Fecal Calprotectin Determination in a Cohort of Children with Cow’s Milk Allergy
Abstract
1. Introduction
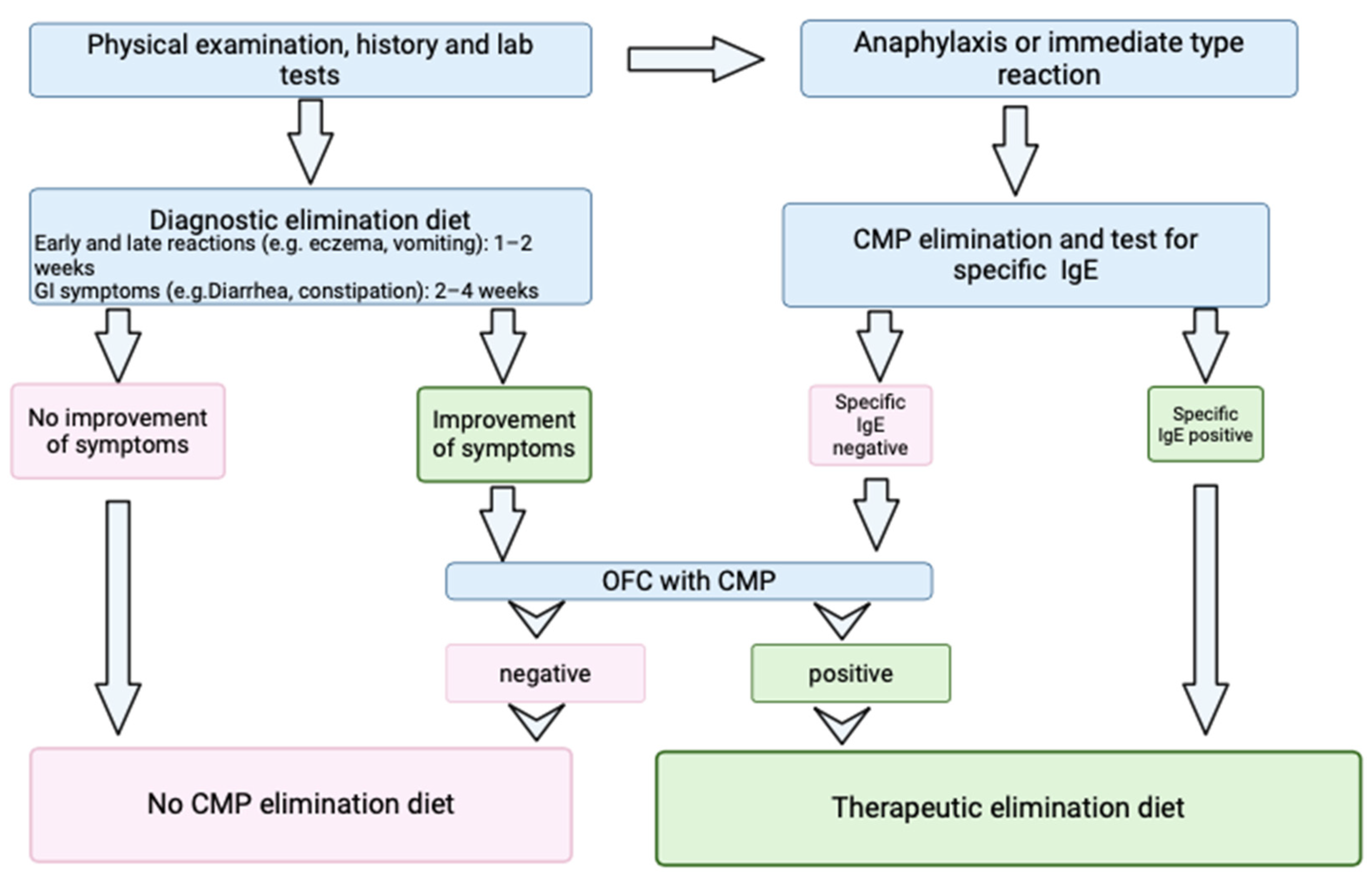
2. Materials and Methods
2.1. Study Design
2.1.1. Fecal Calprotectin Measurement
2.1.2. Ethics
2.1.3. Informed Consent Statement
2.1.4. Statistical Analysis
3. Results
Patients’ Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Licari, A.; Manti, S.; Marseglia, A.; Brambilla, I.; Votto, M.; Castagnoli, R.; Leonardi, S.; Marseglia, G.L. Food allergies: Current and future treatments. Medicina 2019, 55, 120. [Google Scholar] [CrossRef] [PubMed]
- Arvola, T.; Ruuska, T.; Keränen, J.; Hyöty, H.; Salminen, S.; Isolauri, E. Rectal bleeding in infancy: Clinical, allergological, and microbiological examination. Pediatrics 2006, 117, e760–e768. [Google Scholar] [CrossRef]
- Vandenplas, Y.; Koletzko, S.; Isolauri, E.; Hill, D.; Oranje, A.P.; Brueton, M.; Staiano, A.; Dupont, C. Guidelines for the diagnosis and management of cow’s milk protein allergy in infants. Arch. Dis. Child. 2007, 92, 902–908. [Google Scholar] [CrossRef] [PubMed]
- Koletzko, S.; Niggemann, B.; Arato, A.; Dias, J.A.; Heuschkel, R.; Husby, S.; Mearin, M.L.; Papadopoulou, A.; Ruemmele, F.M.; Staiano, A.; et al. Diagnostic approach and management of cow’s-milk protein allergy in infants and children: ESPGHAN GI committee practical guidelines. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Sicherer, S.H. Epidemiology of food allergy. J. Allergy Clin. Immunol. 2011, 127, 594–602. [Google Scholar] [CrossRef]
