Association of Sociodemographic, Socioeconomic and Lifestyle Characteristics with Low Protein and Energy Intake in the Healthy Swiss Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Calculation Protein and Energy Intake Classification
2.3. Sociodemographic Factors
2.4. Socioeconomic Factors
2.5. Lifestyle Factors
2.6. Weighting Strategy
2.7. Statistical Analysis
3. Results
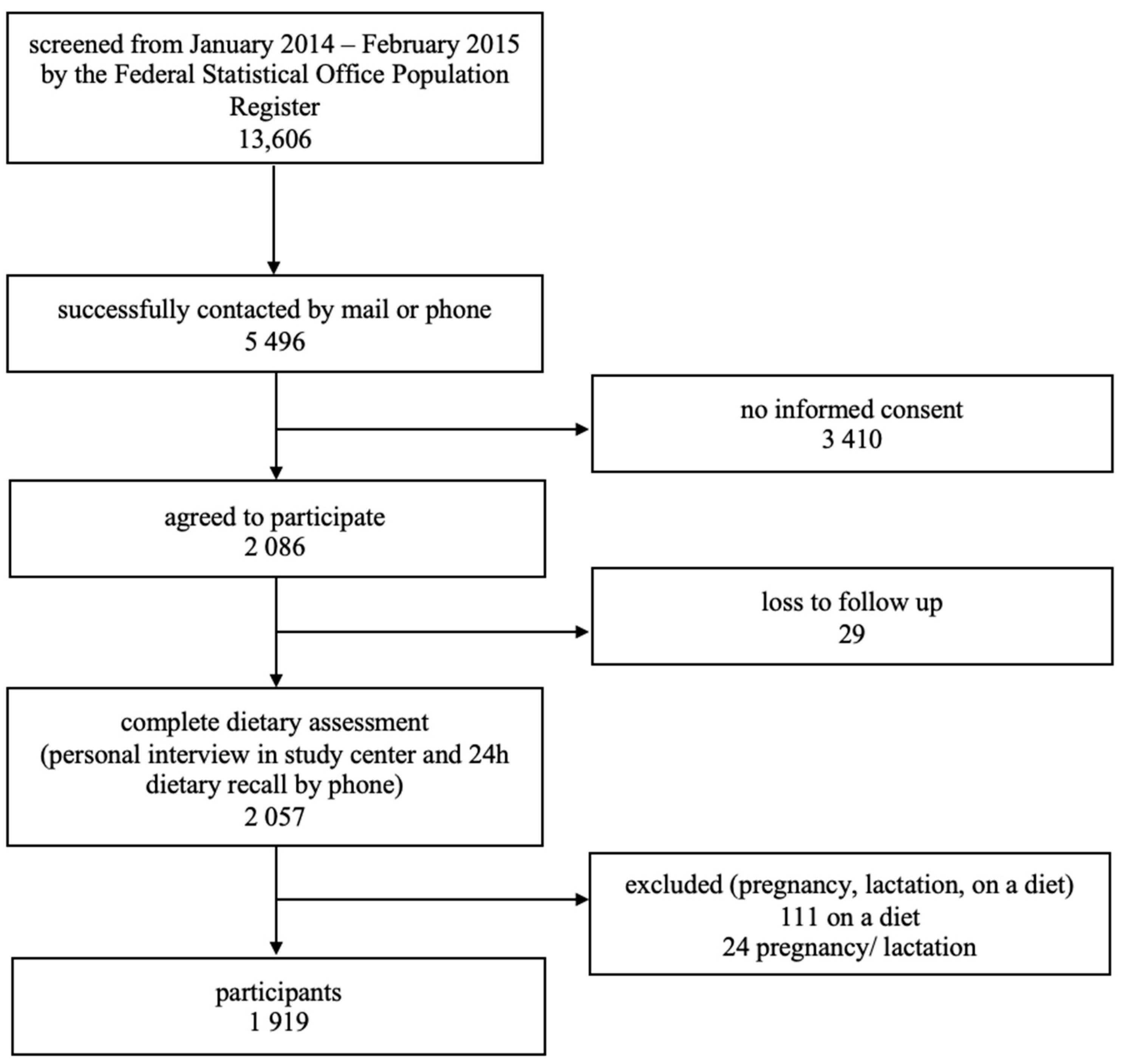
3.1. Recruitment
3.2. Population Characteristics
3.3. Predictors of Energy Intake below Resting Metabolic Rate (RMR)
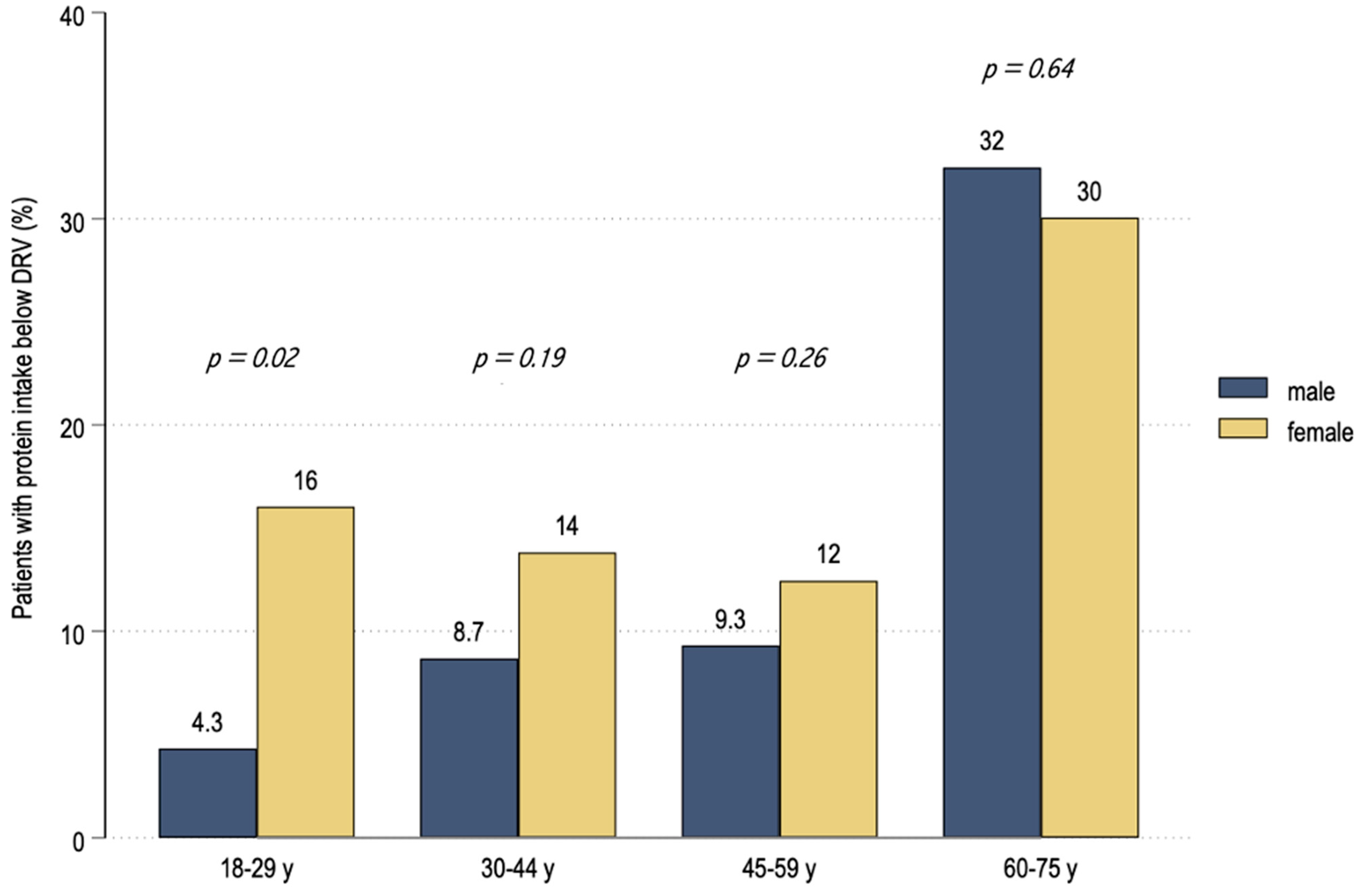
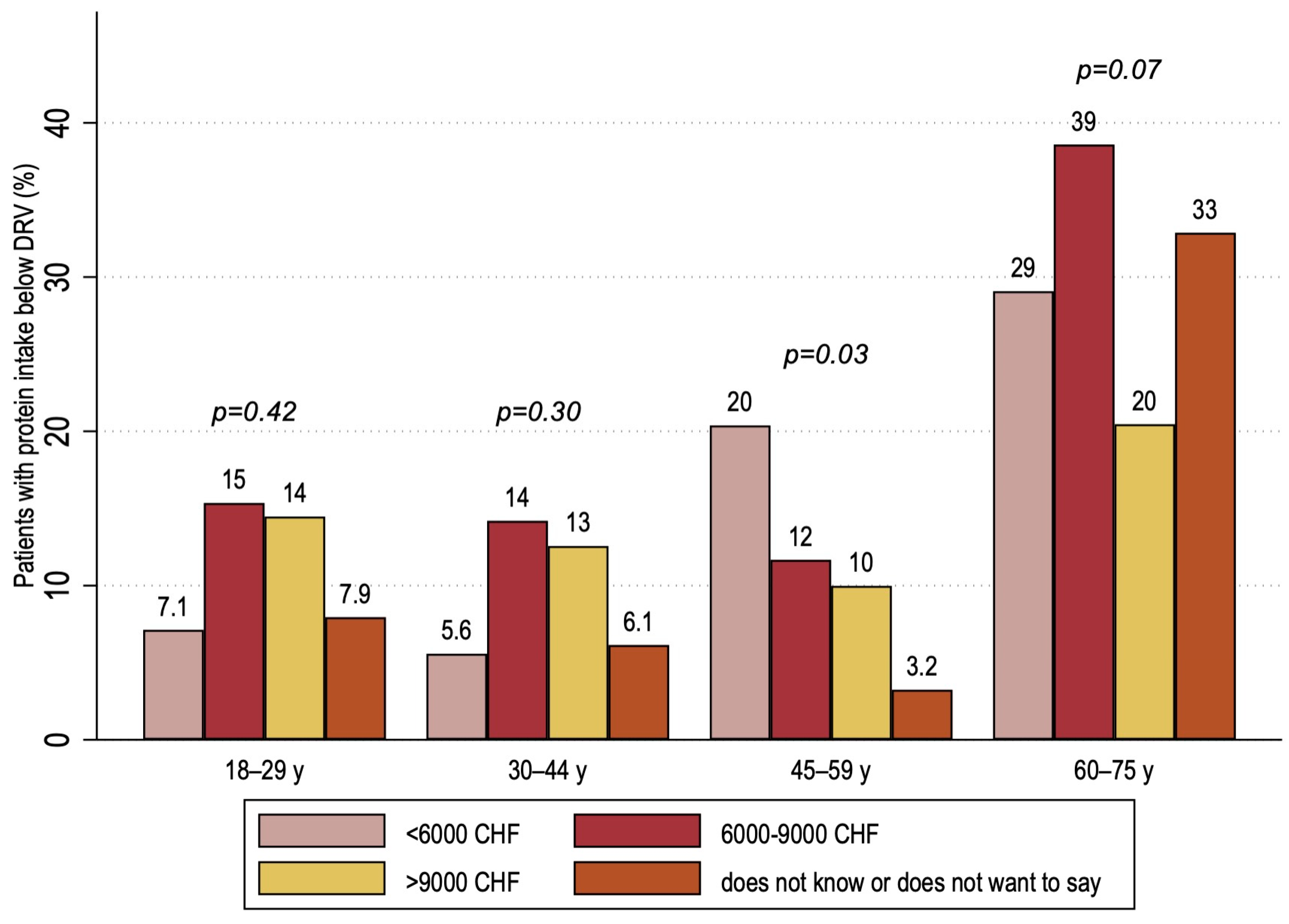
3.4. Predictors for Not Meeting Protein Dietary Reference Values (DRV)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Society, G.N. Referenzwerte fur die Nahrstoffzufuhr/Reference Values for Nutrient Intake 2017. Available online: https://www.dge.de/wissenschaft/referenzwerte/?L=0 (accessed on 16 September 2022).
- World Health Organization. Healthy Diet. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 16 September 2022).
- Phillips, J.A. Dietary Guidelines for Americans, 2020–2025. Workplace Health Saf. 2021, 69, 395. [Google Scholar] [CrossRef] [PubMed]
- European Food Safety Authority. 2022. Available online: https://www.efsa.europa.eu/en/topics/topic/dietary-reference-values (accessed on 16 September 2022).
