutritional Epidemiology, 3rd ed.; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Martin-Moreno, J.M.; Boyle, P.; Gorgojo, L.; Maisonneuve, P.; Fernandez-Rodriguez, J.C.; Salvini, S.; Willett, W.C. Development and Validation of a Food Frequency Questionnaire in Spain. Int. J. Epidemiol. 1993, 22, 512–519. [Google Scholar] [CrossRef] [PubMed]
- De La Fuente-Arrillaga, C.; Vzquez Ruiz, Z.; Bes-Rastrollo, M.; Sampson, L.; Martinez-González, M.A. Reproducibility of an FFQ Validated in Spain. Public Health Nutr. 2010, 13, 1364–1372. [Google Scholar] [CrossRef]
- Oncina-Cánovas, A.; Vioque, J.; González-Palacios, S.; Martínez-González, M.Á.; Salas-Salvadó, J.; Corella, D.; Zomeño, D.; Martínez, J.A.; Alonso-Gómez, Á.M.; Wärnberg, J.; et al. Pro-Vegetarian Food Patterns and Cardiometabolic Risk in the PREDIMED-Plus Study: A Cross-Sectional Baseline Analysis. Eur. J. Nutr. 2022, 61, 357–372. [Google Scholar] [CrossRef]
- Bes-Rastrollo, M.; Pérez Valdivieso, J.R.; Sánchez-Villegas, A.; Alonso, Á.; Martínez-González, M.A. Validación Del Peso e Índice de Masa Corporal Auto-Declarados de Los Participantes de Una Cohorte de Graduados Universitarios. Rev. Esp. Obes. 2005, 3, 352–358. [Google Scholar]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean Diet and Survival in a Greek Population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef]
- Van Der Weele, T.J.; Ding, P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern. Med. 2017, 167, 268–274. [Google Scholar] [CrossRef]
- Kim, J.; Kim, H.; Giovannucci, E.L. Plant-Based Diet Quality and the Risk of Total and Disease-Specific Mortality: A Population-Based Prospective Study. Clin. Nutr. 2021, 40, 5718–5725. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Caulfield, L.E.; Garcia-Larsen, V.; Steffen, L.M.; Coresh, J.; Rebholz, C.M. Plant-Based Diets Are Associated with a Lower Risk of Incident Cardiovascular Disease, Cardiovascular Disease Mortality, and All-Cause Mortality in a General Population of Middle-Aged Adults. J. Am. Heart Assoc. 2019, 8, e012865. [Google Scholar] [CrossRef] [PubMed]
- Baden, M.Y.; Liu, G.; Satija, A.; Li, Y.; Sun, Q.; Fung, T.T.; Rimm, E.B.; Willett, W.C.; Hu, F.B.; Bhupathiraju, S.N. Changes in Plant-Based Diet Quality and Total and Cause-Specific Mortality. Circulation 2019, 140, 979–991. [Google Scholar] [CrossRef]
