Enhancing Efficacy of a Brief Obesity and Eating Disorder Prevention Program: Long-Term Results from an Experimental Therapeutics Trial
Abstract
1. Introduction
2. Methods
2.1. Participants and Procedures
2.2. Interventions
2.3. Measures
2.4. Data Analyses
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [PubMed]
- Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity; World Health Organization: Geneva, Switzerland, 1998; pp. 1–178.
- Lowe, M.R.; Annunziato, R.A.; Markowitz, J.T.; Didie, E.; Bellace, D.L.; Riddell, L.; Maille, C.; McKinney, S.; Stice, E. Multiple types of dieting prospectively predict weight gain during the freshman year of college. Appetite 2006, 47, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Allman-Farinelli, M.; Partridge, S.R.; McGeechan, K.; Balestracci, K.; Hebden, L.; Wong, A.; Phongsavan, P.; Denney-Wilson, E.; Harris, M.F.; Bauman, A.; et al. A mobile health lifestyle program for prevention of weight gain in young adults (TXT2BFit): Nine-month outcomes of a randomized controlled trial. JMIR mHealth uHealth 2016, 4, e78. [Google Scholar] [CrossRef]
- Bertz, F.; Pacanowski, C.R.; Levitsky, D.A. Frequent self-weighing with electronic graphic feedback to prevent age-related weight gain in young adults. Obesity 2015, 23, 2009–2014. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.; Tate, D.; Espeland, M.; Lewis, C.; Gokee LaRose, J.; Gorin, A.; Bahnson, J.; Perdue, L.H.; Hatley, K.E.; Ferguson, E.; et al. Innovative Self-regulation strategies reduce weight gain in young adults: The study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. JAMA Intern. Med. 2016, 176, 755–762. [Google Scholar] [CrossRef]
- Stice, E.; Cameron, R.P.; Killen, J.D.; Hayward, C.; Taylor, C.B. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J. Consult. Clin. Psychol. 1999, 67, 967–974. [Google Scholar] [CrossRef]
- Stice, E.; Presnell, K.; Shaw, H.; Rohde, P. Psychological and behavioral risk factors for obesity onset in adolescent girls: A prospective study. J. Consult. Clin. Psychol. 2005, 73, 195–202. [Google Scholar] [CrossRef]