- Rona, R.J.; Keil, T.; Summers, C.; Zuidmeer, L.; Sodergren, E.; Sigurdardottir, S.T.; Lindner, T.; Goldhahn, K.; Dahlstrom, J.; McBride, D.; et al. The prevalence of food allergy: A meta-analysis. J. Allergy Clin. Immunol. 2007, 120, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Høst, A.; Høst, A.; Halken, S.; Jacobsen, H.P.; Christensen, A.E.; Herskind, A.M.; Plesner, K. Clinical course of cow’s milk protein allergy/intolerance and atopic diseases in childhood. Pediatr. Allergy Immunol. Suppl. 2002, 13, 23–28. [Google Scholar] [CrossRef]
- Ambroszkiewicz, J.; Gajewska, J.; Chełchowska, M.; Rowicka, G. Assessment of inflammatory markers in children with cow’s milk allergy treated with a milk-free diet. Nutrients 2021, 13, 1057. [Google Scholar] [CrossRef] [PubMed]
- Anvari, S.; Miller, J.; Yeh, C.; Davis, C.M. IgE-Mediated Food Allergy. Clin. Rev. Allergy Immunol. 2019, 57, 244–260. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, M.; Coppola, L.; Coppola, A.; Capozzi, L. Iron deficiency in childhood and adolescence: Retrospective review. Hemat. 2006, 11, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Trillo Belizón, C.; Ortega Páez, E.; Medina Claros, A.F.; Rodríguez Sánchez, I.; Reina González, A.; Vera Medialdea, R.; Ramón Salguero, J.M. Faecal calprotectin as an aid to the diagnosis of non-IgE mediated cow’s milk protein allergy. An. Pediatr. 2016, 84, 318. [Google Scholar] [CrossRef] [PubMed]
- Mori, F.; Barni, S.; Cianferoni, A.; Pucci, N.; de Martino, M.; Novembre, E. Cytokine expression in CD3+ cells in an infant with food protein-induced enterocolitis syndrome (FPIES): Case report. Clin. Dev. Immunol. 2009, 67, 81–93. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Sicherer, S.; Berin, M.C. Pathophysiology of Non-IgE-Mediated Food Allergy. Immunotargets Ther. 2021, 10, 431–446. [Google Scholar] [CrossRef]