- Dr. Bucher Della Torre Sophie DJCC. Project “Nutritional Reference Values (NRVs) for Switzerland”. Federal Food Safety and Veterinary Office FSVO Contract No 0714001567. June 2021. Available online: https://www.blv.admin.ch/dam/blv/de/dokumente/lebensmittel-und-ernaehrung/ernaehrung/nutri-score/bericht-naehrwertreferenzwerte-schweiz.pdf.download.pdf/Full%20report_NRV_HEdS_final.pdf (accessed on 16 September 2022).
- Schuetz, P.; Seres, D.; Lobo, D.N.; Gomes, F.; Kaegi-Braun, N.; Stanga, Z. Management of disease-related malnutrition for patients being treated in hospital. Lancet 2021, 398, 1927–1938. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Hanna, K.L.; Collins, P.F. Relationship between living alone and food and nutrient intake. Nutr. Rev. 2015, 73, 594–611. [Google Scholar] [CrossRef] [PubMed]
- Dumartheray, E.W.; Krieg, M.A.; Cornuz, J.; Whittamore, D.R.; Lanham-New, S.A.; Burckhardt, P. Energy and nutrient intake of Swiss women aged 75–87 years. J. Hum. Nutr. Diet. 2006, 19, 431–435. [Google Scholar] [CrossRef]
- Marques-Vidal, P.; Rousi, E.; Paccaud, F.; Gaspoz, J.M.; Theler, J.M.; Bochud, M.; Stringhini, S.; Guessous, I. Dietary Intake according to Gender and Education: A Twenty-Year Trend in a Swiss Adult Population. Nutrients 2015, 7, 9558–9572. [Google Scholar] [CrossRef]