- Jafari, S.; Hezaveh, E.; Jalilpiran, Y.; Jayedi, A.; Wong, A.; Safaiyan, A.; Barzegar, A. Plant-Based Diets and Risk of Disease Mortality: A Systematic Review and Meta-Analysis of Cohort Studies. Crit. Rev. Food Sci. Nutr. 2022, 62, 7760–7772. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Shen, J.; Xuan, J.; Zhu, A.; Ji, J.S.; Liu, X.; Cao, Y.; Zong, G.; Zeng, Y.; Wang, X.; et al. Plant-Based Dietary Patterns in Relation to Mortality among Older Adults in China. Nat. Aging 2022, 2, 224–230. [Google Scholar] [CrossRef]
- Yuan, F.; Wen, W.; Shu, X.O.; Lipworth, L.; Shrubsole, M.J.; Yu, D.; Zheng, W. Plant-Based Diets and Mortality in Black and Low-Income Americans: Findings from a Large Prospective Cohort Study. Am. J. Clin. Nutr. 2025, 121, 1346–1353. [Google Scholar] [CrossRef]
- Etesami, E.; Nikparast, A.; Rahmani, J.; Rezaei, M.; Ghanavati, M. The Association between Overall, Healthy, and Unhealthy Plant-Based Diet Indexes and Risk of All-Cause and Cause-Specific Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Food Funct. 2025, 16, 2194–2212. [Google Scholar] [CrossRef]
- Delgado-Velandia, M.; Maroto-Rodríguez, J.; Ortolá, R.; García-Esquinas, E.; Rodríguez-Artalejo, F.; Sotos-Prieto, M. Plant-Based Diets and All-Cause and Cardiovascular Mortality in a Nationwide Cohort in Spain: The ENRICA Study. Mayo Clin. Proc. 2022, 97, 2005–2015. [Google Scholar] [CrossRef]
- Oncina-Cánovas, A.; Torres-Collado, L.; García-de-la-Hera, M.; Compañ-Gabucio, L.M.; González-Palacios, S.; Signes-Pastor, A.J.; Vioque, J. Pro-Vegetarian Dietary Patterns and Mortality by All-Cause and Specific Causes in an Older Mediterranean Population. J. Nutr. Health Aging 2024, 28, 100239. [Google Scholar] [CrossRef]
- Thompson, A.S.; Tresserra-Rimbau, A.; Karavasiloglou, N.; Jennings, A.; Cantwell, M.; Hill, C.; Perez-Cornago, A.; Bondonno, N.P.; Murphy, N.; Rohrmann, S.; et al. Association of Healthful Plant-Based Diet Adherence with Risk of Mortality and Major Chronic Diseases among Adults in the UK. JAMA Netw. Open 2023, 6, e234714. [Google Scholar] [CrossRef]
- Kim, H.; Caulfield, L.E.; Rebholz, C.M. Healthy Plant-Based Diets Are Associated with Lower Risk of All-Cause Mortality in US Adults. J. Nutr. 2018, 148, 624–631. [Google Scholar] [CrossRef]