- Berni Canani, R.; De Filippis, F.; Nocerino, R.; Paparo, L.; Di Scala, C.; Cosenza, L.; Della Gatta, G.; Calignano, A.; De Caro, C.; Laiola, M.; et al. Gut microbiota composition and butyrate production in children affected by non-IgE-mediated cow’s milk allergy. Sci. Rep. 2018, 8, 12500. [Google Scholar] [CrossRef] [PubMed]
- Labrosse, R.; Graham, F.; Caubet, J.C. Non-Ige-mediated gastrointestinal food allergies in children: An update. Nutrients 2020, 12, 2086. [Google Scholar] [CrossRef] [PubMed]
- Burris, A.D.; Burris, J. Cow’s Milk Protein Allergy in Term and Preterm Infants: Clinical Manifestations, Immunologic Pathophysiology, and Management Strategies. Neoreviews 2020, 21, e79. [Google Scholar] [CrossRef]
- Burks, W.; Tang, M.; Sicherer, S.; Muraro, A.; Eigenmann, P.A.; Ebisawa, M.; Fiocchi, A.; Chiang, W.; Beyer, K.; Wood, R.; et al. ICON: Food allergy. J. Allergy Clin. Immunol. 2012, 129, 906–909. [Google Scholar] [CrossRef]
- NIAID-Sponsored Expert Panel; Boyce, J.A.; Assa’ad, A.; Burks, A.W.; Jones, S.M.; Sampson, H.A.; Wood, R.A.; Plaut, M.; Cooper, S.F.; Fenton, M.J.; et al. Guidelines for the diagnosis and management of food allergy in the United States: Report of the NIAID-sponsored expert panel. J. Allergy Clin. Immunol. 2010, 126 (Suppl. S6), S1–S58. [Google Scholar] [CrossRef]
- Vandenplas, Y.; Bajerova, K.; Dupont, C.; Eigenmann, P.; Kuitunen, M.; Meyer, R.; Ribes-Koninckx, C.; Salvatore, S.; Shamir, R.; Szajewska, H. The Cow’s Milk Related Symptom Score: The 2022 Update. Nutrients 2022, 14, 2682. [Google Scholar] [CrossRef]
