Abstract
The prevalence and socioeconomic impact of Metabolic dysfunction-associated steatotic liver disease (MASLD) is increasing. Despite the recent Food and Drug Administration (FDA) approval of Resmetirom as the first drug for patients with Metabolic dysfunction-associated steatohepatitis (MASH) and significant fibrosis, and several ongoing clinical trials, lifestyle changes aimed at achieving sustained weight loss remain a cornerstone in the management of these patients. In addition to regular and structured physical activity, diet is crucial. Several studies have demonstrated the benefits of the Mediterranean diet in this regard, and there is also emerging evidence on the vegetarian diet and its different patterns. This review aims to summarize the currently available evidence on the potential benefits of a vegetarian diet in patients with MASLD, as well as exploring its potential limitations.
1. Introduction
Metabolic dysfunction-associated steatotic liver disease (MASLD) is a significant global public health problem and is predicted to become the leading cause of liver transplantation in the coming decades [1]. It is strictly associated with obesity, type 2 diabetes (T2D), and dyslipidemia, and is characterized by hepatic fat accumulation in the presence of one or more cardiometabolic risk factors, in the absence of significant alcohol consumption or other secondary causes of liver steatosis [1,2,3]. In 2023, the term MASLD was introduced as part of an updated nomenclature with the aim of better defining this common liver disease, with a particular emphasis on metabolic dysfunction and the necessity of assessing individual metabolic syndrome components. This reclassification underscores the need for a multidisciplinary approach for MASLD management, involving hepatologists, endocrinologists, cardiologists, and nutrition specialists [4,5,6,7].
The pathophysiology of MASLD is closely linked to excess adiposity and insulin resistance, which drive hepatic fat accumulation, inflammation, and progressive liver damage. The MASLD spectrum includes simple steatosis (SLD) and metabolic dysfunction-associated steatohepatitis (MASH), the latter potentially progressing to advanced chronic liver disease (ACLD) and hepatocellular carcinoma (HCC) development [3,8,9].
In light of the global rise in metabolic syndrome, there is an expectation that the prevalence of MASLD will increase further, underscoring the need for early diagnosis, effective management strategies, and greater awareness [1,10]. The global prevalence of MASLD has risen from an estimated 25% in 2016 to over 30% today [11]. Notable regional variations have been observed, with higher prevalence rates recorded in Latin America and the Middle East compared to East Asia and Western Europe, where rates are estimated at around 25% [12].
The Food and Drug Administration’s approval of Resmetirom in 2024 is a notable advancement in the treatment of non-cirrhotic MASH. However, lifestyle modification remains the fundamental approach for managing this liver disease [7,13,14,15,16]. The primary strategy involves weight reduction through dietary modification and regular physical activity, with evidence indicating that a reduction in body weight of at least 5% is necessary to decrease liver fat, while a reduction of 7–10% is required to improve liver inflammation, and >10% to improve liver fibrosis [17].
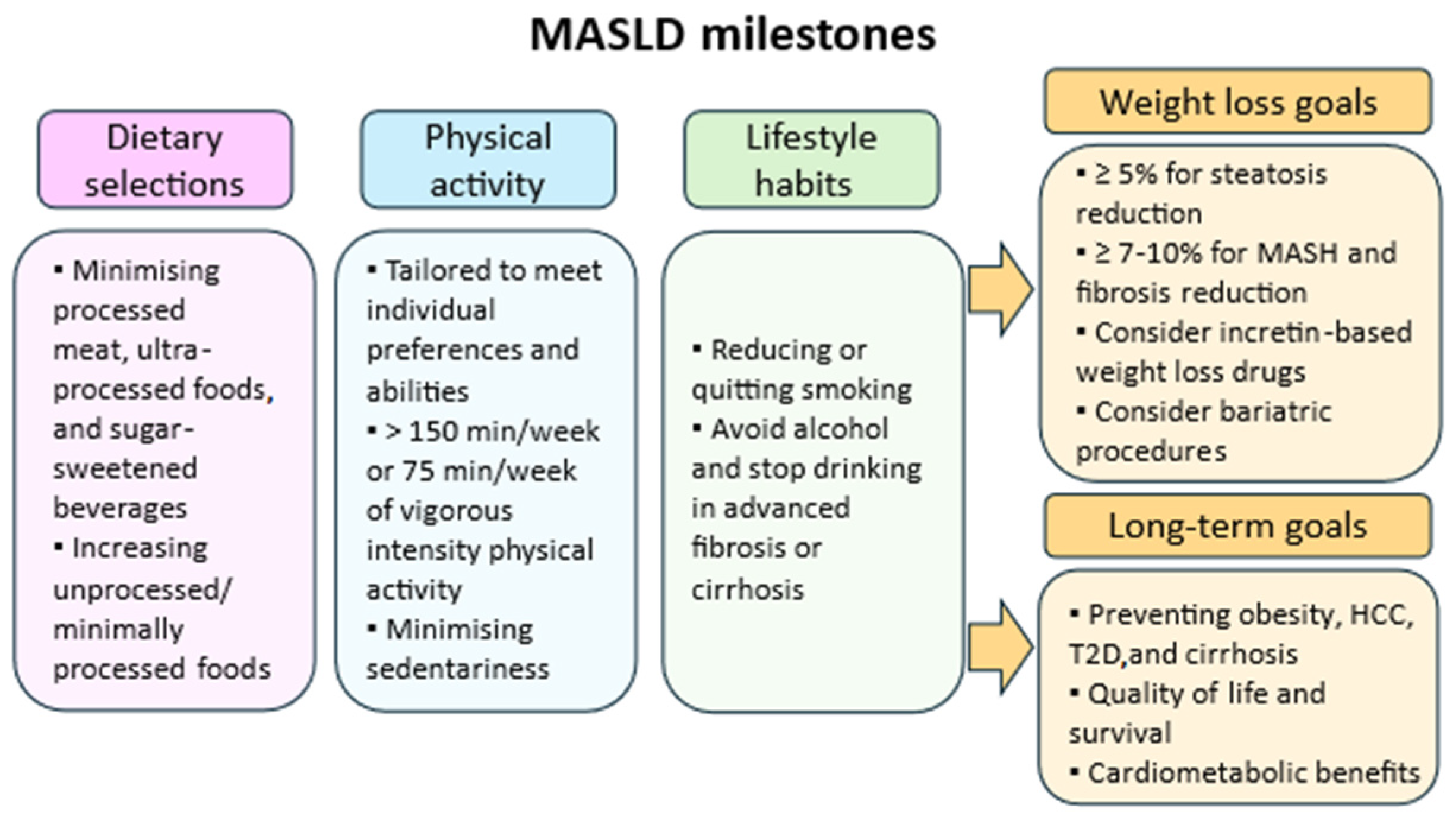
Several dietary patterns have been explored for the treatment of MASLD, with the Mediterranean diet being the most studied and recommended [18,19]. Other plant-based dietary approaches, including the Dietary Approaches to Stop Hypertension (DASH) diet and vegetarian diet, have also demonstrated potential benefits [7,18,20,21]. The vegetarian diet, in particular, has gained attention due its potential to reduce liver fat, decrease systemic inflammation, and improve insulin sensitivity. However, despite increasing interest, evidence of its impact on MASLD remains limited. Furthermore, for individuals who do not achieve significant weight loss with lifestyle changes alone, pharmacotherapy and bariatric procedures may be considered [1,7,22,23] (Figure 1).
