Impact of Mediterranean Diet on Lipid Composition in the Colaus-PsyColaus Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population and Study Design
2.2. Dietary Assessment
2.3. Quantification of the Mediterranean Diet Adherence Scores
2.4. Lipids
2.5. Other Covariates
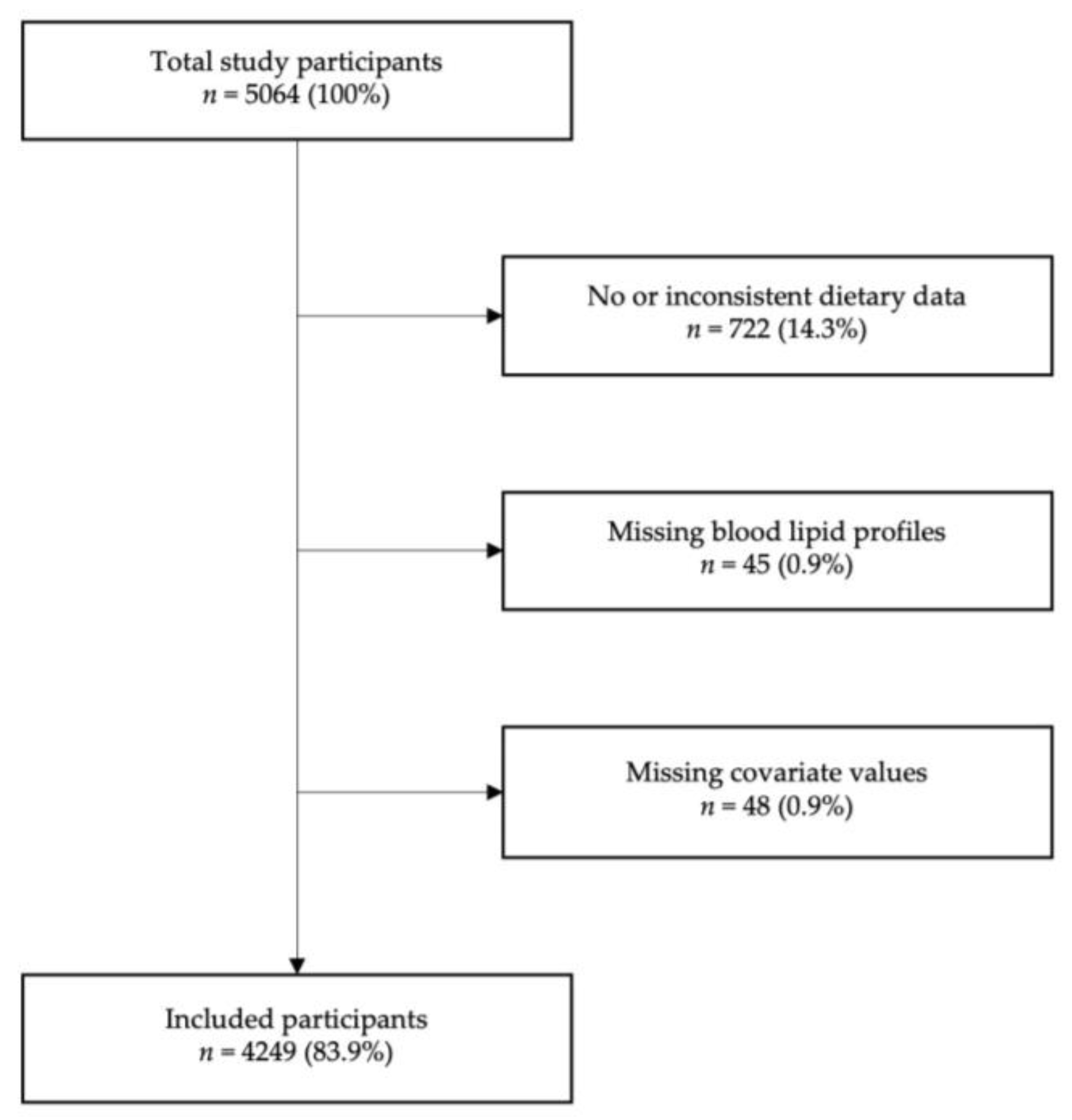
2.6. Inclusion and Exclusion Criteria
2.7. Statistical Analysis
3. Results
3.1. Selection and Characteristics of the Participants
3.2. Mediterranean Diet Scores and Characteristics of the Participants
3.3. Association between MD and Lipid Levels/Hypolipidemic Treatment at FU1
3.4. Association between MD Scores and Incident Dyslipidemia
3.5. Association between MD Scores and Changes in Lipid Levels between FU1 and FU2/FU3
4. Discussion
4.1. Main Findings
4.2. Association of MD Score with Lipid Profile
4.3. Association of MD Score with Incident Dyslipidemia and Lipid Evolution
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. J. Prev. Cardiol. 2022, 29, 5–115. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Moorthy, M.V.; Demler, O.V.; Hu, F.B.; Ridker, P.M.; Chasman, D.I.; Mora, S. Assessment of Risk Factors and Biomarkers Associated with Risk of Cardiovascular Disease Among Women Consuming a Medi-terranean Diet. JAMA Netw. Open 2018, 1, e185708. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Willett, W.C. The Mediterranean diet and health: A comprehensive overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supple-mented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Rosato, V.; Temple, N.J.; La Vecchia, C.; Castellan, G.; Tavani, A.; Guercio, V. Mediterranean diet and cardio-vascular disease: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2019, 58, 173–191. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediter-ranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean Diet and Survival in a Greek Population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef]
- Platania, A.; Zappala, G.; Mirabella, M.U.; Gullo, C.; Mellini, G.; Beneventano, G.; Maugeri, G.; Marranzano, M. Association between Mediterranean diet adherence and dyslipidaemia in a cohort of adults living in the Med-iterranean area. Int. J. Food Sci. Nutr. 2018, 69, 608–618. [Google Scholar] [CrossRef]