- Saarinen, K.M.; Pelkonen, A.S.; Mäkelä, M.J. Clinical course and prognosis of cow’s milk allergy are dependent on milk-specific IgE status. J. Allergy Clin. Immunol. 2005, 116, 869–875. [Google Scholar] [CrossRef]
- Isaksen, B. Calprotectin inhibits matrix metalloproteinases by sequestration of zinc. Mol. Pathol. 2001, 54, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Stríz, I.; Trebichavský, I. Calprotectin—A Pleiotropic Molecule in Acute and Chronic Inflammation. Physiol. Res. 2004, 53, 245–253. [Google Scholar] [CrossRef]
- Canani, R.B.; de Horatio, L.T.; Terrin, G.; Romano, M.T.; Miele, E.; Staiano, A.; Rapacciuolo, L.; Polito, G.; Bisesti, V.; Manguso, F.; et al. Combined use of noninvasive tests is useful in the initial diagnostic approach to a child with suspected inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 2006, 42, 9–15. [Google Scholar] [CrossRef]
- von Roon, A.C.; Karamountzos, L.; Purkayastha, S.; Reese, G.E.; Darzi, A.W.; Teare, J.P.; Paraskeva, P.; Tekkis, P.P. Diagnostic precision of fecal calprotectin for inflammatory bowel disease and colorectal malignancy. Am. J. Gastroenterol. 2007, 102, 803–813. [Google Scholar] [CrossRef]
- Chang, M.H.; Chou, J.W.; Chen, S.M.; Tsai, M.C.; Sun, Y.S.; Lin, C.C.; Lin, C.P. Faecal calprotectin as a novel biomarker for differentiating between inflammatory bowel disease and irritable bowel syndrome. Mol. Medic. Rep. 2014, 10, 522–526. [Google Scholar] [CrossRef]
- Berni Canani, R.; Rapacciuolo, L.; Romano, M.T.; Tanturri de Horatio, L.; Terrin, G.; Manguso, F.; Cirillo, P.; Paparo, F.; Troncone, R. Diagnostic value of faecal calprotectin in pediatric gastroenterology clinical practice. Dig. Liver Dis. 2004, 36, 467–470. [Google Scholar] [CrossRef]
