Waist-to-Height Ratio Is a Stronger Mediator in the Association between DASH Diet and Hypertension: Potential Micro/Macro Nutrients Intake Pathways
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Demographic, DASH Diet, Anthropometric Measurements and Nutrients Assessment
2.3. Hypertension
2.4. Statistical Analysis
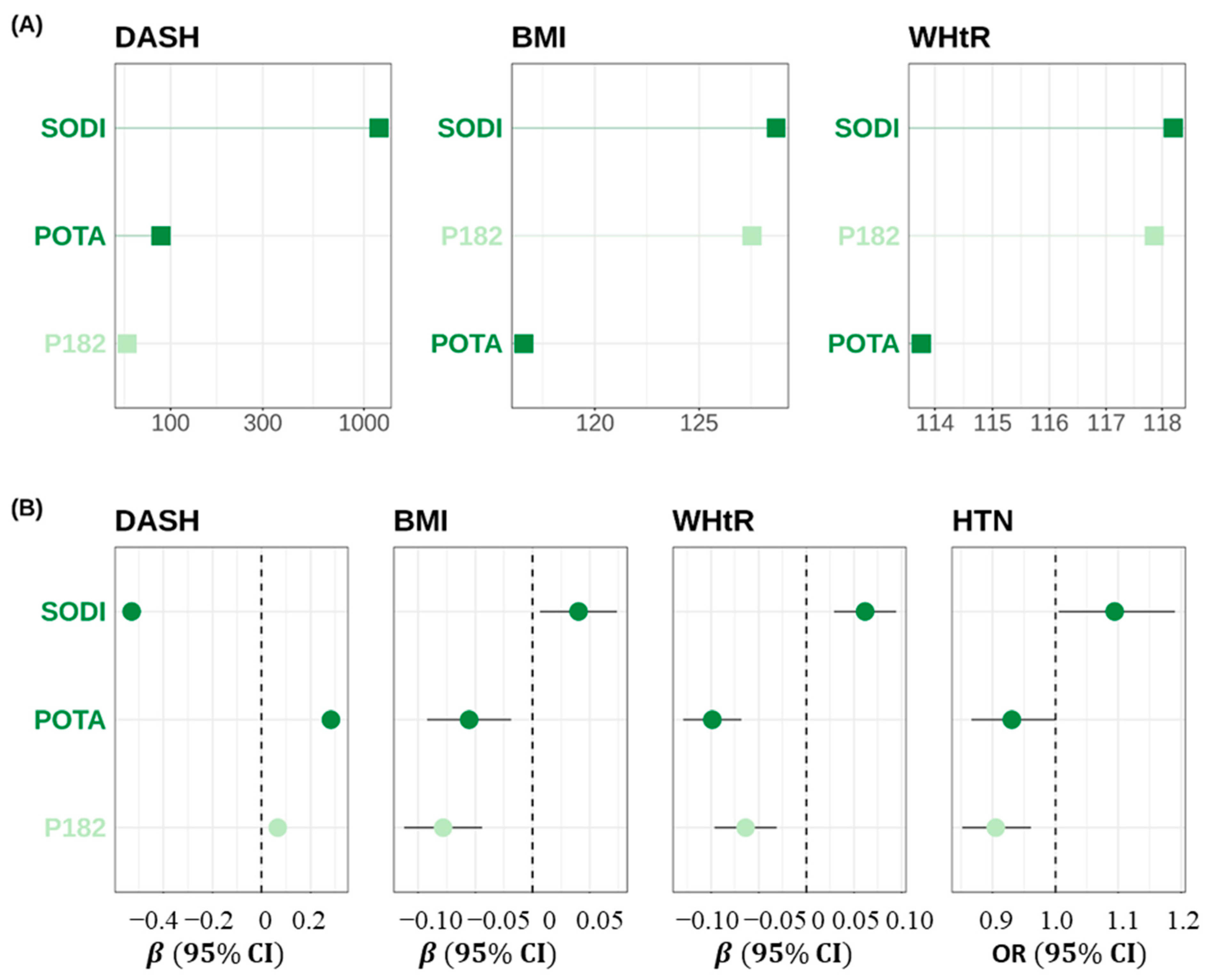
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Gibbs, J.; Gaskin, E.; Ji, C.; Miller, M.A.; Cappuccio, F.P. The effect of plant-based dietary patterns on blood pressure: A systematic review and meta-analysis of controlled intervention trials. J. Hypertens. 2021, 39, 23–37. [Google Scholar] [CrossRef]
- Unwin, D.J.; Tobin, S.D.; Murray, S.W.; Delon, C.; Brady, A.J. Substantial and sustained improvements in blood pressure, weight and lipid profiles from a carbohydrate restricted diet: An observational study of insulin resistant patients in primary care. Int. J. Environ. Res. Public Health 2019, 16, 2680. [Google Scholar] [CrossRef] [PubMed]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef]
- Filippou, C.D.; Tsioufis, C.P.; Thomopoulos, C.G.; Mihas, C.C.; Dimitriadis, K.S.; Sotiropoulou, L.I.; Chrysochoou, C.A.; Nihoyannopoulos, P.I.; Tousoulis, D.M. Dietary approaches to stop hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Adv. Nutr. 2020, 11, 1150–1160. [Google Scholar] [CrossRef]
- Abiodun, O.A.; Jagun, O.A.; Olu-Abiodun, O.O.; Sotunsa, J.O. Correlation between Body mass index, Waist Hip ratio, blood sugar levels and blood pressure in apparently healthy adult Nigerians. IOSR J. Dent. Med. Sci. 2014, 13, 56–61. [Google Scholar] [CrossRef]
- Omisore, A.G.; Omisore, B.; Abioye-Kuteyi, E.A.; Bello, I.S.; Olowookere, S.A. In-school adolescents’weight status and blood pressure profile in South-western Nigeria: Urban-rural comparison. BMC Obes. 2018, 5, 2. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Sun, M.; Su, Y.; Li, M.; Ma, S.; Zhang, Y.; Zhang, A.; Cai, S.; Cheng, B.; Bao, Q.; et al. Mediation effect of central obesity on the association between the Dietary Approaches to Stop Hypertension diet and hypertension. J. Hum. Hypertens. 2020, 34, 631–639. [Google Scholar]
