Nutritional Status and Recurrent Major Cardiovascular Events Following Acute Myocardial Infarction—A Follow-Up Study in a Primary Percutaneous Coronary Intervention Center
Abstract
1. Introduction
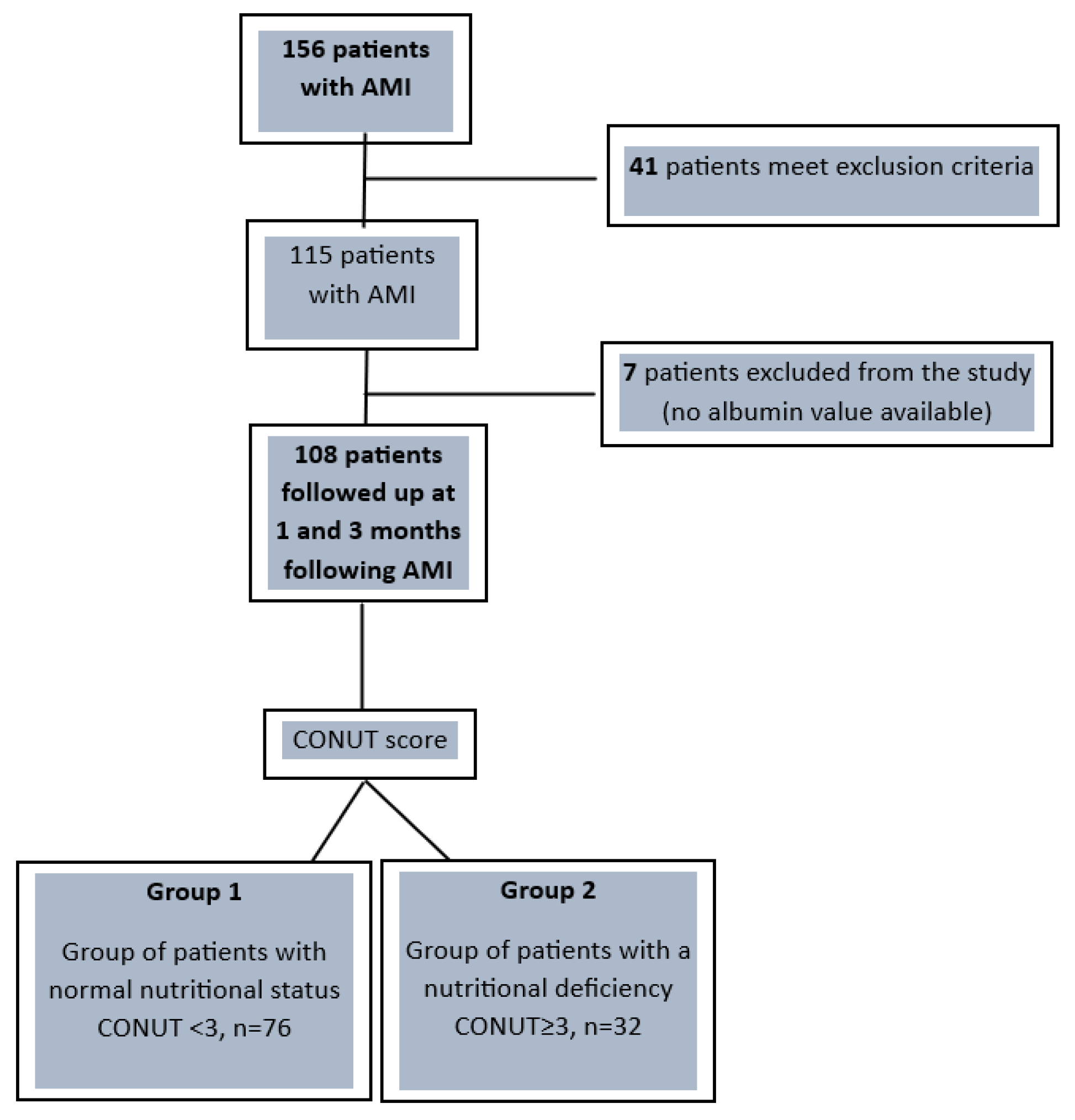
2. Materials and Methods
Statistical Analysis
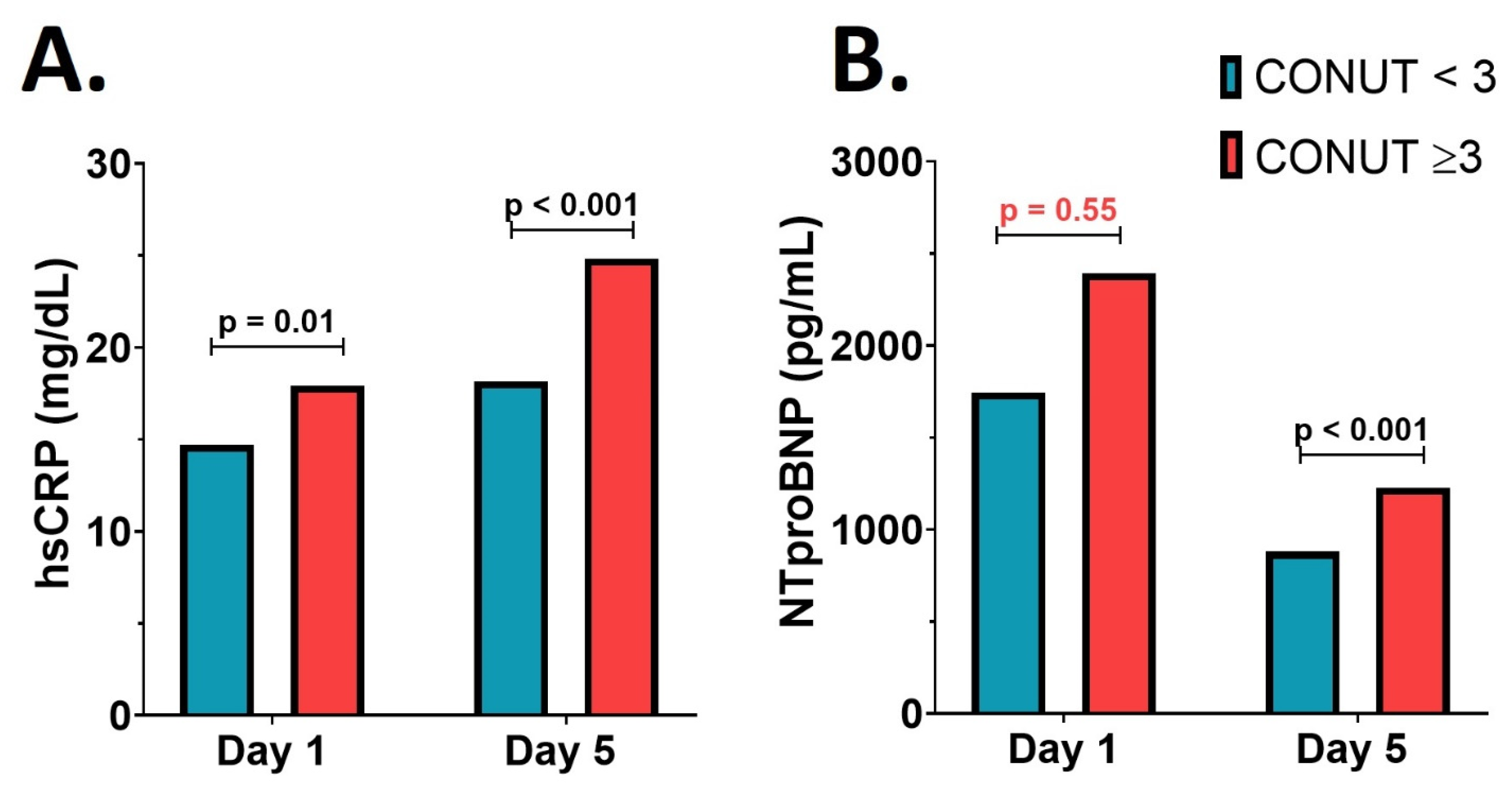
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Czapla, M.; Karniej, P.; Juárez-Vela, R.; Łokieć, K. The Association between Nutritional Status and In-Hospital Mortality among Patients with Acute Coronary Syndrome—A Result of the Retrospective Nutritional Status Heart Study (NSHS). Nutrients 2020, 12, 3091. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, T.; Jacobsen, R.K.; Toft, U.; Aadahl, M.; Glümer, C.; Pisinger, C. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ 2014, 348, g3617. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Quintana, E.; Sánchez-Matos, M.M.; Estupiñán-León, H.; Rojas-Brito, A.B.; González-Martín, J.M.; Rodríguez-González, F.; Tugores, A. Malnutrition is independently associated with an increased risk of major cardiovascular events in adult patients with congenital heart disease. Nutr. Metab. Cardiovasc. Dis. NMCD 2021, 31, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Basta, G.; Chatzianagnostou, K.; Paradossi, U.; Botto, N.; Del Turco, S.; Taddei, A.; Berti, S.; Mazzone, A. The prognostic impact of objective nutritional indices in elderly patients with ST-elevation myocardial infarction undergoing primary coronary intervention. Int. J. Cardiol. 2016, 221, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, D.H.; Bopp, M.M.; Roberson, P.K. Protein-energy Undernutrition and Life-threatening Complications among the Hospitalized Elderly. J. Gen. Intern. Med. 2002, 17, 923–932. [Google Scholar] [CrossRef] [PubMed]
- van Dronkelaar, C.; Tieland, M.; Cederholm, T.; Reijnierse, E.M.; Weijs, P.J.M.; Kruizenga, H. Malnutrition Screening Tools Are Not Sensitive Enough to Identify Older Hospital Patients with Malnutrition. Nutrients 2023, 15, 5126. [Google Scholar] [CrossRef]
- de Ulibarri Pérez, J.I.; Picón César, M.J.; García Benavent, E.; Mancha Alvarez-Estrada, A. Early detection and control of hospital malnutrition. Nutr. Hosp. 2022, 17, 139–146. [Google Scholar]