- Xiong, L.J.; Xie, X.L.; Li, Y.; Deng, X.Z. Current status of fecal calprotectin as a diagnostic or monitoring biomarker for cow’s milk protein allergy in children: A scoping review. World J. Pediatr. 2021, 17, 63–70. [Google Scholar] [CrossRef]
- Vandenplas, Y.; Broekaert, I.; Domellöf, M.; Indrio, F.; Lapillonne, A.; Pienar, C.; Ribes-Koninckx, C.; Shamir, R.; Szajewska, H.; Thapar, N.; et al. An ESPGHAN Position Paper on the Diagnosis, Management, and Prevention of Cow’s Milk Allergy. J. Ped. Gastr. Nut. 2024, 78, 386–413. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J.A.S.; Sicherer, S.H. Diagnosis of food allergy: Epicutaneous skin tests, in vitro tests, and oral food challenge. Curr. Allergy Asthma Rep. 2011, 11, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Ricciuto, A.; Griffiths, A.M. Clinical value of fecal calprotectin. Crit. Rev. Clin. Lab. Sci. 2019, 56, 307–320. [Google Scholar] [CrossRef]
- Ayling, R.M.; Kok, K. Fecal Calprotectin. Adv. Clin. Chem. 2018, 87, 161–190. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Li, F.; Wang, J.; Ma, J.; Sheng, X. Upregulation of calprotectin in mild IgE-mediated ovalbumin hypersensitivity. Oncotarget 2017, 8, 37342–37354. [Google Scholar] [CrossRef][Green Version]
- Baldassarre, M.E.; Laforgia, N.; Fanelli, M.; Laneve, A.; Grosso, R.; Lifschitz, C. Lactobacillus GG Improves Recovery in Infants with Blood in the Stools and Presumptive Allergic Colitis Compared with Extensively Hydrolyzed Formula Alone. J. Pediatr. 2010, 156, 397–401. [Google Scholar] [CrossRef]
