Ultra-Processed Foods—Dietary Foe or Potential Ally?
Abstract
1. Introduction
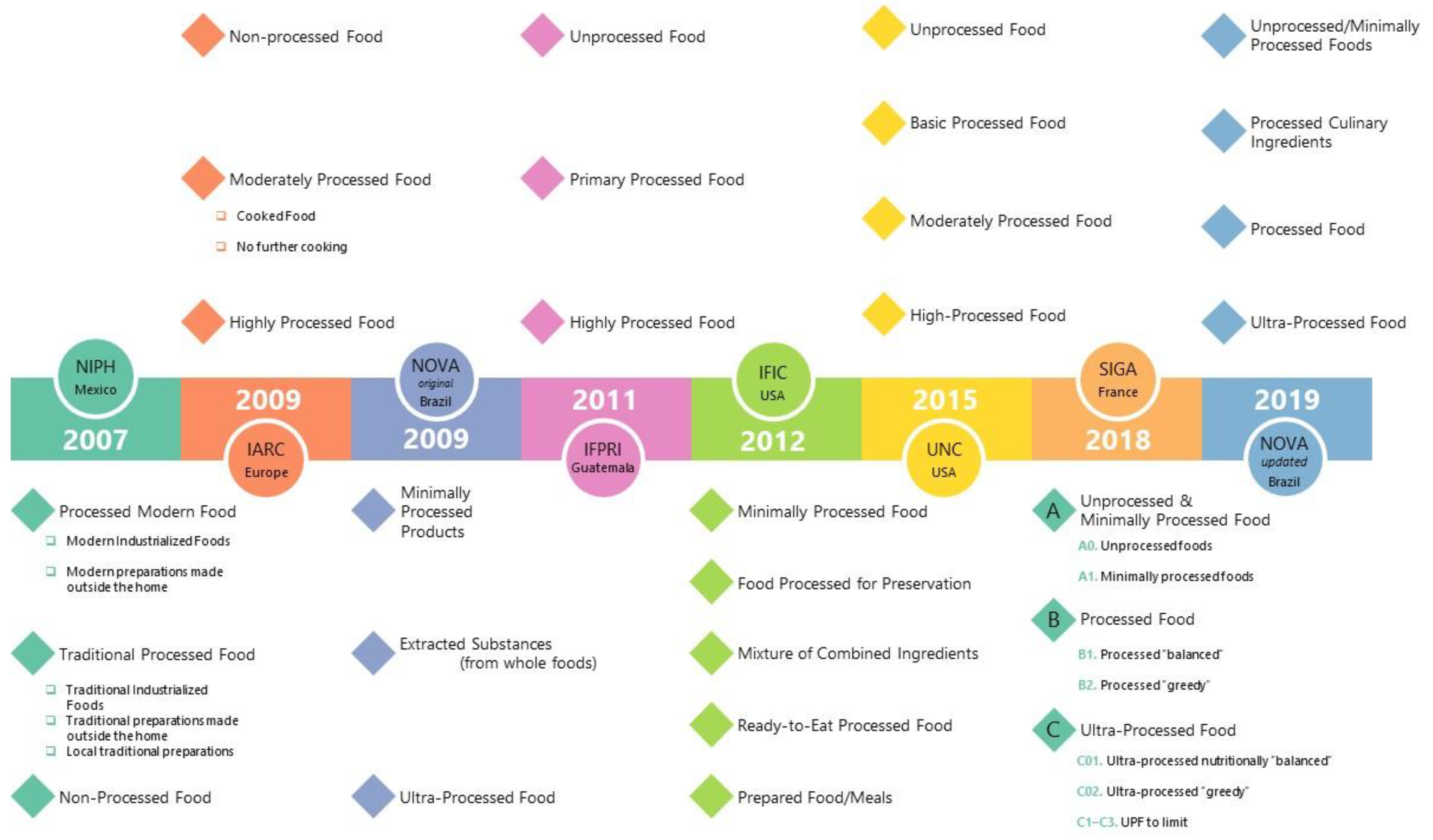
2. Food Classification Systems
3. The NOVA Classification System
4. Investigating Causality
- ❖
- Energy Balance. Over recent decades, numerous studies have found positive associations between UPF consumption and obesity risk [16,18,20,21,22,23]. In a prospective cohort study, Beslay et al. (2020) reported a positive correlation between UPF consumption and obesity [24]. Participants with a higher proportion of UPFs in their diet had a higher risk of obesity (hazard ratio (HR) = 1.09 [1.05–1.13], p < 0.001). In a randomized controlled trial conducted by Hall et al. (2019), individuals were presented with processed and unprocessed diets matched in calories, nutrients, and energy density, and the caloric intake was higher on the processed diet (UPF diet 508 ± 106 kcal/day higher, p = 0.0001), although there were limitations in the matching of food volume and fiber type and amount between groups [25,26]. A cross-sectional study by Monteiro et al. (2018) found that increased household availability of UPFs is positively associated with the prevalence of obesity, noting that with each percentage point increase in energy share of UPF products, there is potentially an increase of 0.25 percentage points in obesity prevalence [27]. In a Brazilian longitudinal study from 2008 to 2010 [23], Silva et al. (2018) observed higher BMIs in those who habitually consumed larger amounts of UPFs in their diets with those consuming the highest amount of UPFs having a mean BMI 0.80 kg/m2 higher (95% CI 0·53, 1·07) than individuals who consumed the least amount of UPFs in their diets. Thus, epidemiological evidence signals an association between increased UPF consumption and obesity, which is considered a gateway disease to other NCDs. However, using a machine learning algorithm to classify the degree of processing for many food products on the market, Menichetti et al. (2023) found positive associations between UPF consumption and NCD-related outcomes despite controlling for body mass index and caloric intake [17]. This suggests that positive energy balance may not be an obligatory driver of causality.
- ❖