- Takahashi, H.; Ito, Y.; Ishii, H.; Aoyama, T.; Kamoi, D.; Kasuga, H.; Yasuda, K.; Maruyama, S.; Matsuo, S.; Murohara, T.; et al. Geriatric nutritional risk index accurately predicts cardiovascular mortality in incident hemodialysis patients. J. Cardiol. 2014, 64, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Vickers, N.J. Animal Communication: When I’m Calling You, Will You Answer Too? Curr. Biol. 2017, 27, R713–R715. [Google Scholar] [CrossRef] [PubMed]
- Kunimura, A.; Ishii, H.; Uetani, T.; Aoki, T.; Harada, K.; Hirayama, K.; Negishi, Y.; Shibata, Y.; Sumi, T.; Kawashima, K.; et al. Impact of Geriatric Nutritional Risk Index on cardiovascular outcomes in patients with stable coronary artery disease. J. Cardiol. 2017, 69, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2013, 62, e147–e239. [Google Scholar] [CrossRef] [PubMed]
- Coles, A.H.; Fisher, K.A.; Darling, C.; McManus, D.; Maitas, O.; Yarzebski, J.; Gore, J.M.; Lessard, D.; Goldberg, R.J. Recent trends in post-discharge mortality among patients with an initial acute myocardial infarction. Am. J. Cardiol. 2012, 110, 1073–1077. [Google Scholar] [CrossRef] [PubMed]
- Moon, C.M.; Kim, Y.H.; Ahn, Y.K.; Jeong, M.H.; Jeong, G.W. Metabolic alterations in acute myocardial ischemia-reperfusion injury and necrosis using in vivo hyperpolarized [1-13C] pyruvate MR spectroscopy. Sci. Rep. 2019, 9, 18427. [Google Scholar] [CrossRef] [PubMed]
- Anker, S.D.; Ponikowski, P.; Varney, S.; Chua, T.P.; Clark, A.L.; Webb-Peploe, K.M.; Harrington, D.; Kox, W.J.; Poole-Wilson, P.A.; Coats, A.J. Wasting as independent risk factor for mortality in chronic heart failure. Lancet 1997, 349, 1050–1053. [Google Scholar] [CrossRef] [PubMed]
- Lena, A.; Ebner, N.; Coats, A.J.S.; Anker, M.S. Cardiaccachexia: The mandate to increase clinician awareness. Curr. Opin. Support. Palliat. Care 2019, 13, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Blîndu, E.; Benedek, I.; Rodean, I.P.; Halațiu, V.B.; Raț, N.; Țolescu, C.; Mihăilă, T.; Roșca, A.; Mátyás, B.-B.; Szabó, E.; et al. Regional Differences in the Level of Inflammation Between the Right and Left Coronary Arteries—A Coronary Computed Tomography Angiography Study of Epicardial Fat Attenuation Index in Four Scenarios of Cardiovascular Emergencies. J. Cardiovasc. Emergencies 2023, 9, 111–119. [Google Scholar] [CrossRef]
