The Emerging Prevalence of Obesity within Families in Europe and its Associations with Family Socio-Demographic Characteristics and Lifestyle Factors; A Cross-Sectional Analysis of Baseline Data from the Feel4Diabetes Study
Abstract
1. Introduction
2. Materials and Methods
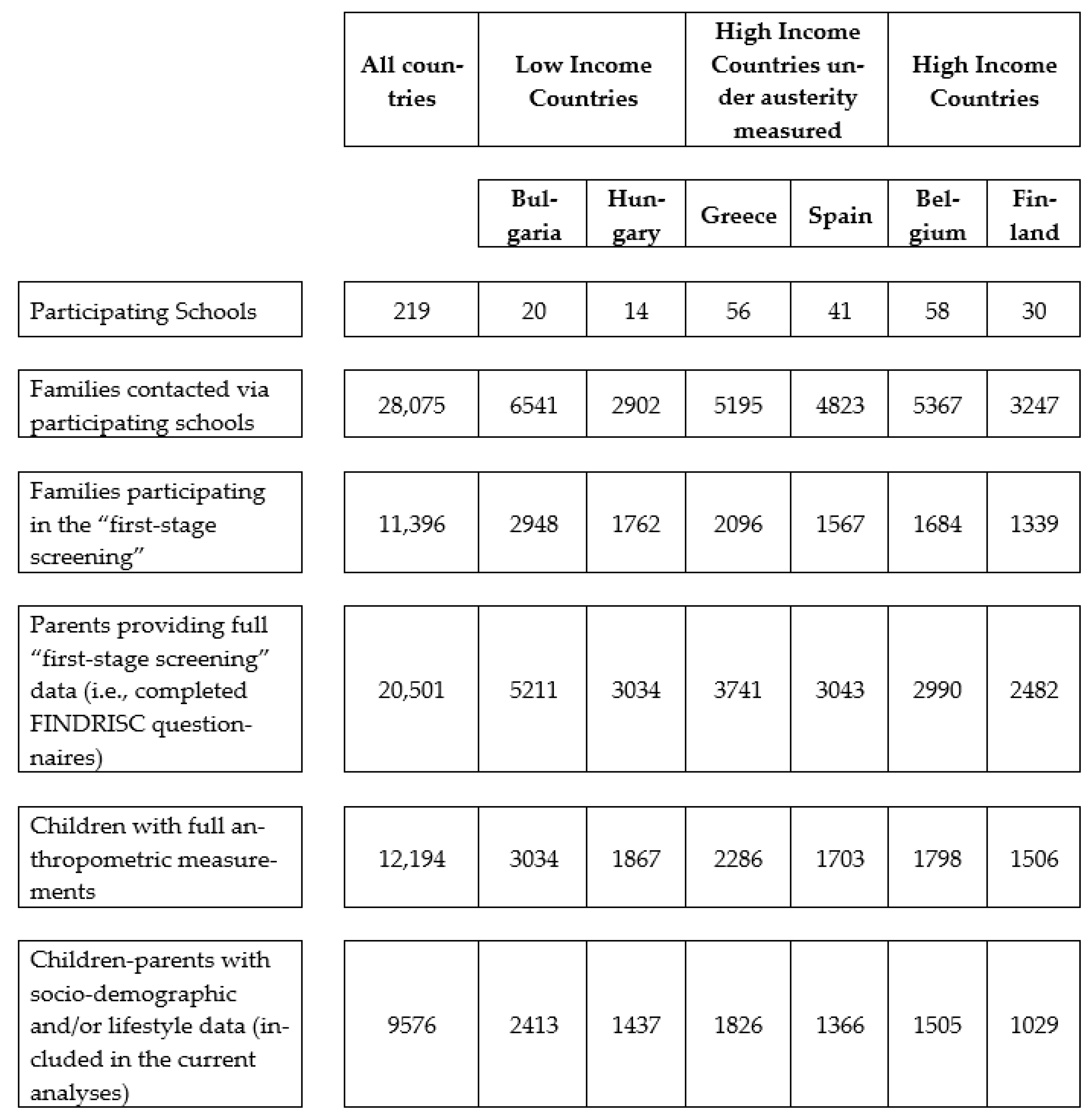
2.1. Study Design and Sampling Procedures
2.2. Ethics Approvals and Consent Forms
2.3. Data Collection
2.3.1. Socio-Demographic Characteristics
2.3.2. Anthropometry
2.3.3. Lifestyle Factors
Dietary Intake
Physical Activity and Screen Time
2.4. Statistical Analysis
3. Results
3.1. Prevalence of Family Obesity in the Total Sample, by Country’s Economic Classification, and by Country
3.2. Socio-Demographic Characteristics of Families in the Total Sample and by Economic Classification of Countries
3.3. Dietary Intake, Physical Activity Levels, and Screen Time of Families in the Total Sample and by Economic Classification of Countries
3.4. Associations between Sociodemographic Characteristics and Family Obesity
3.5. Associations between Lifestyle Factors and Family Obesity
3.6. Associations between Sociodemographic Characteristics and Lifestyle Factors with Family Obesity
4. Discussion
5. Conclusions and Implications for Practice and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 7 January 2022).
- World Health Organization. The Global Health Observatory. Noncommunicable Diseases. Available online: https://www.who.int/data/gho/data/themes/noncommunicable-diseases (accessed on 7 January 2022).
