In-Hospital Formula Feeding Hindered Exclusive Breastfeeding: Breastfeeding Self-Efficacy as a Mediating Factor
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measurements
2.2.1. In-Hospital Formula Feeding (Exposure of Interest)
2.2.2. Breastfeeding Self-Efficacy (Mediator of Interest)
2.2.3. Exclusive Breastfeeding Outcomes
2.2.4. Covariates
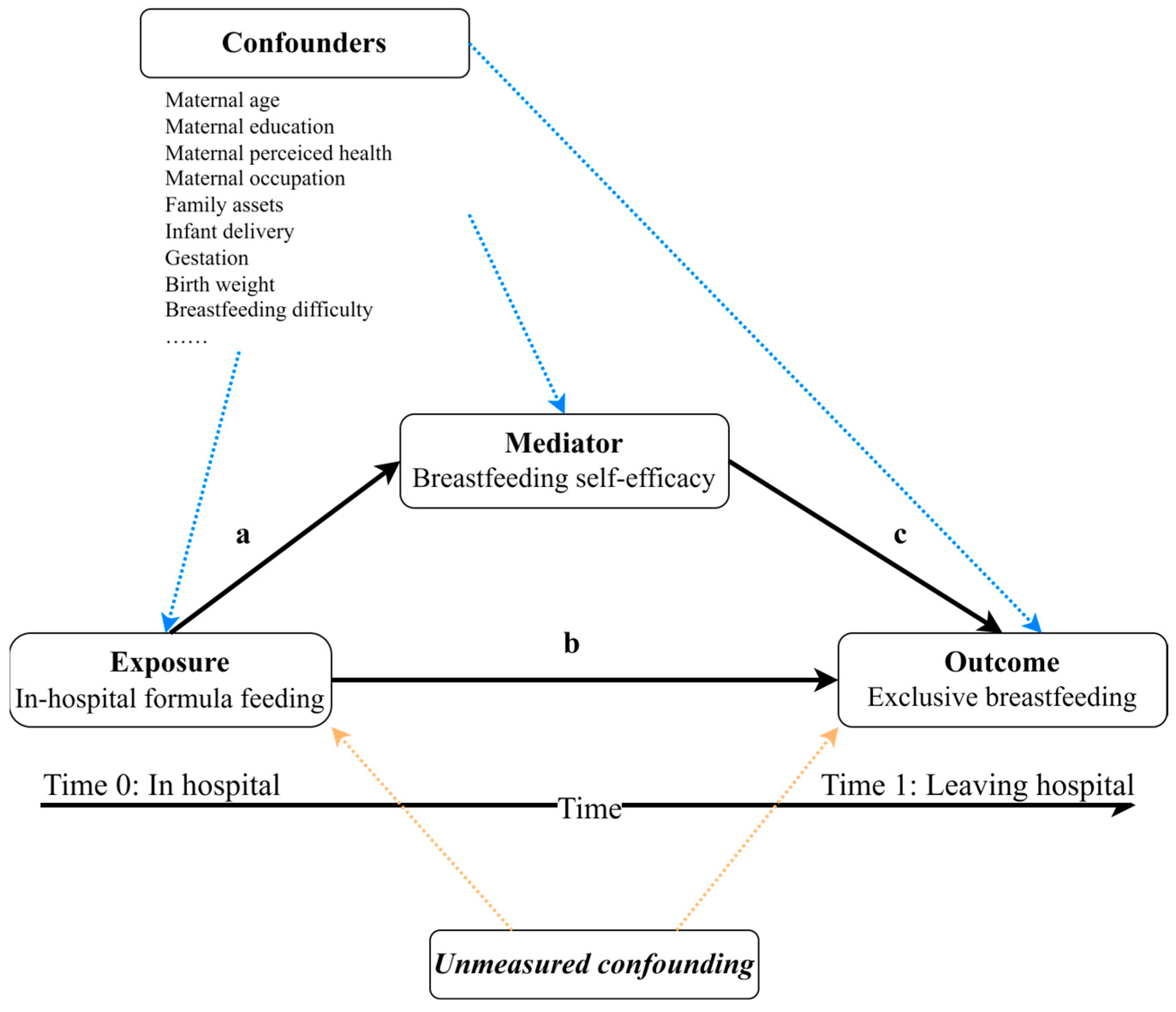
2.3. Assumed Causal Relationships
2.4. Analysis
3. Results
3.1. Summary Statistics
3.2. Associations between IHFF, BSE, and EBF Outcomes
3.3. Causal Mediation Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO; UNICEF. Indicators for Assessing Infant and Young Child Feeding Practices: Definitions and Measurement Methods; World Health Organization: Geneva, Switzerland, 2021; ISBN 9789240018389. [Google Scholar]
- Sankar, M.J.; Sinha, B.; Chowdhury, R.; Bhandari, N.; Taneja, S.; Martines, J.; Bahl, R. Optimal Breastfeeding Practices and Infant and Child Mortality: A Systematic Review and Meta-Analysis. Acta Paediatr. 2015, 104, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Bland, R.M.; Connelly, A.; Reilly, J.J. Impact of Adherence to WHO Infant Feeding Recommendations on Later Risk of Obesity and Non-Communicable Diseases: Systematic Review. Matern. Child. Nutr. 2016, 12, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Horta, B.L.; Loret de Mola, C.; Victora, C.G. Breastfeeding and Intelligence: A Systematic Review and Meta-Analysis. Acta Paediatr. 2015, 104, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, S.; Webb, E.L.; Calvert, C.; Glynn, J.R.; Sunny, B.S.; Crampin, A.C.; McLean, E.; Munthali-Mkandawire, S.; Lazarous Nkhata Dube, A.; Kalobekamo, F.; et al. Effects of Exclusive Breastfeeding on Educational Attainment and Longitudinal Trajectories of Grade Progression among Children in a 13-Year Follow-up Study in Malawi. Sci. Rep. 2023, 13, 11413. [Google Scholar] [CrossRef]
- Chowdhury, R.; Sinha, B.; Sankar, M.J.; Taneja, S.; Bhandari, N.; Rollins, N.; Bahl, R.; Martines, J. Breastfeeding and Maternal Health Outcomes: A Systematic Review and Meta-Analysis. Acta Paediatr. 2015, 104, 96–113. [Google Scholar] [CrossRef] [PubMed]
- WHO Breastfeeding(<6 Month). Available online: https://data.unicef.org/resources/dataset/breastfeeding/ (accessed on 7 March 2023).
- McAndrew, F.; Thompson, J.; Fellows, L.; Large, A.; Speed, M.; Renfrew, M.J. Infant Feeding Survey 2010; Health and Social Care Information Centre: Colchester, UK, 2010. [Google Scholar]