Figure 1.
Key lifestyle milestones in MASLD management, including dietary choices, physical activity, and behavioral habits. Weight loss targets and long-term goals focus on reducing liver fat, improving fibrosis, and preventing metabolic and hepatic complications. Abbreviations: MASH (Metabolic dysfunction-associated steatohepatitis), HCC (Hepatocellular carcinoma), T2D (Type 2 diabetes).
The present narrative review aims to summarize the currently available evidence on vegetarian dietary patterns, including their various subtypes, and evaluate their potential impact on MASLD.
2. Search Strategy and Inclusion Criteria
A comprehensive search of the literature was conducted to identify relevant studies on vegetarian dietary patterns in the management of MASLD. The search included major databases—PubMed, Scopus, and Web of Science—and covered publications up to March 2025. The following keywords were used: “vegetarian diet” OR “plant-based diet” OR “vegan diet” AND “MASLD” OR “NAFLD” OR “nonalcoholic fatty liver disease” OR “metabolic dysfunction-associated steatotic liver disease”. Titles and abstracts were screened for relevance, and full texts of eligible articles were reviewed. Both observational and interventional studies were considered. Inclusion criteria required studies to report clinical, biochemical, or imaging-based liver outcomes in adult human populations following vegetarian or plant-based diets (PBDs).
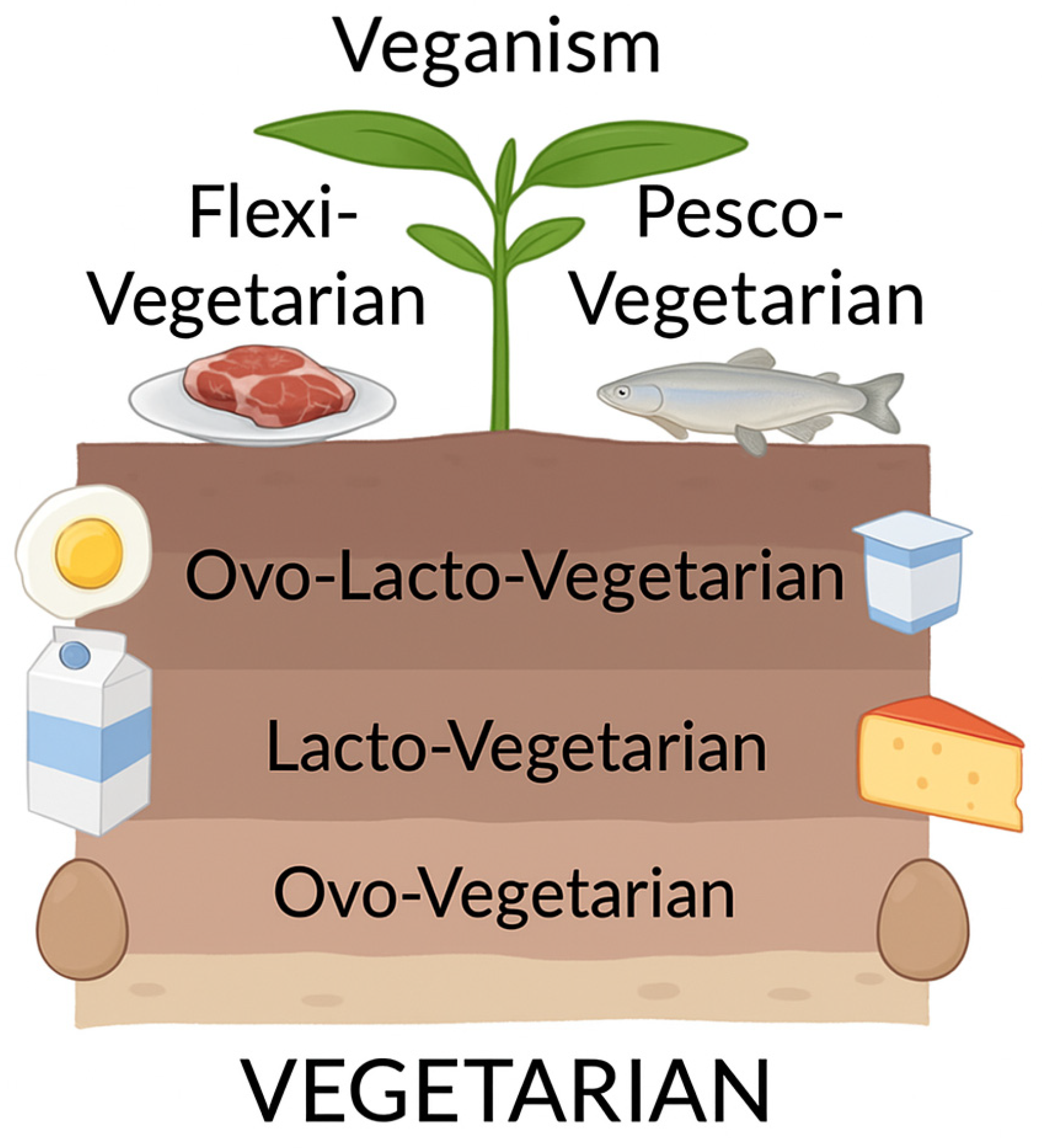
3. Vegetarian Diet: Definitions and Benefits
Vegetarianism is a broad term encompassing a variety of dietary patterns that differ in their degree of restriction. It is generally defined as the exclusion of meat from the diet [24,25,26]. At the least restrictive end of the spectrum is flexitarianism, which allows occasional consumption of meat, followed by pescetarianism, where only fish and seafood are allowed. The most common form, lacto-ovo vegetarianism, excludes meat but allows eggs and dairy products. Finally, veganism, also known as strict vegetarianism, involves the elimination of all animal-derived products [24] (Figure 2).