- Tolescu, C.; Masca, V.; Bajka, B.; Benedek, I. COVID Infection and Spontaneous Coronary Dissection in a Pregnant Woman—A Therapeutic Challenge. J. Cardiovasc. Emergencies 2023, 9, 79–82. [Google Scholar] [CrossRef]
- Rodean, I.P.; Biriș, C.I.; Halațiu, V.B.; Modiga, A.; Lazăr, L.; Benedek, I.; Benedek, T. Is There a Link between COVID-19 Infection, Periodontal Disease and Acute Myocardial Infarction? Life 2021, 11, 1050. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Shah, J.A.; Solangi, B.A.; Ammar, A.; Kumar, M.; Khan, N.; Sial, J.A.; Saghir, T.; Qamar, N.; Karim, M. The Burden of Short-term Major Adverse Cardiac Events and its Determinants after Emergency Percutaneous Coronary Revascularization: A Prospective Follow-up Study. J. Saudi Heart Assoc. 2022, 34, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Horiuchi, Y.; Tanimoto, S.; Okuno, T.; Aoki, J.; Yahagi, K.; Sato, Y.; Tanaka, T.; Koseki, K.; Komiyama, K.; Nakajima, H.; et al. Hemodynamic correlates of nutritional indexes in heart failure. J. Cardiol. 2018, 71, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Narumi, T.; Arimoto, T.; Funayama, A.; Kadowaki, S.; Otaki, Y.; Nishiyama, S.; Takahashi, H.; Shishido, T.; Miyashita, T.; Miyamoto, T.; et al. The prognostic importance of objective nutritional indexes in patients with chronic heart failure. J. Cardiol. 2013, 62, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Boban, M.; Bulj, N.; Kolačević Zeljković, M.; Radeljić, V.; Krcmar, T.; Trbusic, M.; Delić-Brkljačić, D.; Alebic, T.; Vcev, A. Nutritional Considerations of Cardiovascular Diseases and Treatments. Nutr. Metab. Insights 2019, 12, 1178638819833705. [Google Scholar] [CrossRef] [PubMed]