- Pérez-Escamilla, R.; Pollitt, E.; Lönnerdal, B.; Dewey, K.G. Infant Feeding Policies in Maternity Wards and Their Effect on Breast-Feeding Success: An Analytical Overview. Am. J. Public Health 1994, 84, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Escamilla, R.; Hromi-Fiedler, A.; Rhodes, E.C.; Neves, P.A.R.; Vaz, J.; Vilar-Compte, M.; Segura-Pérez, S.; Nyhan, K. Impact of Prelacteal Feeds and Neonatal Introduction of Breast Milk Substitutes on Breastfeeding Outcomes: A Systematic Review and Meta-Analysis. Matern. Child. Nutr. 2022, 18, e13368. [Google Scholar] [CrossRef]
- Chantry, C.J.; Dewey, K.G.; Peerson, J.M.; Wagner, E.A.; Nommsen-Rivers, L.A. In-Hospital Formula Use Increases Early Breastfeeding Cessation Among First-Time Mothers Intending to Exclusively Breastfeed. J. Pediatr. 2014, 164, 1339–1345.e5. [Google Scholar] [CrossRef]
- McCoy, M.B.; Heggie, P. In-Hospital Formula Feeding and Breastfeeding Duration. Pediatrics 2020, 146, e20192946. [Google Scholar] [CrossRef]
- Whipps, M.D.M.; Yoshikawa, H.; Demirci, J.R.; Hill, J. Estimating the Impact of In-Hospital Infant Formula Supplementation on Breastfeeding Success. Breastfeed. Med. 2021, 16, 530–538. [Google Scholar] [CrossRef]
- Segura-Pérez, S.; Richter, L.; Rhodes, E.C.; Hromi-Fiedler, A.; Vilar-Compte, M.; Adnew, M.; Nyhan, K.; Pérez-Escamilla, R. Risk Factors for Self-Reported Insufficient Milk during the First 6 Months of Life: A Systematic Review. Matern. Child. Nutr. 2022, 18, e13353. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J.M.; Perrine, C.G.; Scanlon, K.S.; Li, R. Provision of Non-Breast Milk Supplements to Healthy Breastfed Newborns in U.S. Hospitals, 2009 to 2013. Matern. Child Health J. 2016, 20, 2228–2232. [Google Scholar] [CrossRef] [PubMed]
- Boban, M.; Zakarija-Grković, I. In-Hospital Formula Supplementation of Healthy Newborns: Practices, Reasons, and Their Medical Justification. Breastfeed. Med. 2016, 11, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Parry, J.E.; Ip, D.K.M.; Chau, P.Y.K.; Wu, K.M.; Tarrant, M. Predictors and Consequences of In-Hospital Formula Supplementation for Healthy Breastfeeding Newborns. J. Hum. Lact. Off. J. Int. Lact. Consult. Assoc. 2013, 29, 527–536. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.L. Theoretical Underpinnings of Breastfeeding Confidence: A Self-Efficacy Framework. J. Hum. Lact. Off. J. Int. Lact. Consult. Assoc. 