Figure 2.
Classification of vegetarian dietary patterns.
The distribution of vegetarians around the world is not uniform. While the prevalence of vegetarianism in Western countries ranges from 4.3 to 9%, the highest proportion is found in India, where around 30% of the population follow a vegetarian diet [27,28,29,30,31].
4. Overall Benefits of a Vegetarian Diet
The decision to adopt a vegetarian diet is motivated by a variety of factors, the most important of which are ethical concerns and health benefits. From a health perspective, there is growing evidence of the benefits of a vegetarian diet in reducing the risk of chronic diseases, including metabolic disorders. A meta-analysis of 32 cross-sectional studies, involving over 20,000 individuals, found that vegetarian diets were associated with lower mean blood pressure compared with omnivorous diets [32]. A further meta-analysis of 15 randomized controlled trials (RCTs) involving 856 subjects supported these findings, confirming that vegetarian diets significantly reduce systolic (SBP) and diastolic blood pressure (DBP), with vegan diets having a greater effect on SBP than lacto-ovo vegetarian diets [33]. However, a separate meta-analysis of nine RCTs, involving 677 individuals, failed to find a significant association between vegan diets and blood pressure reduction, highlighting the heterogeneity observed based on dietary subtypes and study populations [34].
Several studies have shown a link between vegetarian diets and weight loss, suggesting a potential role in the management of body composition. A meta-analysis by Barnard et al. reported that prescription of a PBD was associated with a mean weight loss of 3.4 kg in an intent-to-treat analysis and 4.6 kg in a comprehensive analysis [35]. A further analysis of vegan diets and T2D found that individuals following a vegan diet had a lower prevalence and incidence of T2D, as well as improved glycemic control and glucose homeostasis [36].
Notable cardiovascular benefits were also observed. Vegan diets are rich in soluble dietary fibers (SFs), which can reduce LDL cholesterol by 5–10% without affecting HDL cholesterol or triglyceride levels [37]. This is probably due to the high viscosity of SFs, which reduces absorption of cholesterol and bile acids, and increases their fecal excretion. Moreover, PBDs also contain phytosterols (PSs), which can help to reduce cholesterol absorption by 30–40% [37]. Findings from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Oxford also suggest a protective effect of a vegetarian diet against ischemic heart disease (IHD). After 18 years of observation, vegetarians had a 23% lower risk of IHD compared to meat-eaters, while vegans had an 18% lower risk [38]. When vegetarians and vegans were grouped together, the risk reduction was 22%, which remained significant at 17% after adjustment for BMI. The observed effects were probably due to lower LDL cholesterol levels and slightly lower SBP in the PBD groups. However, despite these cardiovascular benefits, vegetarians had a 17% higher risk of stroke, mainly due to a 48% increased risk of hemorrhagic stroke. Possible explanations include low LDL cholesterol levels and vitamin B12 deficiency, leading to elevated homocysteine levels [39].
With regards to cancer risk, a meta-analysis of seven studies involving 124,706 participants found that vegetarians had an 18% lower incidence of cancer compared with meat-eaters (relative risk [RR]: 0.82; 95% confidence interval [CI]: 0.67–0.97) [40]. A similar finding was reported in the EPIC-Oxford study, which examined a cohort of 65,000 subjects. This study found that the overall risk of cancer was 10% lower in vegetarians and 18% lower in vegans compared to meat-eaters [41].
5. Vegetarian Diet and MASLD
Vegetarian diets emphasize the consumption of fruits, vegetables, nuts, seeds, legumes, and whole grains, while minimizing animal products and processed foods [25,42]. However, several challenges need to be considered, including difficulties with adherence, the need for personalized dietary planning, and ensuring adequate nutrient intake to prevent deficiencies [43].
These diets are increasingly recognized for their potential role in the prevention and management of chronic diseases, including MASLD, where higher adherence to PBDs has been associated with a lower risk of liver steatosis, independent of genetic susceptibility [44,45].
Several studies have investigated the impact of vegetarian diets on MASLD prevalence and liver-related outcomes (Table 1).
