The Influence of Relative Reinforcing Value of Food, Sensitization, Energy Intake and Diet Quality on zBMI Change over Two Years in Adolescents: A Longitudinal Cohort Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
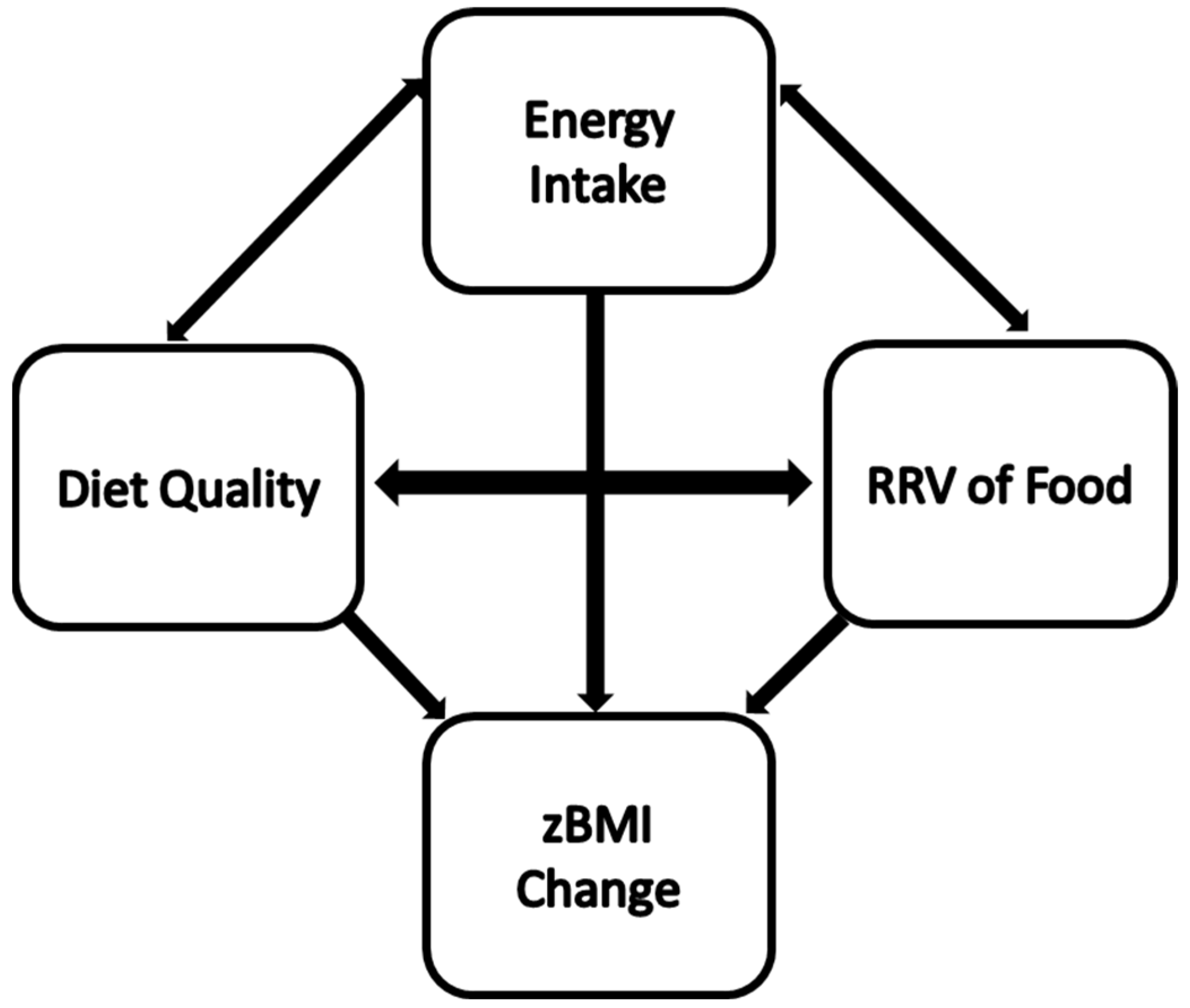
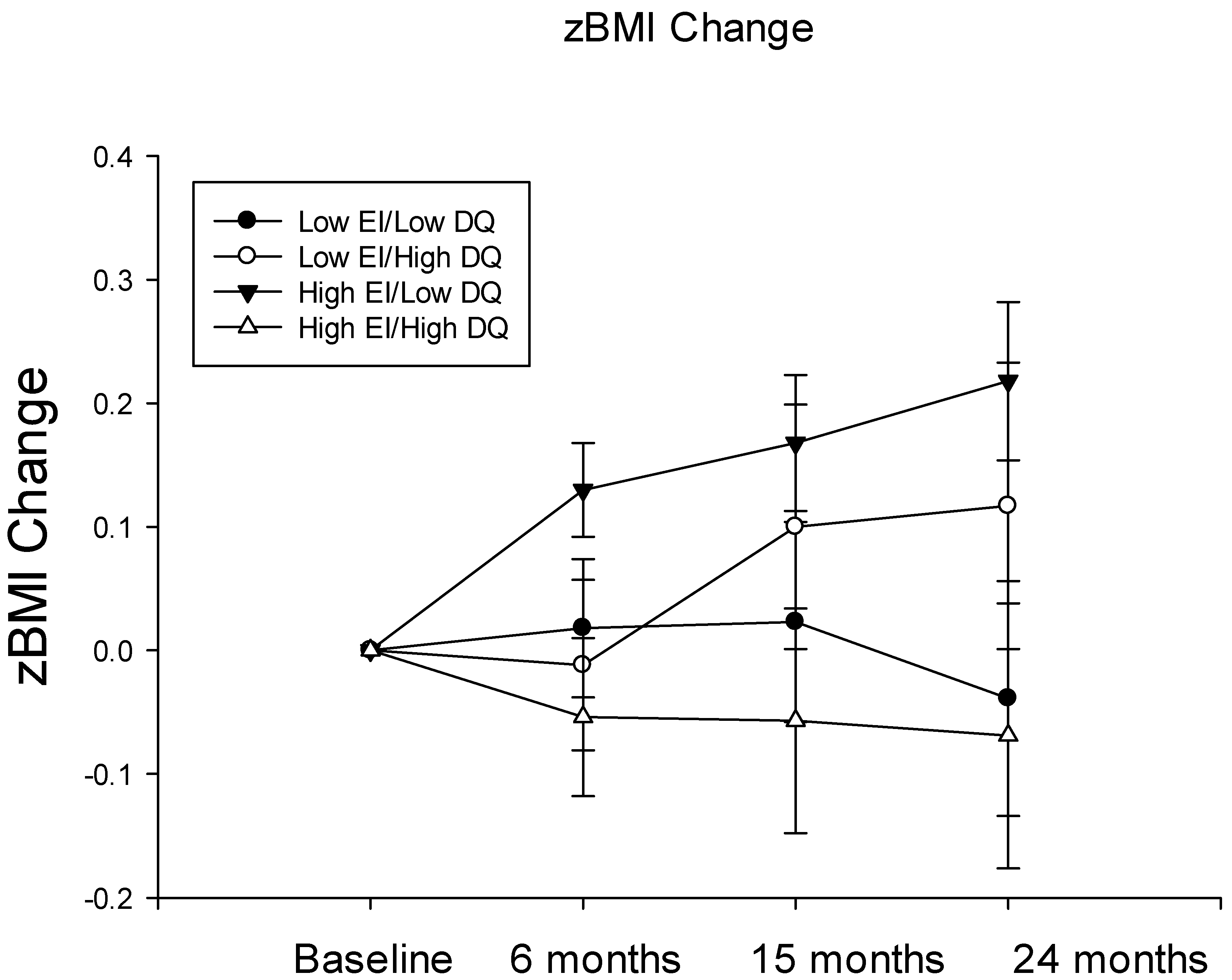
Hypothesis Testing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Epstein, L.H.; Lin, H.; Carr, K.A.; Fletcher, K.D. Food reinforcement and obesity. Psychological moderators. Appetite 2012, 58, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; Temple, J.L.; Neaderhiser, B.J.; Salis, R.J.; Erbe, R.W.; Leddy, J.J. Food reinforcement, the dopamine D2 receptor genotype, and energy intake in obese and nonobese humans. Behav. Neurosci. 2007, 121, 877–886. [Google Scholar] [CrossRef]
- Epstein, L.H.; Leddy, J.J. Food reinforcement. Appetite 2006, 46, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Goldfield, G.S.; Epstein, L.H.; Davidson, M.; Saad, F. Validation of a questionnaire measure of the relative reinforcing value of food. Eat. Behav. 2005, 6, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Clark, E.N.; Dewey, A.M.; Temple, J.L. Effects of daily snack food intake on food reinforcement depend on body mass index and energy density. Am. J. Clin. Nutr. 2010, 91, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L.; Bulkley, A.M.; Badawy, R.L.; Krause, N.; McCann, S.; Epstein, L.H. Differential effects of daily snack food intake on the reinforcing value of food in obese and nonobese women. Am. J. Clin. Nutr. 2009, 90, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L.; Chappel, A.; Shalik, J.; Volcy, S.; Epstein, L.H. Daily consumption of individual snack foods decreases their reinforcing value. Eat. Behav. 2008, 9, 267–276. [Google Scholar] [CrossRef]
- Temple, J.L.; Van der Kloet, E.; Atkins, A.M.; Crandall, A.K.; Ziegler, A.M. Daily exposure to either a high- or low-energy-dense snack food reduces its reinforcing value in adolescents. Obesity 2017, 25, 432–437. [Google Scholar] [CrossRef]
- Temple, J.L.; Ziegler, A.M.; Crandall, A.K.; Mansouri, T.; Epstein, L.H. Sensitization of the reinforcing value of food: A nove risk factor for overweight in adolescents. Int. J. Obes. 2020, 44, 1918–1927. [Google Scholar] [CrossRef]