1999, 15, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Brockway, M.; Benzies, K.; Hayden, K.A. Interventions to Improve Breastfeeding Self-Efficacy and Resultant Breastfeeding Rates: A Systematic Review and Meta-Analysis. J. Hum. Lact. Off. J. Int. Lact. Consult. Assoc. 2017, 33, 486–499. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.-L. The Breastfeeding Self-Efficacy Scale: Psychometric Assessment of the Short Form. J. Obstet. Gynecol. Neonatal Nurs. JOGNN 2003, 32, 734–744. [Google Scholar] [CrossRef] [PubMed]
- Ip, W.-Y.; Gao, L.-L.; Choi, K.-C.; Chau, J.P.-C.; Xiao, Y. The Short Form of the Breastfeeding Self-Efficacy Scale as a Prognostic Factor of Exclusive Breastfeeding among Mandarin-Speaking Chinese Mothers. J. Hum. Lact. Off. J. Int. Lact. Consult. Assoc. 2016, 32, 711–720. [Google Scholar] [CrossRef]
- Nanishi, K.; Green, J.; Taguri, M.; Jimba, M. Determining a Cut-Off Point for Scores of the Breastfeeding Self-Efficacy Scale-Short Form: Secondary Data Analysis of an Intervention Study in Japan. PLoS ONE 2015, 10, e0129698. [Google Scholar] [CrossRef]
- Vehling, L.; Chan, D.; McGavock, J.; Becker, A.B.; Subbarao, P.; Moraes, T.J.; Mandhane, P.J.; Turvey, S.E.; Lefebvre, D.L.; Sears, M.R.; et al. Exclusive Breastfeeding in Hospital Predicts Longer Breastfeeding Duration in Canada: Implications for Health Equity. Birth 2018, 45, 440–449. [Google Scholar] [CrossRef]
- Ferguson, K.D.; McCann, M.; Katikireddi, S.V.; Thomson, H.; Green, M.J.; Smith, D.J.; Lewsey, J.D. Evidence Synthesis for Constructing Directed Acyclic Graphs (ESC-DAGs): A Novel and Systematic Method for Building Directed Acyclic Graphs. Int. J. Epidemiol. 2020, 49, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Ye, R.; Akhtar, M.; Dill, S.-E.; Yuan, P.; Zhou, H.; Rozelle, S. Adherence to Micronutrient Powder for Home Fortification of Foods among Infants and Toddlers in Rural China: A Structural Equation Modeling Approach. BMC Public Health 2022, 22, 2250. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Recommendations for Care of the Preterm or Low-Birth-Weight Infant; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Emsley, R.; Liu, H. PARAMED: Stata Module to Perform Causal Mediation Analysis Using Parametric Regression Models. Available online: https://econpapers.repec.org/software/bocbocode/s457581.htm (accessed on 7 August 2023).