- Centers for Disease and Control Prevention. Morbidity and Mortality Weekly Report. Body Mass Index and Risk for COVID-19–Related Hospitalization, Intensive Care Unit Admission, Invasive Mechanical Ventilation, and Death—United States, March–December 2020. Available online: https://www.cdc.gov/mmwr/volumes/70/wr/mm7010e4.htm?s_cid=mm7010e4_x (accessed on 7 January 2022).
- World OBESITY. COVID-19 and Obesity: The 2021 Atlas. The Cost of not Addressing the Global Obesity Crisis. Available online: https://www.worldobesityday.org/assets/downloads/COVID-19-and-Obesity-The-2021-Atlas.pdf (accessed on 7 January 2022).
- Reilly, J.J.; Armstrong, J.; Dorosty, A.R.; Emmett, P.; Ness, A.; Rogers, I.; Steer, C.; Sherriff, A. Early life risk factors for obesity in childhood: Cohort study. BMJ 2005, 330, 1357. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Guthrie, C.; Sanderson, S.; Lehtinen-Jacks, S.; Martelin, T.; Laatikainen, T. Food and activity preferences in children of lean and obese parents. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 971–977. [Google Scholar] [CrossRef]
- Morgan, P.J.; Okely, A.D.; Cliff, D.P.; Jones, R.A.; Baur, L.A. Correlates of objectively measured physical activity in obese children. Obesity 2008, 16, 2634–2641. [Google Scholar] [CrossRef]
- Parikka, S.; Mäki, P.; Levälahti, E.; Lehtinen-Jacks, S.; Martelin, T.; Laatikainen, T. Associations between parental BMI, socioeconomic factors, family structure and overweight in Finnish children: A path model approach. BMC Public Health 2015, 15, 271. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.; Zhang, Y.; Zhang, S.; He, Y.; Gao, J.; Wang, L.; Wang, Y.; Hang, D.; Ma, Y. Association between environmental composite quality index score and obesity in children and their family: A cross-sectional study in northeast China. Chemosphere 2022, 297, 134204. [Google Scholar] [CrossRef] [PubMed]
- Pachucki, M.C.; Lovenheim, M.F.; Harding, M. Within-family obesity associations: Evaluation of parent, child, and sibling relationships. Am. J. Prev. Med. 2014, 47, 382–391. [Google Scholar] [CrossRef]
- Valverde, M.A.; Patin, R.V.; Oliveira, F.L.; Lopez, F.A.; Vitolo, M.R. Outcomes of obese children and adolescents enrolled in a multidisciplinary health program. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Manios, Y.; Androutsos, O.; Lambrinou, C.P.; Cardon, G.; Lindstrom, J.; Annemans, L.; Mateo-Gallego, R.; de Sabata, M.S.; Iotova, V.; Kivela, J.; et al. A school- and community-based intervention to promote healthy lifestyle and prevent type 2 diabetes in vulnerable families across Europe: Design and implementation of the Feel4Diabetes-study. Public Health Nutr. 2018, 21, 3281–3290. [Google Scholar] [CrossRef]
- Anastasiou, C.A.; Fappa, E.; Zachari, K.; Mavrogianni, C.; Van Stappen, V.; Kivelä, J.; Virtanen, E.; González-Gil, E.M.; Flores-Barrantes, P.; Nánási, A. Development and reliability of questionnaires for the assessment of diet and physical activity behaviors in a multi-country sample in Europe the Feel4Diabetes Study. BMC Endocr. Disord. 2020, 20, 135. [Google Scholar] [CrossRef] [PubMed]
- Androutsos, O.; Anastasiou, C.; Lambrinou, C.P.; Mavrogianni, C.; Cardon, G.; Van Stappen, V.; Kivelä, J.; Wikström, K.; Moreno, L.A.; Iotova, V. Intra- and inter- observer reliability of anthropometric measurements and blood pressure in primary schoolchildren and adults: The Feel4Diabetes-study. BMC Endocr. Disord. 2020, 20, 27. [Google Scholar] [CrossRef]
- The World Bank. World Bank Country and Lending Groups–Country Classification. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519 (accessed on 8 January 2022).
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013, 310, 2191–2194. [Google Scholar]
- Lexico. Middle Age. Available online: https://www.lexico.com/en/definition/middle_age (accessed on 11 January 2022).
- Merriam-Webster. Middle Age. Available online: https://www.merriam-webster.com/dictionary/middle%20age (accessed on 11 January 2022).
- Collins. Middle Age. Available online: https://www.collinsdictionary.com/dictionary/english/middle-age (accessed on 11 January 2022).
- European Commision/EACEA/Eurydice, 2018. Compulsory Education in Europe 2018/19. Eurydice–Facts and Figures. Luxemburg: Publications Office of the European Union. Available online: https://eacea.ec.europa.eu/national-policies/eurydice/sites/default/files/compulsory_education_2018_19.pdf (accessed on 11 January 2022).