- Temple, J.L.; Ziegler, A.M.; Crandall, A.K.; Mansouri, T.; Hatzinger, L.; Barich, R.; Epstein, L.H. Sensitization of the reinforcing value of high energy density foods is associated with increased zBMI gain in adolescents. Int. J. Obes. 2022, 46, 581–587. [Google Scholar] [CrossRef]
- Ma, Y.; Olendzki, B.C.; Pagoto, S.L.; Hurley, T.G.; Magner, R.P.; Ockene, I.S.; Schneider, K.L.; Merriam, P.A.; Hebert, J.R. Number of 24-hour diet recalls needed to estimate energy intake. Ann. Epidemiol. 2009, 19, 553–559. [Google Scholar] [CrossRef]
- Kirkpatrick, S.I.; Subar, A.F.; Douglass, D.; Zimmerman, T.P.; Thompson, F.E.; Kahle, L.L.; George, S.M.; Dodd, K.W.; Potischman, N. Performance of the Automated Self-Administered 24-hour Recall relative to a measure of true intakes and to an interviewer-administered 24-h recall. Am. J. Clin. Nutr. 2014, 100, 233–240. [Google Scholar] [CrossRef]
- Naska, A.; Lagiou, A.; Lagiou, P. Dietary assessment methods in epidemiological research: Current state of the art and future prospects. F1000Research 2017, 6, 926. [Google Scholar] [CrossRef]
- Kirkpatrick, S.I.; Dodd, K.W.; Potischman, N.; Zimmerman, T.P.; Douglass, D.; Guenther, P.M.; Durward, C.; Atoloye, A.T.; Kahle, L.L.; Subar, A.F.; et al. Healthy Eating Index-2015 Scores among Adults Based on Observed vs. Recalled Dietary Intake. J. Acad. Nutr. Diet. 2021, 121, 2233–2241.e2231. [Google Scholar] [CrossRef]
- Sanjeevi, N.; Freeland-Graves, J.H.; Sachdev, P.K. Association of loss of Supplemental Nutrition Assistance Program benefits with food insecurity and dietary intake of adults and children. Am. J. Clin. Nutr. 2021, 114, 683–689. [Google Scholar] [CrossRef]
- Zhang, W.; Wang, X.; Huang, J.; Wang, S.; Yao, Q.; Li, H. Healthy Eating Index-2015 in relation to risk of metabolic dysfunction-associated fatty liver disease among US population: National Health and Nutrition Examination Survey 2017–2018. Front. Nutr. 2022, 9, 1043901. [Google Scholar] [CrossRef] [PubMed]
- Kindler, J.M.; Gallo, S.; Khoury, P.R.; Urbina, E.M.; Zemel, B.S. Diet Quality and Bone Density in Youth with Healthy Weight, Obesity, and Type 2 Diabetes. Nutrients 2021, 13, 3288. [Google Scholar] [CrossRef] [PubMed]
- Vahid, F.; Jalili, M.; Rahmani, W.; Nasiri, Z.; Bohn, T. A Higher Healthy Eating Index Is Associated with Decreased Markers of Inflammation and Lower Odds for Being Overweight/Obese Based on a Case-Control Study. Nutrients 2022, 14, 5127. [Google Scholar] [CrossRef]