- Sharma, Y.; Miller, M.; Kaambwa, B.; Shahi, R.; Hakendorf, P.; Horwood, C.; Thompson, C. Factors influencing early and late readmissions in Australian hospitalised patients and investigating role of admission nutrition status as a predictor of hospital readmissions: A cohort study. BMJ Open 2018, 8, e022246. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.; Kondrup, J.; Prokopowicz, J.; Schiesser, M.; Krähenbühl, L.; Meier, R.; Liberda, M.; EuroOOPS study group. EuroOOPS: An international, multicentre study to implement nutritional risk screening and evaluate clinical outcome. Clin. Nutr. 2008, 27, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.H.; Kook, H.Y.; Hong, Y.J.; Kim, J.H.; Ahn, Y.; Jeong, M.H. Influence of undernutrition at admission on clinical outcomes in patients with acute myocardial infarction. J. Cardiol. 2017, 69, 555–560. [Google Scholar] [CrossRef]
- Rus, V.; Chitu, M.; Cernea, S.; Benedek, I.; Hodas, R.; Zavate, R.; Nyulas, T.; Hintea, M.; Benedek, T. Altered nutritional status, inflammation and systemic vulnerability in patients with acute myocardial infarction undergoing percutaneous coronary revascularisation: A prospective study in a level 3 cardiac critical care unit. Nutr. Diet. 2020, 77, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Sze, S.; Pellicori, P.; Kazmi, S.; Rigby, A.; Cleland, J.G.F.; Wong, K.; Clark, A.L. Prevalence and Prognostic Significance of Malnutrition Using 3 Scoring Systems Among Outpatients with Heart Failure A Comparison with Body Mass Index. JACC Heart Fail. 2018, 6, 476–486. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, S.; Ureshino, H.; Kidoguchi, K.; Kusaba, K.; Kizuka-Sano, H.; Sano, H.; Nishioka, A.; Yamaguchi, K.; Kamachi, K.; Itamura, H.; et al. Clinical impact of the conut score in patients with multiple myeloma. Ann. Hematol. 2020, 99, 113–119. [Google Scholar] [CrossRef]
- Wada, H.; Dohi, T.; Miyauchi, K.; Shitara, J.; Endo, H.; Doi, S.; Naito, R.; Konishi, H.; Tsuboi, S.; Ogita, M.; et al. Impact of serum albumin levels on long-term outcomes in patients undergoing percutaneous coronary intervention. Heart Vessels 2017, 32, 1085–1092. [Google Scholar] [CrossRef]