- Tao, H.W.; Han, W.W.; Fang, F.; Miao, M.Y.; Du, H.Z.; Li, Z.N.; Chen, J.S.; Qin, L.Q.; Chen, G.C. Plant-Based Diets, Mediating Biomarkers, and Mortality Risk among Adults with Diabetes or Prediabetes. Food Funct. 2024, 15, 4223–4232. [Google Scholar] [CrossRef]
- Kim, J.; Wilkens, L.R.; Haiman, C.A.; Le Marchand, L.; Park, S.Y. Plant-Based Dietary Patterns and Mortality from All Causes, Cardiovascular Disease, and Cancer: The Multiethnic Cohort Study. Clin. Nutr. 2024, 43, 1447–1453. [Google Scholar] [CrossRef]
- Huang, S.; Lou, Y.; Wang, S.; You, Q.; Jiang, Q.; Cao, S. Association of Changes in Plant-Based Diet Consumption with All-Cause Mortality among Older Adults in China: A Prospective Study from 2008 to 2019. J. Nutr. Health Aging 2024, 28, 100027. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Zhang, S.; Jiang, Y.; Li, J.; Yang, C. Plant-Based Diet and Risk of All-Cause Mortality: A Systematic Review and Meta-Analysis. Front. Nutr. 2024, 11, 1481363. [Google Scholar] [CrossRef] [PubMed]
- Weston, L.J.; Kim, H.; Talegawkar, S.A.; Tucker, K.L.; Correa, A.; Rebholz, C.M. Plant-Based Diets and Incident Cardiovascular Disease and All-Cause Mortality in African Americans: A Cohort Study. PLoS Med. 2022, 19, e1003863. [Google Scholar] [CrossRef] [PubMed]
- Zazpe, I.; Santiago, S.; Toledo, E.; Bes-Rastrollo, M.; de la Fuente-Arrillaga, C.; Martínez-González, M.Á. Diet Quality Indices in the SUN Cohort: Observed Changes and Predictors of Changes in Scores Over a 10-Year Period. J. Acad. Nutr. Diet. 2021, 121, 1948–1960.e7. [Google Scholar] [CrossRef] [PubMed]
- Gan, Z.H.; Cheong, H.C.; Tu, Y.K.; Kuo, P.H. Association between Plant-Based Dietary Patterns and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 3952. [Google Scholar] [CrossRef]
- Li, Y.; Wang, D.D.; Nguyen, X.M.T.; Song, R.J.; Ho, Y.L.; Hu, F.B.; Willett, W.C.; Wilson, P.W.F.; Cho, K.; Gaziano, J.M.; et al. Plant-Based Diets and the Incidence of Cardiovascular Disease: The Million Veteran Program. BMJ Nutr. Prev. Health 2023, 6, 212–220. [Google Scholar] [CrossRef]
- Capodici, A.; Mocciaro, G.; Gori, D.; Landry, M.J.; Masini, A.; Sanmarchi, F.; Fiore, M.; Coa, A.A.; Castagna, G.; Gardner, C.D.; et al. Cardiovascular Health and Cancer Risk Associated with Plant Based Diets: An Umbrella Review. PLoS ONE 2024, 19, e0300711. [Google Scholar] [CrossRef]