A 2015 cross-sectional and retrospective study by Choi et al. compared 615 Buddhist monks who followed a vegetarian diet with a control group, but the results did not support a protective effect of vegetarianism against MASLD, as the prevalence was slightly higher in the vegetarian group (29.9% vs. 25.05%, p = 0.055) [46]. In contrast, a 2018 cross-sectional study by Chiu et al., which analyzed data from the Tzu Chi Health Study (2127 non-vegetarians and 1273 vegetarians), found that a vegetarian diet—characterized by replacing meat and fish with soy and refined carbohydrates with whole grains—was inversely associated with MASLD, BMI, and liver fibrosis severity [47]. Similarly, Mazidi et al. analyzed data from 18,345 US adults (NHANES 2005–2010) and found that adherence to a healthy PBD was associated with lower blood levels of liver enzymes (ALT, AST) and a reduced fatty liver index (FLI), while an unhealthy PBD showed the opposite trend. Participants in the highest tertile of PBD had a 21% lower odds of MASLD (OR: 0.79, 95% CI: 0.74–0.82), reinforcing the importance of PBD quality for liver health [48].
In addition to observational data, interventional studies further support the potential benefits of a vegetarian diet. A 16-week RCT, by Kahleova et al., in 244 overweight adults evaluated the effects of a low-fat vegan diet on body weight, insulin resistance, and liver fat. The intervention group showed a significant reduction in body weight (−5.9 kg, p < 0.001), increased postprandial metabolism (+14.1%, p < 0.001), and improved insulin sensitivity. There was also a 34.4% reduction in hepatocellular lipid levels (p = 0.002), and a 10.4% reduction in intramyocellular lipid content (p = 0.03) [49]. A 3-month RCT by Garousi et al. enrolled 75 overweight/obese patients with MASLD and randomized them to a lacto-ovo-vegetarian diet (LOV-D) or a standard weight-loss diet (SWL-D). Adherence to the LOV-D resulted in significant improvements in liver enzymes, anthropometric measures, glycemic markers, and lipid profiles. Moreover, the ultrasounds showed a greater reduction in liver steatosis in the LOV-D group compared to the SWL-D group [50].
The importance of diet quality was further highlighted in a longitudinal cohort study by Lv et al. that followed 159,222 participants over a median follow-up of 9.5 years. The study documented 1541 incident cases of MASLD and found that adherence to a healthy PBD was associated with a 26% lower risk of MASLD (HR 0.74, 95% CI 0.62–0.87, p-trend < 0.0001), independent of genetic predisposition. Conversely, an unhealthful PBD was associated with a 24% increased risk of MASLD (HR 1.24, 95% CI 1.05–1.46, p-trend = 0.02) [45]. Similarly, a Korean cohort study using data from the Health Examinees Study followed participants for a median of 4.2 years, during which a total of 1532 cases of MASLD were identified. The study concluded that individuals with the highest adherence to a healthy PBD had a significantly reduced risk of developing MASLD, with a risk reduction of 29% in men (HR 0.71, 95% CI 0.55–0.91, p = 0.0031) and 39% in women (HR 0.61, 95% CI 0.48–0.78, p < 0.0001), respectively [51].
These findings are further supported by a cross-sectional study by Li, X. et al. of 3900 US adults, which found that a healthy PBD was associated with 36% lower odds of MASLD (OR = 0.64, p-trend = 0.006). The study also found that an unhealthy PBD was associated with an increased risk of MASLD (OR = 1.37, p-trend = 0.009). The protective effect was strongest in non-Hispanic whites (p-interaction = 0.009) [52].
In addition, a pilot study by Chiarioni et al. investigated the effects of a personalized vegan diet in 32 MASLD patients with abnormal liver enzymes over a six-months period. The intervention resulted in a significant improvement in liver enzyme levels (p < 0.001 compared to baseline for AST, ALT, and GGT), despite modest weight changes. Loss of ≥5% of body weight was observed in 12 patients (46.1%), but this did not correlate with the normalization of liver function tests (p = 0.5), suggesting that the benefits of the vegan diet go beyond weight loss [53].
Finally, emerging evidence suggests that combining PBDs with specific dietary strategies may be useful in liver disease. A recent RCT by Shafiee et al. evaluated the combined effects of time-restricted feeding (TRF; 16/8) and LOV-D in MASLD. The intervention group showed significant reductions in body weight (−8.07 ± 4.31 kg), BMI (−2.70 ± 1.32 kg/m [2]), waist circumference (−8.00 ± 4.06 cm), ALT (−17.14 ± 14.33 U/L), GGT (−21.09 ± 24.06 U/L), FLI (−26.90 ± 15.81), insulin levels (−3.89 ± 4.69 mU/L), and TNF-α (−11.85 ± 12.52 pg/mL) (all p < 0.05). Improvements were also seen in the lipid profile, with lower triglycerides levels (−46.85 ± 54.55 mg/dL) and higher HDL-C (3.91 ± 5.07 mg/dL) [54].

Table 1.
Summary of studies on vegetarian and plant-based diets in MASLD.
Table 1.
Summary of studies on vegetarian and plant-based diets in MASLD.
