Parental Knowledge and Preventive Strategies in Pediatric IgE-Mediated Food Allergy—Results from a Cross-Sectional Survey
Abstract
1. Introduction
2. Materials and Methods
3. Results
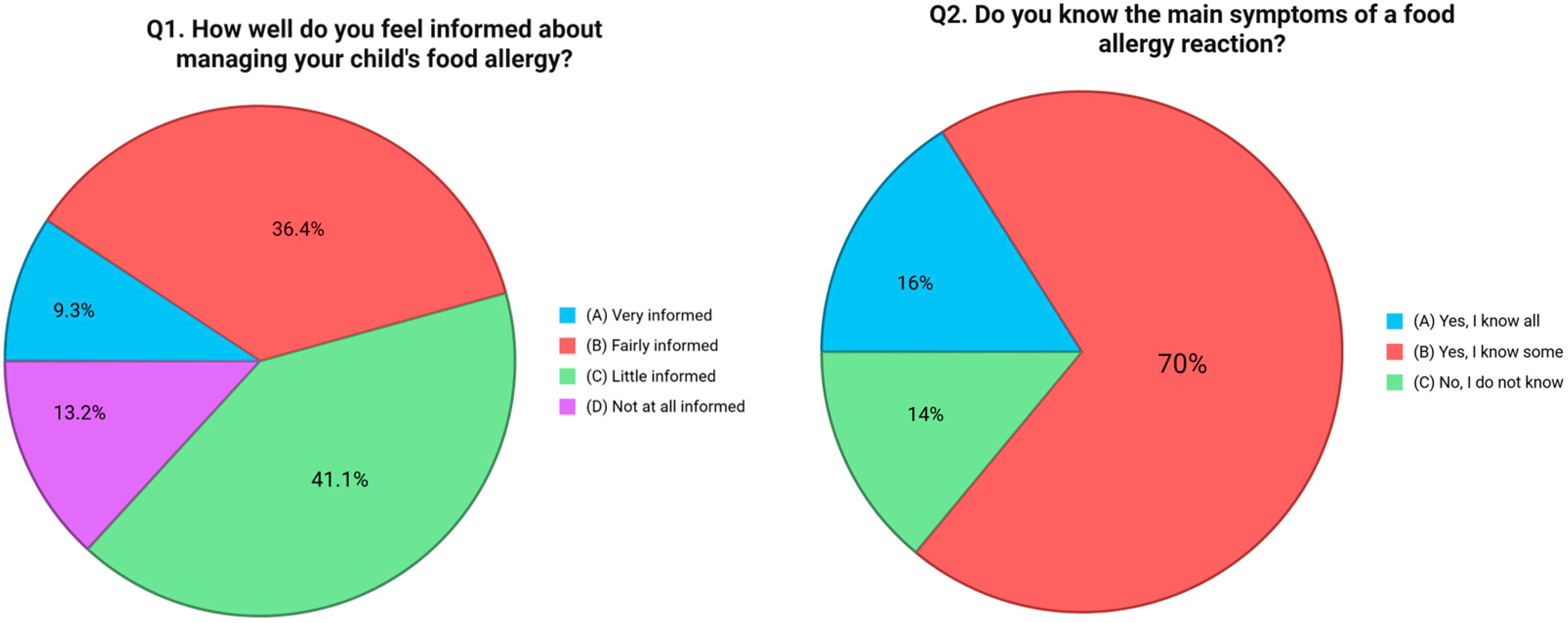
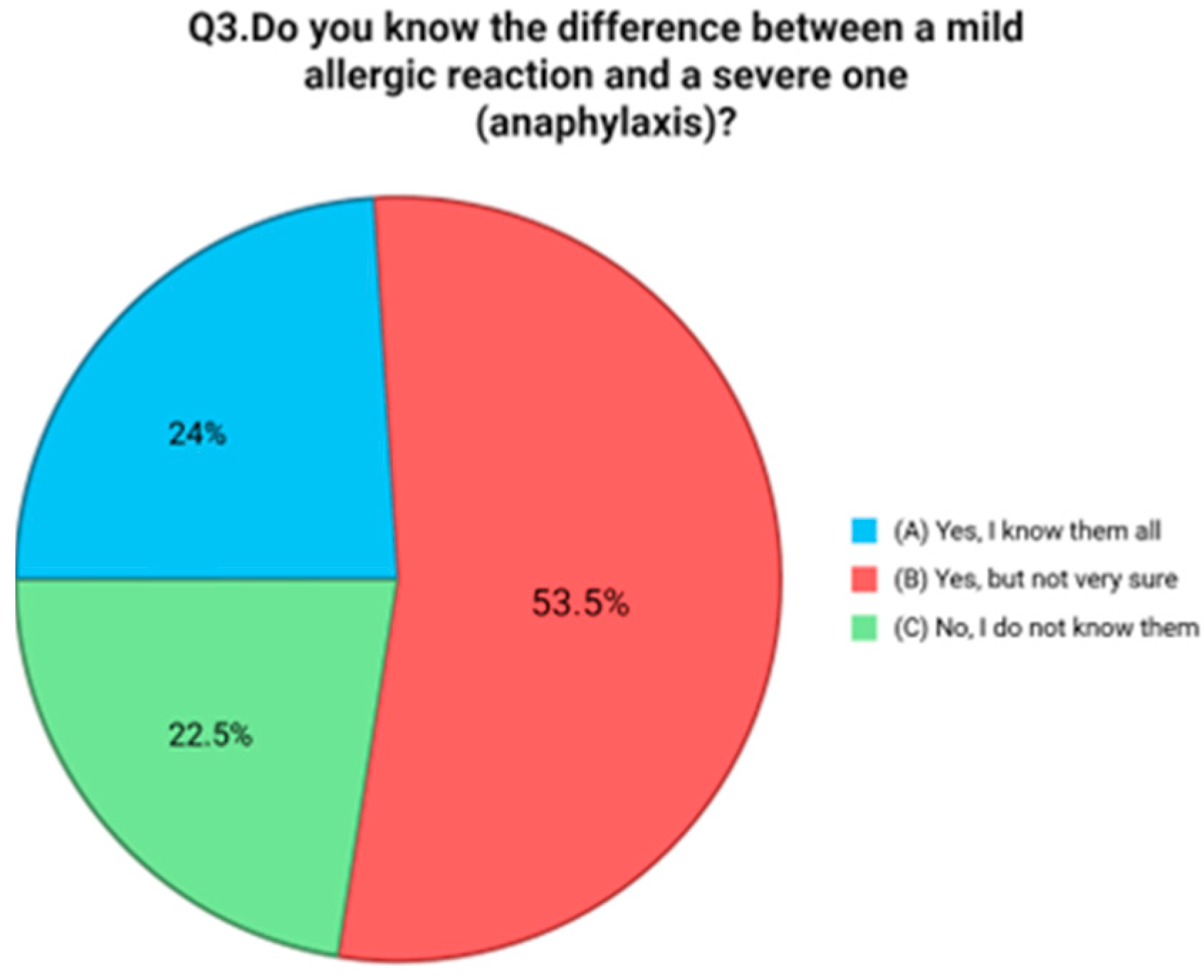
3.1. Caregiver Knowledge and Perceptions
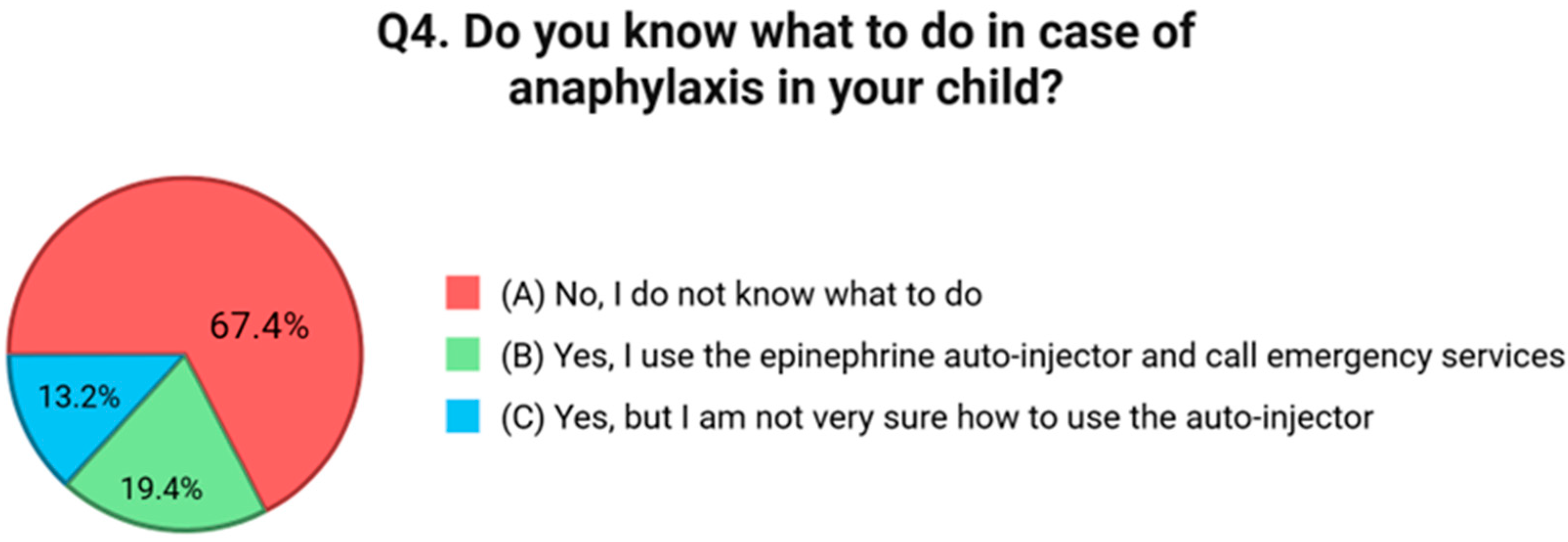
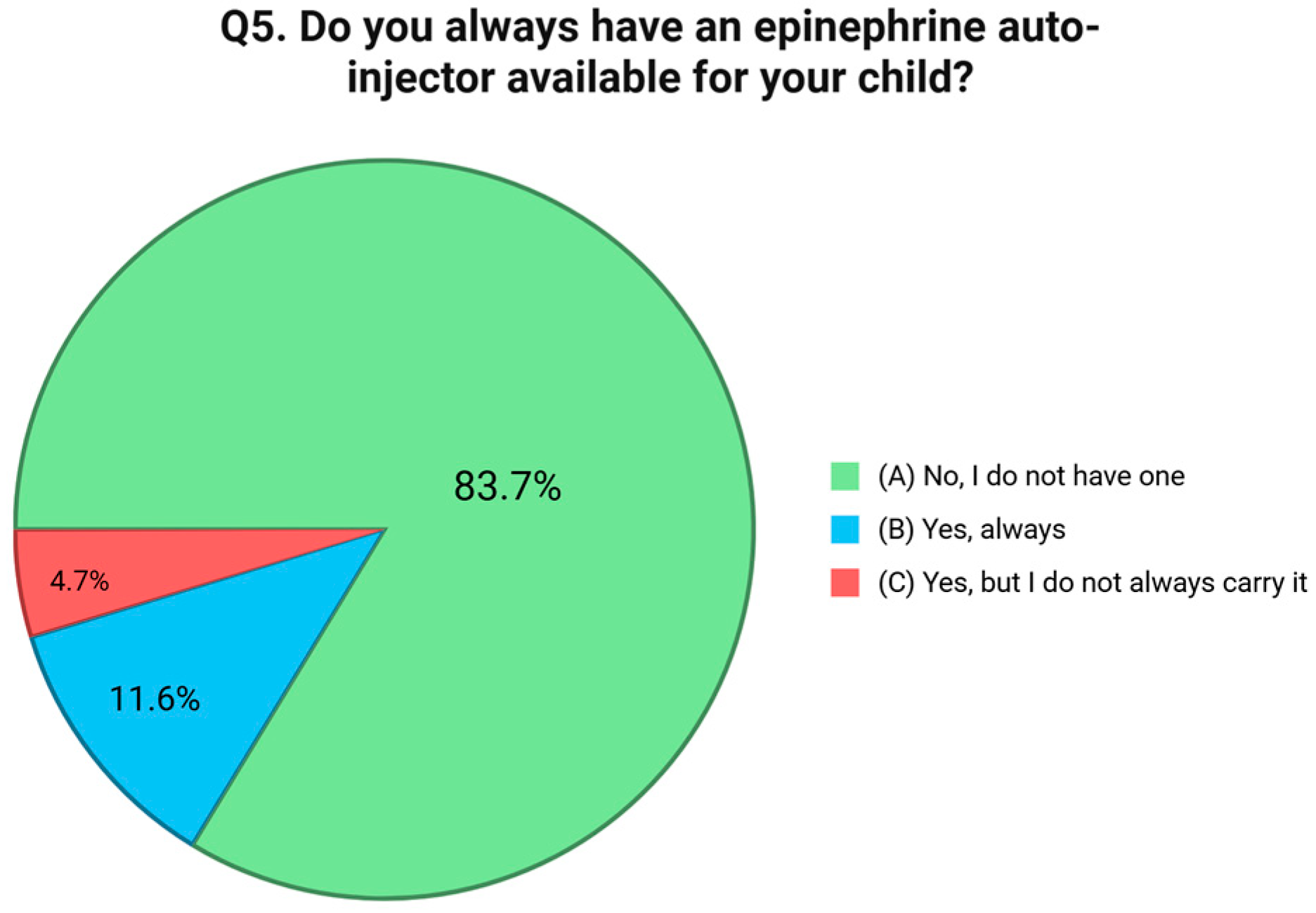
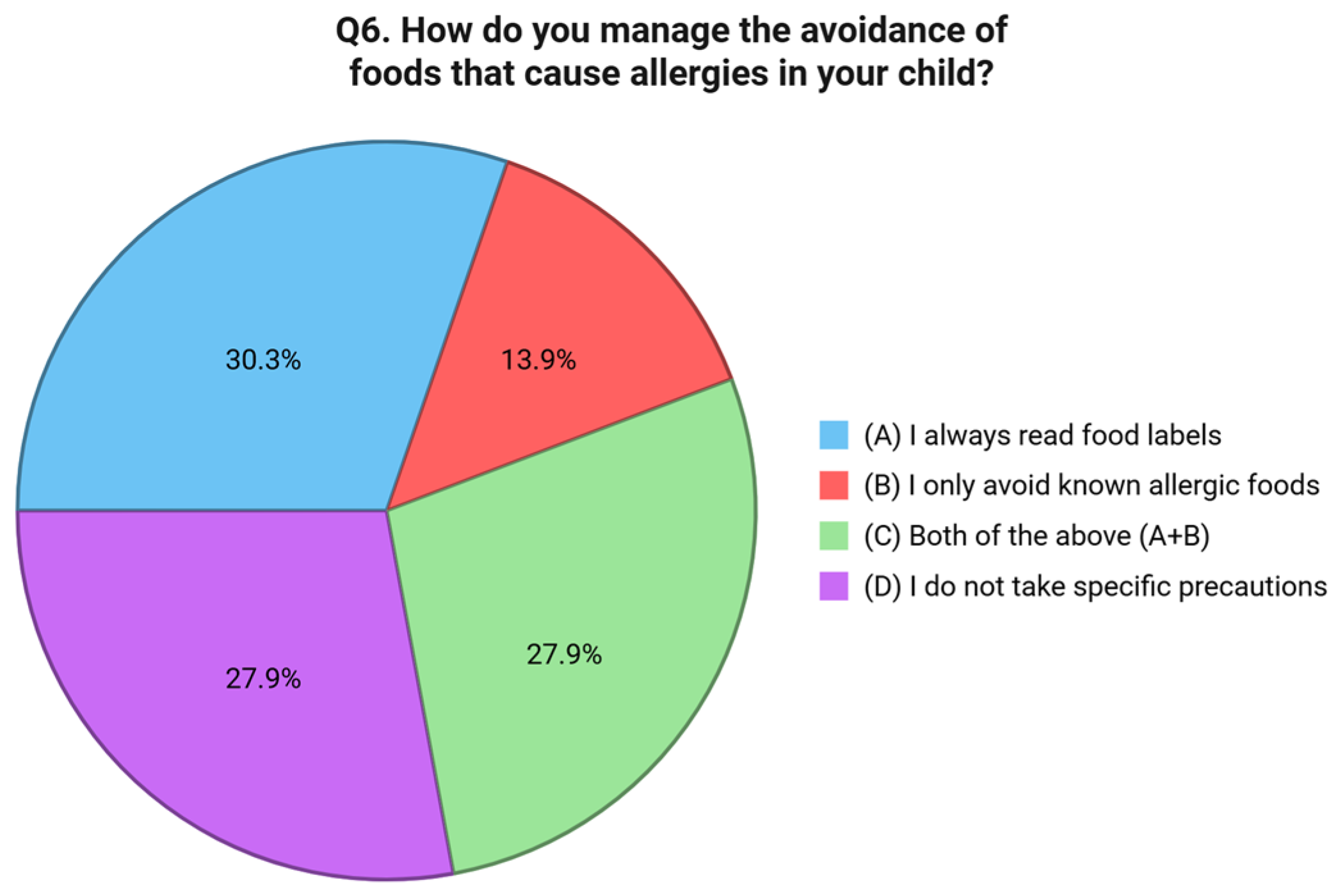
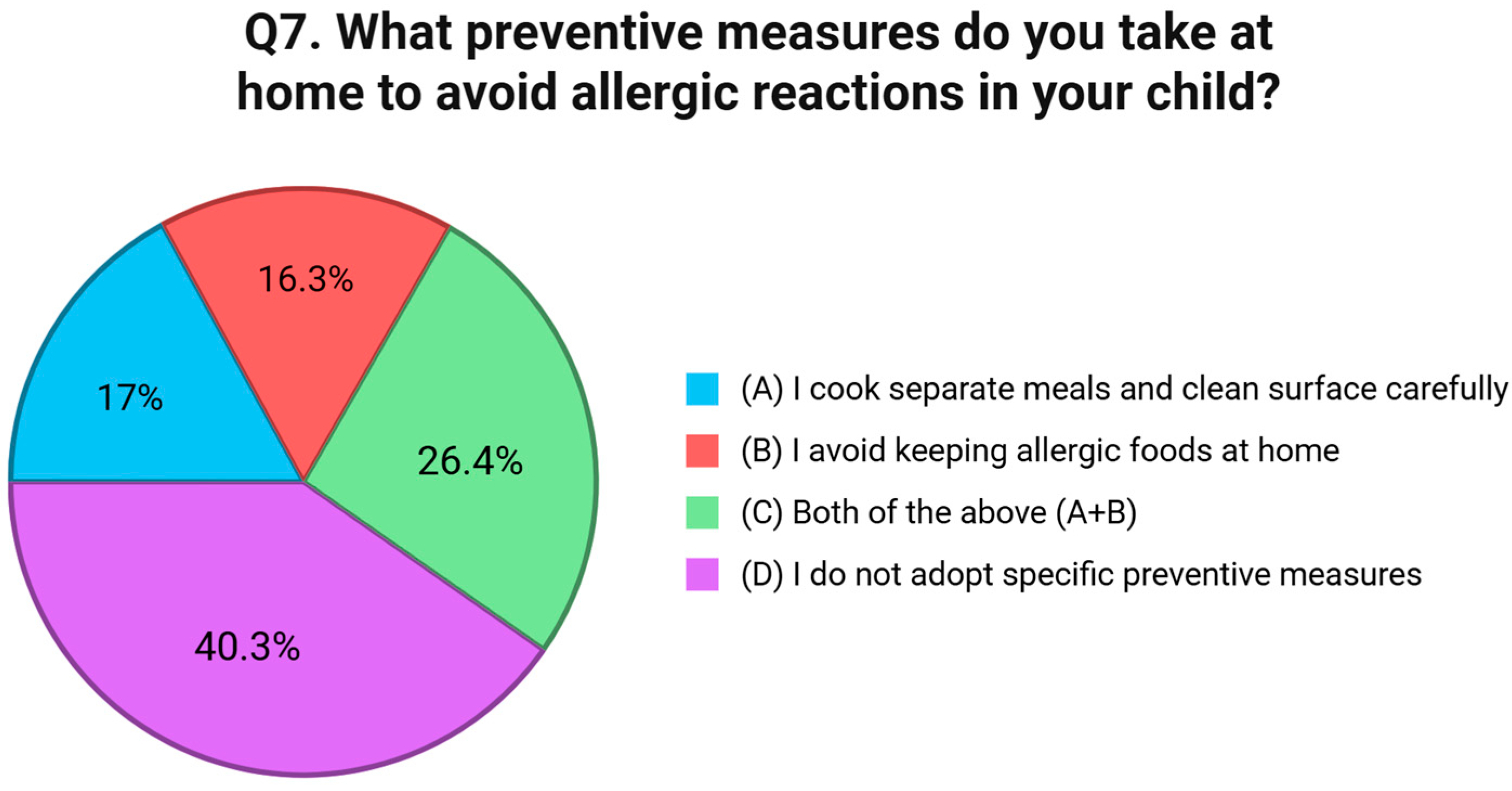
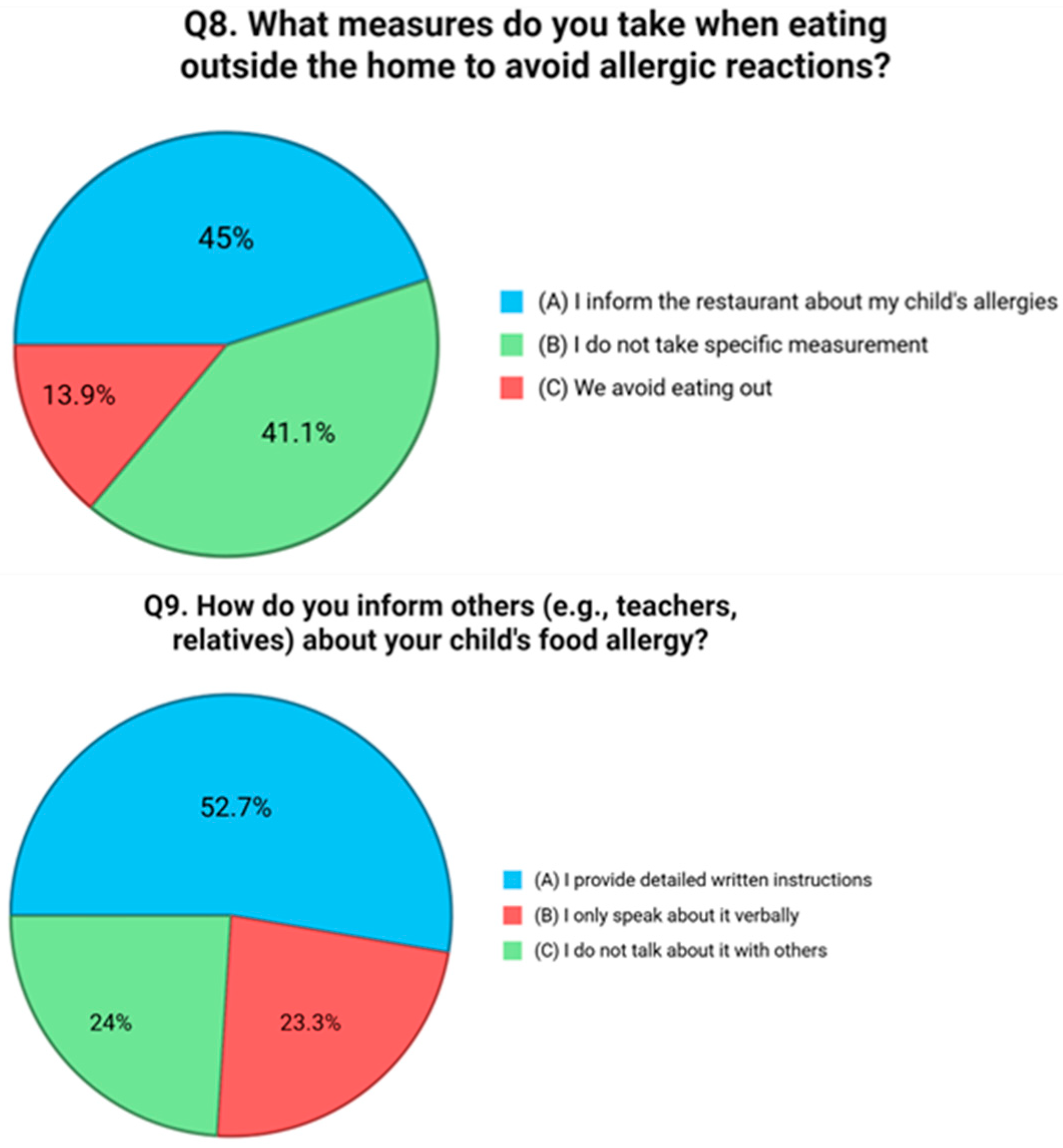
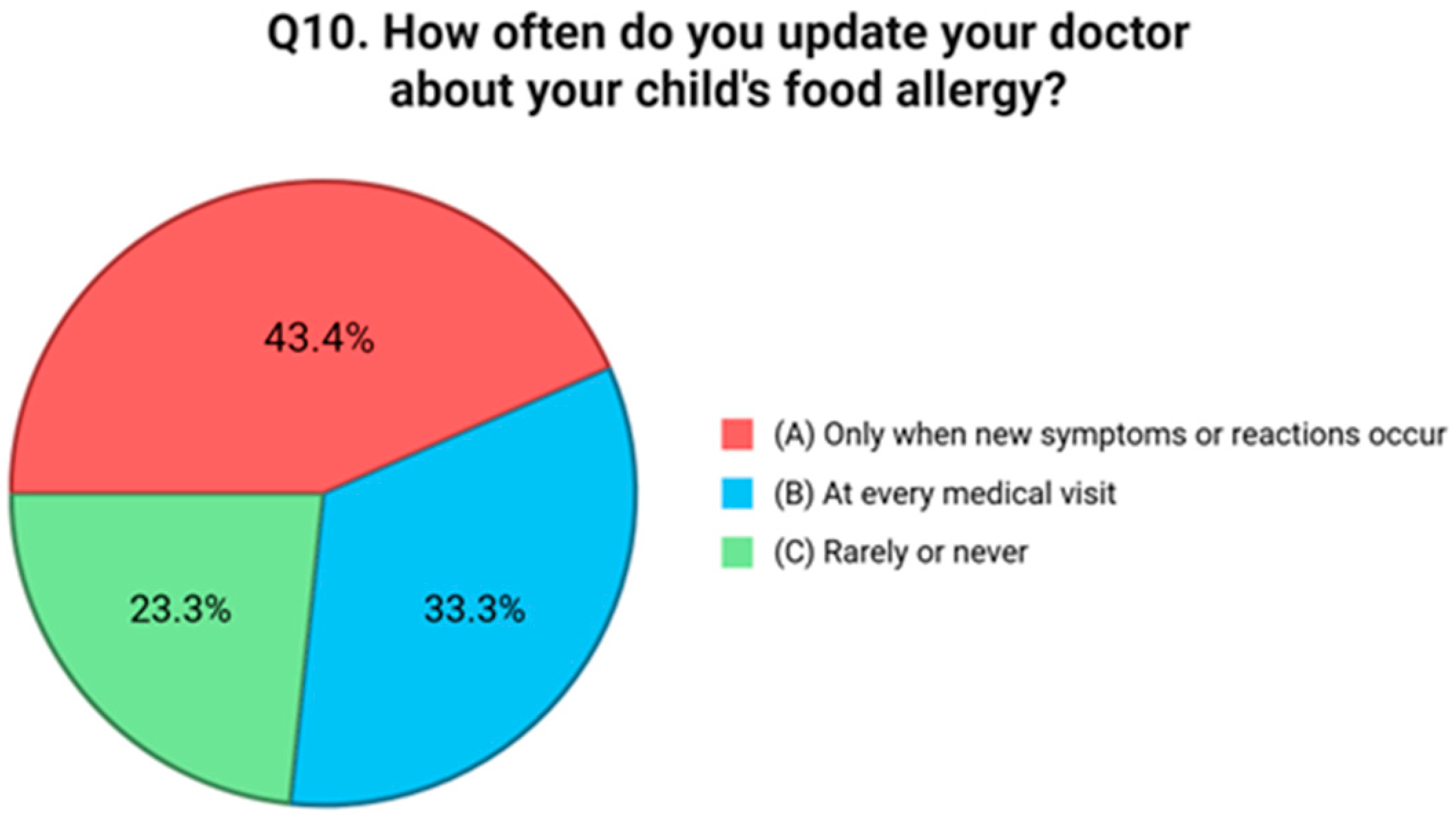
3.2. Behavioral Practices and Risk Management
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FA | Food Allergy |
| OIT | Oral Immunotherapy |
| IgE | Immunoglobulin E |
| FDA | Food and Drug Administration |
| EAACI | European Academy of Allergy and clinical Immunology |
| SIAIP | Italian Society of Allergy and Immunology |
| PTSD | Post Traumatic Stress Disorder |
References