- Nutrient Content. While early work on UPFs focused on their content of refined carbohydrates, saturated fats, and salt, this is no longer an obligatory attribute of UPFs. There are currently nutrient-dense UPFs on the market that refute the hypothesized linear relationship between nutritional value and processing techniques. Notably, a proof-of-concept study, conducted by Hess et al. (2023), illustrated a menu composed of 91% kcal from UPFs that complied with recommendations from the 2020 Dietary Guidelines for Americans and had a Healthy Eating Index-2015 score of 86 out of a possible 100 points [3]. This study demonstrates that UPF products that are nutritionally adequate exist, although whether or not they affect the risk of NCDs is not yet known. Relative to the role of poor nutritional status per se in NCD pathogenesis, the evidence is mixed, which weakens arguments that inadequate nutrient intake is a driver of NCD risk. Rather, poor nutritional status may serve as a biomarker that other causal processes are in play. It can be argued that the findings from Menichetti et al. (2023) support the biomarker hypothesis [17].
- ❖
- Food Processing and Non-Culinary Additives. Food processing techniques implicated in NCD risk include hydrogenation, extrusion, pre-frying and/or the addition of colorants, emulsifiers, and preservatives. It has been hypothesized that the way foods are “manufactured” relative to their capacity to alter the gut microbiome directly affects metabolic diseases through alterations in the immunity–inflammation axis [19]. The central argument is that UPFs are the actual drivers of the Western dietary pattern’s effect on NCDs. Food processing alterations fall into four categories that merit investigation: (1) consumption of refined macronutrients that are highly digestible, (2) effects of additives (emulsifiers and non-caloric artificial sweeteners), a proposition that has been challenged [28,29], (3) microbial products formed during food handling and processing before a food is consumed (although this can also be a problem, with minimally processed or home-processed foods that are the sources of many more cases of foodborne illness), and (4) novel chemicals formed in a food during processing, e.g., acrylamides and advanced glycation end products, which notably can also be formed during preparation of foods in the home environment.
5. UPF Trends
6. Moving Forward: Ban or Reformulate UPFs?
- ❖ Promote healthy eating and food environments according to “national circumstances”.
- ❖ Counteract the displacement of “fresh”/minimally processed foods by UPFs via preserving food systems, supporting family farmers, promoting healthy food preparation, and cooking in public institutions, such as schools.
- ❖ Create public health policies and market incentives to make unprocessed/minimally processed food more valued, available, and affordable.
- ❖ Create statutory regulatory measures for UPFs that have little nutritional value.