- Belizón, C.T.; Páez, E.O.; Claros, A.F.M.; Sánchez, I.R.; González, A.R.; Medialdea, R.V.; Salguero, J.M.R. Calprotectina fecal como apoyo al diagnóstico en la alergia a las proteínas de leche de vaca no IgE mediada. An. Pediatr. 2016, 84, 318–323. [Google Scholar] [CrossRef]
- Beşer, Ö.F.; Sancak, S.; Erkan, T.; Kutlu, T.; Çokuğraş, H.; Çokuğraş, F.Ç. Can fecal calprotectin level be used as a markers of inflammation in the diagnosis and follow-up of cow’s milk protein allergy? Allergy Asthma Immunol. Res. 2014, 6, 33–38. [Google Scholar] [CrossRef]
- Zhang, Z.H.; Wang, W.; Zhang, X.H.; Pan, J.; Chen, X. Fecal Calprotectin in Children with Cow’s Milk Protein Allergy: A Systematic Review and Meta-Analysis. Int. Arch. All. Immunol. 2022, 183, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Qiu, L.; Wang, J.; Ren, F.; Shen, L.; Li, F. Can fecal calprotectin levels be used to monitor infant milk protein allergies? Allergy Asthma Clin. Immunol. 2021, 17, 132. [Google Scholar] [CrossRef] [PubMed]
- Roca, M.; Donat, E.; Rodriguez Varela, A.; Carvajal, E.; Cano, F.; Armisen, A.; Ekoff, H.; Cañada-Martínez, A.J.; Rydell, N.; Ribes-Koninckx, C. Fecal calprotectin and eosinophil-derived neurotoxin in children with non-Ige-mediated cow’s milk protein allergy. J. Clin. Med. 2021, 10, 1595. [Google Scholar] [CrossRef]
- Koninckx, C.R.; Donat, E.; Benninga, M.A.; Broekaert, I.J.; Gottrand, F.; Kolho, K.L.; Lionetti, P.; Miele, E.; Orel, R.; Papadopoulou, A.; et al. The Use of Fecal Calprotectin Testing in Paediatric Disorders: A Position Paper of the European Society for Paediatric Gastroenterology and Nutrition Gastroenterology Committee. J. Pediatr. Gastroenterol. Nutr. 2021, 72, 617–640. [Google Scholar] [CrossRef] [PubMed]