- Sampath, V.; Abrams, E.M.; Adlou, B.; Akdis, C.; Akdis, M.; Brough, H.A.; Chan, S.; Chatchatee, P.; Chinthrajah, R.S.; Cocco, R.R.; et al. Food allergy across the globe. J. Allergy Clin. Immunol. 2021, 148, 1347–1364. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.F.; Riggioni, C.; Du Toit, G.; Skypala, I. An algorithm for the diagnosis and management of IgE-mediated food allergy, 2024 update. Allergy 2025, 80, 629–632. [Google Scholar] [CrossRef] [PubMed]
- Nurmatov, U.B.; Lo Scalzo, L.; Galletta, F.; Krasnenkova, M.; Arasi, S.; Ansotegui, I.J.; Tagiyeva-Milne, N.; Fiocchi, A. Biologics in IgE-mediated food allergy: A systematic review and meta-analysis of interventional studies. World Allergy Organ. J. 2025, 18, 101069. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration. FDA Approves First Medication to Help Reduce Allergic Reactions to Multiple Foods After Accidental Exposure. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-medication-help-reduce-allergic-reactions-multiple-foods-after-accidental (accessed on 4 June 2025).
- Santos, M.J.L.; Merrill, K.A.; Gerdts, J.D.; Ben-Shoshan, M.; Protudjer, J.L.P. Food Allergy Education and Management in Schools: A Scoping Review on Current Practices and Gaps. Nutrients 2022, 14, 732. [Google Scholar] [CrossRef] [PubMed]
- Sugunasingha, N.; Jones, F.W.; Jones, C.J. Interventions for caregivers of children with food allergy: A systematic review. Pediatr. Allergy Immunol. 2020, 31, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Muraro, A.; Worm, M.; Alviani, C.; Cardona, V.; DunnGalvin, A.; Garvey, L.H.; Riggioni, C.; de Silva, D.; Angier, E.; Arasi, S.; et al. EAACI guidelines: Anaphylaxis (2021 update). Allergy 2022, 77, 357–377. [Google Scholar] [CrossRef] [PubMed]
- Taha, S.; Rabaiah, R.; Dweikat, A.; Abu-Ali, L.; Yaeesh, H.; Jbour, R.; Al-Jabi, S.W.; Zyoud, S.H. Parental knowledge and attitudes toward food allergies: A cross-sectional study on determinants and educational needs. BMC Public Health 2024, 24, 2668. [Google Scholar] [CrossRef] [PubMed]