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194. [Google Scholar] [CrossRef] [PubMed]
- Frieden, J.; Stefanie, W. Understanding the Political Economy of the Eurozone Crisis. Annu. Rev. Political Sci. 2017, 20, 371–390. [Google Scholar] [CrossRef]
- Hayes, A.; Tan, E.J.; Killedar, A.; Lung, T. Socioeconomic inequalities in obesity: Modelling future trends in Australia. BMJ Open. 2019, 9, e026525. [Google Scholar] [CrossRef] [PubMed]
- Benusic, M.; Cheskin, L.J. Obesity prevalence in large US cities: Association with socioeconomic indicators, race/ethnicity and physical activity. J. Public Health 2021, 43, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Siopis, G.; Jones, A.; Allman-Farinelli, M. The dietetic workforce distribution geographic atlas provides insight into the inequitable access for dietetic services for people with type 2 diabetes in Australia. Nutr Diet. 2020, 77, 121–130. [Google Scholar] [CrossRef]
- Stormacq, C.; Van den Broucke, S.; Wosinski, J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot. Int. 2019, 34, e1–e17. [Google Scholar] [CrossRef]
- Siopis, G.; Colagiuri, S.; Allman-Farinelli, M. People with type 2 diabetes report dietitians, social support and health literacy facilitate their dietary change. J. Nutr. Ed. Behav. 2020, 53, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Siopis, G.; Colagiuri, S.; Allman-Farinelli, M. Doctors identify regulatory barriers for their patients with type 2 diabetes to access the nutrition expertise of dietitians. Aust. J. Prim. Care. 2020, 27, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Siopis, G.; Colagiuri, S.; Allman-Farinelli, M. Dietitians’ experiences and perspectives regarding access to and delivery of dietetic services for people with type 2 diabetes mellitus. Heliyon 2020, 6, e03344. [Google Scholar] [CrossRef] [PubMed]
- Mavrogianni, C.; Moschonis, G.; Karaglani, E.; Cardon, G.; Iotova, V.; De Miguel-Etayo, P.; González-Gil, E.M.; Tsochev, K.; Tankova, T.; Rurik, I.; et al. European Childhood Obesity Risk Evaluation (CORE) index based on perinatal factors and maternal sociodemographic characteristics: The Feel4Diabetes-study. Eur. J. Pediatr. 2021, 180, 2549–2561. [Google Scholar] [CrossRef] [PubMed]
- Moschonis, G.; Tsoutsoulopoulou, K.; Efstathopoulou, E.; Androutsos, O.; Lambrinou, C.-P.; Georgiou, A.; Filippou, C.; Lidoriki, I.; Reppas, K.; Androutsos, O. Conceptual framework of a simplified multi-dimensional model presenting the environmental and personal determinants of cardiometabolic risk behaviors in childhood. Expert. Rev. Cardiovasc. Ther. 2015, 13, 673–692. [Google Scholar] [CrossRef]
- Brouwer, S.I.; Küpers, L.K.; Kors, L.; Sijtsma, A.; Sauer, P.J.J.; Renders, C.M.; Corpeleijn, E. Parental physical activity is associated with objectively measured physical activity in young children in a sex-specific manner: The GECKO Drenthe cohort. BMC Public Health 2018, 18, 1033. [Google Scholar] [CrossRef]
- Zecevic, C.A.; Tremblay, L.; Lovsin, T.; Michel, L. Parental Influence on Young Children’s Physical Activity. Int. J. Pediatr. 2010, 2010, 468526. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, S.; De Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors Influencing Children’s Eating Behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef] [PubMed]
- Savage, J.S.; Fisher, J.O.; Birch, L.L. Parental influence on eating behavior: Conception to adolescence. J. Law Med. Ethics. 2007, 35, 22–34. [Google Scholar] [CrossRef]
- Yee, A.Z.; Lwin, M.O.; Ho, S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef]