7. A Working Model to Guide Product Development and Consumer Choices
8. Limitations
9. Summary
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Martini, D.; Godos, J.; Bonaccio, M.; Vitaglione, P.; Grosso, G. Ultra-Processed Foods and Nutritional Dietary Profile: A Meta-Analysis of Nationally Representative Samples. Nutrients 2021, 13, 3390. [Google Scholar] [CrossRef] [PubMed]
- Temple, N.J. The Origins of the Obesity Epidemic in the USA-Lessons for Today. Nutrients 2022, 14, 4253. [Google Scholar] [CrossRef] [PubMed]
- Hess, J.M.; Comeau, M.E.; Casperson, S.; Slavin, J.L.; Johnson, G.H.; Messina, M.; Raatz, S.; Scheett, A.J.; Bodensteiner, A.; Palmer, D.G. Dietary Guidelines Meet NOVA: Developing a Menu for A Healthy Dietary Pattern Using Ultra-Processed Foods. J. Nutr. 2023, 153, 2472–2481. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Hawk, T.; Aggarwal, A.; Drewnowski, A. Characterizing Ultra-Processed Foods by Energy Density, Nutrient Density, and Cost. Front. Nutr. 2019, 6, 70. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Martínez Steele, E.; Du, M.; Pomeranz, J.L.; O'Connor, L.E.; Herrick, K.A.; Luo, H.; Zhang, X.; Mozaffarian, D.; Zhang, F.F. Trends in Consumption of Ultraprocessed Foods Among US Youths Aged 2–19 Years, 1999–2018. JAMA 2021, 326, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Martínez Steele, E.; Baraldi, L.G.; Louzada, M.L.; Moubarac, J.C.; Mozaffarian, D.; Monteiro, C.A. Ultra-processed foods and added sugars in the US diet: Evidence from a nationally representative cross-sectional study. BMJ Open 2016, 6, e009892. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025. Available online: http://www.dietaryguidelines.gov/ (accessed on 5 December 2023).
- de Araújo, T.P.; de Moraes, M.M.; Afonso, C.; Santos, C.; Rodrigues, S.S.P. Food Processing: Comparison of Different Food Classification Systems. Nutrients 2022, 14, 729. [Google Scholar] [CrossRef] [PubMed]
- Sadler, C.R.; Grassby, T.; Hart, K.; Raats, M.; Sokolovic, M.; Timotijevic, L. Processed food classification: Conceptualization and challenges. Trends Food Sci. Technol. 2021, 112, 149–162. [Google Scholar] [CrossRef]
- Martinez-Perez, C.; San-Cristobal, R.; Guallar-Castillon, P.; Martínez-González, M.; Salas-Salvadó, J.; Corella, D.; Castañer, O.; Martinez, J.A.; Alonso-Gómez, Á.; Wärnberg, J.; et al. Use of Different Food Classification Systems to Assess the Association between Ultra-Processed Food Consumption and Cardiometabolic Health in an Elderly Population with Metabolic Syndrome (PREDIMED-Plus Cohort). Nutrients 2021, 13, 2471. [Google Scholar] [CrossRef]
- Petrus, R.R.; Sobral, P.J.; Tadini, C.C.; Gonclaves, C.B. The NOVA classification system: A critical perspective in food science. Trends Food Sci. Technol. 2021, 116, 603–608. [Google Scholar] [CrossRef]
- Monteiro, C.A. Nutrition and health. The issue is not food, nor nutrients, so much as processing. Public Health Nutr. 2009, 12, 729–731. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.C.; Louzada, M.L.C.; Pereira-Machado, P. Ultra-processed Foods, Diet Quality, and Health Using the NOVA Classification System; Food and Agricultural Organization of the United Nations: Rome, Italy, 2019. [Google Scholar]
- Capozzi, F.; Magkos, F.; Fava, F.; Milani, G.P.; Agostoni, C.; Astrup, A.; Saguy, I.S. A Multidisciplinary Perspective of Ultra-Processed Foods and Associated Food Processing Technologies: A View of the Sustainable Road Ahead. Nutrients 2021, 13, 3948. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Steele, E.; Khandpur, N.; Batis, C.; Bes-Rastrollo, M.; Bonaccio, M.; Cediel, G.; Huybrechts, I.; Juul, F.; Levy, R.B.; da Costa Louzada, M.L.; et al. Best practices for applying the Nova food classification system. Nat. Food 2023, 4, 445–448. [Google Scholar] [CrossRef] [PubMed]