| Author | Year | Aim | Main Findings | Study Design |
|---|---|---|---|---|
| Choi, S.H. et al. [46] | 2015 | To assess the association between vegetarianism and MASLD prevalence in a religious population. | Vegetarian diet was not protective against MASLD; slightly higher prevalence observed in vegetarians. | Cross-sectional, retrospective study of 615 Buddhist monks vs. controls. |
| Chiu, T.H. et al. [47] | 2018 | To investigate the association between vegetarian diet, liver fat, and fibrosis in healthy adults. | Vegetarian diet inversely associated with fatty liver and liver fibrosis, probably mediated by lower BMI and healthier food substitutions. | Cross-sectional study (Tzu Chi Health Study) of 3400 Taiwanese adults. |
| Mazidi, M. et al. [48] | 2018 | To evaluate associations between PBD types and MASLD/liver markers in US adults. | Inverse link between a healthy PBD and likelihood of MASLD with better liver function tests; an unhealthy PBD had the opposite effect. | Observational study (NHANES 2005–2010) of 18,345 participants. |
| Kahleova, H. et al. [49] | 2020 | To test effects of a low-fat vegan diet on liver and metabolic outcomes in overweight adults. | Vegan diet reduced body weight and liver fat, improved insulin sensitivity and postprandial metabolism. | 16-week RCT with 244 participants randomized to a low-fat vegan diet or control group. |
| Chiarioni, G. et al. [53] | 2021 | To investigate the effects of a personalized vegan diet in MASLD patients with elevated liver enzymes. | Improved liver enzymes despite modest weight loss; normalization not directly related to weight change. | 6-month prospective pilot study in 32 MASLD patients. |
| Li, X. et al. [52] | 2022 | To investigate the association between PBD and MASLD using transient elastography. | hPBD inversely associated with MASLD odds (OR 0.64); uPBD positively associated. Protective effect strongest in non-Hispanic whites. | Cross-sectional study (NHANES 2017–2018), 3900 US adults. |
| Garousi, N. et al. [50] | 2023 | To compare a LOV diet with a standard weight-loss diet in overweight/obese MASLD patients. | 3-month LOV-D improved liver steatosis, anthropometrics, glycemia, and lipid profiles more than standard diet. | Randomized controlled trial, 75 MASLD patients. |
| Lv, Y. et al. [45] | 2023 | To investigate long-term effects of PBD quality on MASLD risk in relation to genetics. | hPBD linked to 26% lower MASLD risk; uPBD associated with increased risk. Effects independent of genetic predisposition. | Longitudinal cohort (UK Biobank), 159,222 participants, 9.5 years of follow-up. |
| Ulzii, B.N. et al. [51] | 2024 | To evaluate the association between PBD types and MASLD risk in Korean adults. | Higher adherence to hPBD reduced MASLD risk (HR 0.71 in men; 0.61 in women); uPBD associated with increased risk. | Prospective cohort study (Health Examinees Study), 1532 cases, 4.2 years. |
| Shafiee, M. et al. [54] | 2025 | To assess impact of TRF combined with LOV-D on MASLD outcomes. | TRF + LOV-D improved weight, liver enzymes, insulin, lipid profile and inflammatory markers, suggesting a viable MASLD management approach. | 12-week RCT in 46 MASLD patients. |
Abbreviations: MASLD, metabolic dysfunction-associated steatotic liver disease; PBD, plant-based diet index; hPBD, healthful PBD; uPBD, unhealthful PBD; LOV-D, lacto-ovo-vegetarian diet; TRF, time-restricted feeding; RCT, randomized controlled trial.
6. Practical Considerations for a Vegetarian Diet in MASLD Management
International guidelines recommend lifestyle modification as the primary strategy for managing MASLD [7,55,56]. The Mediterranean diet, an extensively studied dietary pattern, remains the most recommended [7,55,56]. An alternative dietary strategy for the management of MASLD is the vegetarian diet, which offers metabolic benefits due to its high fiber, antioxidant, and polyunsaturated fatty acid (PUFA) content [24]. In addition, the reduced calorie density of vegetarian diets is beneficial in the context of weight management, an important component of MASLD management [57,58].
Despite these potential benefits, the use of PBDs should be approached with caution, particularly in individuals with insulin resistance, as high intakes of carbohydrates from certain plant sources may lead to the accumulation of liver fat. In addition, the use of dietary planning and supplementation to address nutrient deficiencies, particularly vitamin B12, n-3 PUFAs, and iron, is recommended. It is noteworthy that studies have found B12 deficiency in up to 50% of vegans, highlighting the importance of fortified meals and regular monitoring to prevent adverse effects [59]. An altered n-6/n-3 ratio has been observed in patients with MASLD, suggesting that optimizing n-3 PUFA intake through diet or supplementation may further improve liver health [7].
From a practical standpoint, the provision of tailored dietary advice and organized patient education is essential for ensuring long-term adherence to a vegetarian diet. To ensure a balanced macronutrient profile and to avoid excessive reliance on refined carbohydrates, it is recommended that MASLD patients be supported by healthcare professionals, such as dietitians and nutritionists, in selecting nutrient-dense plant-based diets.
7. Conclusions
Pending the availability of Resmetirom in Europe for patients with non-cirrhotic MASH and the results of ongoing phase 3 trials, dietary interventions remain the first line of therapy for the management of patients with MASLD, particularly with the goal of achieving significant weight loss, as this can define an improvement in liver histology [7,13]. Although no firm conclusions can be drawn on the relative merits of vegetarian versus Mediterranean diets in terms of outcomes in patients with MASLD, it is clear that these dietary patterns have distinct advantages in the management of obesity, metabolic dysfunction, and cardiovascular risk factors. The development of personalized dietary recommendations that integrate genetic predisposition and biomarker-based approaches is a key area for future research with the aim of optimizing PBD interventions for patients with MASLD. Artificial intelligence is also emerging as a potentially useful tool for patients with MASLD. In particular, AI-based chatbots could be used as a tool that patients can turn to at any time to ask questions about their dietary regimen, potentially improving adherence and the likelihood of achieving treatment goals [60,61]. The integration of traditional and innovative resources and the holistic approach to the patient with MASLD are certainly cornerstones in the management of this increasingly prevalent disease.
Author Contributions
Conceptualization, N.P. and A.A.; investigation, N.P., D.D.D. and M.S.; resources, D.D.D. and M.S.; writing—original draft preparation, N.P., D.D.D. and M.S.; writing—review and editing, F.C. and R.V.; supervision, A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors who have taken part in this study declare they do not have anything to disclose regarding funding or conflicts of interest with respect to this manuscript.