- Jun, S.; Cowan, A.E.; Bhadra, A.; Dodd, K.W.; Dwyer, J.T.; Eicher-Miller, H.A.; Gahche, J.J.; Guenther, P.M.; Potischman, N.; Tooze, J.A.; et al. Older adults with obesity have higher risks of some micronutrient inadequacies and lower overall dietary quality compared to peers with a healthy weight, National Health and Nutrition Examination Surveys (NHANES), 2011–2014. Public Health Nutr. 2020, 23, 2268–2279. [Google Scholar] [CrossRef] [PubMed]
- McGee, M.; Unger, S.; Hamilton, J.; Birken, C.S.; Pausova, Z.; Kiss, A.; Bando, N.; O’Connor, D.L. Associations between Diet Quality and Body Composition in Young Children Born with Very Low Body Weight. J. Nutr. 2020, 150, 2961–2968. [Google Scholar] [CrossRef] [PubMed]
- Koebnick, C.; Coleman, K.J.; Black, M.H.; Smith, N.; Der-Sarkissian, J.K.; Jacobsen, S.J.; Porter, A.H. Cohort profile: The KPSC Children’s Health Study, a population-based study of 920 000 children and adolescents in southern California. Int. J. Epidemiol. 2012, 41, 627–633. [Google Scholar] [CrossRef]
- Shields, M.; Tremblay, M.S. Canadian childhood obesity estimates based on WHO, IOTF and CDC cut-points. Int. J. Pediatr. Obes. 2010, 5, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J.; Ogden, C.L.; Grummer-Strawn, L.M.; Flegal, K.M.; Guo, S.S.; Wei, R.; Mei, Z.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. CDC growth charts: United States. Adv. Data 2000, 314, 11–27. [Google Scholar]
- Burrows, T.L.; Martin, R.J.; Collins, C.E. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J. Am. Diet. Assoc. 2010, 110, 1501–1510. [Google Scholar] [CrossRef]
- USDA Food Nad Nutrient Database for Dietary Studies 3.0. 2008. Available online: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/fndds/fndds3_doc.pdf (accessed on 27 April 2023).
- Available online: https://www.dietaryguidelines.gov/ (accessed on 27 April 2023).
- Temple, J.L.; Epstein, L.H. Sensitization of food reinforcement is related to weight status and baseline food reinforcement. Int. J. Obes. 2012, 36, 1102–1107. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L. Factors that influence the reinforcing value of foods and beverages. Physiol. Behav. 2014, 136, 97–103. [Google Scholar] [CrossRef]