- Merras-Salmio, L.; Kolho, K.L.; Pelkonen, A.S.; Kuitunen, M.; Mäkelä, M.J.; Savilahti, E. Markers of gut mucosal inflammation and cow’s milk specific immunoglobulins in non-IgE cow’s milk allergy. Clin. Transl. Allergy 2014, 4, 8. [Google Scholar] [CrossRef]
- Lendvai-Emmert, D.; Emmert, V.; Makai, A.; Fusz, K.; Prémusz, V.; Eklics, K.; Sarlós, P.; Tóth, P.; Amrein, K.; Tóth, G. Fecal calprotectin levels in pediatric cow’s milk protein allergy. Front. Pediatr. 2022, 10, 945212. [Google Scholar] [CrossRef] [PubMed]
- Zain-Alabedeen, S.; Kamel, N.; Amin, M.; Vernon-Roberts, A.; Day, A.S.; Khashana, A. Fecal Calprotectin and Cow’s Milk-Related-Symptoms Score in Children with Cow’s Milk Protein Allergy. Pediatr. Gastroenterol. Hepatol. Nutr. 2023, 26, 43–49. [Google Scholar] [CrossRef] [PubMed]


| Patients’ Characteristics | (n = 51) |
|---|---|
| Boys/girls | 34/17 (67/33%) |
| Age (years) | 1.3 [0.7, 2.2] |
| Weight (kg) | 10.5 [8.8, 12.8] |
| Height (cm) | 78.0 [73.5, 90.5] |
| Breastfed/formula fed/mixed feeding | 25/15/11 (49/30/21%) |
| IgE-mediated/non-IgE-mediated CMA | 25/26 (49/51%) |
| Tot IgE > 15/<15 (kU/L) | 22/28 (56/44%) |
| sIgE to CM > 0.35/<0.35 kU/L | 29/21 (58/42%) |
| sIgE to α-lactalbumin > 0.35/<0.35 kU/L | 13/37 (74/26%) |
| sIgE to β-lactoglobulin > 0.35/<0.35 kU/L | 18/55 (25/75%) |
| sIgE to casein > 0.35/<0.35 kU/L | 14/36 (28/72%) |
| Symptoms | |
| Vomiting | 20 (44%) |
| Diarrhea/Constipation | 37 (73%) |
| Abdominal pain | 21 (41%) |
| Skin involvement (urticaria, dermatitis) | 38 (75%) |