- Polloni, L.; Baldi, I.; Amadi, M.; Tonazzo, V.; Bonaguro, R.; Lazzarotto, F.; Toniolo, A.; Gregori, D.; Muraro, A. Management of Children with Food-Induced Anaphylaxis: A Cross-Sectional Survey of Parental Knowledge, Attitude, and Practices. Front. Pediatr. 2022, 10, 886551. [Google Scholar] [CrossRef] [PubMed]
- Narchi, H.; Elghoudi, A.; Al Dhaheri, K. Barriers and challenges affecting parents’ use of adrenaline auto-injector in children with anaphylaxis. World J. Clin. Pediatr. 2022, 11, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Cronin, C.; Keohane, H.; O’Rourke, E.; O’Kelly, C.; Ramesh, Y.; Flores, L.; Gallagher, A.; Dumitrescu, A.; Velasco, R.; Trujillo, J. Assessing the Knowledge of Anaphylaxis Management and Adrenaline Auto-Injector Administration Among Parents of Children with Food Allergies: A Cross-Sectional Study. Allergies 2024, 4, 80–93. [Google Scholar] [CrossRef]
- Stockhammer, D.; Katelaris, C.H.; Simpson, M.D.; Vanniasinkam, T. Parent perceptions in managing children with food allergy: An Australian perspective. World Allergy Organ. J. 2020, 13, 100468. [Google Scholar] [CrossRef] [PubMed]
- Moen, Ø.L.; Opheim, E.; Trollvik, A. Parents’ Experiences Raising a Child with Food Allergy: A Qualitative Review. J. Pediatr. Nurs. 2019, 46, e52–e63. [Google Scholar] [CrossRef] [PubMed]
- Dinardo, G.; Fierro, V.; Del Giudice, M.M.; Urbani, S.; Fiocchi, A. Food-labeling issues for severe food-allergic consumers. Curr. Opin. Allergy Clin. Immunol. 2023, 23, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Fiocchi, A.; Risso, D.; DunnGalvin, A.; González Díaz, S.N.; Monaci, L.; Fierro, V.; Ansotegui, I.J. Food labeling issues for severe food allergic patients. World Allergy Organ. J. 2021, 14, 100598. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, S.; Théolier, J.; Gerdts, J.; Godefroy, S.B. Dining Out with Food Allergies: Two Decades of Evidence Calling for Enhanced Consumer Protection. Int. J. Hosp. Manag. 2024, 122, 103825. [Google Scholar] [CrossRef]
