The Intuitive Eating Scale-2 Adapted for Mexican Pregnant Women: Psychometric Properties and Influence of Sociodemographic Variables
Abstract
1. Introduction
2. Materials and Methods
2.1. Scale Adaptation
2.2. Assessment of Psychometric Properties
2.2.1. Participants and Procedures
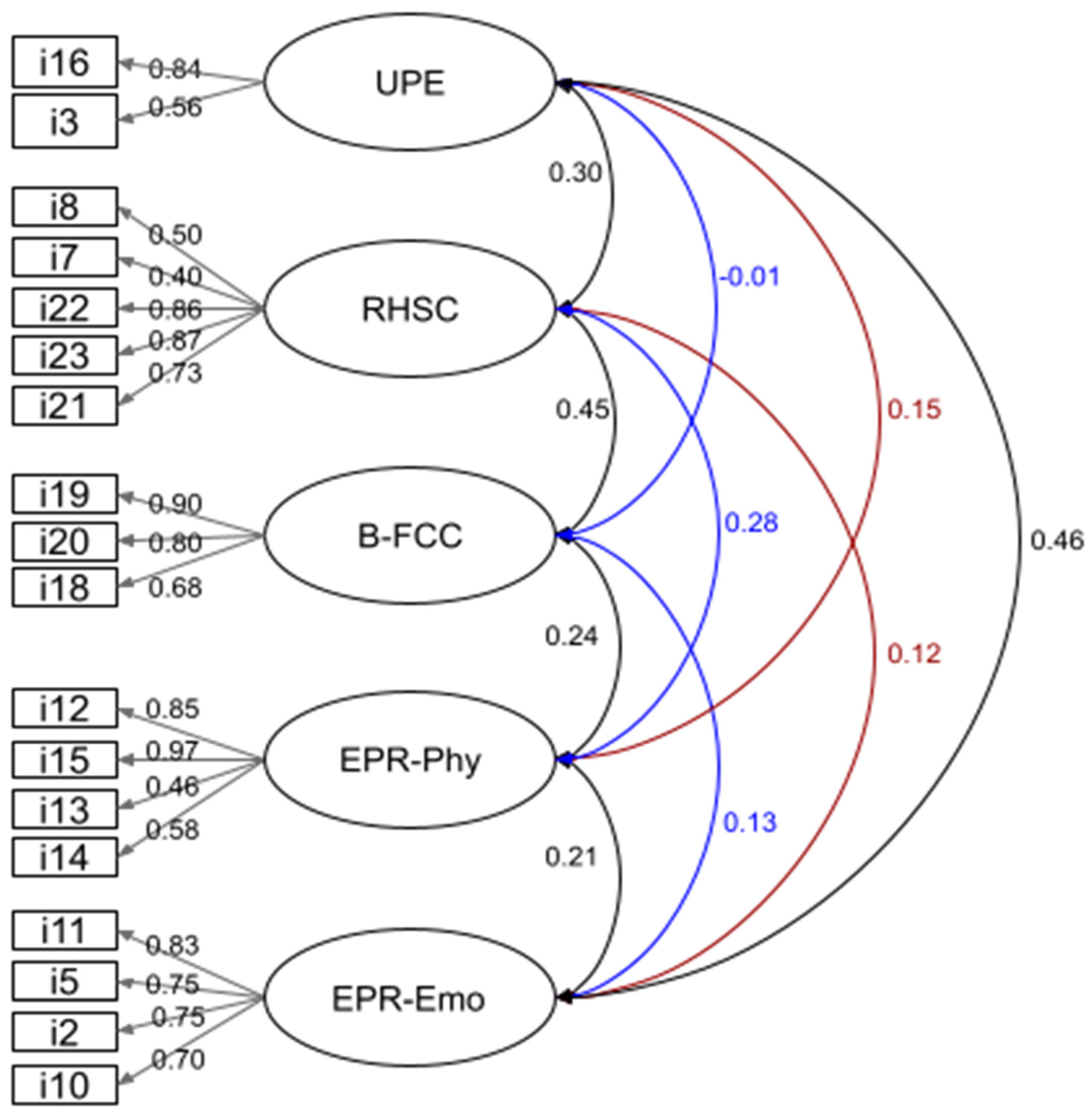
2.2.2. Reliability and Factor Analyses
2.3. Intuitive Eating and Sociodemographic Variables
3. Results
3.1. Psychometric Properties of the Adapted Scale
3.1.1. Participants’ Characteristics
3.1.2. Reliability Tests and Factor Analyses
3.2. Associations and Regression Analysis among Intuitive Eating Traits, and with Psychosocial and Reproductive Variables
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bacon, L.; Aphramor, L. Weight Science: Evaluating the Evidence for a Paradigm Shift. Nutr. J. 2011, 10, 9. [Google Scholar] [CrossRef] [PubMed]
- Tylka, T.L.; Annunziato, R.A.; Burgard, D.; Daníelsdóttir, S.; Shuman, E.; Davis, C.; Calogero, R.M. The Weight-Inclusive versus Weight-Normative Approach to Health: Evaluating the Evidence for Prioritizing Well-Being over Weight Loss. J. Obes. 2014, 2014, 983495. [Google Scholar] [CrossRef] [PubMed]
- National Research Council; Institute of Medicine; Board on Children, Youth, and Families; Food and Nutrition Board; Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain during Pregnancy: Reexamining the Guidelines; National Academies Press: Washington, DC, USA, 2010; ISBN 9780309131131. [Google Scholar]
- International Weight Management in Pregnancy (i-WIP) Collaborative Group. Effect of Diet and Physical Activity Based Interventions in Pregnancy on Gestational Weight Gain and Pregnancy Outcomes: Meta-Analysis of Individual Participant Data from Randomised Trials. BMJ 2017, 358, j3119. [Google Scholar] [CrossRef]
- Tylka, T.L. Development and Psychometric Evaluation of a Measure of Intuitive Eating. J. Couns. Psychol. 2006, 53, 226–240. [Google Scholar] [CrossRef]
- Tylka, T.L.; Van Diest, A.M.K. The Intuitive Eating Scale-2: Item Refinement and Psychometric Evaluation with College Women and Men. J. Couns. Psychol. 2013, 60, 137–153. [Google Scholar] [CrossRef]