| Measurements | |
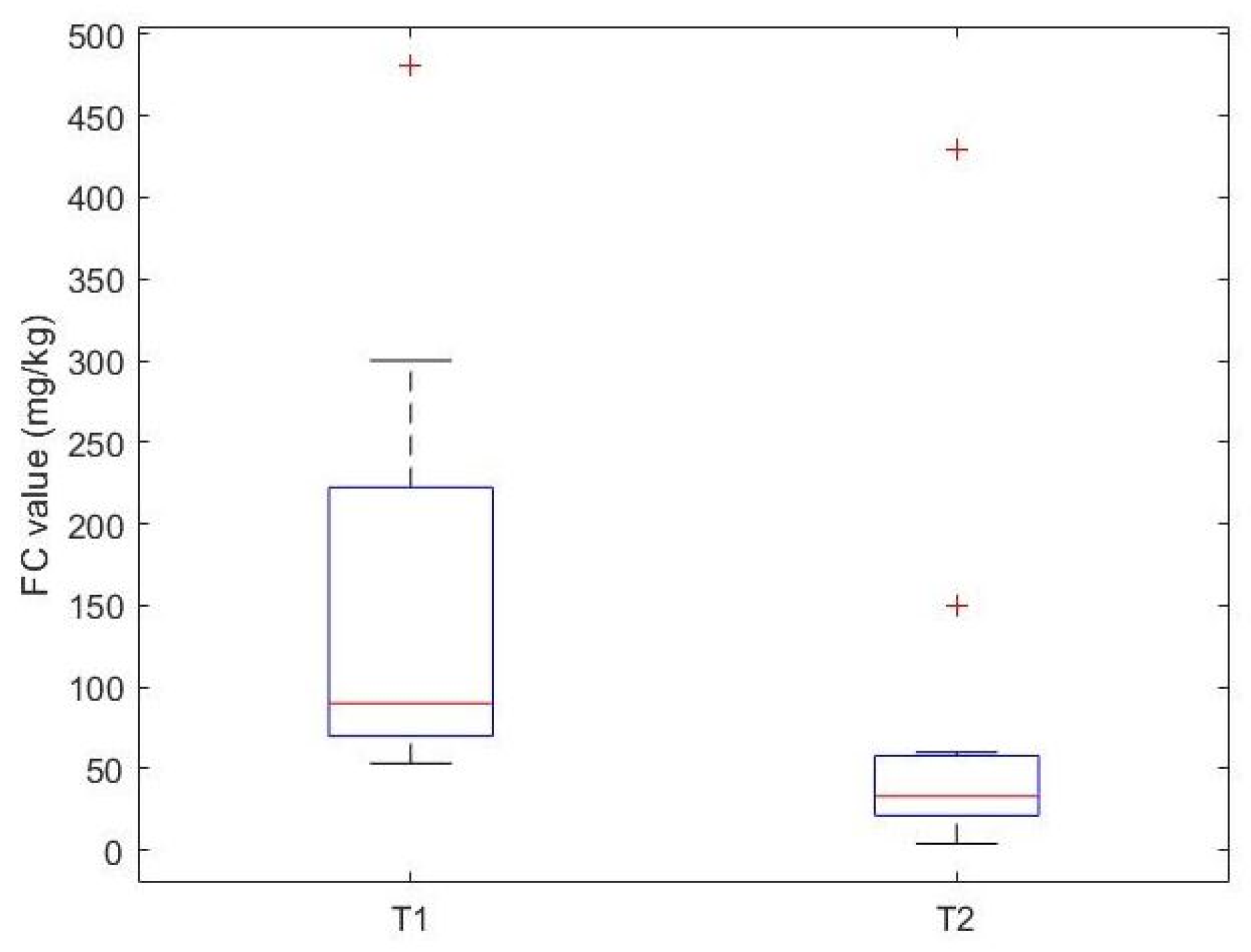
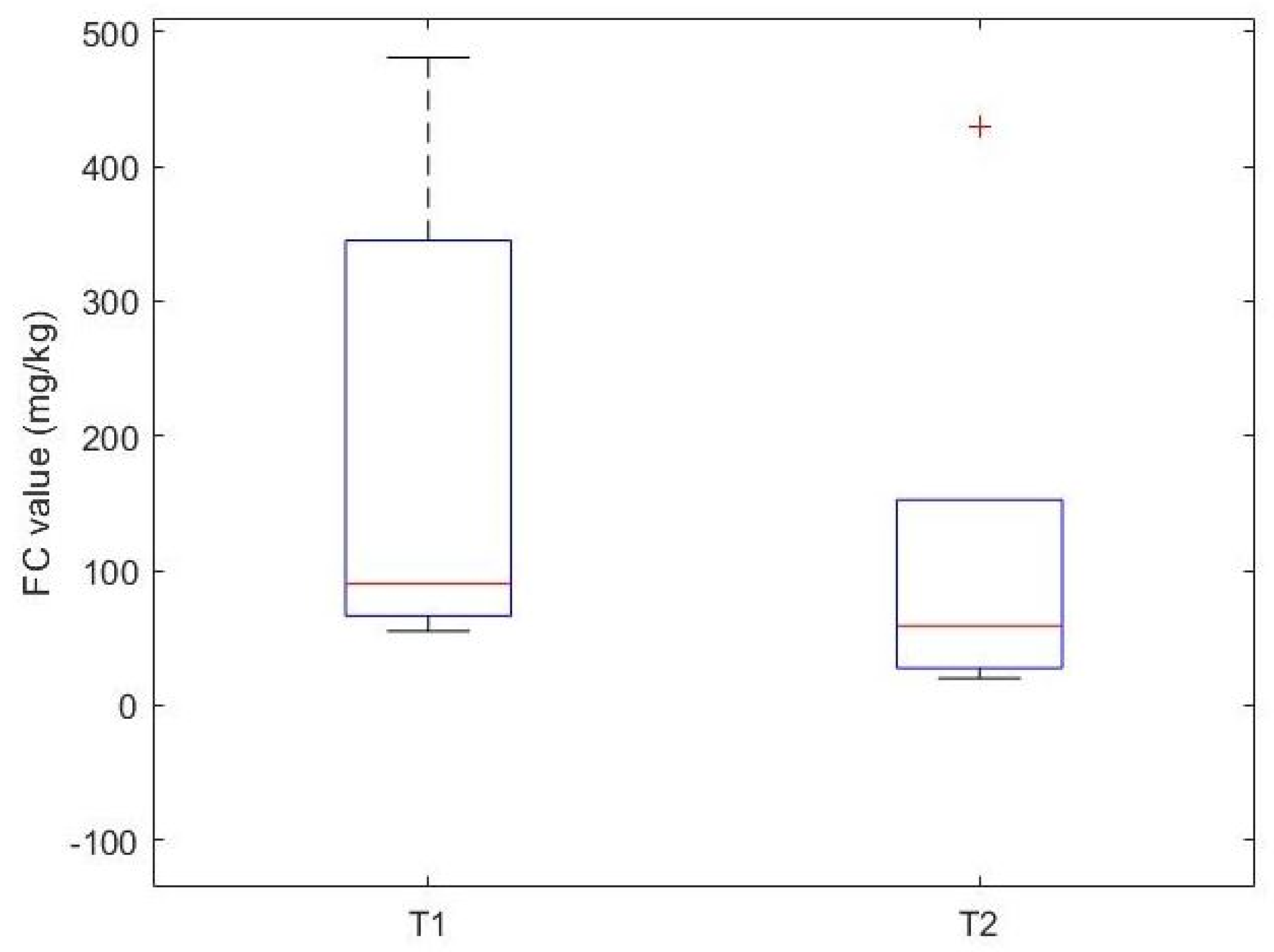
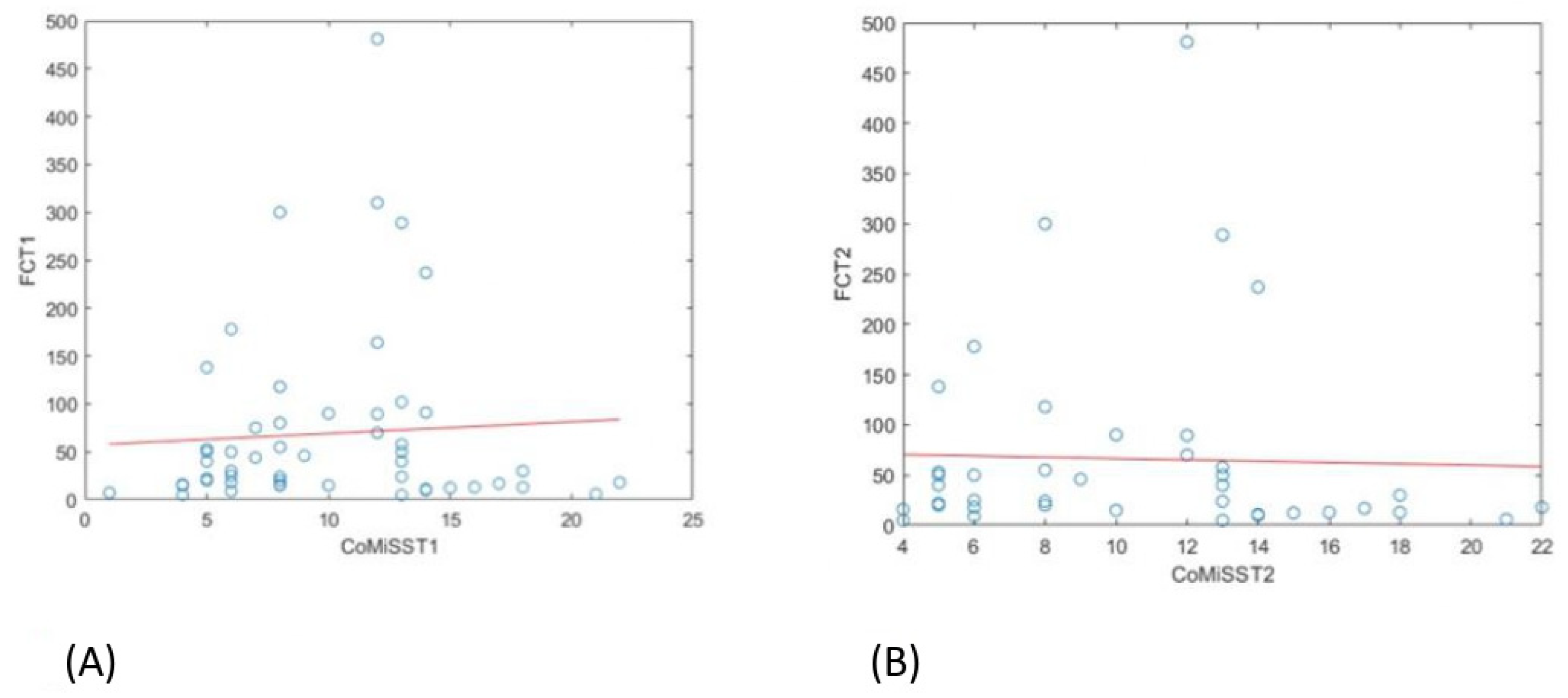
| Calprotectin T1 (mg/kg) | 30 [15.5, 63.9] |
| Calprotectin T2 (mg/kg) | 16.1 [10.0, 30.0] |
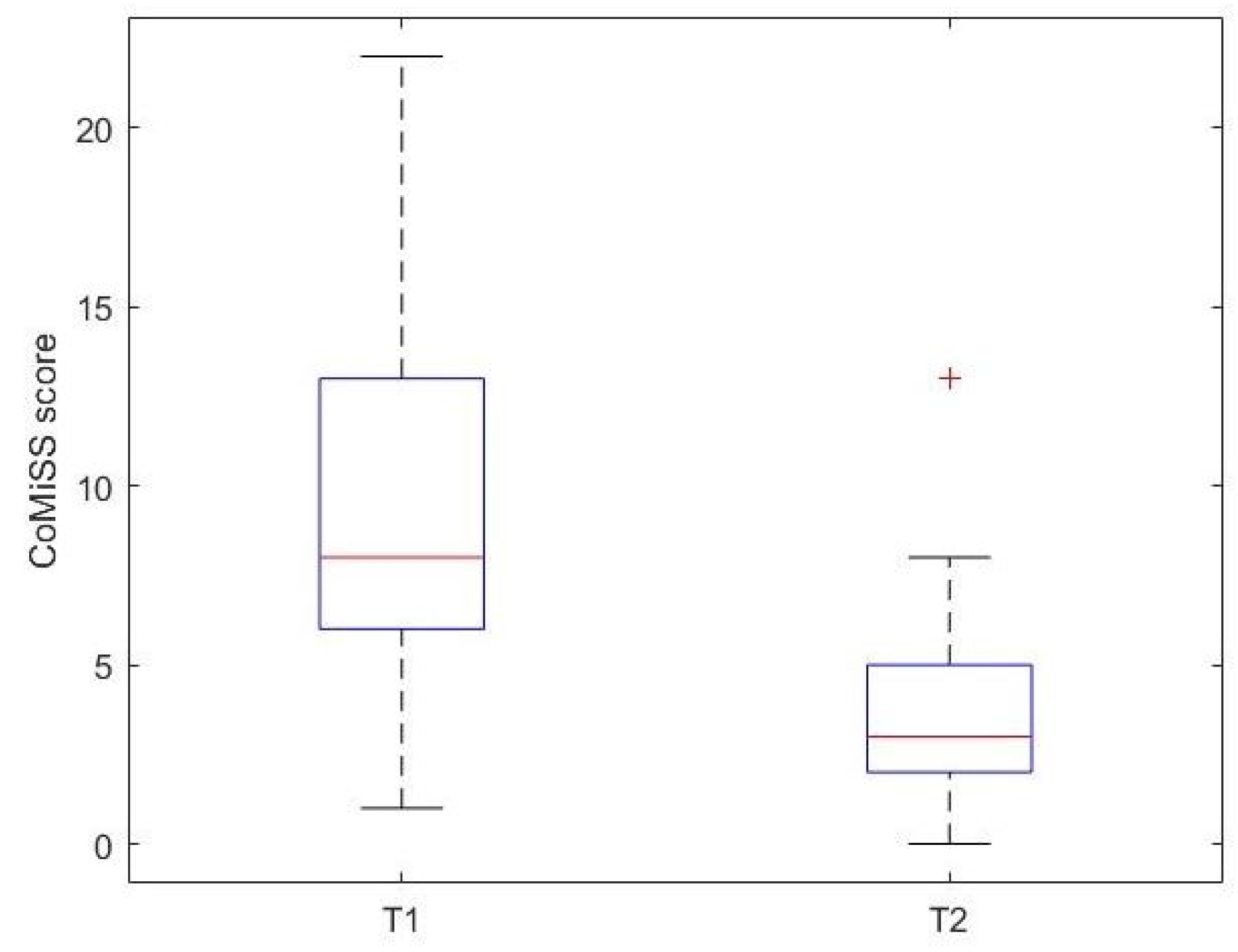
| CoMiSS T1 | 8.5 [6.0, 13.0] |
| CoMiSS T2 | 3.0 [2.0, 5.0] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anania, C.; Mondì, F.; Brindisi, G.; Spagnoli, A.; De Canditiis, D.; Gesmini, A.; Marchetti, L.; Fichera, A.; Piccioni, M.G.; Zicari, A.M.; et al. Fecal Calprotectin Determination in a Cohort of Children with Cow’s Milk Allergy. Nutrients 2025, 17, 194. https://doi.org/10.3390/nu17010194
Anania C, Mondì F, Brindisi G, Spagnoli A, De Canditiis D, Gesmini A, Marchetti L, Fichera A, Piccioni MG, Zicari AM, et al. Fecal Calprotectin Determination in a Cohort of Children with Cow’s Milk Allergy. Nutrients. 2025; 17(1):194. https://doi.org/10.3390/nu17010194
Chicago/Turabian StyleAnania, Caterina, Filippo Mondì, Giulia Brindisi, Alessandra Spagnoli, Daniela De Canditiis, Arianna Gesmini, Lavinia Marchetti, Alessia Fichera, Maria Grazia Piccioni, Anna Maria Zicari, and et al. 2025. "Fecal Calprotectin Determination in a Cohort of Children with Cow’s Milk Allergy" Nutrients 17, no. 1: 194. https://doi.org/10.3390/nu17010194
APA StyleAnania, C., Mondì, F., Brindisi, G., Spagnoli, A., De Canditiis, D., Gesmini, A., Marchetti, L., Fichera, A., Piccioni, M. G., Zicari, A. M., & Olivero, F. (2025). Fecal Calprotectin Determination in a Cohort of Children with Cow’s Milk Allergy. Nutrients, 17(1), 194. https://doi.org/10.3390/nu17010194