References
- Huang, D.Q.; Wong, V.W.S.; Rinella, M.E.; Boursier, J.; Lazarus, J.V.; Yki-Järvinen, H.; Loomba, R. Metabolic dysfunction-associated steatotic liver disease in adults. Nat. Rev. Dis. Primers 2025, 11, 14. [Google Scholar] [CrossRef] [PubMed]
- Targher, G.; Byrne, C.D.; Tilg, H. MASLD: A systemic metabolic disorder with cardiovascular and malignant complications. Gut 2024, 73, 691–702. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. NAFLD Nomenclature consensus group A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 2023, 79, 1542–1556. [Google Scholar] [CrossRef]
- Hsu, C.L.; Loomba, R. From NAFLD to MASLD: Implications of the new nomenclature for preclinical and clinical research. Nat. Metab. 2024, 6, 600–602. [Google Scholar] [CrossRef]
- Loomba, R.; Wong, V.W. Implications of the new nomenclature of steatotic liver disease and definition of metabolic dysfunction-associated steatotic liver disease. Aliment. Pharmacol. Ther. 2024, 59, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.M.; Younossi, Z.M.; Diehl, A.M.; Charlton, M.R.; Lazarus, J.V. Envisioning how to advance the MASH field. Nat. Rev. Gastroenterol. Hepatol. 2024, 21, 726–738. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD). J. Hepatol. 2024, 81, 492–542. [Google Scholar] [CrossRef]
- Pugliese, N.; Alfarone, L.; Arcari, I.; Giugliano, S.; Parigi, T.L.; Rescigno, M.; Lleo, A.; Aghemo, A. Clinical features and management issues of NAFLD-related HCC: What we know so far. Expert Rev. Gastroenterol. Hepatol. 2023, 17, 31–43. [Google Scholar] [CrossRef]
- Leyh, C.; Coombes, J.D.; Schmidt, H.H.; Canbay, A.; Manka, P.P.; Best, J. MASLD-Related HCC-Update on Pathogenesis and Current Treatment Options. J. Pers. Med. 2024, 14, 370. [Google Scholar] [CrossRef]
- Kopka, C.J.; Pugliese, N.; Brennan, P.N.; Lazarus, J.V. We must address the MASLD awareness gap, improve educational quality and prepare for the digitally quantified self. Liver Int. Off. J. Int. Assoc. Study Liver 2024, 44, 2099–2101. [Google Scholar] [CrossRef]
- Quek, J.; Chan, K.E.; Wong, Z.Y.; Tan, C.; Tan, B.; Lim, W.H.; Tan, D.J.H.; Tang, A.S.P.; Tay, P.; Xiao, J.; et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2023, 8, 20–30. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Golabi, P.; Paik, J.M.; Henry, A.; Van Dongen, C.; Henry, L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): A systematic review. Hepatology 2023, 77, 1335–1347. [Google Scholar] [CrossRef] [PubMed]
- Keam, S.J. Resmetirom: First Approval. Drugs 2024, 84, 729–735. [Google Scholar] [CrossRef]
- Harrison, S.A.; Bedossa, P.; Guy, C.D.; Schattenberg, J.M.; Loomba, R.; Taub, R.; Labriola, D.; Moussa, S.E.; Neff, G.W.; Rinella, M.E.; et al. A Phase 3, Randomized, Controlled Trial of Resmetirom in NASH with Liver Fibrosis. N. Engl. J. Med. 2024, 390, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Petta, S.; Targher, G.; Romeo, S.; Pajvani, U.B.; Zheng, M.H.; Aghemo, A.; Valenti, L.V.C. The first MASH drug therapy on the horizon: Current perspectives of resmetirom. Liver Int. Off. J. Int. Assoc. Study Liver 2024, 44, 1526–1536. [Google Scholar] [CrossRef]
- Noureddin, M.; Charlton, M.R.; Harrison, S.A.; Bansal, M.B.; Alkhouri, N.; Loomba, R.; Sanyal, A.J.; Rinella, M.E. Expert Panel Recommendations: Practical Clinical Applications for Initiating and Monitoring Resmetirom in Patients With MASH/NASH and Moderate to Noncirrhotic Advanced Fibrosis. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2024, 22, 2367–2377. [Google Scholar] [CrossRef] [PubMed]
- Vilar-Gomez, E.; Martinez-Perez, Y.; Calzadilla-Bertot, L.; Torres-Gonzalez, A.; Gra-Oramas, B.; Gonzalez-Fabian, L.; Friedman, S.L.; Diago, M.; Romero-Gomez, M. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology 2015, 149, 367–378.e5. [Google Scholar] [CrossRef]
- Pugliese, N.; Plaz Torres, M.C.; Petta, S.; Valenti, L.; Giannini, E.G.; Aghemo, A. Is there an ‘ideal’ diet for patients with NAFLD? Eur. J. Clin. Investig. 2022, 52, e13659. [Google Scholar] [CrossRef]
- Zelber-Sagi, S.; Grinshpan, L.S.; Ivancovsky-Wajcman, D.; Goldenshluger, A.; Gepner, Y. One size does not fit all; practical, personal tailoring of the diet to NAFLD patients. Liver Int. Off. J. Int. Assoc. Study Liver 2022, 42, 1731–1750. [Google Scholar] [CrossRef]
- Katsiki, N.; Stoian, A.P.; Rizzo, M. Dietary patterns in non-alcoholic fatty liver disease (NAFLD): Stay on the straight and narrow path! Clin. E Investig. En Arterioscler. Publ. Of. De La Soc. Esp. De Arterioscler. 2022, 34 (Suppl. S1), S24–S31. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Zelber-Sagi, S.; Henry, L.; Gerber, L.H. Lifestyle interventions in nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 2023, 20, 708–722. [Google Scholar] [CrossRef] [PubMed]