- Hu, T.; Jacobs, D.R., Jr.; Larson, N.I.; Cutler, G.J.; Laska, M.N.; Neumark-Sztainer, D. Higher Diet Quality in Adolescence and Dietary Improvements Are Related to Less Weight Gain During the Transition From Adolescence to Adulthood. J. Pediatr. 2016, 178, 188–193.e183. [Google Scholar] [CrossRef]
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2020, 32, 690. [Google Scholar] [CrossRef]
- Carr, K.A.; Black, W.; Guth, C.; Shapiro, L.; Leone, L.A.; Temple, J.L.; Epstein, L.H. Reinforcing value of food, enriched home environment, and changes in percent overweight in children. Obesity 2023, 31, 1075–1084. [Google Scholar] [CrossRef]
- Hill, C.; Saxton, J.; Webber, L.; Blundell, J.; Wardle, J. The relative reinforcing value of food predicts weight gain in a longitudinal study of 7–10-y-old children. Am. J. Clin. Nutr. 2009, 90, 276–281. [Google Scholar] [CrossRef]
- Temple, J.L.; Legierski, C.M.; Giacomelli, A.M.; Salvy, S.J.; Epstein, L.H. Overweight children find food more reinforcing and consume more energy than do nonoverweight children. Am. J. Clin. Nutr. 2008, 87, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Carr, K.A.; Lin, H.; Fletcher, K.D.; Epstein, L.H. Food reinforcement, dietary disinhibition and weight gain in nonobese adults. Obesity 2014, 22, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; Paluch, R.A.; Carr, K.A.; Temple, J.L.; Bickel, W.K.; MacKillop, J. Reinforcing value and hypothetical behavioral economic demand for food and their relation to BMI. Eat. Behav. 2018, 29, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Dreher, M.L.; Ford, N.A. A Comprehensive Critical Assessment of Increased Fruit and Vegetable Intake on Weight Loss in Women. Nutrients 2020, 12, 1919. [Google Scholar] [CrossRef]
| Dietary Intake Variable | Guideline (Number of Servings Based on Estimated Energy Needs; kcals) | Mean (SD) | % Meeting Guideline |
|---|---|---|---|
| DIETARY COMPONENTS TO EAT | |||
| Fruits (cups/day) | 1400–1800-1.5 2000–2600-2 | 1.5 (1.9) | 37% |
| Vegetables (cups/day) | 1400-1.5 1600-2 1800–2000-2.5 2200–2400-3 ≥2600-3.5 | 1.4 (1.3) | 24% |
| Whole grain (oz eq/day) | 1400-2.5 1600–2000-3 2200-3.5 2400-4 2600-4.5 | 0.5 (0.8) | 4% |
| Dairy (cup eq/day) | 3 servings | 1.4 (1.2) | 11% |
| Protein (ounce eq/day) | 1400-4 1600–1800-5 2000-5.5 2200-6 2400–2600-6.5 | 8.9 (5.8) | 78% |
| DIETARY COMPONENTS TO LIMIT | |||
| Added Sugar | <10% of energy per day | 15.1 (11.3) | 34% |
| Saturated Fat | <10% of energy per day | 11.8 (2.8) | 28% |