- Sandercock, G.R.H.; Ogunleye, A.; Voss, C. Screen time and physical activity in youth: Thief of time or lifestyle choice? J. Phys. Act. Health 2012, 9, 977–984. [Google Scholar] [CrossRef]
- de Araújo, L.G.M.; Turi, B.C.; Locci, B.; Mesquita, C.A.A.; Fonsati, M.B.; Monteiro, H.L. Patterns of Physical Activity and Screen Time Among Brazilian Children. J. Phys. Act. Health 2018, 15, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, A.; Sjöblom, L.; Eke, H.; Bonn, S.E.; Lagerros, Y.T. Screen time and physical activity in children and adolescents aged 10-15 years. PLoS One 2021, 16, e0254255. [Google Scholar] [CrossRef] [PubMed]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Screen time and its effect on dietary habits and lifestyle among schoolchildren. Cent. Eur. J. Public Health 2020, 28, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Christofaro, D.G.; De Andrade, S.M.; Mesas, A.E.; Fernandes, R.A.; Júnior, J.C.F. Higher screen time is associated with overweight, poor dietary habits and physical inactivity in Brazilian adolescents, mainly among girls. Eur. J. Sport Sci. 2016, 16, 498–506. [Google Scholar] [CrossRef]
- Wärnberg, J.; Pérez-Farinós, N.; Benavente-Marín, J.C.; Gómez, S.F.; Labayen, I.; Zapico, A.G.; Gusi, N.; Aznar, S.; Alcaraz, P.E.; González-Valeiro, M. Screen Time and Parents’ Education Level Are Associated with Poor Adherence to the Mediterranean Diet in Spanish Children and Adolescents: The PASOS Study. J. Clin. Med. 2021, 10, 795. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S.J.H.; Griffiths, P.; Johnston, J.P.; Haycraft, E. Clustering and correlates of screen-time and eating behaviours among young children. BMC Public Health 2018, 18, 753. [Google Scholar] [CrossRef]
- de Pinho, M.G.M.; Adami, F.; Jucemar, B.; de Assis, F.; de Vasconcelos, G. Association between screen time and dietary patterns and overweight/obesity among adolescents. Rev. De Nutr. 2017, 30, 377–389. [Google Scholar] [CrossRef]
- Watanabe, Y.; Saito, I.; Henmi, I.; Yoshimura, K.; Maruyama, K.; Yamauchi, K.; Matsuo, T.; Kato, T.; Tanigawa, T.; Kishida, T.; et al. Skipping Breakfast is Correlated with Obesity. J. Rural Med. 2014, 9, 51–58. [Google Scholar] [CrossRef]
- Kesztyüs, D.; Traub, M.; Lauer, R.; Kesztyüs, T.; Steinacker, J.M. Skipping breakfast is detrimental for primary school children: Cross-sectional analysis of determinants for targeted prevention. BMC Public Health 2017, 17, 258. [Google Scholar] [CrossRef]
- Wadolowska, L.; Hamulka, J.; Kowalkowska, J.; Ulewicz, N.; Gornicka, M.; Jeruszka-Bielak, M.; Kostecka, M.; Wawrzyniak, A. Skipping Breakfast and a Meal at School: Its Correlates in Adiposity Context. Report from the ABC of Healthy Eating Study of Polish Teenagers. Nutrients 2019, 11, 1563. [Google Scholar] [CrossRef]
- Ruddick-Collins, L.C.; Johnston, J.D.; Morgan, P.J. The Big Breakfast Study: Chrono-nutrition influence on energy expenditure and bodyweight. Nutr. Bull. 2018, 43, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Cordova, R.; Kliemann, N.; Huybrechts, I.; Rauber, F.; Vamos, E.P.; Levy, R.B.; Wagner, K.-H.; Viallon, V.; Casagrande, C.; Nicolas, G. Consumption of ultra-processed foods associated with weight gain and obesity in adults: A multi-national cohort study. Clin. Nutr. 2021, 40, 5079–5088. [Google Scholar] [CrossRef]
- Rauber, F.; Chang, K.; Vamos, E.P.; da Costa Louzada, M.L.; Monteiro, C.A.; Millett, C.; Levy, R.B. Ultra-processed food consumption and risk of obesity: A prospective cohort study of UK Biobank. Eur. J. Nutr. 2021, 60, 2169–2180. [Google Scholar] [CrossRef] [PubMed]