- Ciardullo, S.; Muraca, E.; Vergani, M.; Invernizzi, P.; Perseghin, G. Advancements in pharmacological treatment of NAFLD/MASLD: A focus on metabolic and liver-targeted interventions. Gastroenterol. Rep. 2024, 12, goae029. [Google Scholar] [CrossRef] [PubMed]
- Huttasch, M.; Roden, M.; Kahl, S. Obesity and MASLD: Is weight loss the (only) key to treat metabolic liver disease? Metab. Clin. Exp. 2024, 157, 155937. [Google Scholar] [CrossRef]
- Clarys, P.; Deliens, T.; Huybrechts, I.; Deriemaeker, P.; Vanaelst, B.; De Keyzer, W.; Hebbelinck, M.; Mullie, P. Comparison of nutritional quality of the vegan, vegetarian, semi-vegetarian, pesco-vegetarian and omnivorous diet. Nutrients 2014, 6, 1318–1332. [Google Scholar] [CrossRef] [PubMed]
- Hargreaves, S.M.; Rosenfeld, D.L.; Moreira, A.V.B.; Zandonadi, R.P. Plant-based and vegetarian diets: An overview and definition of these dietary patterns. Eur. J. Nutr. 2023, 62, 1109–1121. [Google Scholar] [CrossRef]
- Kent, G.; Kehoe, L.; Flynn, A.; Walton, J. Plant-based diets: A review of the definitions and nutritional role in the adult diet. Proc. Nutr. Soc. 2022, 81, 62–74. [Google Scholar] [CrossRef]
- Mensink, G.B.M.; Barbosa, C.L.; Brettschneider, A.K. Prevalence of persons following a vegetarian diet in Germany. J. Health Monit. 2016, 1, 2–14. [Google Scholar] [CrossRef]
- Le, L.T.; Sabaté, J. Beyond meatless, the health effects of vegan diets: Findings from the Adventist cohorts. Nutrients 2014, 6, 2131–2147. [Google Scholar] [CrossRef]
- Ruby, M.B.; Heine, S.J.; Kamble, S.; Cheng, T.K.; Waddar, M. Compassion and contamination. Cultural differences in vegetarianism. Appetite 2013, 71, 340–348. [Google Scholar] [CrossRef]
- Pfeiler, T.M.; Egloff, B. Examining the “Veggie” personality: Results from a representative German sample. Appetite 2018, 120, 246–255. [Google Scholar] [CrossRef]
- Agrawal, S.; Millett, C.J.; Dhillon, P.K.; Subramanian, S.V.; Ebrahim, S. Type of vegetarian diet, obesity and diabetes in adult Indian population. Nutr. J. 2014, 13, 89. [Google Scholar] [CrossRef]
- Yokoyama, Y.; Nishimura, K.; Barnard, N.D.; Takegami, M.; Watanabe, M.; Sekikawa, A.; Okamura, T.; Miyamoto, Y. Vegetarian diets and blood pressure: A meta-analysis. JAMA Intern. Med. 2014, 174, 577–587. [Google Scholar] [CrossRef]
- Lee, K.W.; Loh, H.C.; Ching, S.M.; Devaraj, N.K.; Hoo, F.K. Effects of Vegetarian Diets on Blood Pressure Lowering: A Systematic Review with Meta-Analysis and Trial Sequential Analysis. Nutrients 2020, 12, 1604. [Google Scholar] [CrossRef]
- Gibbs, J.; Gaskin, E.; Ji, C.; Miller, M.A.; Cappuccio, F.P. The effect of plant-based dietary patterns on blood pressure: A systematic review and meta-analysis of controlled intervention trials. J. Hypertens. 2021, 39, 23–37. [Google Scholar] [CrossRef]
- Barnard, N.D.; Levin, S.M.; Yokoyama, Y. A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J. Acad. Nutr. Diet. 2015, 115, 954–969. [Google Scholar] [CrossRef]
- Pollakova, D.; Andreadi, A.; Pacifici, F.; Della-Morte, D.; Lauro, D.; Tubili, C. The Impact of Vegan Diet in the Prevention and Treatment of Type 2 Diabetes: A Systematic Review. Nutrients 2021, 13, 2123. [Google Scholar] [CrossRef]
- Marrone, G.; Guerriero, C.; Palazzetti, D.; Lido, P.; Marolla, A.; Di Daniele, F.; Noce, A. Vegan Diet Health Benefits in Metabolic Syndrome. Nutrients 2021, 13, 817. [Google Scholar] [CrossRef]
- Tong, T.Y.N.; Appleby, P.N.; Bradbury, K.E.; Perez-Cornago, A.; Travis, R.C.; Clarke, R.; Key, T.J. Risks of ischaemic heart disease and stroke in meat eaters, fish eaters, and vegetarians over 18 years of follow-up: Results from the prospective EPIC-Oxford study. BMJ 2019, 366, l4897. [Google Scholar] [CrossRef]
- Sun, L.; Clarke, R.; Bennett, D.; Guo, Y.; Walters, R.G.; Hill, M.; Parish, S.; Millwood, I.Y.; Bian, Z.; Chen, Y.; et al. Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat. Med. 2019, 25, 569–574. [Google Scholar] [CrossRef]
- Huang, T.; Yang, B.; Zheng, J.; Li, G.; Wahlqvist, M.L.; Li, D. Cardiovascular disease mortality and cancer incidence in vegetarians: A meta-analysis and systematic review. Ann. Nutr. Metab. 2012, 60, 233–240. [Google Scholar] [CrossRef]
- Key, T.J.; Appleby, P.N.; Crowe, F.L.; Bradbury, K.E.; Schmidt, J.A.; Travis, R.C. Cancer in British vegetarians: Updated analyses of 4998 incident cancers in a cohort of 32,491 meat eaters, 8612 fish eaters, 18,298 vegetarians, and 2246 vegans. Am. J. Clin. Nutr. 2014, 100 (Suppl. S1), 378S–385S. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.S.; Tresserra-Rimbau, A.; Karavasiloglou, N.; Jennings, A.; Cantwell, M.; Hill, C.; Perez-Cornago, A.; Bondonno, N.P.; Murphy, N.; Rohrmann, S.; et al. Association of Healthful Plant-based Diet Adherence with Risk of Mortality and Major Chronic Diseases Among Adults in the UK. JAMA Netw. Open 2023, 6, e234714. [Google Scholar] [CrossRef] [PubMed]