- Ledoux, T.; Daundasekara, S.S.; Beasley, A.; Robinson, J.; Sampson, M. The Association between Pre-Conception Intuitive Eating and Gestational Weight Gain. Eat. Weight Disord. 2021, 26, 467–474. [Google Scholar] [CrossRef]
- Lee, M.F.; Williams, S.L.; Burke, K.J. Striving for the Thin Ideal Post-Pregnancy: A Cross-Sectional Study of Intuitive Eating in Postpartum Women. J. Reprod. Infant Psychol. 2020, 38, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Paterson, H.; Treharne, G.J.; Horwath, C.; Haszard, J.J.; Herbison, P.; Hay-Smith, E.J.C. Intuitive Eating and Gestational Weight Gain. Eat. Behav. 2019, 34, 101311. [Google Scholar] [CrossRef]
- Daundasekara, S.S.; Beasley, A.D.; O’Connor, D.P.; Sampson, M.; Hernandez, D.; Ledoux, T. Validation of the Intuitive Eating Scale for Pregnant Women. Appetite 2017, 112, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Paterson, H.; Hay-Smith, J.; Treharne, G.; Herbison, P.; Howarth, C. Validation of the Intuitive Eating Scale in Pregnancy. J. Health Psychol. 2018, 23, 701–709. [Google Scholar] [CrossRef] [PubMed]
- Plante, A.-S.; Savard, C.; Lemieux, S.; Carbonneau, É.; Robitaille, J.; Provencher, V.; Morisset, A.-S. Trimester-Specific Intuitive Eating in Association with Gestational Weight Gain and Diet Quality. J. Nutr. Educ. Behav. 2019, 51, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Quansah, D.Y.; Gross, J.; Gilbert, L.; Helbling, C.; Horsch, A.; Puder, J.J. Intuitive Eating Is Associated with Weight and Glucose Control during Pregnancy and in the Early Postpartum Period in Women with Gestational Diabetes Mellitus (GDM): A Clinical Cohort Study. Eat. Behav. 2019, 34, 101304. [Google Scholar] [CrossRef] [PubMed]
- Savard, C.; Yan, E.; Plante, A.-S.; Bégin, C.; Robitaille, J.; Michaud, A.; Lemieux, S.; Provencher, V.; Morisset, A.-S. Positive Attitudes toward Weight Gain in Late Pregnancy Are Associated with Healthy Eating Behaviours. Eat. Weight Disord. 2021, 26, 2051–2058. [Google Scholar] [CrossRef]
- Anastasiades, E.; Maïano, C.; Argyrides, M.; Swami, V. Psychometric Properties of a Greek Translation of the Intuitive Eating Scale-2 (IES-2) in Adults from Cyprus. Body Image 2022, 43, 348–361. [Google Scholar] [CrossRef] [PubMed]