- Kanda, D.; Ikeda, Y.; Takumi, T.; Tokushige, A.; Sonoda, T.; Arikawa, R.; Anzaki, K.; Kosedo, I.; Ohishi, M. Impact of nutritional status on prognosis in acute myocardial infarction patients undergoing percutaneous coronary intervention. BMC Cardiovasc. Disord. 2022, 22, 3. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Zhang, S.; Shen, S.; Deng, L.; Shen, L.; Qian, J.; Ge, J. Association of Controlling Nutritional Status Score with 2-Year Clinical Outcomes in Patients with ST Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Heart Lung Circ. 2020, 29, 1758–1765. [Google Scholar] [CrossRef] [PubMed]
- Arero, G.; Arero, A.G.; Mohammed, S.H.; Vasheghani-Farahani, A. Prognostic Potential of the Controlling Nutritional Status (CONUT) Score in Predicting All-Cause Mortality and Major Adverse Cardiovascular Events in Patients With Coronary Artery Disease: A Meta-Analysis. Front. Nutr. 2022, 9, 850641. [Google Scholar] [CrossRef] [PubMed]
- Rus, V.; Opincariu, D.; Hodas, R.; Nyulas, T.; Hintea, M.; Benedek, T. Interrelation between altered nutritional status and clinical outcomes in patients with acute myocardial infarction admitted in a tertiary intensive cardiac care unit. J. Cardiovasc. Emergencies 2018, 4, 32–40. [Google Scholar] [CrossRef]
- Luke, J.N.; Schmidt, D.F.; Ritte, R.; O’Dea, K.; Brown, A.; Piers, L.S.; Jenkins, A.J.; Rowley, K.G. Nutritional predictors of chronic disease in a central Australian aboriginal cohort: A multi-mixture modelling analysis. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Menzel, A.; Samouda, H.; Dohet, F.; Loap, S.; Ellulu, M.S.; Bohn, T. Common and Novel Markers for Measuring Inflammation and Oxidative Stress Ex Vivo in Research and Clinical Practice-Which to Use Regarding Disease Outcomes? Antioxidants 2021, 10, 414. [Google Scholar] [CrossRef] [PubMed]
| CONUT < 3 (n = 76) | CONUT ≥ 3 (n = 32) | p Value | R.R. | |
|---|---|---|---|---|
| Demographic data | ||||
| Age (years) | 61.30 ± 13.37 | 62.38 ± 12.30 | 0.68 | N.A. |
| Weight (kg) | 72.53 ± 5.20 | 70.81 ± 6.15 | 0.17 | N.A. |
| Height (m) | 1.73 ± 0.13 | 1.71± 0.15 | 0.51 | N.A. |
| BMI (kg/m2) | 24.25 ± 2.53 | 24.23 ± 2.40 | 0.95 | N.A. |
| Medical history | ||||
| CHD | 24 (31.58%) | 11 (34.37%) | 0.95 | 0.92 |
| Hypertension | 52 (68.42%) | 28 (87.50%) | 0.06 | 0.78 |
| Ischemic stroke | 9 (11.84%) | 3 (9.38%) | 0.97 | 1.26 |
| Diabetes mellitus | 12 (15.79%) | 7 (21.87%) | 0.63 | 0.72 |