| Sodium | <2300 mg/day | 2523 (1063) | 47% |
| n = 202 | ||
|---|---|---|
| n | % | |
| Sex Male Female | 97 105 | 48 52 |
| Ethnicity Hispanic or Latino Non-Hispanic or Latino | 15 186 | 7 93 |
| Race American Indian/Alaska Native Asian/Pacific Islander Black/African American White or Caucasian Other/mixed race | 1 4 19 159 17 | 1 2 9 79 8 |
| Household Income <$9999 $10,000–$49,999 $50,000–$69,999 $70,000–$89,999 $90,000–$109,999 $110,000–$139,999 >$140,000 | 1 33 31 31 29 36 40 | 0.5 16 15 15 14 18 20 |
| Parental Education Completed high school Some college/completed vocational training Complete college/university Completed graduate degree | 9 28 71 67 | 4 14 35 33 |
| Mean | SEM | |
| Baseline Descriptives | ||
| Age (years) | 13.3 | 0.06 |
| zBMI | 0.396 | 0.07 |
| Pubertal Development Score | 2.6 | 0.05 |
| Diet Quality Score | 3.4 | 0.10 |
| Energy Intake (kcals) | 1640.2 | 34.5 |
| Two-Year Follow-Up Descriptives | ||
| Age (years) | 15.25 | 0.064 |
| zBMI | 0.443 | 0.007 |
| Pubertal Development Score | 3.23 | 0.04 |
| Diet Quality Score | 1.9 | 0.09 |
| Energy Intake (kcals) | 1815.7 | 65.6 |
| β | SE | T | F | p | |
|---|---|---|---|---|---|
| Model 1—Energy Intake at 24 Months | |||||
| Sex | −290.6 | 63.44 | −4.58 | 20.98 | <0.001 |
| Baseline zBMI | −84.21 | 32.23 | −2.61 | 6.79 | 0.009 |
| V1 Energy Intake | 0.39 | 0.045 | 8.76 | 76.68 | <0.001 |
| V1 Diet Quality | −17.46 | 24.54 | −0.71 | 0.506 | 0.477 |
| V1 RRV of HED Food | −0.346 | 0.112 | −3.08 | 9.51 | 0.002 |
| V1 Sensitization of HED Food | −168.07 | 84.59 | −1.99 | 3.95 | 0.047 |
| Model 2—Diet Quality at 24 Months | |||||
| Sex | 0.168 | 0.103 | −1.31 | 2.66 | 0.1.04 |
| Baseline zBMI | −0.069 | 0.053 | −1.31 | 1.71 | 0.191 |
| V1 Energy Intake | 0.000 | 0.000 | 1.76 | 3.082 | 0.080 |
| V1 Diet Quality | 0.007 | 0.040 | 0.185 | 0.034 | 0.853 |
| V1 RRV of HED Food | −0.001 | 0.000 | −4.91 | 24.12 | <0.001 |
| V1 Sensitization of HED Food | 0.472 | 0.140 | 3.37 | 11.34 | <0.001 |
| Model 3—RRV of HED Food at 24 Months | |||||
| Sex | −0.606 | 0.118 | −5.14 | 26.42 | <0.001 |
| Baseline zBMI | −0.066 | 0.06 | −1.1 | 1.22 | 0.27 |
| V1 Energy Intake | 0.000 | 0.000 | 2.23 | 4.99 | 0.026 |
| V1 Diet Quality | −0.019 | 0.046 | −0.403 | 0.162 | 0.687 |
| V1 RRV of HED Food | 0.002 | 0.000 | 9.56 | 91.35 | <0.001 |