- Linda, V.; Tyler, V. Mediation Analysis Allowing for Exposure-Mediator Interactions and Causal Interpretation: Theoretical Assumptions and Implementation with SAS and SPSS Macros. Psychol. Methods 2013, 18, 137. [Google Scholar] [CrossRef]
- Valente, M.J.; Rijnhart, J.J.M.; Smyth, H.L.; Muniz, F.B.; MacKinnon, D.P. Causal Mediation Programs in R, Mplus, SAS, SPSS, and Stata. Struct. Equ. Model. A Multidiscip. J. 2020, 27, 975–984. [Google Scholar] [CrossRef]
- Sugiyama, M.; Tsuchiya, K.J.; Okubo, Y.; Rahman, M.S.; Uchiyama, S.; Harada, T.; Iwabuchi, T.; Okumura, A.; Nakayasu, C.; Amma, Y.; et al. Outdoor Play as a Mitigating Factor in the Association Between Screen Time for Young Children and Neurodevelopmental Outcomes. JAMA Pediatr. 2023, 177, 303–310. [Google Scholar] [CrossRef]
- Robins, J.M.; Greenland, S. Identifiability and Exchangeability for Direct and Indirect Effects. Epidemiology 1992, 3, 143–155. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The Moderator-Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Wang, A.; Arah, O.A. G-Computation Demonstration in Causal Mediation Analysis. Eur. J. Epidemiol. 2015, 30, 1119–1127. [Google Scholar] [CrossRef]
- Pearl, J. Direct and Indirect Effects. In Probabilistic and Causal Inference: The Works of Judea Pearl; Association for Computing Machinery: New York, NY, USA, 2001; Volume 36, pp. 373–392. ISBN 978-1-4503-9586-1. [Google Scholar]
- VanderWeele, T.J.; Vansteelandt, S. Odds Ratios for Mediation Analysis for a Dichotomous Outcome. Am. J. Epidemiol. 2010, 172, 1339–1348. [Google Scholar] [CrossRef]
- Robins, J.M. Semantics of Causal DAG Models and the Identification of Direct and Indirect Effects. In Highly Structured Stochastic Systems; Green, P.J., Hjort, N.L., Richardson, S., Eds.; Oxford Statistical Science Series; Oxford University Press: Oxford, UK, 2003; ISBN 9780198510550. [Google Scholar]
- VanderWeele, T.J. Mediation Analysis: A Practitioner’s Guide. Annu. Rev. Public Health 2016, 37, 17–32. [Google Scholar] [CrossRef]
- Richiardi, L.; Bellocco, R.; Zugna, D. Mediation Analysis in Epidemiology: Methods, Interpretation and Bias. Int. J. Epidemiol. 2013, 42, 1511–1519. [Google Scholar] [CrossRef] [PubMed]
- Flaherman, V.J.; Aby, J.; Burgos, A.E.; Lee, K.A.; Cabana, M.D.; Newman, T.B. Effect of Early Limited Formula on Duration and Exclusivity of Breastfeeding in At-Risk Infants: An RCT. Pediatrics 2013, 131, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Escamilla, R.; Buccini, G.S.; Segura-Pérez, S.; Piwoz, E. Perspective: Should Exclusive Breastfeeding Still Be Recommended for 6 Months? Adv. Nutr. 2019, 10, 931–943. [Google Scholar] [CrossRef] [PubMed]
- Crowley, W.R. Neuroendocrine Regulation of Lactation and Milk Production. Compr. Physiol. 2015, 5, 255–291. [Google Scholar] [CrossRef] [PubMed]
