A Prospective Comparison of Standard and Modified Acute Malnutrition Treatment Protocols during COVID-19 in South Sudan
Abstract
:1. Introduction
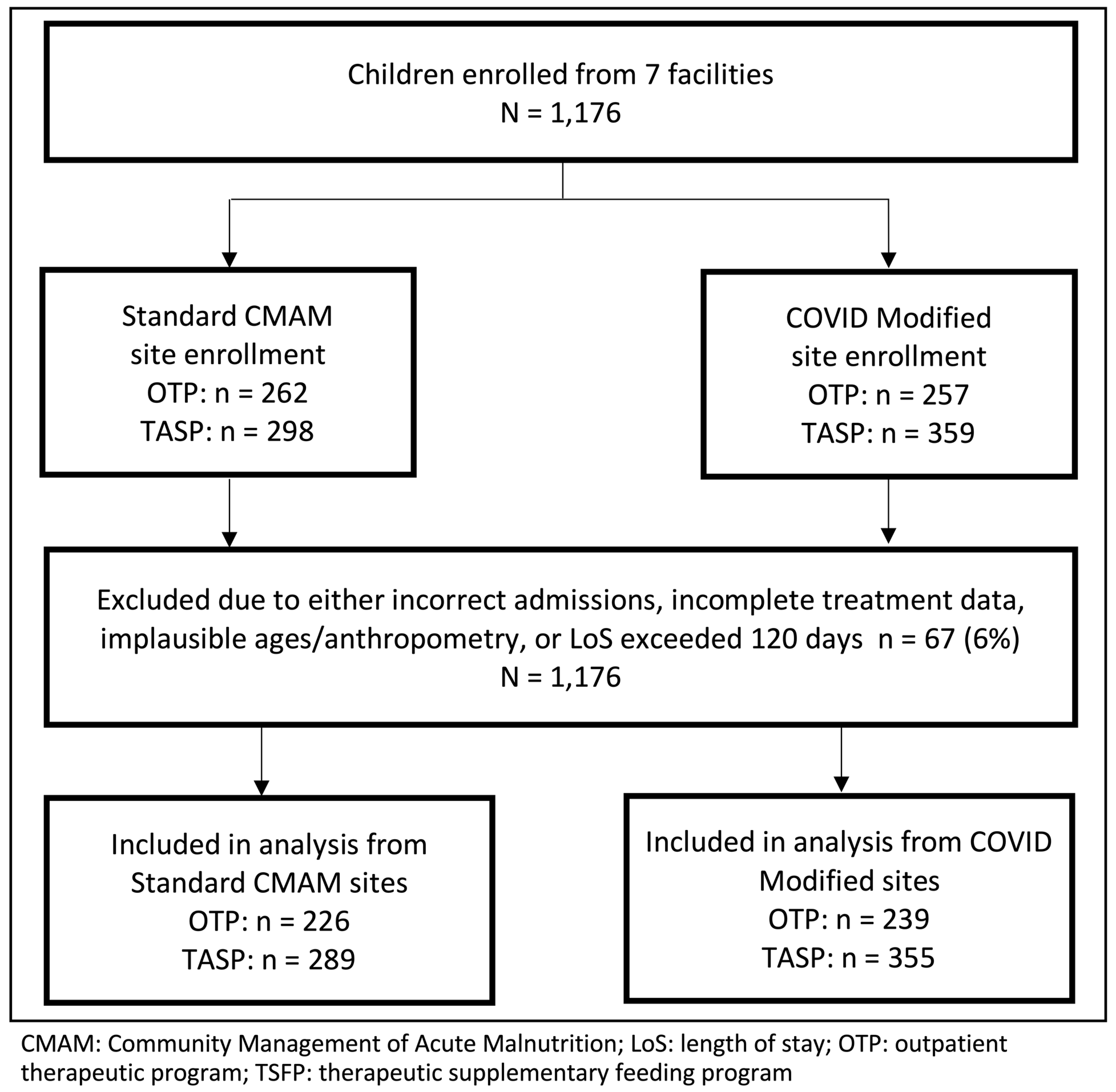
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| OTP Treatment | TSFP Treatment | |||||||
|---|---|---|---|---|---|---|---|---|
| Standard | Modified | Standard | Modified | |||||
| Unadjusted difference | Mean LoS (days) | Difference | Mean LoS (days) | Difference | ||||
| COVID-modified protocol * | 45.5 | 38.3 | −6.88 | (−21.8, 8.0) | 60.5 | 54.0 | −6.52 | (−22.1, 9.1) |
| Adjusted difference ** | ||||||||
| COVID-modified protocol | −6.44 | (−21.1, 7.6) | −5.08 | (−19.4, 8.5) | ||||
| Age at admission (months) | 0.3 | (−3.3, 3.8) | −0.1 | (−2.2, 2.0) | ||||
| Female, sex | 1.3 | (−3.5, 6.1) | −1.0 | (−3.8, 1.8) | ||||
| MUAC at admission (mm) | −1.9 | (−2.6, −1.1) | −2.2 | (−2.8,−1.6) | ||||
| Unadjusted odds | Recovery Rate (%) | Odds of Recovery | Recovery Rate (%) | Odds of Recovery | ||||
| COVID-modified protocol * | 83.3 | 93.3 | 2.67 | (0.99, 6.82) | 72.9 | 79.8 | 1.57 | (0.60, 4.20) |
| Adjusted odds ** | ||||||||
| COVID-modified protocol | 2.07 | (0.39, 9.57) | 1.55 | (0.35, 6.71) | ||||
| Age at admission (months) | 0.89 | (0.39, 2.06) | 1.19 | (0.79, 1.79) | ||||
| Female, sex | 1.44 | (0.77, 2.78) | 0.72 | (0.53, 0.97) | ||||
| MUAC at admission (mm) | 1.28 | (1.15, 1.44) | 1.40 | (1.28, 1.54) | ||||
References
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO); World Bank Group. Levels and Trends in Child Malnutrition. 2021. Available online: https://www.who.int/publications/i/item/9789240025257 (accessed on 16 May 2023).