| V1 Sensitization of HED Food | 1.19 | 0.165 | 7.24 | 52.46 | <0.001 |
| Model 4—zBMI at 24 Months | |||||
| Sex | 0.12 | 0.04 | 2.99 | 8.99 | 0.003 |
| Baseline zBMI | 0.817 | 0.02 | 40.52 | 1641.98 | <0.001 |
| V1 Energy Intake | −0.0005 | 0.0005 | 0.123 | 0.015 | 0.902 |
| V1 Diet Quality | −0.041 | 0.016 | −2.66 | 7.056 | 0.008 |
| V1 RRV of HED Food | 0.0003 | 0.0006 | 0.323 | 0.104 | 0.747 |
| V1 Sensitization of HED Food | 0.125 | 0.056 | 2.23 | 4.98 | 0.026 |
| β | SE | T | F | p | |
|---|---|---|---|---|---|
| zBMI Change Over Time | |||||
| Sex | 0.097 | 0.035 | 2.786 | 7.759 | 0.006 |
| Baseline zBMI | 0.893 | 0.025 | 36.19 | 1310.15 | <0.001 |
| V1 Energy Intake | 0.000 | 0.000 | 2.081 | 4.33 | 0.039 |
| V1 Diet Quality | 0.084 | 0.068 | 1.23 | 1.51 | 0.22 |
| V1 RRV of HED Food | 0.000 | 0.000 | −1.66 | 2.75 | 0.099 |
| Diet Quality ∗ Energy Intake | −0.0008 | 0.0003 | −1.99 | 3.99 | 0.048 |
| Diet Quality ∗ RRV of HED Food | 0.00003 | 0.0008 | 1.675 | 2.81 | 0.096 |
| Energy Intake ∗ RRV of HED Food | −0.0001 | 0.00002 | −0.680 | 0.604 | 0.497 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Temple, J.L.; Mansouri, T.; Andrade, A.L.P.; Ziegler, A.M. The Influence of Relative Reinforcing Value of Food, Sensitization, Energy Intake and Diet Quality on zBMI Change over Two Years in Adolescents: A Longitudinal Cohort Study. Nutrients 2023, 15, 2179. https://doi.org/10.3390/nu15092179
Temple JL, Mansouri T, Andrade ALP, Ziegler AM. The Influence of Relative Reinforcing Value of Food, Sensitization, Energy Intake and Diet Quality on zBMI Change over Two Years in Adolescents: A Longitudinal Cohort Study. Nutrients. 2023; 15(9):2179. https://doi.org/10.3390/nu15092179
Chicago/Turabian StyleTemple, Jennifer L., Tegan Mansouri, Ana Letícia Pereira Andrade, and Amanda M. Ziegler. 2023. "The Influence of Relative Reinforcing Value of Food, Sensitization, Energy Intake and Diet Quality on zBMI Change over Two Years in Adolescents: A Longitudinal Cohort Study" Nutrients 15, no. 9: 2179. https://doi.org/10.3390/nu15092179
APA StyleTemple, J. L., Mansouri, T., Andrade, A. L. P., & Ziegler, A. M. (2023). The Influence of Relative Reinforcing Value of Food, Sensitization, Energy Intake and Diet Quality on zBMI Change over Two Years in Adolescents: A Longitudinal Cohort Study. Nutrients, 15(9), 2179. https://doi.org/10.3390/nu15092179