- Castelnuovo, G.; Perez-Diaz-Del-Campo, N.; Rosso, C.; Armandi, A.; Caviglia, G.P.; Bugianesi, E. A Healthful Plant-Based Diet as an Alternative Dietary Approach in the Management of Metabolic Dysfunction-Associated Steatotic Liver Disease. Nutrients 2024, 16, 2027. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef]
- Lv, Y.; Rong, S.; Deng, Y.; Bao, W.; Xia, Y.; Chen, L. Plant-based diets, genetic predisposition and risk of non-alcoholic fatty liver disease. BMC Med. 2023, 21, 351. [Google Scholar] [CrossRef]
- Choi, S.H.; Oh, D.J.; Kwon, K.H.; Lee, J.K.; Koh, M.S.; Lee, J.H.; Kang, H.W. A vegetarian diet does not protect against nonalcoholic fatty liver disease (NAFLD): A cross-sectional study between Buddhist priests and the general population. Turk. J. Gastroenterol. Off. J. Turk. Soc. Gastroenterol. 2015, 26, 336–343. [Google Scholar] [CrossRef]
- Chiu, T.H.; Lin, M.N.; Pan, W.H.; Chen, Y.C.; Lin, C.L. Vegetarian diet, food substitution, and nonalcoholic fatty liver. Tzu Chi Med. J. 2018, 30, 102–109. [Google Scholar] [CrossRef]
- Mazidi, M.; Kengne, A.P. Higher adherence to plant-based diets are associated with lower likelihood of fatty liver. Clin. Nutr. 2019, 38, 1672–1677. [Google Scholar] [CrossRef]
- Kahleova, H.; Petersen, K.F.; Shulman, G.I.; Alwarith, J.; Rembert, E.; Tura, A.; Hill, M.; Holubkov, R.; Barnard, N.D. Effect of a Low-Fat Vegan Diet on Body Weight, Insulin Sensitivity, Postprandial Metabolism, and Intramyocellular and Hepatocellular Lipid Levels in Overweight Adults: A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e2025454. [Google Scholar] [CrossRef]
- Garousi, N.; Tamizifar, B.; Pourmasoumi, M.; Feizi, A.; Askari, G.; Clark, C.C.T.; Entezari, M.H. Effects of lacto-ovo-vegetarian diet vs. standard-weight-loss diet on obese and overweight adults with non-alcoholic fatty liver disease: A randomised clinical trial. Arch. Physiol. Biochem. 2023, 129, 975–983. [Google Scholar] [CrossRef]
- Ulzii, B.N.; Lim, K.; Shin, S. Association between plant-based diets and risk of metabolic dysfunction-associated steatotic liver disease in Korean adults: A prospective cohort study. Nutrition 2024, 128, 112579. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Peng, Z.; Li, M.; Zeng, X.; Li, H.; Zhu, Y.; Chen, H.; Hu, A.; Zhao, Q.; Zhang, Z.; et al. A Healthful Plant-Based Diet Is Associated with Lower Odds of Nonalcoholic Fatty Liver Disease. Nutrients 2022, 14, 4099. [Google Scholar] [CrossRef] [PubMed]
- Chiarioni, G.; Popa, S.L.; Dalbeni, A.; Senore, C.; Leucuta, D.C.; Baroni, L.; Fantin, A. Vegan Diet Advice Might Benefit Liver Enzymes in Nonalcoholic Fatty Liver Disease: An Open Observational Pilot Study. J. Gastrointest. Liver Dis. JGLD 2021, 30, 81–87. [Google Scholar] [CrossRef]
- Shafiee, M.; Sadeghi, A.; Ghafouri-Taleghani, F.; Nilghaz, M.; Ghods, M.; Narimani, B.; Hekmatdoost, A.; Saidpour, A. Effects of time restricted feeding combined with Lacto Ovo vegetarian diet on metabolic associated fatty liver disease management: A randomized clinical trial. Sci. Rep. 2025, 15, 4463. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E.; Neuschwander-Tetri, B.A.; Siddiqui, M.S.; Abdelmalek, M.F.; Caldwell, S.; Barb, D.; Kleiner, D.E.; Loomba, R. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology 2023, 77, 1797–1835. [Google Scholar] [CrossRef]
- Italian Association for the Study of the Liver (AISF) AISF position paper on nonalcoholic fatty liver disease (NAFLD): Updates and future directions. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2017, 49, 471–483. [CrossRef]
- Machado, A.M.; Guimarães, N.S.; Bocardi, V.B.; da Silva, T.P.R.; Carmo, A.S.D.; Menezes, M.C.; Duarte, C.K. Understanding weight regain after a nutritional weight loss intervention: Systematic review and meta-analysis. Clin. Nutr. ESPEN 2022, 49, 138–153. [Google Scholar] [CrossRef]
- Righetti, R.; Cinque, F.; Volpe, M.T.; Sebastiani, G. Integrating behavioral interventions into a holistic approach to metabolic dysfunction-associated steatotic liver disease. Expert Rev. Gastroenterol. Hepatol. 2024, 18, 303–313. [Google Scholar] [CrossRef]
- Wang, T.; Masedunskas, A.; Willett, W.C.; Fontana, L. Vegetarian and vegan diets: Benefits and drawbacks. Eur. Heart J. 2023, 44, 3423–3439. [Google Scholar] [CrossRef]
- Pugliese, N.; Bertazzoni, A.; Hassan, C.; Schattenberg, J.M.; Aghemo, A. Revolutionizing MASLD: How Artificial Intelligence Is Shaping the Future of Liver Care. Cancers 2025, 17, 722. [Google Scholar] [CrossRef]
- Pugliese, N.; Ravaioli, F. Generative Artificial Intelligence in Nutrition: A Revolution in Accessibility and Personalization. J. Nutr. 2025, 155, 667–668. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).