- Arcelus, J.; Mitchell, A.J.; Wales, J.; Nielsen, S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch. Gen. Psychiatry 2011, 68, 724–731. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D. Can we simultaneously work toward the prevention of obesity and eating disorders in children and adolescents? Int. J. Eat. Disord. 2005, 38, 220–227. [Google Scholar] [CrossRef]
- Leme, A.C.B.; Philippi, S.T.; Thompson, D.; Nicklas, T.; Baranowski, T. “Healthy Habits, Healthy Girls-Brazil”: An obesity prevention program with added focus on eating disorders. Eat. Weight Disord. 2019, 24, 107–119. [Google Scholar] [CrossRef]
- Tanofsky-Kraff, M.; Shomaker, L.B.; Wilfley, D.E.; Young, J.F.; Sbrocco, T.; Stephens, M.; Ranzenhofer, L.M.; Elliott, C.; Brady, S.; Radin, R.M.; et al. Targeted prevention of excess weight gain and eating disorders in high-risk adolescent girls: A randomized controlled trial. Am. J. Clin. Nutr. 2014, 100, 1010–1018. [Google Scholar] [CrossRef]
- Stice, E.; Marti, C.N.; Spoor, S.; Presnell, K.; Shaw, H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. J. Consult. Clin. Psychol. 2008, 76, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Rohde, P.; Gau, J.M.; Butryn, M.L.; Shaw, H.; Cloud, K.; D’Adamo, L. Enhancing efficacy of a dissonance-based obesity and eating disorder prevention program: Experimental therapeutics. J. Consult. Clin. Psychol. 2021, 89, 793–804. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Rohde, P.; Shaw, H.; Marti, C.N. Efficacy trial of a selective prevention program targeting both eating disorder symptoms and unhealthy weight gain among female college students. J. Consult. Clin. Psychol. 2012, 80, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Rohde, P.; Shaw, H.; Marti, C.N. Efficacy trial of a selective prevention program targeting both eating disorders and obesity among female college students: 1- and 2-year follow-up effects. J. Consult. Clin. Psychol. 2013, 81, 183–189. [Google Scholar] [CrossRef]
- Ghaderi, A.; Stice, E.; Andersson, G.; Eno Persson, J.; Allzen, E. A randomized controlled trial of the effectiveness of virtually delivered Body Project (vBP) groups to prevent eating disorders. J. Consult. Clin. Psychol. 2020, 88, 643–656. [Google Scholar] [CrossRef]
- Stice, E.; Rohde, P.; Shaw, H.; Gau, J.M. Clinician-led, peer-led, and internet-delivered dissonance-based eating disorder prevention programs: Effectiveness of these delivery modalities through 4-year follow-up. J. Consult. Clin. Psychol. 2020, 88, 481–494. [Google Scholar] [CrossRef]