- Konstantinou, G.N.; Pampoukidou, O.; Sergelidis, D.; Fotoulaki, M. Managing Food Allergies in Dining Establishments: Challenges and Innovative Solutions. Nutrients 2025, 17, 1737. [Google Scholar] [CrossRef] [PubMed]
- Figueroa-Gómez, X.A.; Oliveras-López, M.J.; Poyanco-Bugueño, M.F.; Ocaña-Peinado, F.M.; López-García de la Serrana, H.; Araya Quezada, M. Knowledge, attitude, and practices of restaurant and foodservice personnel in food allergy: A systematic review and meta-analysis. Heliyon 2024, 10, e33431. [Google Scholar] [CrossRef] [PubMed]
- Ajibade, T.; Bukutu, C.; Marinkovic, A.; Okorie, C.; Izurieta, R.; Sanyaolu, A. A Systematic Review of the Knowledge and Training of Food Service Workers on Food Allergies. AIMS Allergy Immunol. 2023, 7, 195–212. [Google Scholar] [CrossRef]
- Berni Canani, R.; Caffarelli, C.; Calvani, M.; Martelli, A.; Carucci, L.; Cozzolino, T.; Alvisi, P.; Agostoni, C.; Lionetti, P.; Marseglia, G.L.; et al. Diagnostic therapeutic care pathway for pediatric food allergies and intolerances in Italy: A joint position paper by the Italian Society for Pediatric Gastroenterology Hepatology and Nutrition (SIGENP) and the Italian Society for Pediatric Allergy and Immunology (SIAIP). Ital. J. Pediatr. 2022, 48, 87. [Google Scholar] [CrossRef] [PubMed]
- Muraro, A.; Mendoza Hernandez, D.A. Managing food allergy and anaphylaxis: A new model for an integrated approach. Allergol. Int. 2020, 69, 19–27. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galletta, F.; Klain, A.; Manti, S.; Mori, F.; Grella, C.; Tomei, L.; Senatore, A.A.; Licari, A.; Miraglia del Giudice, M.; Indolfi, C. Parental Knowledge and Preventive Strategies in Pediatric IgE-Mediated Food Allergy—Results from a Cross-Sectional Survey. Nutrients 2025, 17, 2387. https://doi.org/10.3390/nu17152387