- Bas, M.; Karaca, K.E.; Saglam, D.; Arıtıcı, G.; Cengiz, E.; Köksal, S.; Buyukkaragoz, A.H. Turkish Version of the Intuitive Eating Scale-2: Validity and Reliability among University Students. Appetite 2017, 114, 391–397. [Google Scholar] [CrossRef]
- Carbonneau, E.; Carbonneau, N.; Lamarche, B.; Provencher, V.; Bégin, C.; Bradette-Laplante, M.; Laramée, C.; Lemieux, S. Validation of a French-Canadian Adaptation of the Intuitive Eating Scale-2 for the Adult Population. Appetite 2016, 105, 37–45. [Google Scholar] [CrossRef]
- da Silva, W.R.; Neves, A.N.; Ferreira, L.; Campos, J.A.D.B.; Swami, V. A Psychometric Investigation of Brazilian Portuguese Versions of the Caregiver Eating Messages Scale and Intuitive Eating Scale-2. Eat. Weight Disord. 2020, 25, 221–230. [Google Scholar] [CrossRef]
- Fekih-Romdhane, F.; Jiang, C.; Obeid, S.; Malaeb, D.; Chammas, N.; Fawaz, M.; Soufia, M.; Meng, R.; Hallit, S. Psychometric Properties of the Arabic Version of the Intuitive Eating Scale-2 (IES-2) in a Sample of Community Adults. J. Eat. Disord. 2023, 11, 53. [Google Scholar] [CrossRef]
- Nejati, B.; Fan, C.-W.; Boone, W.J.; Griffiths, M.D.; Lin, C.-Y.; Pakpour, A.H. Validating the Persian Intuitive Eating Scale-2 among Breast Cancer Survivors Who Are Overweight/Obese. Eval. Health Prof. 2021, 44, 385–394. [Google Scholar] [CrossRef]
- Ruzanska, U.A.; Warschburger, P. Psychometric Evaluation of the German Version of the Intuitive Eating Scale-2 in a Community Sample. Appetite 2017, 117, 126–134. [Google Scholar] [CrossRef]
- Swami, V.; Todd, J.; Zahari, H.S.; Mohd Khatib, N.A.; Toh, E.K.L.; Barron, D. Dimensional Structure, Psychometric Properties, and Sex and Ethnic Invariance of a Bahasa Malaysia (Malay) Translation of the Intuitive Eating Scale-2 (IES-2). Body Image 2020, 32, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Swami, V.; Maïano, C.; Todd, J.; Ghisi, M.; Cardi, V.; Bottesi, G.; Cerea, S. Dimensionality and Psychometric Properties of an Italian Translation of the Intuitive Eating Scale-2 (IES-2): An Assessment Using a Bifactor Exploratory Structural Equation Modelling Framework. Appetite 2021, 166, 105588. [Google Scholar] [CrossRef] [PubMed]
- Vintilă, M.; Todd, J.; Goian, C.; Tudorel, O.; Barbat, C.A.; Swami, V. The Romanian Version of the Intuitive Eating Scale-2: Assessment of Its Psychometric Properties and Gender Invariance in Romanian Adults. Body Image 2020, 35, 225–236. [Google Scholar] [CrossRef]