- Stice, E.; Rohde, P.; Shaw, H.; Gau, J.M. An experimental therapeutics test of whether adding dissonance-induction activities improves the effectiveness of a selective obesity and eating disorder prevention program. Int. J. Obes. 2018, 42, 462–468. [Google Scholar] [CrossRef]
- Stice, E.; Shaw, H.; Burton, E.; Wade, E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. J. Consult. Clin. Psychol. 2006, 74, 263–275. [Google Scholar] [CrossRef]
- Babinski, D.E.; Sibley, M.H.; Ross, J.M.; Pelham, W.E. The effects of single versus mixed gender treatment for adolescent girls with ADHD. J. Clin. Child Adolesc. Psychol. 2013, 42, 243–250. [Google Scholar] [CrossRef]
- Hser, Y.I.; Evans, E.; Huang, D.; Messina, N. Long-term outcomes among drug-dependent mothers treated in women-only versus mixed-gender programs. J. Subst. Abus. Treat. 2011, 41, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Turner, L.H.; Dindia, K.; Pearson, J.C. An investigation of female/male verbal behaviors in same-sex and mixed-sex conversations. Commun. Rep. 1995, 8, 86–96. [Google Scholar] [CrossRef]
- Demos, K.E.; Heatherton, T.F.; Kelley, W.M. Individual differences in nucleus accumbens activity to food and sexual images predict weight gain and sexual behavior. J. Neurosci. 2012, 32, 5549–5552. [Google Scholar] [CrossRef]
- Stice, E.; Burger, K.S.; Yokum, S. Reward Region Responsivity Predicts Future Weight Gain and Moderating Effects of the TaqIA Allele. J. Neurosci. 2015, 35, 10316–10324. [Google Scholar] [CrossRef] [PubMed]
- Yokum, S.; Gearhardt, A.N.; Harris, J.L.; Brownell, K.D.; Stice, E. Individual differences in striatum activity to food commercials predict weight gain in adolescents. Obesity 2014, 22, 2544–2551. [Google Scholar] [CrossRef]
- Yokum, S.; Stice, E. Weight gain is associated with changes in neural response to palatable food tastes varying in sugar and fat and palatable food images: A repeated-measures fMRI study. Am. J. Clin. Nutr. 2019, 110, 1275–1286. [Google Scholar] [CrossRef]
- Calitri, R.; Pothos, E.M.; Tapper, K.; Brunstrom, J.M.; Rogers, P.J. Cognitive biases to healthy and unhealthy food words predict change in BMI. Obesity 2010, 18, 2282–2287. [Google Scholar] [CrossRef]