- Machado, P.P.; Steele, E.M.; Levy, R.B.; da Costa Louzada, M.L.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed food consumption and obesity in the Australian adult population. Nutr. Diabetes 2020, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Wheildon, N.; Ishikawa, S. Food Additive P-80 Impacts Mouse Gut Microbiota Promoting Intestinal Inflammation, Obesity and Liver Dysfunction. SOJ Microbiol. Infect. Dis. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Baran, A.; Sulukan, E.; Türkoğlu, M.; Ghosigharehagaji, A.; Yildirim, S.; Kankaynar, M.; Bolat, I.; Kaya, M.; Topal, A.; Ceyhun, S.B. Is sodium carboxymethyl cellulose (CMC) really completely innocent? It may be triggering obesity. Int. J. Biol. Macromol. 2020, 163, 2465–2473. [Google Scholar] [CrossRef]
- Png, C.W.; Lindén, S.K.; Gilshenan, K.S.; Zoetendal, E.G.; Sweeney, C.S.; Sly, L.I.; Guckin, M.A.; Florin, T.H.J. Mucolytic bacteria with increased prevalence in IBD mucosa augment in vitro utilization of mucin by other bacteria. Am. J. Gastroenterol. 2010, 105, 2420–2428. [Google Scholar] [CrossRef]
- Zhan, C.D.; Sindhu, R.K.; Pang, J.; Ehdaie, A.; Vaziri, N.D. Superoxide dismutase, catalase and glutathione peroxidase in the spontaneously hypertensive rat kidney: Effect of antioxidant-rich diet. J. Hypertens. 2004, 22, 2025–2033. [Google Scholar] [CrossRef] [PubMed]
- Teng, M.; Zhao, F.; Zhou, Y.; Yan, S.; Tian, S.; Yan, J.; Meng, Z.; Bi, S.; Wang, C. Effect of Propiconazole on the Lipid Metabolism of Zebrafish Embryos (Danio rerio). J. Agric. Food Chem. 2019, 67, 4623–4631. [Google Scholar] [CrossRef]

| Total Sample (n = 9576) | Economic Classification of Countries | |||||
|---|---|---|---|---|---|---|
| Low-Income Countries (n = 3850) | High-Income Countries, under Austerity Measures (n = 3192) | High-Income Countries (n = 2534) | p-Value | |||
| Obesity (%) | Family Obesity * | 6.6 | 7.0 c | 7.6 b | 4.5 b,c | <0.001 |
| Two obese parents/non-obese child | 2.7 | 2.7 | 2.9 | 2.5 | 0.703 | |
| One obese parent/obese child | 2.8 | 3.4 c | 3.4 b | 1.3 b,c | <0.001 | |
| Two obese parents/obese child | 1.1 | 0.9 | 1.3 | 0.7 | 0.069 | |
| Child sex (%) | Boys | 49.4 | 48.5 | 50.0 | 50.0 | 0.260 |
| Girls | 50.6 | 51.5 | 50.0 | 50.0 | ||
| Age of Mother (%) | <45 years old | 90.4 | 93.1 a | 85.6 a,b | 91.9 b | <0.001 |
| ≥45 years old | 9.6 | 6.9 a | 14.4 a,b | 8.1 b | ||
| Age of Father (%) | <45 years old | 77.7 | 81.3 a | 68.6 a,b | 83.3 b | <0.001 |
| ≥45 years old | 22.3 | 18.7 a | 31.4 a,b | 16.7 b | ||
| Education of Mother (%) † | <9 years | 8.4 | 11.9 a,c | 7.7 a,b | 4.1 b,c | <0.001 |
| 9–14 years | 35.3 | 34.3 a | 39.2 a,b | 32.6 b | ||
| >14 years | 51.9 | 53.8 c | 53.1 b | 63.3 b,c | ||
| Education of Father (%) † | <9 years | 9.7 | 10.9 c | 11.3 b | 6.2 b,c | <0.001 |
| 9–14 years | 44.4 | 48.3 a | 37.9 a,b | 45.5 b | ||
| >14 years | 46.0 | 40.8 a,c | 50.8 a | 48.3 c | ||
| Occupation of Mother (%) | Unemployed/other # | 29.5 | 32.1 a,c | 35.5 a,b | 19.3 b,c | <0.001 |
| Employed full-time | 57.5 | 62.0 a | 48.2 a,b | 60.9 b | ||
| Employed part-time | 13.1 | 6.0 a,c | 16.5 a,b | 19.8 b,c | ||
| Occupation of Father (%) | Unemployed/other # | 14.1 | 19.2 a,c | 11.9 a,b | 9.4 b,c | <0.001 |
| Employed full-time | 81.5 | 75.4 a,c | 83.1 a,b | 88.6 b,c | ||
| Employed part-time | 4.3 | 5.4 c | 5.0 b | 2.0 b,c | ||
| Lifestyle Factors | Economic Classification of Countries | ||||
|---|---|---|---|---|---|
| Total Sample (n = 9576) | Low-Income Countries (n = 3192) | High-Income Countries, under Austerity Measures (n= 3850) | High-Income Countries (n = 2534) | p-Value * | |
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | ||