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; De Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J.; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef] [PubMed]
- Olofin, I.; McDonald, C.M.; Ezzati, M.; Flaxman, S.; Black, R.E.; Fawzi, W.W.; Caulfield, L.E.; Danaei, G.; for the Nutrition Impact Model Study (anthropometry cohort pooling). Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: A pooled analysis of ten prospective studies. PLoS ONE 2013, 8, e64636. [Google Scholar] [CrossRef] [PubMed]
- Osendarp, S.; Akuoku, J.K.; Black, R.E.; Headey, D.; Ruel, M.; Scott, N.; Shekar, M.; Walker, N.; Flory, A.; Haddad, L.; et al. The COVID-19 crisis will exacerbate maternal and child undernutrition and child mortality in low-and middle-income countries. Nat. Food 2021, 2, 476–484. [Google Scholar] [CrossRef] [PubMed]
- UNICEF; Global Nutrition Cluster; Global Technical Assistance Mechanism for Nutrition. Management of Child Wasting in the Context of COVID-19. Brief No. 1. 2020. Available online: https://www.nutritioncluster.net/resources/management-child-wasting-context-covid-19-brief-no1-march-27th-2020 (accessed on 29 August 2022).
- UNICEF. Treatment of Wasting Using Simplified Approaches: A Rapid Evidence Review. 2020. Available online: https://www.unicef.org/documents/rapid-review-treatment-wasting-using-simplified-approaches (accessed on 16 May 2023).
- Action Against Hunger USA. State of the Evidence 2021: Modifications Aiming to Optimize Acute Malnutrition Treatment in Children Under Five. 2021. Available online: https://www.actionagainsthunger.org/app/uploads/2022/09/ActionAgainstHunger_StateoftheEvidence_CMAM_Modifications_8.21.pdf (accessed on 16 May 2023).