Galletta F, Klain A, Manti S, Mori F, Grella C, Tomei L, Senatore AA, Licari A, Miraglia del Giudice M, Indolfi C. Parental Knowledge and Preventive Strategies in Pediatric IgE-Mediated Food Allergy—Results from a Cross-Sectional Survey. Nutrients. 2025; 17(15):2387. https://doi.org/10.3390/nu17152387
Chicago/Turabian StyleGalletta, Francesca, Angela Klain, Sara Manti, Francesca Mori, Carolina Grella, Leonardo Tomei, Antonio Andrea Senatore, Amelia Licari, Michele Miraglia del Giudice, and Cristiana Indolfi. 2025. "Parental Knowledge and Preventive Strategies in Pediatric IgE-Mediated Food Allergy—Results from a Cross-Sectional Survey" Nutrients 17, no. 15: 2387. https://doi.org/10.3390/nu17152387
APA StyleGalletta, F., Klain, A., Manti, S., Mori, F., Grella, C., Tomei, L., Senatore, A. A., Licari, A., Miraglia del Giudice, M., & Indolfi, C. (2025). Parental Knowledge and Preventive Strategies in Pediatric IgE-Mediated Food Allergy—Results from a Cross-Sectional Survey. Nutrients, 17(15), 2387. https://doi.org/10.3390/nu17152387