| Water (number of cups per day) | 9.0 (7.0, 11.0) | 9.0 (7.0, 12.0) | 10.0 (7.0, 12.0) | 7.0 (5.0, 9.0) | <0.001 |
| Vegetables (number of portions per day) | 2.3 (1.3, 3.0) | 2.3 (1.3, 3.0) | 1.6 (1.0, 2.3) | 3.0 (1.7, 3.0) | <0.001 |
| Fruits (number of portions per day) | 2.9 (1.7, 3.7) | 3.0 (1.7, 4.0) | 2.4 (1.6, 3.4) | 3.0 (1.7, 3.4) | <0.001 |
| Dairy–unsweetened (number of times per day) | 1.0 (0.5, 1.6) | 1.0 (0.4, 1.3) | 1.2 (0.7, 1.8) | 1.2 (0.7, 1.8) | <0.001 |
| Dairy–sweetened (number of times per day) | 0.4 (0.0, 1.0) | 0.4 (0.0, 1.0) | 0.5 (0.0, 1.0) | 0.4 (0.0, 0.8) | <0.001 |
| Cereals–low fibre (number of times per day) | 0.5 (0.2, 1.0) | 0.5 (0.2, 1.0) | 0.7 (0.2, 1.2) | 0.5 (0.2, 1.0) | <0.001 |
| Cereals–wholegrain (number of times per day) | 0.7 (0.0, 1.2) | 0.4 (0.0, 1.0) | 0.4 (0.0, 1.0) | 1.2 (0.7, 1.6) | <0.001 |
| Soft drinks–with sugar (number of portions per day) | 0.2 (0.1, 0.7) | 0.3 (0.1, 1.0) | 0.3 (0.1, 0.6) | 0.3 (0.1, 0.7) | <0.001 |
| Soft drinks–diet (number of portions per day) | 0.1 (0.1, 0.3) | 0.1 (0.1, 0.1) | 0.1 (0.1, 0.3) | 0.1 (0.1, 0.4) | <0.001 |
| Sweets (number of portions per day) | 1.0 (0.6, 2.0) | 1.3 (0.7, 2.3) | 1.0 (0.6, 1.6) | 1.0 (0.4, 2.0) | <0.001 |
| Savoury snacks and fast food (number of portions per day) | 0.3 (0.1, 0.7) | 0.4 (0.1, 1.0) | 0.3 (0.1, 0.4) | 0.3 (0.1, 0.4) | <0.001 |
| Breakfast (number of days per week) | 14.0 (11.0, 14.0) | 13.0 (13.0, 14.0) | 14.0 (11.0, 14.0) | 14.0 (14.0, 14.0) | <0.001 |
| Meeting PA recommendations (number of days per week) | 10.0 (7.0, 12.0) | 10.0 (10.0, 13.0) | 9.0 (6.0, 12.0) | 11.0 (8.0, 13.0) | <0.001 |
| Average screen time (number of hours per day) | 3.3 (2.2, 4.9) | 3.6 (2.4, 5.3) | 3.0 (1.9, 4.3) | 3.6 (2.5, 4.8) | <0.001 |
| Independent Variables | Dependent Variable: Family Obesity | ||||
|---|---|---|---|---|---|
| Total Sample (n = 9576) | Economic Classification of Countries * | ||||
| Low-Income Countries (n = 3192) | High-Income Countries, under Austerity Measures (n = 3850) | High-Income Countries (n = 2534) | |||
| OR (95% C.I.) | OR (95% C.I.) | OR (95% C.I.) | OR (95% C.I.) | ||
| Age of Mother | <45 years old | 1.00 | 1.00 | 1.00 | 1.00 |
| ≥45 years old | 1.50 (1.18, 1.91) | 1.55 (1.01, 2.40) | 1.09 (0.75, 1.57) | 2.73 (1.63, 4.58) | |
| Age of Father | <45 years old | 1.00 | 1.00 | 1.00 | 1.00 |
| ≥45 years old | 1.18 (0.97, 1.42) | 1.02 (0.74, 1.40) | 0.91 (0.68, 1.21) | 2.23 (1.51, 3.47) | |
| Education of Mother † | <9 years | 1.00 | 1.00 | 1.00 | 1.00 |
| 9–14 years | 0.91 (0.69, 1.20) | 1.16 (0.79, 1.70) | 0.75 (0.48, 1.18) | 0.72 (0.33, 1.57) | |
| >14 years | 0.42 (0.32, 0.55) | 0.53 (0.36, 0.79) | 0.36 (0.23, 0.57) | 0.34 (0.16, 0.74) | |
| Education of Father † | <9 years | 1.00 | 1.00 | 1.00 | 1.00 |
| 9–14 years | 0.72 (0.57, 0.92) | 1.01 (0.70, 1.48) | 0.66 (0.45, 0.96) | 0.47 (0.26, 0.84) | |
| >14 years | 0.31 (0.24, 0.41) | 0.44 (0.29, 0.67) | 0.27 (0.18, 0.40) | 0.24 (0.13, 0.44) | |
| Occupation of Mother | unemployed/other # | 1.00 | 1.00 | 1.00 | 1.00 |
| employed full-time | 0.67 (0.56, 0.81) | 0.87 (0.66, 1.13) | 0.75 (0.55, 1.01) | 0.36 (0.23, 0.56) | |
| employed part-time | 0.60 (0.45, 0.81) | 0.94 (0.54, 1.63) | 0.54 (0.34, 0.86) | 0.50 (0.29, 0.85) | |
| Occupation of Father | unemployed/other # | 1.00 | 1.00 | 1.00 | 1.00 |
| employed full-time | 0.81 (0.64, 1.02) | 1.20 (0.85, 1.69) | 0.62 (0.42, 0.92) | 0.52 (0.30, 0.88) | |
| employed part-time | 1.38 (0.93, 2.04) | 1.79 (1.03, 3.09) | 0.90 (0.46, 1.77) | 1.39 (0.49, 3.97) | |
| Independent Variables | Dependent Variable: Family Obesity | |||
|---|---|---|---|---|