| 1 Month Follow-Up | 3 Months Follow-Up | |||||
|---|---|---|---|---|---|---|
| CONUT < 3 (n = 76) | CONUT ≥ 3 (n = 32) | p Value | CONUT < 3 (n = 76) | CONUT ≥ 3 (n = 32) | p Value | |
| Biochemical profile | ||||||
| LDL cholesterol (mg/dL) | 87.22 ± 37.00 | 65.57 ± 12.95 | <0.001 | 65.94 ± 22.936 | 40.67 ± 15.670 | <0.001 |
| HDL cholesterol (mg/dL) | 48.33 ± 14.35 | 40.79 ± 13.56 | 0.06 | 55.25 ± 13.894 | 67.15 ± 26.733 | <0.001 |
| Triglycerides (mg/dL) | 151.54 ± 92.98 | 126.31 ± 82.95 | 0.17 | 131.53 ± 121.02 | 80.85 ± 60.97 | <0.001 |
| Fasting blood glucose (mg/dL) | 124.29 ± 39.22 | 154.96 ± 89.32 | 0.01 | 113.30 ± 21.01 | 124.67 ± 39.21 | 0.053 |
| Urea (mg/dL) | 42.12 ± 32.12 | 47.24 ± 37.42 | 0.50 | 37.58 ± 26.80 | 57.56 ± 37.35 | <0.001 |
| Creatinine (mg/dL) | 1.06 ± 0.40 | 1.10 ± 0.59 | 0.76 | 1.05 ± 0.47 | 1.19 ± 0.39 | 0.14 |
| AST (mg/dL) | 47.80 ± 63.00 | 43.83 ± 60.38 | 0.76 | 21.67 ± 11.33 | 18.04 ± 5.25 | 0.02 |
| ALT (mg/dL) | 45.14 ± 61.16 | 46.03 ± 62.80 | 0.94 | 44.84 ± 29.39 | 30.41 ± 12.65 | <0.001 |
| GGT (mg/dL) | 56.27 ± 31.65 | 64.00 ± 33.02 | 0.82 | 54.69 ± 48.19 | 39.67 ± 7.13 | 0.01 |
| Uric acid (mg/dL) | 5.69 ± 1.71 | 5.40 ± 2.17 | 0.53 | 5.27 ± 1.98 | 5.67 ± 2.13 | 0.40 |
| CK (U/L) | 371.31 ± 623.44 | 197.19 ± 252.45 | 0.08 | 157.37 ± 91.49 | 171.52 ± 99.92 | 0.50 |
| Cl− (mmol/L) | 103.26 ± 2.62 | 103.27 ± 1.34 | 0.98 | 101.14 ± 3.56 | 102.04 ± 3.65 | 0.27 |
| K+ (mmol/L) | 4.35 ± 0.43 | 4.34 ± 0.41 | 0.90 | 4.53 ± 0.50 | 4.59 ± 0.50 | 0.54 |
| Na+ (mmol/L) | 139.84 ± 2.81 | 139.29 ± 3.27 | 0.42 | 138.43 ± 2.42 | 137.19 ± 2.11 | 0.01 |
| Blood cell count | ||||||
| WBC (×103/mm3) | 10.25 ± 3.37 | 10.49 ± 4.80 | 0.80 | 8.27 ± 2.12 | 7.52 ± 0.70 | <0.001 |
| RBC (×106/mm3) | 4.61 ± 0.65 | 4.46 ± 0.65 | 0.29 | 4.91 ± 0.39 | 4.48 ± 0.97 | <0.001 |
| Hb (g/dL) | 14.34 ± 1.63 | 13.97 ± 2.35 | 0.42 | 14.90 ± 1.40 | 13.56 ± 2.70 | <0.001 |
| Hct (%) | 43.56 ± 8.10 | 41.33 ± 6.54 | 0.14 | 43.57 ± 4.22 | 40.59 ± 7.89 | 0.01 |
| PLT (×103/mm3) | 246.77 ± 65.05 | 271.34 ± 92.90 | 0.18 | 237.47 ± 55.92 | 245.78 ± 68.78 | 0.53 |
| Major CV Adverse Events | 1 Month Follow-Up | 3 Months Follow-Up | ||||
|---|---|---|---|---|---|---|