- Si Hassen, W.; Castetbon, K.; Cardon, P.; Enaux, C.; Nicolaou, M.; Lien, N.; Terragni, L.; Holdsworth, M.; Stronks, K.; Hercberg, S.; et al. Socioeconomic Indicators Are Independently Associated with Nutrient Intake in French Adults: A DEDIPAC Study. Nutrients 2016, 8, 158. [Google Scholar] [CrossRef]
- van Rossum, C.T.; van de Mheen, H.; Witteman, J.C.; Grobbee, E.; Mackenbach, J.P. Education and nutrient intake in Dutch elderly people. The Rotterdam Study. Eur. J. Clin. Nutr. 2000, 54, 159–165. [Google Scholar] [CrossRef]
- Chatelan, A.; Marques-Vidal, P.; Bucher, S.; Siegenthaler, S.; Metzger, N.; Zuberbühler, C.A.; Camenzind-Frey, E.; Reggli, A.; Bochud, M.; Beer-Borst, S. Lessons Learnt about Conducting a Multilingual Nutrition Survey in Switzerland: Results from menuCH Pilot Survey. Int. J. Vitam. Nutr. Res. 2017, 87, 25–36. [Google Scholar] [CrossRef]
- Switzerland-National Nutrition Survey menuCH 2014–2015. Center for Primary Care and Public Health (Unisanté), University of Lausanne, Switzerland (Unisanté), Swiss Federal Food Safety and Veterinary Office (FSVO). 1 September 2022. Available online: https://https://menuch.unisante.ch/index.php/catalog/4 (accessed on 18 September 2022).