- Evans, G.W.; Fuller-Rowell, T.E.; Doan, S.N. Childhood cumulative risk and obesity: The mediating role of self-regulatory ability. Pediatrics 2012, 129, e68–e73. [Google Scholar] [CrossRef]
- Francis, L.A.; Susman, E.J. Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch. Pediatr. Adolesc. Med. 2009, 163, 297–302. [Google Scholar] [CrossRef]
- Schlam, T.R.; Wilson, N.L.; Shoda, Y.; Mischel, W.; Ayduk, O. Preschoolers’ delay of gratification predicts their body mass 30 years later. J. Pediatr. 2013, 162, 90–93. [Google Scholar] [CrossRef]
- Lawrence, N.S.; O’Sullivan, J.; Parslow, D.; Javaid, M.; Adams, R.C.; Chambers, C.D.; Kos, K.; Verbruggen, F. Training response inhibition to food is associated with weight loss and reduced energy intake. Appetite 2015, 95, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Veling, H.; van Koningsbruggen, G.M.; Aarts, H.; Stroebe, W. Targeting impulsive processes of eating behavior via the internet. Effects on body weight. Appetite 2014, 78, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Kakoschke, N.; Kemps, E.; Tiggemann, M. Attentional bias modification encourages healthy eating. Eat. Behav. 2014, 15, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Kemps, E.; Tiggemann, M.; Hollitt, S. Biased attentional processing of food cues and modification in obese individuals. Health Psychol. 2014, 33, 1391–1401. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Yokum, S.; Veling, H.; Kemps, E.; Lawrence, N.S. Pilot test of a novel food response and attention training treatment for obesity: Brain imaging data suggest actions shape valuation. Behav. Res. Ther. 2017, 94, 60–70. [Google Scholar] [CrossRef]
- Haines, J.; Neumark-Sztainer, D.; Wall, M.; Story, M. Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obesity 2007, 15, 2748–2760. [Google Scholar] [CrossRef]
- Weyers, A.M.; Mazzetti, S.A.; Love, D.M.; Gomez, A.L.; Kraemer, W.J.; Volek, J.S. Comparison of methods for assessing body composition changes during weight loss. Med. Sci. Sport. Exerc. 2002, 34, 497–502. [Google Scholar] [CrossRef]
- Wood, S.N.; Pya, N.; Safken, B. Smoothing parameter and model selection for general smooth models. J. Am. Stat. Assoc. 2016, 111, 1548–1563. [Google Scholar] [CrossRef]