- Uvnäs Moberg, K.; Ekström-Bergström, A.; Buckley, S.; Massarotti, C.; Pajalic, Z.; Luegmair, K.; Kotlowska, A.; Lengler, L.; Olza, I.; Grylka-Baeschlin, S.; et al. Maternal Plasma Levels of Oxytocin during Breastfeeding-A Systematic Review. PLoS ONE 2020, 15, e0235806. [Google Scholar] [CrossRef]
- Imboden, A.; Sobczak, B.; Kurilla, N.A. Impact of the Infant Formula Shortage on Breastfeeding Rates. J. Pediatr. Health Care Off. Publ. Natl. Assoc. Pediatr. Nurse Assoc. Pract. 2023, 37, 279–286. [Google Scholar] [CrossRef]
- Wilde, C.J.; Prentice, A.; Peaker, M. Breast-Feeding: Matching Supply with Demand in Human Lactation. Proc. Nutr. Soc. 1995, 54, 401–406. [Google Scholar] [CrossRef]
- Kondracki, A.J.; Valente, M.J.; Ibrahimou, B.; Bursac, Z. Risk of Large for Gestational Age Births at Early, Full and Late Term in Relation to Pre-Pregnancy Body Mass Index: Mediation by Gestational Diabetes Status. Paediatr. Perinat. Epidemiol. 2022, 36, 566–576. [Google Scholar] [CrossRef]
- Pérez-Escamilla, R.; Tomori, C.; Hernández-Cordero, S.; Baker, P.; Barros, A.J.D.; Bégin, F.; Chapman, D.J.; Grummer-Strawn, L.M.; McCoy, D.; Menon, P.; et al. Breastfeeding: Crucially Important, but Increasingly Challenged in a Market-Driven World. Lancet 2023, 401, 472–485. [Google Scholar] [CrossRef]
| Items | Not Confident at All | Not Confident | Okay | Confident | Always Confident |
|---|---|---|---|---|---|
| Determine that my child is getting enough milk | 1 | 2 | 3 | 4 | 5 |
| Successfully cope with breastfeeding like I have with other challenging tasks | 1 | 2 | 3 | 4 | 5 |
| Breastfeed my child without using formula as a supplement | 1 | 2 | 3 | 4 | 5 |
| Ensure that my child is properly latched on for the whole feeding | 1 | 2 | 3 | 4 | 5 |
| Manage the breastfeeding situation to my satisfaction | 1 | 2 | 3 | 4 | 5 |
| Manage to breastfeed even if my child is crying | 1 | 2 | 3 | 4 | 5 |
| Keep wanting to breastfeed | 1 | 2 | 3 | 4 | 5 |
| Comfortably breastfeed with my family members present | 1 | 2 | 3 | 4 | 5 |
| Be satisfied with my breastfeeding experience | 1 | 2 | 3 | 4 | 5 |
| Deal with the fact that breastfeeding can be time-consuming | 1 | 2 | 3 | 4 | 5 |
| Finish feeding my child on one breast before switching to the other breast | 1 | 2 | 3 | 4 | 5 |
| Continue to breastfeed my child for every feeding | 1 | 2 | 3 | 4 | 5 |
| Manage to keep up with my child’s breastfeeding demands | 1 | 2 | 3 | 4 | 5 |
| Tell when my child is finished breastfeeding | 1 | 2 | 3 | 4 | 5 |
| No. (%) | p-Value d | |
|---|---|---|
| IHFF | ||
| no | 105 (13.5) | - |
| yes | 673 (86.5) | - |
| BSE ** | 0.001 | |
| low | 404 (51.93) | |
| high | 374 (48.07) | |
| EBF | <0.001 | |
| no | 513 (65.94) | |
| yes | 265 (34.06) | |
| Maternal age a (year) | 28.6 (4.93) | 0.375 |
| Maternal education | 0.267 | |
| junior high school and below | 473 (60.8) | |