- Mifflin, M.D.; St Jeor, S.T.; Hill, L.A.; Scott, B.J.; Daugherty, S.A.; Koh, Y.O. A new predictive equation for resting energy expenditure in healthy individuals. Am. J. Clin. Nutr. 1990, 51, 241–247. [Google Scholar] [CrossRef]
- Deutsche Gesellschaft für Ernährung; Österreichische Gesellschaft für Ernährung. Schweizerische Gesellschaft für Ernährung, Hrsg. Referenzwerte für die Nährstoffzufuhr, 2nd ed.; Deutsche Gesellschaft für Ernährung: Bonn, Germany, 2019. [Google Scholar]
- Babor, T.F.; Higgins-Biddle, J.C. Brief Intervention for Hazardous and Harmful Drinking: A Manual for Use in Primary Care; World Health Organizaton Department of Mental Health and Substance Abuse: Geneva, Switzerland, 2001; p. 52. [Google Scholar]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sport. Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Hagströmer, M.; Oja, P.; Sjöström, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, J.; Chatelan, A.; Bochud, M. Weighting Strategy; Institute of Social and Preventitive Medicine: Lausanne, Switzerland, 2017. [Google Scholar]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the PROT-AGE Study Group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef] [PubMed]
- Tieland, M.; Borgonjen-Van den Berg, K.J.; Van Loon, L.J.; de Groot, L.C. Dietary Protein Intake in Dutch Elderly People: A Focus on Protein Sources. Nutrients 2015, 7, 9697–9706. [Google Scholar] [CrossRef]
- Tieland, M.; Borgonjen-Van den Berg, K.J.; van Loon, L.J.; de Groot, L.C. Dietary protein intake in community-dwelling, frail, and institutionalized elderly people: Scope for improvement. Eur. J. Nutr. 2012, 51, 173–179. [Google Scholar] [CrossRef]
- Pirlich, M.; Schütz, T.; Kemps, M.; Luhman, N.; Minko, N.; Lübke, H.J.; Rossnagel, K.; Willich, S.N.; Lochs, H. Social risk factors for hospital malnutrition. Nutrition 2005, 21, 295–300. [Google Scholar] [CrossRef]
- Hone, M.; Nugent, A.P.; Walton, J.; McNulty, B.A.; Egan, B. Habitual protein intake, protein distribution patterns and dietary sources in Irish adults with stratification by sex and age. J. Hum. Nutr. Diet. 2020, 33, 465–476. [Google Scholar] [CrossRef]
- Houston, D.K.; Nicklas, B.J.; Ding, J.; Harris, T.B.; Tylavsky, F.A.; Newman, A.B.; Lee, J.S.; Sahyoun, N.R.; Visser, M.; Kritchevsky, S.B. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: The Health, Aging, and Body Composition (Health ABC) Study. Am. J. Clin. Nutr. 2008, 87, 150–155. [Google Scholar] [CrossRef]
- Tschanz, L.; Kaelin, I.; Wróbel, A.; Rohrmann, S.; Sych, J. Characterisation of meat consumption across socio-demographic, lifestyle and anthropometric groups in Switzerland: Results from the National Nutrition Survey menuCH. Public Health Nutr. 2022, 25, 3096–3106. [Google Scholar] [CrossRef]
- Steinbach, L.; Rohrmann, S.; Kaelin, I.; Krieger, J.P.; Pestoni, G.; Herter-Aeberli, I.; Faeh, D.; Sych, J. No-meat eaters are less likely to be overweight or obese, but take dietary supplements more often: Results from the Swiss National Nutrition survey menuCH. Public Health Nutr. 2021, 24, 4156–4165. [Google Scholar] [CrossRef]
- van Vliet, S.; Burd, N.A.; van Loon, L.J. The Skeletal Muscle Anabolic Response to Plant- versus Animal-Based Protein Consumption. J. Nutr. 2015, 145, 1981–1991. [Google Scholar] [CrossRef] [PubMed]
- Gorissen, S.H.M.; Witard, O.C. Characterising the muscle anabolic potential of dairy, meat and plant-based protein sources in older adults. Proc. Nutr. Soc. 2018, 77, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Traversy, G.; Chaput, J.P. Alcohol Consumption and Obesity: An Update. Curr. Obes. Rep. 2015, 4, 122–130. [Google Scholar] [CrossRef]