- Duncan, P.R.; Howe, L.D.; Manukusa, Z.; Purdy, S. Determinants of obesity and perception of weight in hypertensive patients in rural South Africa. S. Afr. J. Clin. Nutr. 2014, 27, 56–62. [Google Scholar] [CrossRef]
- Gajalakshmi, V.; Lacey, B.; Kanimozhi, V.; Sherliker, P.; Peto, R.; Lewington, S. Body-mass index, blood pressure, and cause-specific mortality in India: A prospective cohort study of 500810 adults. Lancet Glob. Health. 2018, 6, e787–e794. [Google Scholar] [CrossRef] [PubMed]
- Maffeis, C.; Banzato, C.; Talamini, G.; Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J. Pediatr. 2008, 152, 207–213. [Google Scholar] [CrossRef]
- Wang, Y.; Rimm, E.B.; Stampfer, M.J.; Willett, W.C.; Hu, F.B. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am. J. Clin. Nutr. 2005, 81, 555–563. [Google Scholar] [CrossRef]
- Feng, R.N.; Zhao, C.; Wang, C.; Niu, Y.C.; Li, K.; Guo, F.C.; Li, S.T.; Sun, C.H.; Li, Y. BMI is strongly associated with hypertension, and waist circumference is strongly associated with type 2 diabetes and dyslipidemia, in northern Chinese adults. J. Epidemiol. 2012, 22, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Zhang, D.; Guo, C.; Zhou, Q.; Tian, G.; Liu, D.; Chen, X.; Liu, L.; Liu, F.; Cheng, C.; et al. Association of hypertriglyceridemia waist-to-height ratio and its dynamic status with incident hypertension: The Rural Chinese Cohort Study. J. Hypertens. 2019, 37, 2354–2360. [Google Scholar] [CrossRef]
- Soltani, S.; Shirani, F.; Chitsazi, M.J.; Salehi-Abargouei, A. The effect of dietary approaches to stop hypertension (DASH) diet on weight and body composition in adults: A systematic review and meta-analysis of randomized controlled clinical trials. Obes. Rev. 2016, 17, 442–454. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008. Available online: http://www.health.gov/PAGuidelines (accessed on 20 October 2022).