- Khan, J.; Gul, P.; Rashid, M.T.; Li, Q.; Liu, K. Composition of Whole Grain Dietary Fiber and Phenolics and Their Impact on Markers of Inflammation. Nutrients 2024, 16, 1047. [Google Scholar] [CrossRef]
- Cassidy, A.; Rogers, G.; Peterson, J.J.; Dwyer, J.T.; Lin, H.; Jacques, P.F. Higher Dietary Anthocyanin and Flavonol Intakes Are Associated with Anti-Inflammatory Effects in a Population of US Adults. Am. J. Clin. Nutr. 2015, 102, 172–181. [Google Scholar] [CrossRef]
- Wang, Q.; Liu, R.; Chang, M.; Zhang, H.; Jin, Q.; Wang, X. Dietary Oleic Acid Supplementation and Blood Inflammatory Markers: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Crit. Rev. Food Sci. Nutr. 2022, 62, 2508–2525. [Google Scholar] [CrossRef]
- Song, M.; Fung, T.T.; Hu, F.B.; Willett, W.C.; Longo, V.D.; Chan, A.T.; Giovannucci, E.L. Association of Animal and Plant Protein Intake with All-Cause and Cause-Specific Mortality. JAMA Intern. Med. 2016, 176, 1453–1463. [Google Scholar] [CrossRef]
- Budhathoki, S.; Sawada, N.; Iwasaki, M.; Yamaji, T.; Goto, A.; Kotemori, A.; Ishihara, J.; Takachi, R.; Charvat, H.; Mizoue, T.; et al. Association of Animal and Plant Protein Intake with All-Cause and Cause-Specific Mortality in a Japanese Cohort. JAMA Intern. Med. 2019, 179, 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Ruiz, Z.; Toledo, E.; Vitelli-Storelli, F.; Bes-Rastrollo, M.; Martínez-González, M.Á. Effect of Dietary Phenolic Compounds Intake on Mortality in the “Seguimiento Universidad De Navarra” (SUN) Mediterranean Cohort. Eur. J. Nutr. 2025, 64, 70. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Bes-Rastrollo, M.; Toledo, E.; Gea, A.; Fresán, U.; Barbagallo, M.; Martínez-González, M.A. Dietary Fiber Intake and Mortality in a Mediterranean Population: The “Seguimiento Universidad de Navarra” (SUN) Project. Eur. J. Nutr. 2019, 58, 3009–3022. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Je, Y.; Giovannucci, E.L. Association between Dietary Fat Intake and Mortality from All-Causes, Cardiovascular Disease, and Cancer: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Clin. Nutr. 2021, 40, 1060–1070. [Google Scholar] [CrossRef]
- Wang, Y.B.; Page, A.J.; Gill, T.K.; Melaku, Y.A. The Association between Diet Quality, Plant-Based Diets, Systemic Inflammation, and Mortality Risk: Findings from NHANES. Eur. J. Nutr. 2023, 62, 2723–2737. [Google Scholar] [CrossRef]