- WHO; UN Refugee Agency (UNHCR); UNICEF; World Food Program (WFP). Simplified Approaches for the Treatment of Child Wasting. 2019. Available online: https://www.who.int/news-room/events/detail/2019/03/26/defaultcalendar/simplified-approaches-for-the-treatment-of-child-wasting (accessed on 12 June 2023).
- UNICEF. Briefing Paper: Using Simplified Approaches in Exceptional Circumstances. 2022. Available online: https://www.simplifiedapproaches.org/_files/ugd/2bbe40_4d267de66e5d4af3a43cb799fc2b466d.pdf (accessed on 28 May 2023).
- King, S.; D’Mello-Guyett, L.; Yakowenko, E.; Riems, B.; Gallandat, K.; Mama Chabi, S.; Mohamud, F.A.; Ayoub, K.; Olad, A.H.; Aliou, B.; et al. A multi-country, prospective cohort study to measure rate and risk of relapse among children recovered from severe acute malnutrition in Mali, Somalia, and South Sudan: A study protocol. BMC Nutr. 2022, 8, 90. [Google Scholar] [CrossRef] [PubMed]
- South Sudan Ministry of Health. Community Management of Acute Malnutrition (CMAM) Guidelines. 2017. Available online: https://www.nutritioncluster.net/sites/nutritioncluster.com/files/2020-04/CMAM%20guidelines%20south%20sudan%202017.pdf (accessed on 29 August 2022).
- South Sudan Nutrition Cluster. South Sudan Nutrition Cluster Coordination Bi-Weekly Meeting Minutes: 20 August 2021. 2021. Available online: https://docs.google.com/document/d/1BQNheYDlJxxB5Ivs_bh7naWljk_E3Vok/edit (accessed on 1 September 2022).
- Fiske, I.; Chandler, R. Unmarked: An R package for fitting hierarchical models of wildlife occurrence and abundance. J. Stat. Softw. 2011, 43, 1–23. [Google Scholar] [CrossRef]
- Goodrich, B.; Gabry, J.; Ali, I.; Brilleman, S. Rstanarm: Bayesian Applied Regression Modeling via Stan. R Package Version 2.21.3. 2022. Available online: https://mc-stan.org/rstanarm (accessed on 12 June 2023).
- Stan Development Team. RStan: The R Interface to Stan. R Package Version 2.21.5. 2022. Available online: https://mc-stan.org/ (accessed on 12 June 2023).
- R Software; Version 4.0.3; R Core Team: Vienna, Austria, 2020.
- Sphere Association. The Sphere Handbook: Humanitarian Charter and Minimum Standards in Humanitarian Response, Fourth Edition. 2018. Available online: https://www.spherestandards.org/handbook (accessed on 12 June 2023).
- Lyles, E.; Banks, S.; Ramaswamy, M.; Ismail, S.; Leidman, E.; Doocy, S. Acute malnutrition recovery rates improve with COVID-19 adapted nutrition treatment protocols in South Sudan: A mixed methods study. BMC Nutr. 2023, 9, 46. [Google Scholar] [CrossRef] [PubMed]
- Lyles, E.; Ismail, S.; Ramaswamy, M.; Drame, A.; Leidman, E.; Doocy, S. Simplified treatment protocols improve recovery of children with severe acute malnutrition in South Sudan: Results from a mixed methods study. J. Health Popul. Nutr. 2023. submitted. [Google Scholar]
- The State of Acute Malnutrition. Tracker: Adaptations in the Management of Acute Malnutrition. Available online: https://acutemalnutrition.org/en/innovations-and-covid19-adaptations (accessed on 3 June 2023).