- Fung, T.; Chiuve, S.; McCullough, M.; Rexrode, K.; Hu, F. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar]
- Louca, P.; Nogal, A.; Mompeo, O.; Christofidou, P.; Gibson, R.; Spector, T.D.; Berry, S.E.; Valdes, A.M.; Mangino, M.; Menni, C. Body mass index mediates the effect of the DASH diet on hypertension: Common metabolites underlying the association. J. Hum. Nutr. Diet. 2022, 35, 214–222. [Google Scholar] [CrossRef]
- D’Elia, L.; Barba, G.; Cappuccio, F.P. Sodium intake and hypertension. Nat. Rev. Nephrol. 2011, 8, 219–227. [Google Scholar]
- Appel, L.J.; Brands, M.W.; Daniels, S.R.; Karanja, N.; Elmer, P.J.; Sacks, F.M. Dietary Approaches to Prevent and Treat Hypertension: A Scientific Statement from the American Heart Association. Hypertension 2006, 47, 296–308. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Fahimi, S.; Singh, G.M.; Micha, R.; Khatibzadeh, S.; Engell, R.E.; Lim, S.; Danaei, G.; Ezzati, M.; Powles, J.; et al. Global sodium consumption and death from cardiovascular causes. N. Engl. J. Med. 2014, 371, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhang, Q. Potassium intake and obesity: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2021, 60, 1637–1649. [Google Scholar]
- Golpour-Hamedani, S.; Rafie, N.; Pourmasoumi, M.; Morteza Safavi, S.; Mohammadifard, N. Sodium and potassium intakes and adiposity among Iranian pre-adolescents and adolescents: A cross-sectional study. Nutr. J. 2022, 21, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, H.J. Association between potassium intake and waist-to-height ratio in Korean adults: A cross-sectional study. Nutrients 2021, 13, 1026. [Google Scholar]
- Vaidya, A.; Underwood, P.C.; Hopkins, P.N.; Jeunemaitre, X.; Ferri, C.; Williams, G.H.; Adler, G.K. Abnormal aldosterone physiology and cardiometabolic risk factors. Hypertension 2020, 75, 1063–1072. [Google Scholar] [CrossRef]
- Mente, A.; O’Donnell, M.; Rangarajan, S.; McQueen, M.; Dagenais, G.; Wielgosz, A.; Lear, S.; Ah, S.T.L.; Wei, L.; Diaz, R.; et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: A community-level prospective epidemiological cohort study. Lancet 2019, 393, 183–191. [Google Scholar] [CrossRef]
- Smith, J.K.; Doe, J.H. Omega-3 fatty acid supplementation and body weight: A systematic review and meta-analysis of randomized controlled trials. J. Nutr. 2016, 146, 516–521. [Google Scholar]

| Hypertension Stages | ||||
|---|---|---|---|---|
| Normal (5234) | HTN Stage 1 (1681) | HTN Stage 2 (1309) | p | |
| Categorical Variables, Number (%) | ||||
| Gender | <0.001 | |||
| Male | 2631 (50) | 1043 (62) | 781 (60) | |
| Female | 2603 (50) | 638 (38) | 528 (40) | |
| Education | <0.001 | |||
| <High school | 764 (15) | 283 (17) | 272 (21) | |
| High school | 2800 (53) | 926 (55) | 729 (56) | |
| College and above | 1670 (32) | 472 (28) | 308 (24) | |
| Race/Ethnic | <0.001 | |||
| Hispanic | 1227 (23) | 363 (22) | 251 (19) | |
| None-Hispanic White | 2323 (44) | 730 (43) | 526 (40) | |
| None-Hispanic Black | 944 (18) | 380 (23) | 400 (31) | |
| Other | 740 (14) | 208 (12) | 132 (10) | |
| Marital Status | 0.4 | |||
| Married | 3074 (59) | 1017 (60) | 764 (58) | |
| Live alone | 2160 (41) | 664 (40) | 545 (42) | |
| Smoking Status | <0.001 | |||
| Never | 2895 (55) | 828 (49) | 601 (46) | |
| Former | 1136 (22) | 456 (27) | 397 (30) | |
| Current | 1203 (23) | 397 (24) | 311 (24) | |