- Sidhu, S.R.K.; Kok, C.W.; Kunasegaran, T.; Ramadas, A. Effect of Plant-Based Diets on Gut Microbiota: A Systematic Review of Interventional Studies. Nutrients 2023, 15, 1510. [Google Scholar] [CrossRef]
- Hamjane, N.; Mechita, M.B.; Nourouti, N.G.; Barakat, A. Gut Microbiota Dysbiosis-Associated Obesity and Its Involvement in Cardiovascular Diseases and Type 2 Diabetes. A Systematic Review. Microvasc. Res. 2024, 151, 104601. [Google Scholar] [CrossRef]
- Barbería-Latasa, M.; Martínez-González, M.A.; de la Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Carlos, S.; Gea, A. Predictors of Total Mortality and Their Differential Association on Premature or Late Mortality in the SUN Cohort. Exp. Gerontol. 2023, 172, 112048. [Google Scholar] [CrossRef]
- Soltani, S.; Jayedi, A.; Shab-Bidar, S.; Becerra-Tomás, N.; Salas-Salvadó, J. Adherence to the Mediterranean Diet in Relation to All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2019, 10, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Hemler, E.C.; Hu, F.B. Plant-Based Diets for Personal, Population, and Planetary Health. Adv. Nutr. 2019, 10, S275–S283. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Stubbendorff, A.; Sonestedt, E.; Ramne, S.; Drake, I.; Hallström, E.; Ericson, U. Development of an EAT-Lancet Index and Its Relation to Mortality in a Swedish Population. Am. J. Clin. Nutr. 2022, 115, 705–716. [Google Scholar] [CrossRef]
- Bui, L.P.; Pham, T.T.; Wang, F.; Chai, B.; Sun, Q.; Hu, F.B.; Lee, K.H.; Guasch-Ferre, M.; Willett, W.C. Planetary Health Diet Index and Risk of Total and Cause-Specific Mortality in Three Prospective Cohorts. Am. J. Clin. Nutr. 2024, 120, 80–91. [Google Scholar] [CrossRef] [PubMed]
- Winckers, A.N.E.; MacKenbach, J.D.; Compernolle, S.; Nicolaou, M.; Van Der Ploeg, H.P.; De Bourdeaudhuij, I.; Brug, J.; Lakerveld, J. Educational Differences in the Validity of Self-Reported Physical Activity Energy Balance-Related Behaviours. BMC Public Health 2015, 15, 1299. [Google Scholar] [CrossRef] [PubMed]
- Roos, E.; Prättälä, R.; Lahelma, E.; Kleemola, P.; Pietinen, P. Modern and healthy? Socio-economic differences in the quality of diet. Eur. J. Clin. Nutr. 1996, 50, 753–760. [Google Scholar] [PubMed]
| PVG | hPVG | uPVG | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Q1 | Q2–Q4 | Q5 | Q1 | Q2–Q4 | Q5 | Q1 | Q2–Q4 | Q5 |
| n | 4278 | 10,215 | 3496 | 4090 | 10,634 | 3265 | 4130 | 10,559 | 3300 |