| Total Sample (n = 9576) | Economic Classification of Countries * | |||
| Low-Income Countries (n = 3192) | High-Income Countries, under Austerity Measures (n= 3850) | High-Income Countries (n = 2534) | ||
| OR (95% C.I) | OR (95% C.I) | OR (95% C.I) | OR (95% C.I) | |
| Water (number of cups per day) | 1.09 (1.06, 1.12) | 1.04 (0.99, 1.08) | 1.15 (1.09, 1.22) | 1.05 (0.98, 1.12) |
| Vegetables (number of portions per day) | 0.90 (0.86, 0.95) | 0.94 (0.88, 1.01) | 0.91 (0.83, 1.00) | 0.89 (0.79, 1.02) |
| Fruits (number of portions per day) | 0.96 (0.92, 0.99) | 0.96 (0.91, 1.01) | 0.93 (0.86, 1.00) | 0.99 (0.90, 1.11) |
| Dairy–unsweetened (number of times per day) | 1.03 (0.91, 1.18) | 1.13 (0.91, 1.41) | 0.98 (0.80, 1.21) | 1.12 (0.82, 1.54) |
| Dairy–sweetened (number of times per day) | 1.02 (0.89, 1.18) | 1.12 (0.90, 1.39) | 0.79 (0.63, 0.98) | 1.48 (1.06, 2.08) |
| Cereals–low fibre (number of times per day) | 1.11 (0.96, 1.28) | 1.06 (0.85, 1.31) | 0.98 (0.77, 1.23) | 1.31 (0.92, 1.87) |
| Cereals–wholegrain (number of times per day) | 0.72 (0.62, 0.83) | 0.87 (0.68, 1.11) | 0.80 (0.62, 1.03) | 0.72 (0.53, 0.99) |
| Soft drinks–with sugar (number of portions per day) | 1.05 (0.99, 1.09) | 1.05 (1.00, 1.11) | 0.95 (0.81, 1.13) | 1.05 (0.90, 1.22) |
| Soft drinks–diet (number of portions per day) | 1.10 (1.03, 1.17) | 1.10 (1.02, 1.19) | 1.02 (0.82, 1.28) | 1.20 (1.06, 1.36) |
| Sweets (number of portions per day) | 0.97 (0.91, 1.02) | 0.99 (0.92, 1.06) | 1.02 (0.90, 1.15) | 0.82 (0.68, 0.98) |
| Savoury snacks and fast food (number of portions per day) | 1.11 (1.05, 1.17) | 1.08 (1.02, 1.16) | 1.15 (0.98, 1.34) | 1.21 (0.96, 1.53) |
| Breakfast (number of days per week) | 0.94 (0.91, 0.96) | 0.98 (0.94, 1.02) | 0.92 (0.89, 0.96) | 0.92 (0.85, 0.99) |
| Meeting PA recommendations (number of days per week) | 0.96 (0.93, 0.98) | 0.99 (0.95, 1.03) | 0.91 (0.87, 0.95) | 0.99 (0.93, 1.05) |
| Average screen time (number of hours per day) | 1.05 (1.01, 1.09) | 1.02 (0.96, 1.08) | 1.10 (1.04, 1.17) | 1.05 (0.95, 1.16) |
| Independent Variables | Dependent Variable: Family Obesity | ||||
|---|---|---|---|---|---|
| Total Sample (n = 9576) | Economic Classification of Countries * | ||||
| Low-Income Countries (n = 3192) | High-Income Countries, under Austerity Measures (n= 3850) | High-Income Countries (n = 2534) | |||
| Socio-demographics | OR (95% C.I) | OR (95% C.I) | OR (95% C.I) | OR (95% C.I) | |
| Age of Mother | <45 years old | 1.00 | 1.00 | 1.00 | 1.00 |
| ≥45 years old | 1.50 (0.99, 2.28) | 1.11 (0.55,2.27) | 1.34 (0.63, 2.88) | 2.1 (0.99, 4.65) | |
| Age of Father | <45 years old | 1.00 | 1.00 | 1.00 | 1.00 |
| ≥45 years old | 1.02 (0.75, 1.38) | 1.08 (0.69, 1.69) | 0.79 (0.45, 1.39) | 1.46 (0.78, 2.74) | |
| Education of Mother † | <9 years | 1.00 | 1.00 | 1.00 | 1.00 |
| 9–14 years | 1.08 (0.67, 1.75) | 1.83 (0.80, 4.22) | 0.66 (0.31, 1.39) | 1.49 (0.44, 5.02) | |
| >14 years | 0.79 (0.46, 1.33) | 1.20 (0.48, 2.96) | 0.79 (0.34, 1.88) | 0.80 (0.22, 2.85) | |
| Education of Father † | <9 years | 1.00 | 1.00 | 1.00 | 1.00 |
| 9–14 years | 0.71 (0.48, 1.06) | 0.53 (0.26, 1.11) | 0.73 (0.40, 1.35) | 0.65 (0.29, 1.47) | |
| >14 years | 0.37 (0.24, 0.59) | 0.24 (0.10, 0.54) | 0.39 (0.17, 0.86) | 0.50 (0.20, 1.23) | |
| Occupation of Mother | unemployed/other # | 1.00 | 1.00 | 1.00 | 1.00 |
| employed full-time | 0.86 (0.66, 1.12) | 0.91 (0.62, 1.34) | 0.89 (0.54, 1.45) | 0.55 (0.31, 0.98) | |
| employed part-time | 0.71 (0.47, 1.08) | 0.65 (0.28, 1.49) | 0.78 (0.34, 1.80) | 0.67 (0.34, 1.32) | |
| Occupation of Father | unemployed/other # | 1.00 | 1.00 | 1.00 | 1.00 |