| Alcohol Assumption | <0.001 | |||
| ≤4 drinks/day | 1823 (35) | 694 (41) | 561 (43) | |
| >4 drinks/day | 3411 (65) | 987 (59) | 748 (57) | |
| Physical Activity | 0.2 | |||
| <10 min/week | 2114 (40) | 680 (40) | 580 (44) | |
| 10 min~149 min/week | 1086 (21) | 353 (21) | 253 (19) | |
| 150 min~299 min/week | 416 (7.9) | 134 (8.0) | 111 (8.5) | |
| ≥300 min/week | 1618 (31) | 514 (31) | 365 (28) | |
| DASH score | 0.027 | |||
| Good (DASH score >= 30) | 1205 (23) | 335 (20) | 285 (22) | |
| Poor (DASH score < 30) | 4029 (77) | 1346 (80) | 1024 (78) | |
| Continuous Variable, Median (IQR) | ||||
| Age, year | 40 (29, 54) | 50 (37, 62) | 59 (47, 69) | <0.001 |
| Poverty Income Ratio (PIR) | 2.46 (1.21, 4.63) | 2.55 (1.23, 4.67) | 2.14 (1.13, 3.92) | <0.001 |
| Systolic blood pressure (SBP) | 114 (107, 120) | 131 (125, 135) | 147 (142, 157) | <0.001 |
| Diastolic blood pressure (DBP) | 68 (62, 73) | 80 (71, 84) | 82 (70, 91) | <0.001 |
| Body Mass Index (BMI) | 27 (24, 32) | 29 (25, 34) | 30 (25, 34) | <0.001 |
| Waist-to-height Ratio (WHtR) | 0.13 (0.11, 0.15) | 0.14 (0.12, 0.16) | 0.15 (0.13, 0.17) | <0.001 |
| Weight (WT) | 77 (66, 91) | 83 (72, 99) | 85 (69, 100) | <0.001 |
| WAIST | 21.3 (18.7, 24.5) | 23.5 (20.8, 26.6) | 23.9 (21.0, 27.5) | <0.001 |
| DASH Effect on Mediator (Path a: X->M) | Multiple Mediator Model (Path b: M->HTN) | |||||||
|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||||
| Mediator | Beta | Lower | Upper | p | Beta | Lower | Upper | p |
| BMI | −0.116 | −0.139 | −0.093 | <0.001 | 0.018 | −0.008 | 0.045 | 0.178 |
| WHtR | −0.141 | −0.163 | −0.118 | <0.001 | 0.058 | 0.031 | 0.086 | <0.001 |
| Indirect effect (Path ab: DASH->M->HTN) | % Mediated (ab/c) | Total effect (Path c: DASH->HTN) | ||||||
| 95% CI | Multiple mediation model | 95% CI | ||||||
| Mediator | Beta | Lower | Upper | Beta | Lower | Upper | p | |
| BMI | −0.002 | −0.006 | 0.001 | 9.09% | −0.023 | −0.032 | −0.012 | <0.001 |
| WHtR | −0.008 | −0.012 | −0.004 | 36.36% | Direct effect | |||
| (Path c’: DASH->M->HTN) | ||||||||
| 95% CI | ||||||||
| Total | −0.010 | −0.018 | −0.003 | 45.45% | Beta | Lower | Upper | p |
| −0.013 | −0.024 | −0.002 | 0.025 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuan, M.; Li, Q.; Yang, C.; Zhi, L.; Zhuang, W.; Xu, X.S.; Tao, F. Waist-to-Height Ratio Is a Stronger Mediator in the Association between DASH Diet and Hypertension: Potential Micro/Macro Nutrients Intake Pathways. Nutrients 2023, 15, 2189. https://doi.org/10.3390/nu15092189
Yuan M, Li Q, Yang C, Zhi L, Zhuang W, Xu XS, Tao F. Waist-to-Height Ratio Is a Stronger Mediator in the Association between DASH Diet and Hypertension: Potential Micro/Macro Nutrients Intake Pathways. Nutrients. 2023; 15(9):2189. https://doi.org/10.3390/nu15092189
Chicago/Turabian StyleYuan, Min, Qi Li, Can Yang, Liping Zhi, Weiwei Zhuang, Xu Steven Xu, and Fangbiao Tao. 2023. "Waist-to-Height Ratio Is a Stronger Mediator in the Association between DASH Diet and Hypertension: Potential Micro/Macro Nutrients Intake Pathways" Nutrients 15, no. 9: 2189. https://doi.org/10.3390/nu15092189
APA StyleYuan, M., Li, Q., Yang, C., Zhi, L., Zhuang, W., Xu, X. S., & Tao, F. (2023). Waist-to-Height Ratio Is a Stronger Mediator in the Association between DASH Diet and Hypertension: Potential Micro/Macro Nutrients Intake Pathways. Nutrients, 15(9), 2189. https://doi.org/10.3390/nu15092189