- Comité_de_Nivel_Socioeconómico_AMAI. Nivel Socio Económico AMAI 2018. Nota Metodológica; Asociación Mexicana de Agencias de Inteligencia de Mercado y Opinión: Ciudad de México, México, 2017. [Google Scholar]
- Cucos, L. How to Interpret Model Fit Results in AMOS. Available online: https://uedufy.com/how-to-interpret-model-fit-results-in-amos/ (accessed on 13 July 2022).
- Clark, M.; Ogden, J. The Impact of Pregnancy on Eating Behaviour and Aspects of Weight Concern. Int. J. Obes. Relat. Metab. Disord. 1999, 23, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Forbes, L.E.; Graham, J.E.; Berglund, C.; Bell, R.C. Dietary Change during Pregnancy and Women’s Reasons for Change. Nutrients 2018, 10, 1032. [Google Scholar] [CrossRef] [PubMed]
- Orloff, N.C.; Hormes, J.M. Pickles and Ice Cream! Food Cravings in Pregnancy: Hypotheses, Preliminary Evidence, and Directions for Future Research. Front. Psychol. 2014, 5, 1076. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025, 9th ed.; 2020. Available online: https://www.dietaryguidelines.gov/ (accessed on 13 July 2022).
- Cisneros, C.F. Saber Popular Y Prácticas de Embarazo, Parto Y Puerperio En Yahuío, Sierra Norte de Oaxaca. Perinatol. Reprod. Hum. 2003, 17, 36–52. [Google Scholar]
- de Diego-Cordero, R.; Rivilla-Garcia, E.; Diaz-Jimenez, D.; Lucchetti, G.; Badanta, B. The Role of Cultural Beliefs on Eating Patterns and Food Practices among Pregnant Women: A Systematic Review. Nutr. Rev. 2021, 79, 945–963. [Google Scholar] [CrossRef]
- Verbeke, W.; De Bourdeaudhuij, I. Dietary Behaviour of Pregnant versus Non-Pregnant Women. Appetite 2007, 48, 78–86. [Google Scholar] [CrossRef]
- Garnweidner-Holme, L.; Terragni, L.; Pettersen, K.; Mosdøl, A. Attitudes and Motivations for Healthy Eating among Pregnant Women of Different Ethnic Backgrounds Following Antenatal Care in Oslo, Norway. J. Womens Health Care 2014, 3, 2167–2420. [Google Scholar] [CrossRef]
- Norma Oficial Mexicana 007-SSA2-2016; Para La Atención de La Mujer Durante El Embarazo, Parto Y Puerperio, Y de La Persona Recién Nacida. Diario Oficial de la Federación: Ciudad de México, México, 2016.