- Cancello, R.; Soranna, D.; Brunani, A.; Scacchi, M.; Tagliaferri, A.; Mai, S.; Marzullo, P.; Zambon, A.; Invitti, C. Analysis of Predictive Equations for Estimating Resting Energy Expenditure in a Large Cohort of Morbidly Obese Patients. Front. Endocrinol. 2018, 9, 367. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.; Leung, S.S.; Ho, S.C.; Sham, A.; Lam, T.H.; Janus, E.D. Influence of educational level and marital status on dietary intake, obesity and other cardiovascular risk factors in a Hong Kong Chinese population. Eur. J. Clin. Nutr. 1999, 53, 461–467. [Google Scholar] [CrossRef]
- Haste, F.M.; Brooke, O.G.; Anderson, H.R.; Bland, J.M.; Peacock, J.L. Social determinants of nutrient intake in smokers and non-smokers during pregnancy. J. Epidemiol. Community Health 1990, 44, 205–209. [Google Scholar] [CrossRef]
- Pearson, J.M.; Schlettwein-Gsell, D.; van Staveren, W.; de Groot, L. Living alone does not adversely affect nutrient intake and nutritional status of 70- to 75-year-old men and women in small towns across Europe. Int. J. Food Sci. Nutr. 1998, 49, 131–139. [Google Scholar] [CrossRef]
- Lee, K.W.; Shin, D. Comparison of Dietary Behaviors and the Prevalence of Metabolic Syndrome in Single- and Multi-Person Households among Korean Adults. Healthcare 2021, 9, 1116. [Google Scholar] [CrossRef]
- Alkerwi, A.; Baydarlioglu, B.; Sauvageot, N.; Stranges, S.; Lemmens, P.; Shivappa, N.; Hébert, J.R. Smoking status is inversely associated with overall diet quality: Findings from the ORISCAV-LUX study. Clin. Nutr. 2017, 36, 1275–1282. [Google Scholar] [CrossRef]
- Dallongeville, J.; Marécaux, N.; Fruchart, J.C.; Amouyel, P. Cigarette smoking is associated with unhealthy patterns of nutrient intake: A meta-analysis. J. Nutr. 1998, 128, 1450–1457. [Google Scholar] [CrossRef]
- Dyer, A.R.; Elliott, P.; Stamler, J.; Chan, Q.; Ueshima, H.; Zhou, B.F. Dietary intake in male and female smokers, ex-smokers, and never smokers: The INTERMAP study. J. Hum. Hypertens. 2003, 17, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.R.; Hatsukami, D.K. Effects of three doses of transdermal nicotine on post-cessation eating, hunger and weight. J. Subst. Abus. 1997, 9, 151–159. [Google Scholar] [CrossRef]
- Pestoni, G.; Krieger, J.P.; Sych, J.M.; Faeh, D.; Rohrmann, S. Cultural Differences in Diet and Determinants of Diet Quality in Switzerland: Results from the National Nutrition Survey menuCH. Nutrients 2019, 11, 126. [Google Scholar] [CrossRef] [PubMed]
- Inanir, D.; Kaelin, I.; Pestoni, G.; Faeh, D.; Mueller, N.; Rohrmann, S.; Sych, J. Daily and meal-based assessment of dairy and corresponding protein intake in Switzerland: Results from the National Nutrition Survey menuCH. Eur. J. Nutr. 2021, 60, 2099–2109. [Google Scholar] [CrossRef] [PubMed]
- Friel, S.; Kelleher, C.C.; Nolan, G.; Harrington, J. Social diversity of Irish adults nutritional intake. Eur. J. Clin. Nutr. 2003, 57, 865–875. [Google Scholar] [CrossRef]
- Crispim, S.P.; de Vries, J.H.; Geelen, A.; Souverein, O.W.; Hulshof, P.J.; Lafay, L.; Rousseau, A.S.; Lillegaard, I.T.; Andersen, L.F.; Huybrechts, I.; et al. Two non-consecutive 24 h recalls using EPIC-Soft software are sufficiently valid for comparing protein and potassium intake between five European centres--results from the European Food Consumption Validation (EFCOVAL) study. Br. J. Nutr. 2011, 105, 447–458. [Google Scholar] [CrossRef]
- Chatelan, A.; Beer-Borst, S.; Randriamiharisoa, A.; Pasquier, J.; Blanco, J.M.; Siegenthaler, S.; Paccaud, F.; Slimani, N.; Nicolas, G.; Camenzind-Frey, E.; et al. Major Differences in Diet across Three Linguistic Regions of Switzerland: Results from the First National Nutrition Survey menuCH. Nutrients 2017, 9, 1163. [Google Scholar] [CrossRef]
- SwissVeg. Available online: https://www.swissveg.ch/2021_10_Anzahl_Veganer_Vegetarier?language=de (accessed on 16 September 2022).