- Burnham, K.; Anderson, D.; Huyvaert, K. AIC model selection and multimodel inference in behavioral ecology: Some background, observations, and comparisons. Behav. Ecol. Sociobiol. 2011, 65, 23–35. [Google Scholar] [CrossRef]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef]
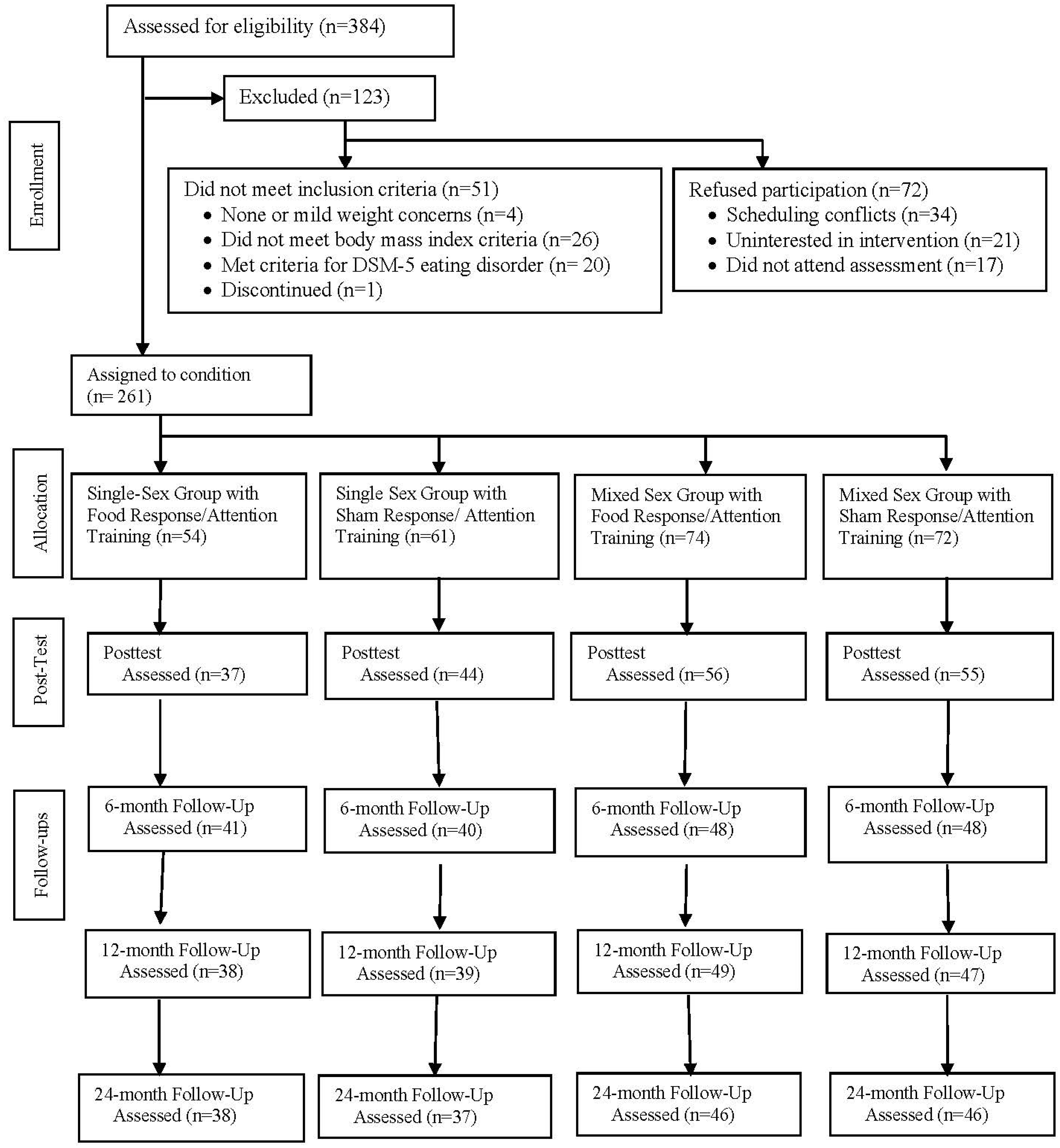
| Follow-Up | ||||||
|---|---|---|---|---|---|---|
| Condition | Outcome | Pretest | Posttest | 6-Month Follow-Up | 1-Year Follow-Up | 2-Year Follow-Up |
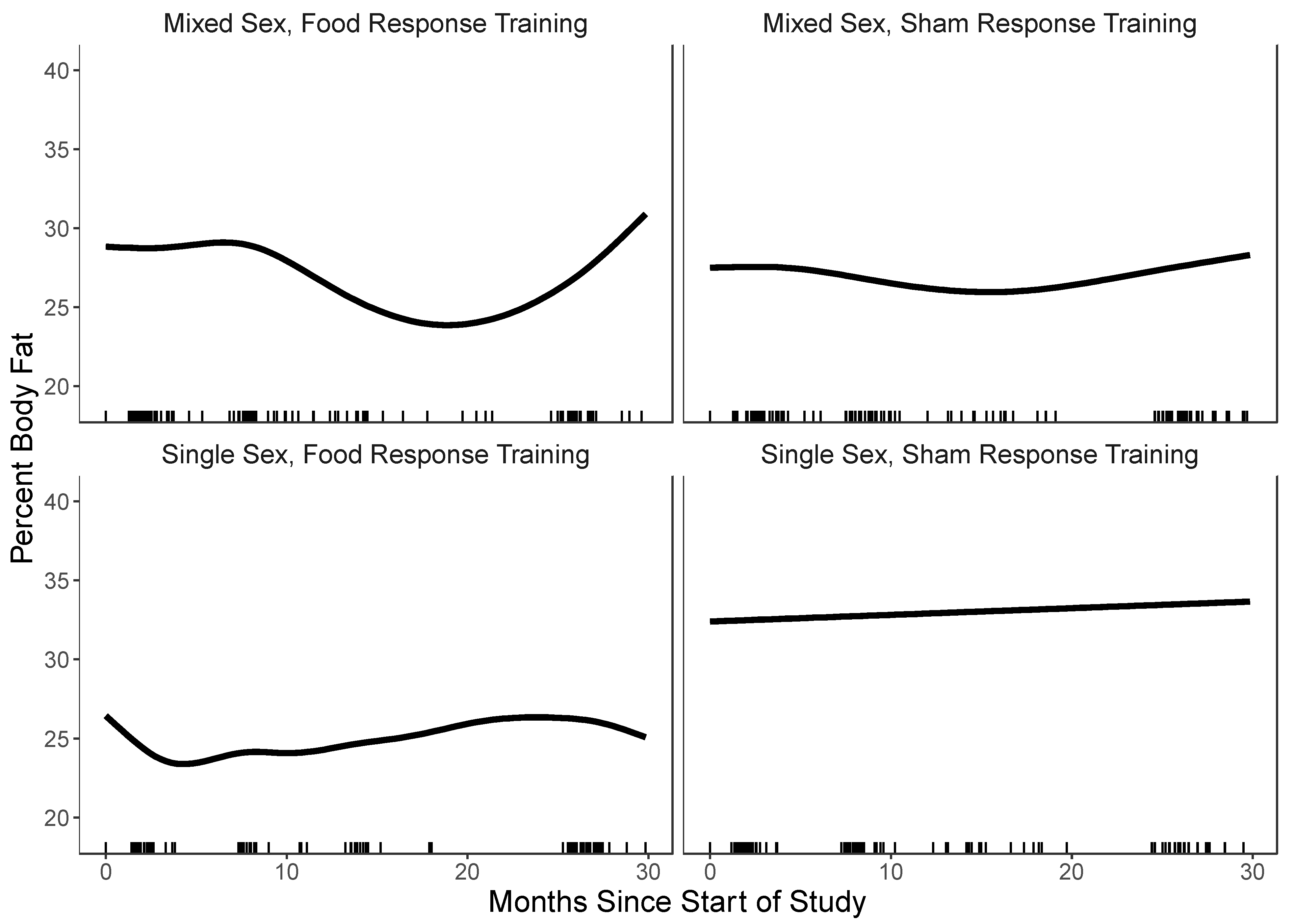
| Single-sex group with food response training | Body Fat | 26.84 (7.33) | 22.93 (6.62) | 23.23 (8.15) | 26.95 (6.58) | 24.13 (8.76) |
| Eating Disorder Symptoms | 12.46 (11.37) | 5.73 (5.92) | 5.12 (5.3) | 5.43 (5.3) | 6.11 (6.98) | |
| Single-sex group with sham training | Body Fat | 32.83 (6.74) | 32.71 (6.57) | 33.98 (7.36) | 31.79 (6.11) | 32.9 (9.28) |
| Eating Disorder Symptoms | 11.92 (8.82) | 6.91 (6.28) | 5.82 (4.53) | 4.44 (4.25) | 6.68 (10.59) | |
| Mixed-sex group with food response training | Body Fat | 29.2 (9.55) | 29.61 (7.65) | 29.94 (9.4) | 23.53 (11.16) | 25.73 (9.67) |
| Eating Disorder Symptoms | 12.56 (11.6) | 6.88 (6.06) | 6.45 (5.92) | 7.17 (7.71) | 5.52 (5.42) | |
| Mixed-sex group with sham training | Body Fat | 27.72 (9.84) | 29.21 (9.13) | 27.62 (75) | 28.59 (8.12) | 27.83 (9.23) |
| Eating Disorder Symptoms | 11.92 (11.89) | 7.87 (13.17) | 6.07 (5.75) | 3.98 (3.13) | 5.53 (5.53) | |
| Percent Body Fat | |||||
|---|---|---|---|---|---|
| T:G:RT | T:G and T:RT | T:G | T:RT | No Interactions | |
| df | 363.80 | 362.57 | 358.88 | 357.04 | 357.63 |
| AIC | 3533.96 | 3543.74 | 3555.18 | 3572.82 | 3573.49 |
| ΔAIC | 0 | 9.78 | 21.22 | 38.86 | 39.53 |
| Eating Disorder Symptoms | |||||
| T:G:RT | T:G and T:RT | T:G | T:RT | No Interactions | |
| df | 264.02 | 262.80 | 262.36 | 261.60 | 261.04 |
| AIC | 4917.85 | 4917.25 | 4917.95 | 4916.30 | 4916.72 |
| ΔAIC | 1.55 | 0.95 | 1.65 | 0 | 0.42 |
| Fixed Effects | Estimate | SE | t-Statistic | p-Value |
|---|---|---|---|---|
| Intercept | 28.18 | 1.08 | 26.00 | <0.001 |
| Single-Sex | −2.74 | 1.66 | −1.65 | 0.100 |
| Sham training | −0.87 | 1.55 | −0.56 | 0.573 |
| Single Sex:sham training | 8.16 | 2.32 | 3.51 | 0.001 |