- Briend, A.; Maire, B.; Fontaine, O.; Garenne, M. Mid-upper arm circumference and weight-for-height to identify high-risk malnourished under-five children. Matern Child Nutr. 2012, 8, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Briend, A.; Alvarez, J.L.; Avril, N.; Bahwere, P.; Bailey, J.; Berkley, J.A.; Binns, P.; Blackwell, N.; Dale, N.; Deconinck, H.; et al. Low mid-upper arm circumference identifies children with a high risk of death who should be the priority target for treatment. BMC Nutr. 2016, 2, 63. [Google Scholar] [CrossRef]
- Grellety, E.; Golden, M.H. Weight-for-height and mid-upper-arm circumference should be used independently to diagnose acute malnutrition: Policy implications. BMC Nutr. 2016, 2, 10. [Google Scholar] [CrossRef]
- Leidman, E.; Couture, A.; Hulland, E.; Bilukha, O. Concordance between estimates of acute malnutrition measured by weight-for-height and by mid-upper arm circumference after age adjustment: Population-representative surveys from humanitarian settings. BMC Nutr. 2019, 5, 39. [Google Scholar] [CrossRef] [PubMed]
- Goossens, S.; Bekele, Y.; Yun, O.; Harczi, G.; Ouannes, M.; Shepherd, S. Mid-upper arm circumference based nutrition programming: Evidence for a new approach in regions with high burden of acute malnutrition. PLoS ONE 2012, 7, e49320. [Google Scholar] [CrossRef] [PubMed]
- Guesdon, B.; Couture, A.; Pantchova, D.; Bilukha, O. Potential consequences of expanded MUAC-only programs on targeting of acutely malnourished children and ready-to-use-therapeutic-food allocation: Lessons from cross-sectional surveys. BMC Nutr. 2020, 6, 5. [Google Scholar] [CrossRef] [PubMed]
- Grellety, E.; Krause, L.K.; Eldin, M.S.; Porten, K.; Isanaka, S. Comparison of weight-for-height and mid-upper arm circumference (MUAC) in a therapeutic feeding programme in South Sudan: Is MUAC alone a sufficient criterion for admission of children at high risk of mortality? Public Health Nutr. 2015, 18, 2575–2581. [Google Scholar] [CrossRef] [PubMed]
- Ahn, E.; Ouma, C.; Loha, M.; Dibaba, A.; Dyment, W.; Kim, J.; Beck, N.S.; Park, T. Do we need to reconsider the CMAM admission and discharge criteria? an analysis of CMAM data in South Sudan. BMC Public Health 2020, 20, 511. [Google Scholar] [CrossRef] [PubMed]
- Cazes, C.; Phelan, K.; Hubert, V.; Boubacar, H.; Bozama, L.I.; Sakubu, G.T.; Senge, B.B.; Baya, N.; Alitanou, R.; Kouamé, A.; et al. Optimising the dosage of ready-to-use therapeutic food in children with uncomplicated severe acute malnutrition in the Democratic Republic of the Congo: A non-inferiority, randomised controlled trial. EClinicalMedicine 2023, 58, 101878. [Google Scholar] [CrossRef] [PubMed]
| Standard Treatment Protocol | COVID-19 Modified Protocol | |
|---|---|---|