| Provegetarian score range | 29–52 | 53–62 | 63–81 | 34–51 | 52–63 | 64–86 | 31–51 | 52–63 | 64–87 |
| Age (years) | 35.3 (11.4) | 37.5 (11.7) | 39.7 (11.8) | 32.9 (9.8) | 37.6 (11.6) | 42.5 (12.2) | 41.0 (12.3) | 37.2 (11.6) | 33.8 (10.2) |
| Female (%) | 59.9 | 61.8 | 59.7 | 60.8 | 61.2 | 60.2 | 60.9 | 61.1 | 60.4 |
| Married (%) | 44.3 | 50.2 | 53.2 | 37.6 | 51.03 | 58.5 | 57.1 | 49.0 | 40.8 |
| Years of university education | 5.0 (1.4) | 5.0 (1.5) | 5.2 (1.6) | 5.0 (1.5) | 5.1 (1.5) | 5.1 (1.5) | 5.1 (1.5) | 5.1 (1.5) | 5.0 (1.4) |
| BMI (kg/m2) | 23.3 (3.4) | 23.5 (3.5) | 23.5 (3.4) | 23.1 (3.4) | 23.5 (3.5) | 23.6 (3.5) | 23.9 (3.5) | 23.4 (3.5) | 23.0 (3.3) |
| Physical activity (METs-h/week) | 21.3 (23.4) | 21.6 (22.3) | 23.1 (24.5) | 19.9 (22.2) | 21.5 (22.3) | 25.6 (25.7) | 23.7 (23.7) | 21.7 (23.1) | 19.9 (21.5) |
| Cumulative smoking habit (pack-years) | 5.3 (9.4) | 5.8 (9.4) | 6.6 (9.7) | 4.0 (7.5) | 6.0 (9.7) | 7.5 (10.5) | 7.3 (10.5) | 5.7 (9.3) | 4.4 (8.3) |
| Smoking (%) | |||||||||
| Never smoker | 52.1 | 49.6 | 46.0 | 56.3 | 48.5 | 44.2 | 44.7 | 49.7 | 55.1 |
| Current smoker | 23.2 | 22.0 | 21.3 | 23.5 | 22.9 | 18.1 | 20.3 | 22.5 | 23.4 |
| Former smoker | 24.6 | 21.3 | 32.7 | 20.2 | 28.6 | 37.7 | 35.0 | 27.8 | 21.6 |
| Television watching (h/d) | 1.7 (1.2) | 1.6 (1.1) | 1.5 (1.1) | 1.7 (1.3) | 1.6 (1.1) | 1.5 (1.1) | 1.6 (1.1) | 1.6 (1.1) | 1.7 (1.2) |
| Snacking between meals (%) | 37.8 | 33.1 | 29.3 | 41.4 | 32.5 | 26.8 | 26.1 | 33.3 | 43.4 |
| Following a special diet (%) | 5.6 | 7.6 | 10.0 | 4.6 | 7.4 | 12.0 | 12.3 | 7.2 | 3.2 |
| Alcohol intake (g/d) | 7.0 (11.2) | 6.5 (9.7) | 6.2 (8.3) | 5.5 (7.9) | 6.6 (9.9) | 7.7 (11.5) | 6.2 (8.8) | 6.6 (9.5) | 6.9 (11.9) |
| Adherence to Mediterranean diet, Trichopoulou (%) | |||||||||
| Low (0–3) | 56.9 | 35.2 | 17.1 | 66.8 | 34.2 | 7.7 | 20.1 | 38.4 | 52.9 |
| Medium (4–5) | 34.3 | 40.9 | 38.8 | 28.1 | 44.1 | 35.3 | 39.9 | 39.8 | 34.9 |
| High (6–9) | 8.9 | 24.0 | 44.1 | 5.1 | 21.6 | 57.0 | 40.1 | 21.9 | 12.2 |
| Supplement use (%) | 17.9 | 18.5 | 19.7 | 17.7 | 18.3 | 20.8 | 19.2 | 18.3 | 18.7 |
| Hypertension at baseline (%) | 8.4 | 9.7 | 10.4 | 6.7 | 9.8 | 12.2 | 12.1 | 9.2 | 7.4 |
| Hypercholesterolemia at baseline (%) | 12.5 | 16.3 | 21.0 | 11.4 | 16.3 | 22.4 | 19.6 | 16.1 | 12.9 |
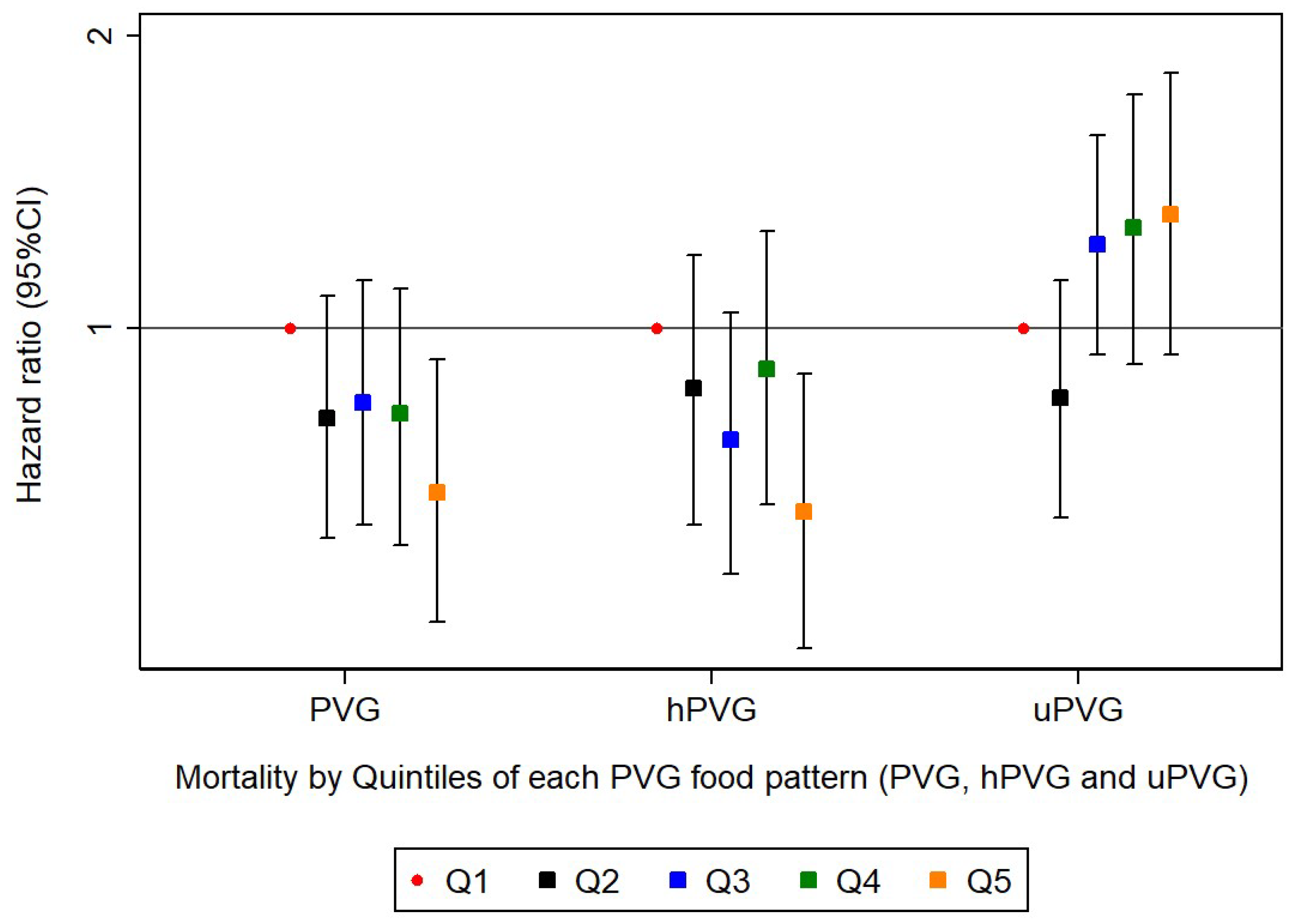