- Bookari, K.; Yeatman, H.; Williamson, M. Falling Short of Dietary Guidelines—What Do Australian Pregnant Women Really Know? A Cross Sectional Study. Women Birth 2017, 30, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Bjelica, A.; Cetkovic, N.; Trninic-Pjevic, A.; Mladenovic-Segedi, L. The Phenomenon of Pregnancy—A Psychological View. Ginekol. Pol. 2018, 89, 102–106. [Google Scholar] [CrossRef] [PubMed]
- López, M.E.G.; Gorn, S.B.; Cantú, M.A.L.; Sugiyama, M.E.I. Malestar Psicológico En Mujeres Con Embarazo de Alto Riesgo. Summa Psicol. 2016, 13, 89–100. [Google Scholar] [CrossRef]
- Wierzejska, R.E. Review of Dietary Recommendations for Twin Pregnancy: Does Nutrition Science Keep up with the Growing Incidence of Multiple Gestations? Nutrients 2022, 14, 1143. [Google Scholar] [CrossRef] [PubMed]
- Roem, K. Nutritional Management of Multiple Pregnancies. Twin Res. 2003, 6, 514–519. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ayyıldız, F.; Akbulut, G.; Ermumcu, M.Ş.K.; Tek, N.A. Emotional and Intuitive Eating: An Emerging Approach to Eating Behaviours Related to Obesity. J. Nutr. Sci. 2023, 12, e19. [Google Scholar] [CrossRef]
- Markey, C.H.; Strodl, E.; Aimé, A.; McCabe, M.; Rodgers, R.; Sicilia, A.; Coco, G.L.; Dion, J.; Mellor, D.; Pietrabissa, G.; et al. A Survey of Eating Styles in Eight Countries: Examining Restrained, Emotional, Intuitive Eating and Their Correlates. Br. J. Health Psychol. 2023, 28, 136–155. [Google Scholar] [CrossRef]
- Warren, J.M.; Smith, N.; Ashwell, M. A Structured Literature Review on the Role of Mindfulness, Mindful Eating and Intuitive Eating in Changing Eating Behaviours: Effectiveness and Associated Potential Mechanisms. Nutr. Res. Rev. 2017, 30, 272–283. [Google Scholar] [CrossRef]
- Burnette, C.B.; Hazzard, V.M.; Hahn, S.L.; Larson, N.; Neumark-Sztainer, D. Like Parent, like Child? Intuitive Eating among Emerging Adults and Their Parents. Appetite 2022, 176, 106132. [Google Scholar] [CrossRef]
- Burnette, C.B.; Hazzard, V.M.; Larson, N.; Hahn, S.L.; Eisenberg, M.E.; Neumark-Sztainer, D. Is Intuitive Eating a Privileged Approach? Cross-Sectional and Longitudinal Associations between Food Insecurity and Intuitive Eating—CORRIGENDUM. Public Health Nutr. 2023, 26, 1730. [Google Scholar] [CrossRef]
- Van Dyke, N.; Drinkwater, E.J. Intuitive Eating Is Positively Associated with Indicators of Physical and Mental Health among Rural Australian Adults. Aust. J. Rural Health 2022, 30, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Keirns, N.G.; Hawkins, M.A.W. Intuitive Eating, Objective Weight Status and Physical Indicators of Health. Obes. Sci. Pract. 2019, 5, 408–415. [Google Scholar] [CrossRef] [PubMed]
| Median (Quartile 1–Quartile 3) | |
|---|---|
| Maternal age (years) | 29.7 (25.0–33.8) |
| Gestational age (weeks) | 26.0 (21.0–31.0) |
| Pregestational BMI (kg/m2) | 25.9 (23.1–30.1) |
| IES-2 total score | 3.5 (3.2–3.8) |
| IES-2 Unconditional Permission to Eat | 3.5 (3.0–4.0) |
| IES-2 Reliance on Hunger and Satiety Cues | 3.6 (3.0–4.0) |
| IES-2 Body–Food Choice Congruence | 3.7 (3.0–4.0) |