| Admission Criteria | MUAC AND/OR WHZ AND/OR bilateral pedal edema | MUAC AND/OR bilateral pedal edema |
| OTP: MUAC < 115 mm, WHZ < −3 TSFP: MUAC 115–124 mm, −3 ≤ WHZ <−2 | OTP: MUAC < 115 mm TSFP: MUAC 115–124 mm | |
| Simplified Ration Dosing | OTP: Weight-based RUTF dosing TSFP: One RUSF sachet daily | OTP: Two RUTF sachets per day TSFP: One RUSF sachet daily |
| OTP: Weekly distribution TSFP: Bi-weekly distribution | OTP: Weekly distribution TSFP: Bi-weekly distribution | |
| Discharge Criteria | Meets MUAC or WHZ criteria (same criteria as used for admission) for two consecutive visits | Meets MUAC criteria for two consecutive visits |
| OTP: MUAC ≥ 115 mm OR WHZ ≥ −3 TSFP: MUAC ≥ 12.5 cm OR WHZ ≥ −2 | OTP: MUAC ≥ 115 mm TSFP: MUAC ≥ 125 mm |
| All Children | Enrollment at OTP | Enrollment at TSFP | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Standard CMAM | COVID Modified | p-Value | Standard CMAM | COVID Modified | p-Value | Standard CMAM | COVID Modified | p-Value | |
| n = 515 | n = 594 | n = 226 | n = 239 | n = 289 | n = 355 | ||||
| Child characteristics | |||||||||
| Female | 57.3% | 54.9% | 0.42 | 53.1% | 54.8% | 0.71 | 60.5% | 54.9% | 0.15 |
| Age in months, mean ± SD | 18.0 ± 9.7 | 20.5 ± 11.2 | <0.001 | 18.3 ± 10.3 | 19.7 ± 11.3 | 0.18 | 17.7 ± 9.3 | 21.0 ± 11.0 | <0.001 |
| <24 months | 76.3% | 65.5% | <0.001 | 74.8% | 66.7% | 0.26 | 77.5% | 64.8% | <0.001 |
| ≥24 months | 23.7% | 34.5% | 25.2% | 33.3% | 22.5% | 35.2% | |||
| Currently breastfed | 68.3% | 63.0% | 0.03 | 68.1% | 65.7% | 0.57 | 68.5% | 61.1% | 0.05 |
| Caregiver characteristics | |||||||||
| Caregiver is female | 98.5% | 100% | 0.002 | 99.1% | 100% | 0.15 | 97.9% | 100% | 0.006 |
| Caregiver age | |||||||||
| ≤18 years | 1.9% | 2.4% | 0.008 | 1.8% | 2.9% | 0.02 | 2.1% | 2.0% | 0.20 |
| 19–37 years | 74.6% | 71.0% | 72.1% | 69.0% | 76.5% | 72.4% | |||
| 38–58 years | 13.6% | 10.3% | 14.6% | 8.4% | 12.8% | 11.6% | |||
| Age unknown | 9.9% | 16.3% | 11.5% | 19.7% | 8.7% | 14.1% | |||
| Caregiver married | 95.7% | 86.5% | <0.001 | 96.9% | 83.7% | <0.001 | 94.8% | 88.5% | 0.004 |
| Caregiver has no formal education | 77.7% | 81.0% | 0.17 | 80.1% | 84.5% | 0.21 | 75.8% | 78.6% | 0.40 |
| Household characteristics | |||||||||
| Female head of household | 71.8% | 75.3% | 0.20 | 67.7% | 78.7% | 0.008 | 75.1% | 73.0% | 0.54 |
| Household size, mean ± SD | 7.7 ± 4.6 | 9.8 ± 10.3 | <0.001 | 8.1 ± 6.5 | 10.3 ± 12.0 | 0.01 | 7.4 ± 2.3 | 9.4 ± 8.9 | <0.001 |
| Currently displaced | 5.8% | 3.2% | 0.03 | 6.2% | 0.8% | 0.002 | 5.6% | 4.8% | 0.66 |
| Received assistance in past 3 months | 7.4% | 4.9% | 0.08 | 7.5% | 3.8% | 0.08 | 7.3% | 5.6% | 0.40 |
| Household hunger score, mean ± SD | 2.2 ± 1.1 | 2.7 ± 0.9 | <0.001 | 2.1 ± 1.1 | 2.7 ± 0.9 | <0.001 | 2.3 ± 1.1 | 2.7 ± 0.9 | <0.001 |