| PVG Food Pattern | Q1 | Q2 | Q3 | Q4 | Q5 | p for trend |
| n | 4278 | 3957 | 3365 | 2893 | 3496 | |
| Deaths/person-years | 105/57,223 | 103/52,188 | 95/43,815 | 76/37,463 | 81/44,176 | |
| Sex and age adjusted | 1.00 (ref.) | 0.85 (0.65–1.12) | 0.88 (0.67–1.16) | 0.84 (0.63–1.13) | 0.71 (0.53–0.95) | 0.030 |
| Model 1 | 1.00 (ref.) | 0.81 (0.61–1.07) | 0.84 (0.63–1.12) | 0.81 (0.60–1.10) | 0.69 (0.51–0.93) | 0.023 |
| Model 2 | 1.00 (ref.) | 0.81 (0.61–1.08) | 0.84 (0.63–1.12) | 0.82 (0.60–1.10) | 0.68 (0.50–0.93) | 0.020 |
| Repeated measurements of diet | 1.00 (ref.) | 0.79 (0.59–1.05) | 0.82 (0.61–1.09) | 0.79 (0.59–1.06) | 0.69 (0.51–0.93) | 0.034 |
| hPVG Food Pattern | Q1 | Q2 | Q3 | Q4 | Q5 | p for trend |
| n | 4090 | 3725 | 3889 | 3020 | 3265 | |
| Deaths/person-years | 72/54,737 | 92/48,522 | 98/51,384 | 96/38,828 | 102/41,394 | |
| Sex and age adjusted | 1.00 (ref.) | 0.97 (0.71–1.32) | 0.84 (0.62–1.14) | 0.95 (0.69–1.31) | 0.71 (0.52–0.98) | 0.030 |
| Model 1 | 1.00 (ref.) | 0.88 (0.64–1.20) | 0.78 (0.57–1.05) | 0.92 (0.67–1.26) | 0.67 (0.49–0.92) | 0.022 |
| Model 2 | 1.00 (ref.) | 0.87 (0.63–1.19) | 0.77 (0.56–1.04) | 0.91 (0.66–1.26) | 0.65 (0.47–0.90) | 0.016 |
| Repeated measurements of diet | 1.00 (ref.) | 0.78 (0.57–1.08) | 0.75 (0.54–1.02) | 0.86 (0.63–1.18) | 0.66 (0.48–0.91) | 0.059 |
| uPVG Food Pattern | Q1 | Q2 | Q3 | Q4 | Q5 | p for trend |
| n | 4130 | 3740 | 3779 | 3040 | 3300 | |
| Deaths/person-years | 138/52,033 | 86/48,611 | 103/49,829 | 69/40,134 | 64/44,259 | |
| Sex and age adjusted | 1.00 (ref.) | 0.82 (0.62–1.09) | 1.18 (0.91–1.52) | 1.17 (0.87–1.59) | 1.22 (0.90–1.67) | 0.068 |
| Model 1 | 1.00 (ref.) | 0.84 (0.64–1.12) | 1.23 (0.94–1.59) | 1.27 (0.93–1.74) | 1.29 (0.92–1.81) | 0.041 |
| Model 2 | 1.00 (ref.) | 0.85 (0.64–1.12) | 1.22 (0.94–1.58) | 1.27 (0.92–1.74) | 1.31 (0.94–1.83) | 0.037 |
| Repeated measurements of diet | 1.00 (ref.) | 1.06 (0.81–1.39) | 1.15 (0.88–1.50) | 1.37 (1.00–1.87) | 1.40 (1.00–1.97) | 0.019 |
| n | Deaths | PVG | hPVG | uPVG | |
|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |||
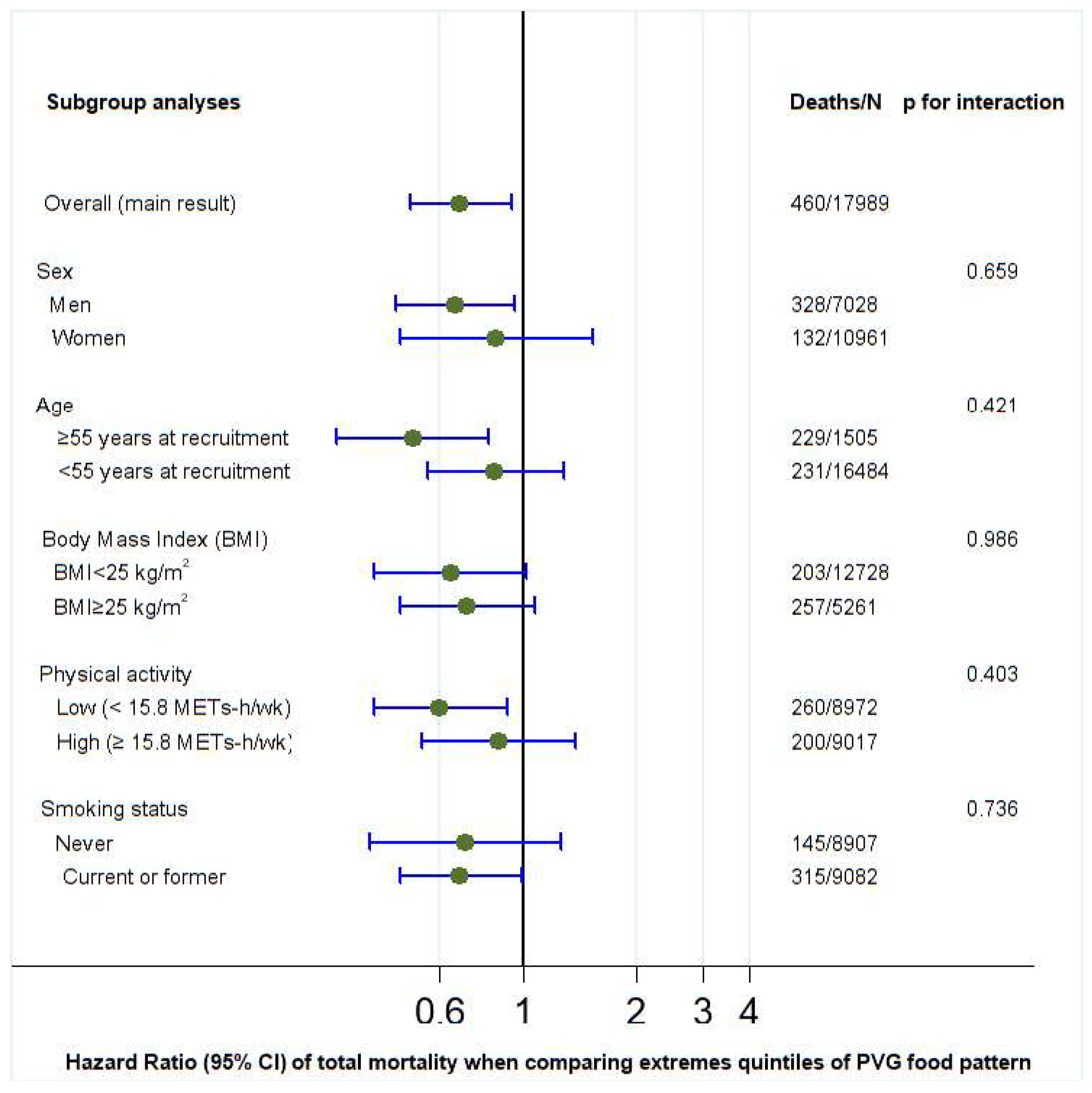
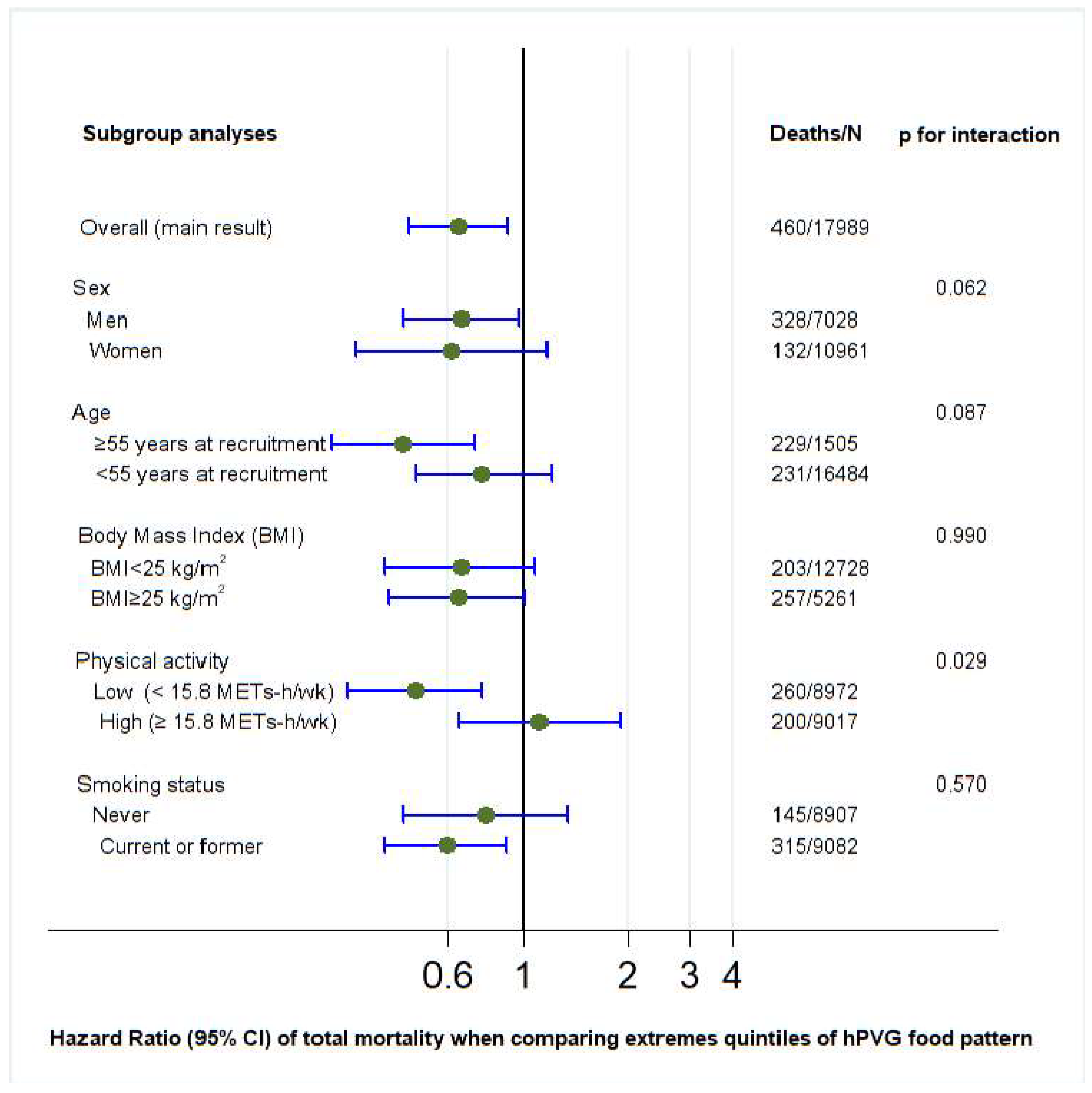
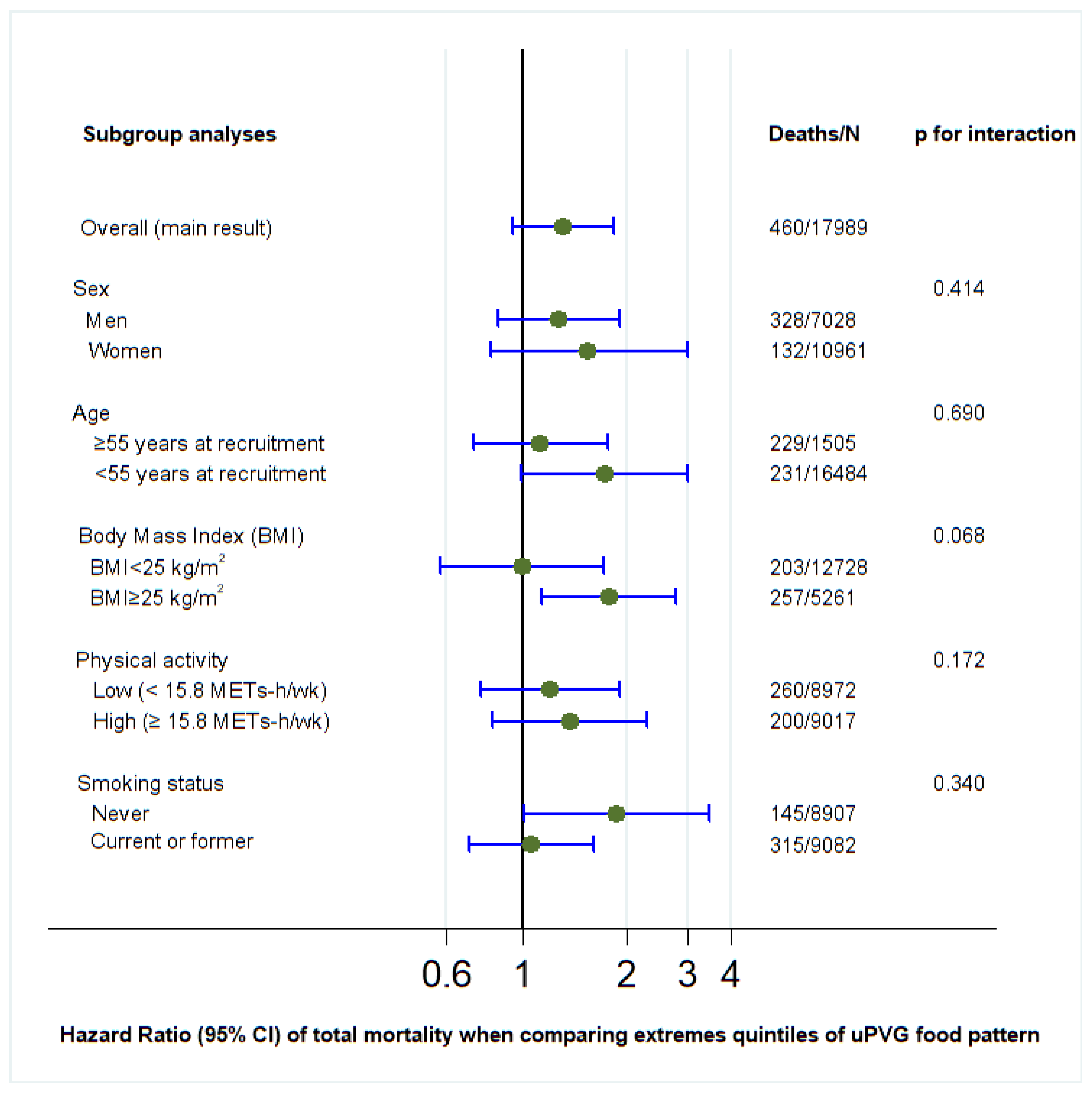
| Overall | 17,989 | 460 | 0.68 (0.50–0.93) | 0.65 (0.47–0.90) | 1.31 (0.94–1.83) |
| Energy limits: 5th–95th centiles | 17,973 | 443 | 0.69 (0.50–0.95) | 0.64 (0.47–0.89) | 1.35 (0.96–1.90) |