- Mertens, E.; Mullie, P.; Deforche, B.; Lefevre, J.; Charlier, R.; Huybrechts, I.; Clarys, P. Cross-sectional study on the relationship between the Mediterranean Diet Score and blood lipids. Nutr. J. 2014, 13, 88. [Google Scholar] [CrossRef]
- Magriplis, E.; Panagiotakos, D.; Mitsopoulou, A.-V.; Karageorgou, D.; Bakogianni, I.; Dimakopoulos, I.; Micha, R.; Michas, G.; Chourdakis, M.; Chrousos, G.P.; et al. Prevalence of hyperlipidaemia in adults and its relation to the Mediterranean diet: The Hellenic National Nutrition and Health Survey (HNNHS). Eur. J. Prev. Cardiol. 2019, 26, 1957–1967. [Google Scholar] [CrossRef]
- Hershey, M.S.; Sotos-Prieto, M.; Ruiz-Canela, M.; Christophi, C.A.; Moffatt, S.; Martínez-González, M.Á.; Kales, S.N. The Mediterranean lifestyle (MEDLIFE) index and metabolic syndrome in a non-Mediterranean working population. Clin. Nutr. 2021, 40, 2494–2503. [Google Scholar] [CrossRef] [PubMed]
- Formisano, E.; Pasta, A.; Cremonini, A.L.; Di Lorenzo, I.; Sukkar, S.G.; Pisciotta, L. Effects of a Mediterranean Diet, Dairy, and Meat Products on Different Phenotypes of Dyslipidemia: A Preliminary Retrospective Analysis. Nutrients 2021, 13, 1161. [Google Scholar] [CrossRef] [PubMed]
- Peñalvo, J.L.; Oliva, B.; Sotos-Prieto, M.; Uzhova, I.; Moreno-Franco, B.; León-Latre, M.; Ordovás, J.M. Greater Adherence to a Mediterranean Dietary Pattern Is Associated With Improved Plasma Lipid Profile: The Aragon Health Workers Study Cohort. Rev. Esp. Cardiol. Engl. Ed. 2015, 68, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Ruiz-Canela, M.; Song, Y.; Christophi, C.; Mofatt, S.; Rodriguez-Artalejo, F.; Kales, S.N. The Effects of a Mediterranean Diet Intervention on Targeted Plasma Metabolic Biomarkers among US Firefighters: A Pilot Cluster-Randomized Trial. Nutrients 2020, 12, 3610. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterra-nean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 2019, 28–29. [Google Scholar] [CrossRef]
- Firmann, M.; Mayor, V.; Vidal, P.M.; Bochud, M.; Pécoud, A.; Hayoz, D.; Paccaud, F.; Preisig, M.; Song, K.S.; Yuan, X.; et al. The CoLaus study: A population-based study to investigate the epidemiology and genetic de-terminants of cardiovascular risk factors and metabolic syndrome. BMC Cardiovasc. Disord. 2008, 8, 6. [Google Scholar] [CrossRef]