| Little to no hunger | 25.1% | 11.4% | <0.001 | 30.4% | 12.9% | <0.001 | 20.9% | 10.4% | 0.001 |
| Moderate hunger | 72.6% | 85.8% | 67.0% | 85.8% | 77.0% | 85.8% | |||
| Severe hunger | 2.4% | 2.8% | 2.7% | 1.3% | 2.1% | 3.8% | |||
| Meals consumed the previous day, mean ± SD | 1.5 ± 0.6 | 1.6 ± 0.6 | 0.05 | 1.6 ± 0.5 | 1.7 ± 0.6 | 0.08 | 1.5 ± 0.6 | 1.6 ± 0.6 | 0.17 |
| Distance to a treatment facility (km), mean ± SD | 5.7 ± 4.8 | 5.1 ± 4.3 | 0.01 | 5.6 ± 5.0 | 5.0 ± 4.3 | 0.20 | 5.9 ± 4.6 | 5.1 ± 4.2 | 0.03 |
| OTP Treatment | TSFP Treatment | |||||
|---|---|---|---|---|---|---|
| Standard CMAM | COVID Modified | p-Value | Standard CMAM | COVID Modified | p-Value | |
| n = 226 | n = 239 | n = 429 | n = 471 | |||
| Admission anthropometry | ||||||
| MUAC, mean ± SD | 11.5 ± 0.6 | 11.2 ± 0.3 | <0.001 | 12.1 ± 0.3 | 12.1 ± 0.2 | 0.13 |
| MUAC < 11.5 cm | 58.9% | 100% | 0.0% | 0.0% | ||
| 11.5 cm ≤ MUAC < 12.5 cm | 39.4% | 0.0% | 90.0% | 100% | ||
| MUAC ≥ 12.5 cm | 1.8% | 0.0% | 10.0% | 0.0% | ||
| WHZ, mean ± SD | (−3.2) ± 0.8 | (−2.1) ± 0.7 | ||||
| WHZ < −3 | 67.7% | 7.0% | ||||
| −3 ≤ WHZ < −2 | 24.3% | 51.4% | ||||
| WHZ ≥ −2 | 8.0% | 41.6% | ||||
| Discharge anthropometry | ||||||
| MUAC, mean ± SD | 12.0 ± 0.5 | 11.8 ± 0.2 | <0.001 | 12.6 ± 0.6 | 12.6 ± 0.5 | 0.82 |
| MUAC < 11.5 cm | 8.9% | 6.3% | 7.2% | 8.1% | ||
| 11.5 cm ≤ MUAC < 12.5 cm | 72.6% | 92.9% | 17.5% | 12.1% | ||
| MUAC ≥ 12.5 cm | 18.6% | 0.8% | 75.3% | 79.8% | ||
| Total MUAC gain (cm) | 0.5 ± 0.4 | 0.6 ± 0.3 | 0.02 | 0.5 ± 0.5 | 0.5 ± 0.5 | 0.55 |
| Average MUAC gain per day (mm/day) | 0.16 ± 0.2 | 0.2 ± 0.2 | <0.001 | 0.07 ± 0.1 | 0.1 ± 0.2 | 0.002 |
| Time in treatment | ||||||
| Length of stay (days) Mean ± SD | 42.8 ± 21.7 | 38.3 ± 24.1 | 0.03 | 61.9 ± 21.9 | 54.0 ± 21.7 | <0.001 |
| Median (IQR) † | 35 (29) | 28 (32) | <0.001 | 58 (35) | 55 (33) | <0.001 |
| Time to recovery (days) Mean ± SD | 40.2 ± 18.5 | 37.0 ± 23.0 | 0.12 | 61.3 ± 19.0 | 51.2 ± 19.7 | <0.001 |
| Median (IQR) † | 35 (22) | 28 (28) | <0.001 | 58 (27.5) | 50 (29.5) | <0.001 |
| Time to recovery (days) excluding LoS > 90 Mean ± SD | 39.0 ± 16.8 | 34.1 ± 19.0 | 0.006 | 57.7 ± 15.9 | 50.4 ± 18.9 | <0.001 |
| Median (IQR) † | 35 (22) | 28 (22) | <0.001 | 58 (27) | 49 (30) | <0.001 |
| Discharge outcomes * | ||||||
| Recovered | 87.2% | 93.3% | 0.03 | 72.7% | 79.8% | 0.01 |
| Default | 0.0% | 0.0% | 8.9% | 7.6% | ||
| Traditional default | 0.0% | 0.0% | 1.6% | 1.1% | ||
| Default due to stock-out | 0.0% | 0.0% | 7.2% | 6.6% | ||
| Non-responsive | 11.5% | 5.0% | 4.2% | 1.9% | ||
| Transferred | ||||||
| Transfer to OTP | 0.0% | 0.0% | 8.4% | 7.2% | ||
| Transfer to a new facility | 0.4% | 0.4% | 2.6% | 2.1% | ||