| Excluding deaths in two first years | 17,919 | 431 | 0.69 (0.51–0.95) | 0.66 (0.47–0.92) | 1.26 (0.89–1.79) |
| Excluding special diet | 16,620 | 406 | 0.73 (0.53–1.00) | 0.65 (0.46–0.92) | 1.30 (0.91–1.86) |
| Additionally adjusted for margarine | 17,989 | 460 | 0.68 (0.51–0.93) | 0.65 (0.47–0.90) | 1.31 (0.94–1.83) |
| Additionally adjusted for other vegetable fats and oils | 17,989 | 460 | 0.69 (0.51–0.93) | 0.66 (0.47–0.90) | 1.30 (0.93–1.83) |
| Additionally adjusted for prevalent depression | 17,989 | 460 | 0.69 (0.53–0.98) | 0.66 (0.48–0.91) | 1.30 (0.93–1.82) |
| Including only cancer deaths | 17,756 | 227 | 0.70 (0.45–1.08) | 0.66 (0.42–1.05) | 1.13 (0.69–1.83) |
| Including only CVD deaths | 17,615 | 86 | 0.55 (0.28–1.18) | 1.12 (0.42–2.96) | 1.30 (0.64–2.66) |
| Without excluding participants with chronic diseases * | 19,069 | 621 | 0.77 (0.59–1.00) | 0.72 (0.54–0.95) | 1.31 (0.98–1.76) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martinez-Tabar, A.; Ruiz-Canela, M.; Bullon-Vela, V.; Sayon-Orea, C.; Carlos, S.; Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Adherence to the Provegetarian Food Patterns and Incidence of All-Cause Mortality in a Mediterranean Population: The SUN Cohort. Nutrients 2025, 17, 2472. https://doi.org/10.3390/nu17152472
Martinez-Tabar A, Ruiz-Canela M, Bullon-Vela V, Sayon-Orea C, Carlos S, Martinez-Gonzalez MA, Bes-Rastrollo M. Adherence to the Provegetarian Food Patterns and Incidence of All-Cause Mortality in a Mediterranean Population: The SUN Cohort. Nutrients. 2025; 17(15):2472. https://doi.org/10.3390/nu17152472
Chicago/Turabian StyleMartinez-Tabar, Ainara, Miguel Ruiz-Canela, Vanessa Bullon-Vela, Carmen Sayon-Orea, Silvia Carlos, Miguel A. Martinez-Gonzalez, and Maira Bes-Rastrollo. 2025. "Adherence to the Provegetarian Food Patterns and Incidence of All-Cause Mortality in a Mediterranean Population: The SUN Cohort" Nutrients 17, no. 15: 2472. https://doi.org/10.3390/nu17152472
APA StyleMartinez-Tabar, A., Ruiz-Canela, M., Bullon-Vela, V., Sayon-Orea, C., Carlos, S., Martinez-Gonzalez, M. A., & Bes-Rastrollo, M. (2025). Adherence to the Provegetarian Food Patterns and Incidence of All-Cause Mortality in a Mediterranean Population: The SUN Cohort. Nutrients, 17(15), 2472. https://doi.org/10.3390/nu17152472