| IES-2 Eating for Physical Rather Than Emotional Reasons, physical component | 3.5 (2.7–4.0) |
| IES-2 Eating for Physical Rather Than Emotional Reasons, emotional component | 4.0 (3.2–4.5) |
| n (%) | |
| Number of pregnancies | |
| First pregnancy | 199 (38.7) |
| 2nd or 3rd | 216 (42.0) |
| 4th or more | 99 (19.3) |
| Previous miscarriages/stillbirths | 194 (37.7) |
| Singleton pregnancy | 486 (94.5) |
| Living with a current illness | 237 (46.1) |
| Schooling | |
| Elementary school | 19 (3.7) |
| Secondary school | 118 (23.0) |
| High school | 226 (44.0) |
| Undergraduate school | 124 (24.1) |
| Graduate school | 27 (5.3) |
| Occupation | |
| Stays at home * | 354 (68.9) |
| Works outside home | 160 (31.1) |
| Lives with the baby’s father | |
| Yes | 328 (64.0) |
| Household welfare | |
| Medium to high | 132 (25.7) |
| Low | 382 (74.3) |
| Factor | Item |
|---|---|
| Permiso incondicional para comer (Unconditional Permission to Eat) | 3. Si tengo antojo de cierto alimento me doy permiso de comerlo. 16. Me doy permiso de comer cualquier comida que desee en el momento. |
| Confianza en las señales de hambre/saciedad (Reliance on Hunger and Satiety Cues) | 7. Confío en que mi cuerpo me dice qué debo comer. 8. Confío en que mi cuerpo me dice cuánto debo comer. 21. Confío en mis señales de hambre para saber cuándo comer. 22. Confío en mis señales de llenado (saciedad) para saber cuándo dejar de comer. 23. Confío en mi cuerpo para saber cuándo dejar de comer. |
| Congruencia en la elección cuerpo-comida (Body–Food Choice Congruence) | 18. La mayoría de las veces deseo comer alimentos nutritivos. 19. Principalmente como alimentos que hacen que mi cuerpo funcione eficientemente (bien). 20. Principalmente como alimentos que le dan a mi cuerpo energía y aguante. |
| Comer por razones físicas en vez de emocionales (componente físico). (Eating for Physical Rather Than Emotional Reasons, physical component) | 12. Soy capaz de sobrellevar mis emociones negativas (ansiedad, tristeza) sin recurrir a la comida para sentirme mejor. 13. Cuando estoy aburrida NO como solamente para tener algo que hacer. 14. Cuando me siento sola NO recurro a la comida para sentirme mejor. 15. Encuentro otras formas de sobrellevar el estrés y la ansiedad que comiendo. |
| Comer por razones físicas en vez de emocionales (componente emocional). (Eating for Physical Rather Than Emotional Reasons, emotional component) | 2. Me doy cuenta de que como cuando me siento emocional (ansiosa, deprimida, triste), aunque no tenga hambre. 5. Me doy cuenta de que como cuando me siento sola, aunque no tenga hambre. 10. Uso la comida para ayudarme con mis emociones negativas. 11. Me doy cuenta de que como cuando estoy estresada, aunque no tenga hambre. |
| IES-2 | UPE | RHSC | B-FCC | EPR-Ph | EPR-Emo | Maternal Age | pg-BMI | Number of Pregnancies | Previous Miscarriages | Type of Pregnancy | Gestational Age | Current Illness | Schooling | Occupation | Lives with Baby’s Father | Household Welfare | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IES-2 | _ | _ | _ | _ | _ | _ | 0.042 (0.343) | −0.182 (<0.001) | −0.038 (0.390) | 0.003 (0.946) | 0.149 (0.001) | −0.063 (0.156) | −0.057 (0.196) | 0.058 (0.190) | 0.065 (0.138) | 0.069 (0.121) | 0.053 (0.234) |