- Langsetmo, L.; Harrison, S.; Jonnalagadda, S.; Pereira, S.L.; Shikany, J.M.; Farsijani, S.; Lane, N.E.; Cauley, J.A.; Stone, K.; Cawthon, P.M. Low Protein Intake Irrespective of Source is Associated with Higher Mortality among Older Community-dwelling Men. J. Nutr. Health Aging 2020, 24, 900–905. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Marzetti, E.; Picca, A.; Cesari, M.; Uchida, M.C.; Calvani, R. Protein Intake and Frailty: A Matter of Quantity, Quality, and Timing. Nutrients 2020, 12, 2915. [Google Scholar] [CrossRef]
| Total | |
|---|---|
| N = 1919 | |
| Mean Intake | |
| Protein | 1.22 g/kgBW |
| Energy | 2183 kcal |
| Sociodemographic factors | |
| Age | |
| 18–29 years | 374 (19.5%) |
| 30–44 years | 470 (24.5%) |
| 45–59 years | 596 (31.1%) |
| 60–75 years | 479 (25.0%) |
| Sex | |
| Male | 900 (46.9%) |
| Female | 1019 (53.1%) |
| Nationality | |
| Non-Swiss | 244 (12.7%) |
| Swiss | 1675 (87.3%) |
| Language Region | |
| German speaking | 1249 (65.1%) |
| French Speaking | 473 (24.6%) |
| Italian Speaking | 197 (10.3%) |
| Household Type | |
| Without Children | 1214 (63.3%) |
| With Children | 702 (36.6%) |
| Missing | 3 (0.2%) |
| Marital Status | |
| Not married | 868 (45.2%) |
| Married | 1048 (54.6%) |
| Missing | 3 (0.2%) |
| Socioeconomic factors | |
| Education, Highest Degree | |
| Primary | 81 (4.2%) |
| Secondary | 904 (47.1%) |
| Tertiary | 931 (48.5%) |
| Missing | 3 (0.2%) |
| Gross Household Income | |
| <6000 CHF/month | 328 (17.1%) |
| 6000–9000 CHF/month | 391 (20.4%) |
| >9000 CHF/month | 662 (34.5%) |
| Does not know/refuses to say | 224 (11.7%) |
| Missing | 314 (16.4%) |
| Lifestyle factors | |
| BMI | |
| <18.5 kg/m2 | 50 (2.6%) |
| 18.5–24 kg/m2 | 1063 (55.4%) |
| 25–29 kg/m2 | 579 (30.2%) |
| 30–34 kg/m2 | 172 (9.0%) |
| 35–39 kg/m2 | 40 (2.1%) |
| >45 kg/m2 | 9 (0.5%) |
| Missing | 6 (0.3%) |
| Self-Reported Physical Activity | |
| Low | 736 (38.4%) |
| Moderate | 585 (30.5%) |
| High | 551 (28.7%) |
| Missing | 47 (2.4%) |
| Smoking Status | |
| Never | 856 (44.6%) |
| Former | 639 (33.3%) |
| Current | 420 (21.9%) |
| Missing | 4 (0.2%) |
| Alcohol Consumption | |
| No or low alcohol consumption | 525 (27.4%) |
| Higher consumption | 1394 (72.6%) |
| Meat Consumption | |
| Yes | 1881 (98.0%) |
| No | 38 (2.0%) |
| Eating Habits | |
| ≤4 meals outside home | 1010 (52.6%) |
| >4 meals outside home | 909 (47.4%) |
| Energy Intake above RMR | Energy Intake below RMR | |||
|---|---|---|---|---|
| N = 1709 | N = 210 | |||
| Sociodemographic factors | ||||
| OR univariate (95% CI), p-value | OR multivariate (95% CI, p-value | |||
| Age | ||||
| 18–29 years | 335 (19.6%) | 39 (18.6%) | reference | |
| 30–44 years | 411 (24.0%) | 59 (28.1%) | 0.87 (0.5 to 1.51), p = 0.611 | 0.76 (0.37–1.56), p = 0.453 |
| 45–59 years | 530 (31.0%) | 66 (31.4%) | 0.93 (0.54 to 1.61), p = 0.799 | 0.78 (0.39–1.55), p = 0.483 |
| 60–75 years | 433 (25.3%) | 46 (21.9%) | 0.92 (0.49 to 1.7), p = 0.784 | 0.65 (0.27–1.58), p = 0.339 |
| Sex | ||||
| Male | 794 (46.5%) | 106 (50.5%) | reference | |
| Female | 915 (53.5%) | 104 (49.5%) | 0.73 (0.5 to 1.05), p = 0.087 | 1.26 (0.81–1.97), p = 0.306 |
| Nationality | ||||
| Non-Swiss | 211 (12.3%) | 33 (15.7%) | reference | |
| Swiss | 1498 (87.7%) | 177 (84.3%) | 0.68 (0.42 to 1.09), p = 0.109 | 0.66 (0.38–1.14), p = 0.137 |
| Language Region | ||||
| German speaking | 1134 (66.4%) | 115 (54.8%) | reference | |
| French Speaking | 416 (24.3%) | 57 (27.1%) | 1.17 (0.78 to 1.76), p = 0.444 | 1.16 (0.72–1.87), p = 0.551 |
| Italian Speaking | 159 (9.3%) | 38 (18.1%) | 1.89 (1.18 to 3.03), p = 0.008 | 1.42 (0.79–2.56), p = 0.242 |
| Household Type | ||||
| Without Children | 1095 (64.1%) | 119 (56.7%) | reference | |