- Mambrini, S.P.; Menichetti, F.; Ravella, S.; Pellizzari, M.; De Amicis, R.; Foppiani, A.; Battezzati, A.; Bertoli, S.; Leone, A. Ultra-Processed Food Consumption and Incidence of Obesity and Cardiometabolic Risk Factors in Adults: A Systematic Review of Prospective Studies. Nutrients 2023, 15, 2583. [Google Scholar] [CrossRef] [PubMed]
- Menichetti, G.; Ravandi, B.; Mozaffarian, D.; Barabási, A.L. Machine learning prediction of the degree of food processing. Nat. Commun. 2023, 14, 2312. [Google Scholar] [CrossRef] [PubMed]
- Poti, J.M.; Braga, B.; Qin, B. Ultra-processed Food Intake and Obesity: What Really Matters for Health-Processing or Nutrient Content? Curr. Obes. Rep. 2017, 6, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Zinöcker, M.K.; Lindseth, I.A. The Western Diet-Microbiome-Host Interaction and Its Role in Metabolic Disease. Nutrients 2018, 10, 365. [Google Scholar] [CrossRef] [PubMed]
- Askari, M.; Heshmati, J.; Shahinfar, H.; Tripathi, N.; Daneshzad, E. Ultra-processed food and the risk of overweight and obesity: A systematic review and meta-analysis of observational studies. Int. J. Obes. 2020, 44, 2080–2091. [Google Scholar] [CrossRef] [PubMed]
- De Amicis, R.; Mambrini, S.P.; Pellizzari, M.; Foppiani, A.; Bertoli, S.; Battezzati, A.; Leone, A. Ultra-processed foods and obesity and adiposity parameters among children and adolescents: A systematic review. Eur. J. Nutr. 2022, 61, 2297–2311. [Google Scholar] [CrossRef]
- Moradi, S.; Entezari, M.H.; Mohammadi, H.; Jayedi, A.; Lazaridi, A.V.; Kermani, M.A.H.; Miraghajani, M. Ultra-processed food consumption and adult obesity risk: A systematic review and dose-response meta-analysis. Crit. Rev. Food Sci. Nutr. 2023, 63, 249–260. [Google Scholar] [CrossRef]
- Silva, F.M.; Giatti, L.; de Figueiredo, R.C.; Molina, M.D.C.B.; de Oliveira Cardoso, L.; Duncan, B.B.; Barreto, S.M. Consumption of ultra-processed food and obesity: Cross sectional results from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) cohort (2008-2010). Public Health Nutr. 2018, 21, 2271–2279. [Google Scholar] [CrossRef] [PubMed]
- Beslay, M.; Srour, B.; Méjean, C.; Allès, B.; Fiolet, T.; Debras, C.; Chazelas, E.; Deschasaux, M.; Wendeu-Foyet, M.G.; Hercberg, S.; et al. Ultra-processed food intake in association with BMI change and risk of overweight and obesity: A prospective analysis of the French NutriNet-Santé cohort. PLoS Med. 2020, 17, e1003256. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019, 30, 226. [Google Scholar] [CrossRef] [PubMed]
- Forde, C.G. Beyond ultra-processed: Considering the future role of food processing in human health. Proc. Nutr. Soc. 2023, 82, 406–418. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Moubarac, J.C.; Levy, R.B.; Canella, D.S.; Louzada, M.L.D.C.; Cannon, G. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr. 2018, 21, 18–26. [Google Scholar] [CrossRef] [PubMed]
- De Siena, M.; Raoul, P.; Costantini, L.; Scarpellini, E.; Cintoni, M.; Gasbarrini, A.; Rinninella, E.; Mele, M.C. Food Emulsifiers and Metabolic Syndrome: The Role of the Gut Microbiota. Foods 2022, 11, 2205. [Google Scholar] [CrossRef] [PubMed]
- Vo, T.D.; Lynch, B.S.; Roberts, A. Dietary Exposures to Common Emulsifiers and Their Impact on the Gut Microbiota: Is There a Cause for Concern? Compr. Rev. Food Sci. Food Saf. 2019, 18, 31–47. [Google Scholar] [CrossRef] [PubMed]
- Baraldi, L.G.; Martinez Steele, E.; Canella, D.S.; Monteiro, C.A. Consumption of ultra-processed foods and associated sociodemographic factors in the USA between 2007 and 2012: Evidence from a nationally representative cross-sectional study. BMJ Open 2018, 8, e020574. [Google Scholar] [CrossRef] [PubMed]