| UPE | - | 0.248 (<0.001) | −0.047 (0.292) | 0.078 (0.079) | −0.148 (0.001) | −0.090 (0.043) | −0.134 (0.002) | −0.034 (0.442) | 0.009 (0.833) | 0.072 (0.105) | 0.018 (0.678) | −0.078 (0.079) | 0.031 (0.483) | 0.021 (0.642) | 0.003 (0.946) | −0.007 (0.872) | |
| RHSC | - | 0.360 (<0.001) | 0.222 (<0.001) | 0.064 (0.148) | 0.017 (0.698) | −0.221 (<0.001) | 0.004 (0.927) | 0.032 (0.466) | 0.124 (0.005) | −0.014 (0.758) | −0.050 (0.254) | 0.023 (0.600) | 0.025 (0.572) | 0.056 (0.203) | 0.043 (0.330) | ||
| B-FCC | - | 0.175 (<0.001) | 0.114 (0.010) | 0.155 (<0.001) | −0.148 (0.001) | 0.021 (0.631) | −0.026 (0.563) | 0.098 (0.026) | −0.031 (0.483) | 0.077 (0.080) | 0.056 (0.204) | −0.017 (0.696) | 0.057 (0.193) | 0.082 (0.062) | |||
| EPR-Ph | - | 0.210 (<0.001) | 0.121 (0.006) | −0.030 (0.501) | −0.039 (0.376) | 0.023 (0.604) | 0.077 (0.081) | −0.070 (0.111) | −0.038 (0.388) | 0.136 (0.002) | 0.134 (0.002) | 0.058 (0.191) | 0.073 (0.098) | ||||
| EPR-Emo | - | −0.090 (0.042) | −0.033 (0.457) | −0.010 (0.818) | −0.005 (0.901) | 0.034 (0.445) | −0.062 (0.164) | −0.048 (0.275) | −0.125 (0.004) | −0.007 (0.882) | 0.020 (0.648) | −0.030 (0.500) |
| Total IES Score | |
|---|---|
| Predictors | β (95% CI) p-Value |
| Type of pregnancy | 0.295 (0.121, 0.470) 0.001 |
| Household welfare | 0.123 (0.011, 0.236) 0.032 |
| Maternal age | 0.009 (0.002, 0.016) 0.013 |
| Gestational weeks | −0.006 (−0.012, 0.000) 0.040 |
| Current illness | −0.102 (−0.202, −0.003) 0.044 |
| pg-BMI | −0.18 (−0.015, −0.011) <0.001 |
| R2 (adjusted R2) | 0.087 (0.076) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flores-Quijano, M.E.; Mota-González, C.; Rozada, G.; León-Rico, J.C.; Gómez-López, M.E.; Vega-Sánchez, R. The Intuitive Eating Scale-2 Adapted for Mexican Pregnant Women: Psychometric Properties and Influence of Sociodemographic Variables. Nutrients 2023, 15, 4837. https://doi.org/10.3390/nu15224837
Flores-Quijano ME, Mota-González C, Rozada G, León-Rico JC, Gómez-López ME, Vega-Sánchez R. The Intuitive Eating Scale-2 Adapted for Mexican Pregnant Women: Psychometric Properties and Influence of Sociodemographic Variables. Nutrients. 2023; 15(22):4837. https://doi.org/10.3390/nu15224837
Chicago/Turabian StyleFlores-Quijano, María Eugenia, Cecilia Mota-González, Guadalupe Rozada, Jacqueline Citlalli León-Rico, María Eugenia Gómez-López, and Rodrigo Vega-Sánchez. 2023. "The Intuitive Eating Scale-2 Adapted for Mexican Pregnant Women: Psychometric Properties and Influence of Sociodemographic Variables" Nutrients 15, no. 22: 4837. https://doi.org/10.3390/nu15224837
APA StyleFlores-Quijano, M. E., Mota-González, C., Rozada, G., León-Rico, J. C., Gómez-López, M. E., & Vega-Sánchez, R. (2023). The Intuitive Eating Scale-2 Adapted for Mexican Pregnant Women: Psychometric Properties and Influence of Sociodemographic Variables. Nutrients, 15(22), 4837. https://doi.org/10.3390/nu15224837