| CONUT < 3 (n = 76) | CONUT ≥ 3 (n = 32) | p Value | CONUT < 3 (n = 76) | CONUT ≥ 3 (n = 32) | p Value | |
| Number of patients presenting MACE | ||||||
| Total MACE (%) | 7 (9.2%) | 15 (46.9%) | <0.0001 | 8 (10.5%) | 22 (68.8%) | <0.0001 |
| Number of events | (n = 7) | (n = 31) | (n = 17) | (n = 38) | ||
| CV death (%) | 0 | 0 | N.A. | 1 | 3 | 0.04 |
| Non-fatal MI (%) | 7 | 12 | <0.001 | 5 | 9 | <0.001 |
| Resuscitated cardiac arrest (%) | 0 | 3 | 0.02 | 3 | 3 | 0.16 |
| Revascularization (%) | 0 | 3 | 0.02 | 0 | 4 | 0.003 |
| Ventricular arrhythmias (%) | 0 | 4 | 0.007 | 1 | 6 | <0.001 |
| AV blocks (%) | 0 | 9 | <0.001 | 4 | 9 | <0.001 |
| Ischemic troke (%) | 0 | 0 | N.A. | 3 | 4 | 0.06 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czinege, M.; Halațiu, V.-B.; Nyulas, V.; Cojocariu, L.-O.; Ion, B.; Mașca, V.; Țolescu, C.; Benedek, T. Nutritional Status and Recurrent Major Cardiovascular Events Following Acute Myocardial Infarction—A Follow-Up Study in a Primary Percutaneous Coronary Intervention Center. Nutrients 2024, 16, 1088. https://doi.org/10.3390/nu16071088
Czinege M, Halațiu V-B, Nyulas V, Cojocariu L-O, Ion B, Mașca V, Țolescu C, Benedek T. Nutritional Status and Recurrent Major Cardiovascular Events Following Acute Myocardial Infarction—A Follow-Up Study in a Primary Percutaneous Coronary Intervention Center. Nutrients. 2024; 16(7):1088. https://doi.org/10.3390/nu16071088
Chicago/Turabian StyleCzinege, Maria, Vasile-Bogdan Halațiu, Victoria Nyulas, Liliana-Oana Cojocariu, Bianca Ion, Violeta Mașca, Constantin Țolescu, and Theodora Benedek. 2024. "Nutritional Status and Recurrent Major Cardiovascular Events Following Acute Myocardial Infarction—A Follow-Up Study in a Primary Percutaneous Coronary Intervention Center" Nutrients 16, no. 7: 1088. https://doi.org/10.3390/nu16071088
APA StyleCzinege, M., Halațiu, V.-B., Nyulas, V., Cojocariu, L.-O., Ion, B., Mașca, V., Țolescu, C., & Benedek, T. (2024). Nutritional Status and Recurrent Major Cardiovascular Events Following Acute Myocardial Infarction—A Follow-Up Study in a Primary Percutaneous Coronary Intervention Center. Nutrients, 16(7), 1088. https://doi.org/10.3390/nu16071088