| employed full-time | 0.89 (0.65, 1.22) | 0.96 (0.62, 1.49) | 0.66 (0.35, 1.26) | 1.04 (0.50, 2.16) | |
| employed part-time | 1.41 (0.81, 2.47) | 0.90 (0.36, 2.20) | 1.18 (0.45, 3.05) | 3.21 (0.89, 11.5) | |
| Lifestyle factors | |||||
| Water (number of cups per day) | 1.11 (1.06, 1.15) | 1.06 (1.01, 1.12) | 1.24 (1.12, 1.37) | 1.24 (1.12, 1.37) | |
| Vegetables (number of portions per day) | 0.95 (0.89, 1.02) | 0.97 (0.87, 1.07) | 0.96 (0.82, 1.11) | 0.96 (0.82, 1.11) | |
| Fruits (number of portions per day) | 0.97 (0.92, 1.03) | 0.97 (0.91, 1.05) | 0.95 (0.83, 1.08) | 0.95 (0.83, 1.08) | |
| Dairy–sweetened (number of times per day) | 0.90 (0.72, 1.13) | 0.77 (0.54, 1.09) | 0.88 (0.57, 1.35) | 0.88 (0.57, 1.35) | |
| Cereals–wholegrain (number of times per day) | 0.91 (0.75, 1.11) | 0.97 (0.70, 1.34) | 0.92 (0.62, 1.37) | 0.92 (0.62, 1.37) | |
| Soft drinks–diet (number of portions per day) | 1.08 (0.99, 1.18) | 1.05 (0.94, 1.18) | 0.77 (0.33, 1.83) | 0.77 (0.33, 1.83) | |
| Sweets (number of portions per day) | 0.87 (0.78, 0.97) | 0.92 (0.81, 1.05) | 0.92 (0.71, 1.19) | 0.92 (0.71, 1.19) | |
| Savoury snacks and fast food (number of portions per day) | 1.14 (1.01, 1.28) | 1.12 (0.97, 1.29) | 0.97 (0.64, 1.50) | 0.97 (0.64, 1.50) | |
| Breakfast (number of days per week) | 1.01 (0.97, 1.04) | 1.02 (0.97, 1.08) | 0.99 (0.93, 1.06) | 0.99 (0.93, 1.06) | |
| Meeting PA recommendations (number of days per week) | 0.95 (0.92, 0.98) | 0.95 (0.90, 0.99) | 0.91 (0.86, 0.97) | 0.91 (0.86, 0.97) | |
| Average screen time (number of hours per day) | 1.03 (0.97, 1.08) | 1.02 (0.95, 1.10) | 1.03 (0.93, 1.14) | 1.03 (0.93, 1.14) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siopis, G.; Moschonis, G.; Reppas, K.; Iotova, V.; Bazdarska, Y.; Chakurova, N.; Rurik, I.; Radó, A.S.; Cardon, G.; Craemer, M.D.; et al. The Emerging Prevalence of Obesity within Families in Europe and its Associations with Family Socio-Demographic Characteristics and Lifestyle Factors; A Cross-Sectional Analysis of Baseline Data from the Feel4Diabetes Study. Nutrients 2023, 15, 1283. https://doi.org/10.3390/nu15051283
Siopis G, Moschonis G, Reppas K, Iotova V, Bazdarska Y, Chakurova N, Rurik I, Radó AS, Cardon G, Craemer MD, et al. The Emerging Prevalence of Obesity within Families in Europe and its Associations with Family Socio-Demographic Characteristics and Lifestyle Factors; A Cross-Sectional Analysis of Baseline Data from the Feel4Diabetes Study. Nutrients. 2023; 15(5):1283. https://doi.org/10.3390/nu15051283
Chicago/Turabian StyleSiopis, George, George Moschonis, Kyriakos Reppas, Violeta Iotova, Yuliya Bazdarska, Nevena Chakurova, Imre Rurik, Anette Si Radó, Greet Cardon, Marieke De Craemer, and et al. 2023. "The Emerging Prevalence of Obesity within Families in Europe and its Associations with Family Socio-Demographic Characteristics and Lifestyle Factors; A Cross-Sectional Analysis of Baseline Data from the Feel4Diabetes Study" Nutrients 15, no. 5: 1283. https://doi.org/10.3390/nu15051283
APA StyleSiopis, G., Moschonis, G., Reppas, K., Iotova, V., Bazdarska, Y., Chakurova, N., Rurik, I., Radó, A. S., Cardon, G., Craemer, M. D., Wikström, K., Valve, P., Moreno, L. A., De Miguel-Etayo, P., Makrilakis, K., Liatis, S., Manios, Y., & on behalf of the Feel4Diabetes-Study Group. (2023). The Emerging Prevalence of Obesity within Families in Europe and its Associations with Family Socio-Demographic Characteristics and Lifestyle Factors; A Cross-Sectional Analysis of Baseline Data from the Feel4Diabetes Study. Nutrients, 15(5), 1283. https://doi.org/10.3390/nu15051283