- Marino, M.; Puppo, F.; Del Bo', C.; Vinelli, V.; Riso, P.; Porrini, M.; Martini, D. A Systematic Review of Worldwide Consumption of Ultra-Processed Foods: Findings and Criticisms. Nutrients 2021, 13, 2778. [Google Scholar] [CrossRef]
- Tobias, D.K.; Hall, K.D. Eliminate or reformulate ultra-processed foods? Biological mechanisms matter. Cell Metab. 2021, 33, 2314–2315. [Google Scholar] [CrossRef]
- Juul, F.; Parekh, N.; Martinez-Steele, E.; Monteiro, C.A.; Chang, V.W. Ultra-processed food consumption among US adults from 2001 to 2018. Am. J. Clin. Nutr. 2022, 115, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Keum, N.; Giovannucci, E.; Fadnes, L.T.; Boffetta, P.; Greenwood, D.C.; Tonstad, S.; Vatten, L.J.; Riboli, E.; Norat, T. Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: Systematic review and dose-response meta-analysis of prospective studies. BMJ 2016, 353, i2716. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.G. Evaluation of the evidence between consumption of refined grains and health outcomes. Nutr. Rev. 2012, 70, 80–99. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Bogensberger, B.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2018, 118, 74–100. [Google Scholar] [CrossRef] [PubMed]
- Ong, A.D.; Uchino, B.N.; Wethington, E. Loneliness and Health in Older Adults: A Mini-Review and Synthesis. Gerontology 2016, 62, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Shan, Z.; Rehm, C.D.; Rogers, G.; Ruan, M.; Wang, D.D.; Hu, F.B.; Mozaffarian, D.; Zhang, F.F.; Bhupathiraju, S.N. Trends in Dietary Carbohydrate, Protein, and Fat Intake and Diet Quality Among US Adults, 1999-2016. JAMA 2019, 322, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Scrinis, G.; Monteiro, C.A. Ultra-processed foods and the limits of product reformulation. Public Health Nutr. 2018, 21, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.; Hofman, K.; Moubarac, J.C.; Thow, A.M. Public health response to ultra-processed food and drinks. BMJ 2020, 369, m2391. [Google Scholar] [CrossRef] [PubMed]
- Milley, M.A.; Forrest Faison, C., III; Dana, M.G.; O’keefe, G.B.; Ediger, M.A. (Eds.) Nutrition and Menu Standards for Human Performance Optimization. Departments of the Army: Washington, DC, USA, 2017; pp. 1–25. [Google Scholar]
- Sotelo-Díaz, I.; Blanco-Lizarazo, C.M. A systematic review of the nutritional implications of military rations. Nutr. Health 2019, 25, 153–161. [Google Scholar] [CrossRef]
- McClung, H.L.; Armstrong, N.J.; Hennigar, S.R.; Staab, J.S.; Montain, S.J.; Karl, J.P. Randomized Trial Comparing Consumption of Military Rations to Usual Intake for 21 Consecutive Days: Nutrient Adequacy and Indicators of Health Status. J. Acad. Nutr. Diet. 2020, 120, 1791–1804. [Google Scholar] [CrossRef]
- Dixon, A. MRE Production for 2014 Does Away With Lasagna, Refried Beans, and Fajitas. NCO J. 2013. [Google Scholar]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nees, S.; Lutsiv, T.; Thompson, H.J. Ultra-Processed Foods—Dietary Foe or Potential Ally? Nutrients 2024, 16, 1013. https://doi.org/10.3390/nu16071013
Nees S, Lutsiv T, Thompson HJ. Ultra-Processed Foods—Dietary Foe or Potential Ally? Nutrients. 2024; 16(7):1013. https://doi.org/10.3390/nu16071013
Chicago/Turabian StyleNees, Sabrina, Tymofiy Lutsiv, and Henry J. Thompson. 2024. "Ultra-Processed Foods—Dietary Foe or Potential Ally?" Nutrients 16, no. 7: 1013. https://doi.org/10.3390/nu16071013
APA StyleNees, S., Lutsiv, T., & Thompson, H. J. (2024). Ultra-Processed Foods—Dietary Foe or Potential Ally? Nutrients, 16(7), 1013. https://doi.org/10.3390/nu16071013