| Transfer to inpatient care | 0.4% | 0.8% | 0.2% | 0.0% | ||
| Death | 0.0% | 0.0% | 0.0% | 0.2% | ||
| Improper/Early discharge | 0.4% | 0.4% | 3.0% | 1.1% | ||
| OTP Treatment | TSFP Treatment | |||||||
|---|---|---|---|---|---|---|---|---|
| Standard | Modified | Standard | Modified | |||||
| Unadjusted difference | Mean LoS (days) | Difference | Mean LoS (days) | Difference | ||||
| COVID-modified protocol * | 42.9 | 38.3 | −4.8 | (−20.8, 9.1) | 61.8 | 54.0 | −6.92 | (−21.6, 9.0) |
| Adjusted difference ** | ||||||||
| COVID-modified protocol | −9.95 | (−25.3, 4.7) | −7.75 | (−21.7, 6.8) | ||||
| Age at admission (months) | 0.7 | (−2.3, 3.8) | −0.2 | (−2.2, 1.8) | ||||
| Female, sex | −0.1 | (−4.1, 3.9) | −1.7 | (−4.4, 1.1) | ||||
| MUAC at admission (mm) | −1.1 | (−1.5, −0.6) | −1.3 | (−1.8, −0.8) | ||||
| Unadjusted odds | Recovery Rate (%) | Odds of Recovery | Recovery Rate (%) | Odds of Recovery | ||||
| COVID-modified protocol * | 86.7 | 93.3 | 2.09 | (0.77, 5.60) | 72.7 | 79.8 | 1.37 | (0.47, 3.98) |
| Adjusted odds ** | ||||||||
| COVID-modified protocol | 2.63 | (0.70, 9.09) | 1.80 | (0.42, 7.24) | ||||
| Age at admission (months) | 1.08 | (0.55, 2.13) | 1.09 | (0.76, 1.55) | ||||
| Female, sex | 1.20 | (0.72, 2.12) | 0.77 | (0.59, 1.00) | ||||
| MUAC at admission (mm) | 1.16 | (1.08, 1.25) | 1.28 | (1.19, 1.38) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doocy, S.; King, S.; Ismail, S.; Leidman, E.; Stobaugh, H.; The Action Against Hunger/US Centers for Disease Control and Prevention Study Team. A Prospective Comparison of Standard and Modified Acute Malnutrition Treatment Protocols during COVID-19 in South Sudan. Nutrients 2023, 15, 4853. https://doi.org/10.3390/nu15234853
Doocy S, King S, Ismail S, Leidman E, Stobaugh H, The Action Against Hunger/US Centers for Disease Control and Prevention Study Team. A Prospective Comparison of Standard and Modified Acute Malnutrition Treatment Protocols during COVID-19 in South Sudan. Nutrients. 2023; 15(23):4853. https://doi.org/10.3390/nu15234853
Chicago/Turabian StyleDoocy, Shannon, Sarah King, Sule Ismail, Eva Leidman, Heather Stobaugh, and The Action Against Hunger/US Centers for Disease Control and Prevention Study Team. 2023. "A Prospective Comparison of Standard and Modified Acute Malnutrition Treatment Protocols during COVID-19 in South Sudan" Nutrients 15, no. 23: 4853. https://doi.org/10.3390/nu15234853
APA StyleDoocy, S., King, S., Ismail, S., Leidman, E., Stobaugh, H., & The Action Against Hunger/US Centers for Disease Control and Prevention Study Team. (2023). A Prospective Comparison of Standard and Modified Acute Malnutrition Treatment Protocols during COVID-19 in South Sudan. Nutrients, 15(23), 4853. https://doi.org/10.3390/nu15234853