| With Children | 612 (35.8%) | 90 (42.9%) | 1.2 (0.82 to 1.75), p = 0.353 | 1.41 (0.89–2.24), p = 0.147 |
| Marital Status | ||||
| Not married | 775 (45.3%) | 93 (44.3%) | reference | |
| Married | 932 (54.5%) | 116 (55.2%) | 0.86 (0.59 to 1.25), p = 0.433 | 1.04 (0.61–1.75), p = 0.896 |
| Socioeconomic factors | ||||
| Education, Highest Degree | ||||
| Primary | 66 (3.9%) | 15 (7.1%) | reference | |
| Secondary | 795 (46.5%) | 109 (51.9%) | 0.52 (0.23 to 1.16), p = 0.109 | 0.79 (0.35–1.79), p = 0.575 |
| Tertiary | 846 (49.5%) | 85 (40.5%) | 0.43 (0.19 to 0.97), p = 0.041 | 0.85 (0.37–1.96), p = 0.704 |
| Gross Household Income | ||||
| <6000 CHF/month | 292 (17.1%) | 36 (17.1%) | reference | |
| 6000–9000 CHF/month | 351 (20.5%) | 40 (19.0%) | 0.84 (0.46 to 1.56), p = 0.586 | 0.79 (0.41–1.51), p = 0.471 |
| >9000 CHF/month | 602 (35.2%) | 60 (28.6%) | 0.54 (0.31 to 0.92), p = 0.025 | 0.49 (0.26–0.94), p = 0.032 |
| Does not know/refuses to say | 195 (11.4%) | 29 (13.8%) | 1.17 (0.61 to 2.27), p = 0.632 | 1.37 (0.67–2.8), p = 0.384 |
| Lifestyle factors | ||||
| BMI | ||||
| <18.5 kg/m2 | 48 (2.8%) | 2 (1.0%) | 0.62 (0.11–3.55), p = 0.588 | 0.61 (0.1–3.69), p = 0.589 |
| 18.5–24 kg/m2 | 999 (58.5%) | 64 (30.5%) | reference | reference |
| 25–29 kg/m2 | 493 (28.8%) | 86 (41.0%) | 2.61 (1.66–4.12), p < 0.001 | 4.62 (2.82–7.56), p < 0.001 |
| ≥30 kg/m2 | 169 (9.9%) | 58 (27.6%) | 4.89 (2.94–8.12), p < 0.001 | 6.55 (3.77–11.38), p < 0.001 |
| Self-Reported Physical Activity | ||||
| Not meeting WHO recommendations | 675 (39.5%) | 89 (42.4%) | reference | |
| Meeting WHO recommendations | 1018 (59.6%) | 119 (56.7%) | 0.83 (0.57 to 1.22), p = 0.343 | 0.76 (0.5–1.15), p = 0.196 |
| Smoking Status | ||||
| Never or former | 776 (45.4%) | 80 (38.1%) | reference | |
| Current | 930 (54.4%) | 129 (61.4%) | 1.33 (0.91 to 1.96), p = 0.144 | 1.47 (0.95–2.26), p = 0.083 |
| Alcohol Consumption | ||||
| No or low alcohol consumption | 452 (26.4%) | 73 (34.8%) | reference | |
| Higher consumption | 1257 (73.6%) | 137 (65.2%) | 0.69 (0.47 to 1.02), p = 0.06 | 0.61 (0.38–0.97), p = 0.037 |
| Meat Consumption | ||||
| no | 35 (2.0%) | 3 (1.4%) | reference | |
| yes | 1674 (98.0%) | 207 (98.6%) | 2.37 (0.69 to 8.09), p = 0.17 | 3.85 (0.46–32.49), p = 0.216 |
| Eating Habits | ||||
| ≤4 meals outside home | 892 (52.2%) | 118 (56.2%) | reference | |
| >4 meals outside home | 817 (47.8%) | 92 (43.8%) | 0.91 (0.63 to 1.32), p = 0.63 | 1.13 (0.67–1.89), p = 0.653 |
| Protein Intake above DRV | Protein Intake below DRV | |||
|---|---|---|---|---|
| N = 1597 | N = 322 | |||
| Sociodemographic factors | ||||
| OR univariate (95% CI), p-value | OR multivariate (95% CI, p-value | |||
| Age | ||||
| 18–29 years | 335 (21.0%) | 39 (12.1%) | reference | |
| 30–44 years | 409 (25.6%) | 61 (18.9%) | 1.09 (0.63–1.89), p = 0.76 | 0.88 (0.48–1.59), p = 0.668 |
| 45–59 years | 519 (32.5%) | 77 (23.9%) | 1.03 (0.62–1.71), p = 0.9 | 0.83 (0.47–1.47), p = 0.519 |
| 60–75 years | 334 (20.9%) | 145 (45.0%) | 3.91 (2.42–6.31), p < 0.001 | 2.94 (1.57–5.52), p = 0.001 |
| Sex | ||||
| Male | 773 (48.4%) | 127 (39.4%) | reference | |
| Female | 824 (51.6%) | 195 (60.6%) | 1.32 (0.97–1.8), p = 0.08 | 1.73 (1.15–2.6), p = 0.008 |
| Nationality | ||||
| Non-Swiss | 220 (13.8%) | 24 (7.5%) | reference | |
| Swiss | 1377 (86.2%) | 298 (92.5%) | 1.63 (0.98–2.71), p = 0.06 | 1.23 (0.72–2.12), p = 0.45 |
| Language Region | ||||
| German speaking | 1036 (64.9%) | 213 (66.1%) | reference | |
| French Speaking | 396 (24.8%) | 77 (23.9%) | 0.95 (0.68–1.32), p = 0.741 | 1.01 (0.68–1.51), p = 0.948 |
| Italian Speaking | 165 (10.3%) | 32 (9.9%) | 0.99 (0.59–1.67), p = 0.982 | 1.04 (0.51–2.13), p = 0.917 |
| Household Type | ||||