| high school and above | 305 (39.2) | |
| Maternal perceived personal health | 0.141 | |
| poor | 217 (27.89) | |
| good | 561 (72.11) | |
| Maternal occupation status | 0.418 | |
| unemployed | 616 (79.18) | |
| employed | 162 (20.82) | |
| Family assets | 0.98 | |
| poor | 401 (51.54) | |
| good | 377 (48.46) | |
| Infant delivery ** | 0.001 | |
| caesarean | 445 (57.2) | |
| vaginal | 333 (42.8) | |
| Infant age a (months) | 2.77 (1.73) | 0.4 |
| Infant sex | 0.397 | |
| male | 393 (50.51) | |
| female | 385 (49.49) | |
| Gestation | 0.413 | |
| preterm | 113 (14.52) | |
| full term | 665 (85.48) | |
| Birth weight (g) | 0.107 | |
| low birth weight | 47 (6.04) | |
| non-low birth weight | 731 (93.96) | |
| Breastfeeding difficulty b | 0.813 | |
| without difficulties | 33 (4.24) | |
| with difficulties | 745 (95.76) | |
| Pregnancy complications c | 0.571 | |
| no | 271 (34.83) | |
| yes | 507 (65.17) | |
| Parity ** | 0.007 | |
| multiparous | 486 (62.47) | |
| primiparous | 292 (37.53) |
| EBF | BSE | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| IHFF | ||||
| Crude | 0.41 | 0.27 to 0.63 | 0.50 | 0.33 to 0.76 |
| Adjusted a | 0.44 | 0.29 to 0.68 | 0.48 | 0.31 to 0.74 |
| BSE b | ||||
| Crude | 3.67 | 2.67 to 5.02 | ||
| Adjusted a | 3.90 | 2.80 to 5.43 | ||
| OR (95% CI) | |
|---|---|
| Total effect (TE b) | 0.47 (0.29 to 0.76) |
| Natural direct effect (NDE c) | 0.58 (0.36 to 0.94) |
| Natural indirect effect (NIE c) | 0.81 (0.72 to 0.91) |
| Percentage of indirect effect d | 28% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, L.; Wu, Y.; Xian, X.; Feng, J.; Mao, Y.; Balakrishnan, S.; Weber, A.M.; Darmstadt, G.L.; Chen, Y.; Sylvia, S.; et al. In-Hospital Formula Feeding Hindered Exclusive Breastfeeding: Breastfeeding Self-Efficacy as a Mediating Factor. Nutrients 2023, 15, 5074. https://doi.org/10.3390/nu15245074
Liu L, Wu Y, Xian X, Feng J, Mao Y, Balakrishnan S, Weber AM, Darmstadt GL, Chen Y, Sylvia S, et al. In-Hospital Formula Feeding Hindered Exclusive Breastfeeding: Breastfeeding Self-Efficacy as a Mediating Factor. Nutrients. 2023; 15(24):5074. https://doi.org/10.3390/nu15245074
Chicago/Turabian StyleLiu, Lu, Yuju Wu, Xiannan Xian, Jieyuan Feng, Yuping Mao, Siva Balakrishnan, Ann M. Weber, Gary L. Darmstadt, Yunwei Chen, Sean Sylvia, and et al. 2023. "In-Hospital Formula Feeding Hindered Exclusive Breastfeeding: Breastfeeding Self-Efficacy as a Mediating Factor" Nutrients 15, no. 24: 5074. https://doi.org/10.3390/nu15245074
APA StyleLiu, L., Wu, Y., Xian, X., Feng, J., Mao, Y., Balakrishnan, S., Weber, A. M., Darmstadt, G. L., Chen, Y., Sylvia, S., Zhou, H., & Rozelle, S. (2023). In-Hospital Formula Feeding Hindered Exclusive Breastfeeding: Breastfeeding Self-Efficacy as a Mediating Factor. Nutrients, 15(24), 5074. https://doi.org/10.3390/nu15245074