| Smooth Functions | EDF | F-statistic | p-value | |
| Time | 0.80 | 0.80 | 0.810 | |
| Time:Mixed-Sex, Food Response Training | 4.07 | 3.79 | 0.010 | |
| Time:Single-Sex, Food Response Training | 4.60 | 2.91 | 0.010 | |
| Time:Mixed-Sex, Sham Training | 2.71 | 0.09 | 0.208 | |
| Time:Single-Sex, Sham Training | 0.80 | 0.80 | 0.790 | |
| Random Effects | EDF | F-statistic | p-value | |
| Random Intercept | 235.63 | 83.94 | <0.001 | |
| Random Slope | 110.28 | 52.376 | <0.001 |
| Condition | Did Not Develop Eating Disorder | Developed Eating Disorder |
|---|---|---|
| Single-sex group with food response training | 45 | 6 |
| Single-sex group with sham training | 55 | 3 |
| Mixed-sex group with food response training | 62 | 3 |
| Mixed-sex group with sham training | 53 | 3 |
| Condition | Did Not Transition to Unhealthy Weight | Transitioned to Unhealthy Weight |
| Single-sex group with food response training | 30 | 8 |
| Single-sex group with sham training | 37 | 8 |
| Mixed-sex group with food response training | 38 | 9 |
| Mixed-sex group with sham training | 43 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stice, E.; Rohde, P.; Butryn, M.L.; Desjardins, C.; Shaw, H. Enhancing Efficacy of a Brief Obesity and Eating Disorder Prevention Program: Long-Term Results from an Experimental Therapeutics Trial. Nutrients 2023, 15, 1008. https://doi.org/10.3390/nu15041008
Stice E, Rohde P, Butryn ML, Desjardins C, Shaw H. Enhancing Efficacy of a Brief Obesity and Eating Disorder Prevention Program: Long-Term Results from an Experimental Therapeutics Trial. Nutrients. 2023; 15(4):1008. https://doi.org/10.3390/nu15041008
Chicago/Turabian StyleStice, Eric, Paul Rohde, Meghan L. Butryn, Christopher Desjardins, and Heather Shaw. 2023. "Enhancing Efficacy of a Brief Obesity and Eating Disorder Prevention Program: Long-Term Results from an Experimental Therapeutics Trial" Nutrients 15, no. 4: 1008. https://doi.org/10.3390/nu15041008
APA StyleStice, E., Rohde, P., Butryn, M. L., Desjardins, C., & Shaw, H. (2023). Enhancing Efficacy of a Brief Obesity and Eating Disorder Prevention Program: Long-Term Results from an Experimental Therapeutics Trial. Nutrients, 15(4), 1008. https://doi.org/10.3390/nu15041008