| Without Children | 990 (62.0%) | 224 (69.6%) | reference | |
| With Children | 605 (37.9%) | 97 (30.1%) | 0.57 (0.41–0.78), p < 0.001 | 0.94 (0.62–1.43), p = 0.776 |
| Marital Status | ||||
| Not married | 735 (46.0%) | 133 (41.3%) | reference | |
| Married | 860 (53.9%) | 188 (58.4%) | 1.03 (0.76–1.4), p = 0.83 | 1.07 (0.69–1.67), p = 0.753 |
| Socioeconomic factors | ||||
| Education, Highest Degree | ||||
| Primary | 67 (4.2%) | 14 (4.3%) | reference | |
| Secondary | 737 (46.1%) | 167 (51.9%) | 1.19 (0.59–2.42), p = 0.629 | 1.18 (0.55–2.52), p = 0.667 |
| Tertiary | 791 (49.5%) | 140 (43.5%) | 1.11 (0.54–2.28), p = 0.769 | 1.27 (0.6–2.71), p = 0.53 |
| Gross Household Income | ||||
| <6000 CHF/month | 270 (16.9%) | 58 (18.0%) | reference | |
| 6000–9000 CHF/month | 311 (19.5%) | 80 (24.8%) | 1.29 (0.81–2.06), p = 0.286 | 1.35 (0.8–2.28), p = 0.267 |
| >9000 CHF/month | 565 (35.4%) | 97 (30.1%) | 0.76 (0.49–1.17), p = 0.207 | 1.02 (0.59–1.75), p = 0.939 |
| Does not know/refuses to say | 194 (12.1%) | 30 (9.3%) | 0.59 (0.34–1.05), p = 0.071 | 0.8 (0.43–1.48), p = 0.477 |
| Lifestyle factors | ||||
| BMI | ||||
| <18.5 kg/m2 | 46 (2.9%) | 4 (1.2%) | 0.21 (0.07–0.61), p = 0.004 | 0.11 (0.02–0.53), p = 0.006 |
| 18.5–24 kg/m2 | 923 (57.8%) | 140 (43.5%) | reference | reference |
| 25–29 kg/m2 | 450 (28.2%) | 129 (40.1%) | 1.76 (1.25–2.46), p = 0.001 | 1.88 (1.23–2.89), p = 0.004 |
| ≥30 kg/m2 | 178 (11.1%) | 49 (15.2%) | 1.57 (1.02–2.42), p = 0.041 | 1.38 (0.83–2.3), p = 0.22 |
| Self-Reported Physical Activity | ||||
| Not meeting WHO recommendations | 636 (39.8%) | 128 (39.8%) | reference | |
| Meeting WHO recommendations | 945 (59.2%) | 192 (59.6%) | 1.13 (0.83–1.54), p = 0.43 | 1.01 (0.72–1.42), p = 0.937 |
| Smoking Status | ||||
| Never or former | 713 (44.6%) | 143 (44.4%) | reference | |
| Current | 881 (55.2%) | 178 (55.3%) | 0.86 (0.63–1.16), p = 0.323 | 0.91 (0.64–1.29), p = 0.583 |
| Alcohol Consumption | ||||
| No or low alcohol consumption | 420 (26.3%) | 105 (32.6%) | reference | |
| Higher consumption | 1177 (73.7%) | 217 (67.4%) | 0.74 (0.54–1.02), p = 0.07 | 0.63 (0.42–0.93), p = 0.019 |
| Meat Consumption | ||||
| no | 23 (1.4%) | 15 (4.7%) | reference | |
| yes | 1574 (98.6%) | 307 (95.3%) | 0.27 (0.11–0.64), p < 0.001 | 0.23 (0.1–0.53), p = 0.001 |
| Eating habits | ||||
| ≤4 meals outside home | 797 (49.9%) | 213 (66.1%) | reference | |
| >4 meals outside home | 800 (50.1%) | 109 (33.9%) | 0.53 (0.39–0.73), p < 0.001 | 0.95 (0.63–1.43), p = 0.802 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wimmer, R.; Audétat, A.; Binggeli, J.; Schuetz, P.; Kaegi-Braun, N. Association of Sociodemographic, Socioeconomic and Lifestyle Characteristics with Low Protein and Energy Intake in the Healthy Swiss Population. Nutrients 2023, 15, 2200. https://doi.org/10.3390/nu15092200
Wimmer R, Audétat A, Binggeli J, Schuetz P, Kaegi-Braun N. Association of Sociodemographic, Socioeconomic and Lifestyle Characteristics with Low Protein and Energy Intake in the Healthy Swiss Population. Nutrients. 2023; 15(9):2200. https://doi.org/10.3390/nu15092200
Chicago/Turabian StyleWimmer, Roxana, Andrea Audétat, Julia Binggeli, Philipp Schuetz, and Nina Kaegi-Braun. 2023. "Association of Sociodemographic, Socioeconomic and Lifestyle Characteristics with Low Protein and Energy Intake in the Healthy Swiss Population" Nutrients 15, no. 9: 2200. https://doi.org/10.3390/nu15092200
APA StyleWimmer, R., Audétat, A., Binggeli, J., Schuetz, P., & Kaegi-Braun, N. (2023). Association of Sociodemographic, Socioeconomic and Lifestyle Characteristics with Low Protein and Energy Intake in the Healthy Swiss Population. Nutrients, 15(9), 2200. https://doi.org/10.3390/nu15092200