- Bernstein, M.; Huot, I.; Morabia, A. Amélioration des performances d’un questionnaire alimentaire se-mi-quantitatif comparé à un rappel des 24 heures. Santé Publique Vandoeuvre-Lès-Nancy 1995, 4, 403–413. [Google Scholar]
- Beer-Borst, S.; Costanza, M.C.; Pechère-Bertschi, A.; Morabia, A. Twelve-year trends and correlates of dietary salt intakes for the general adult population of Geneva, Switzerland. Eur. J. Clin. Nutr. 2009, 63, 155–164. [Google Scholar] [CrossRef]
- Marques-Vidal, P.; Ross, A.; Wynn, E.; Rezzi, S.; Paccaud, F.; Decarli, B. Reproducibility and relative validity of a food-frequency questionnaire for French-speaking Swiss adults. Food Nutr. Res. 2011, 55, 5905. [Google Scholar] [CrossRef]
- Vormund, K.; Braun, J.; Rohrmann, S.; Bopp, M.; Ballmer, P.; Faeh, D. Mediterranean diet and mortality in Switzerland: An alpine paradox? Eur. J. Nutr. 2015, 54, 139–148. [Google Scholar] [CrossRef]
- Hoffman, R.; Gerber, M. Evaluating and adapting the Mediterranean diet for non-Mediterranean populations: A critical appraisal. Nutr. Rev. 2013, 71, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Chatelan, A.; Beer-Borst, S.; Randriamiharisoa, A.; Pasquier, J.; Blanco, J.; Siegenthaler, S.; Paccaud, F.; Slimani, N.; Nicolas, G.; Camenzind-Frey, E.; et al. Major Differences in Diet across Three Linguistic Regions of Swit-zerland: Results from the First National Nutrition Survey menuCH. Nutrients 2017, 9, 1163. [Google Scholar] [CrossRef] [PubMed]
- Freisling, H.; Fahey, M.T.; Moskal, A.; Ocké, M.C.; Ferrari, P.; Jenab, M.; Norat, T.; Naska, A.; Welch, A.A.; Na-varro, C.; et al. Region-Specific Nutrient Intake Patterns Exhibit a Geographical Gradient within and between European Countries. J. Nutr. 2010, 140, 1280–1286. [Google Scholar] [CrossRef] [PubMed]
| Trichopoulou | p-Value | Vormund | p-Value | |
|---|---|---|---|---|
| Untreated (n = 3485) | ||||
| Total cholesterol | 0.006 | 0.729 | −0.015 | 0.387 |
| LDL cholesterol | −0.006 | 0.705 | −0.026 | 0.132 |
| HDL cholesterol | 0.044 | 0.009 | 0.071 | <0.001 |
| Triglycerides | −0.032 | 0.057 | −0.076 | <0.001 |
| Treated (n = 764) | ||||
| Total cholesterol | −0.070 | 0.052 | −0.073 | 0.043 |
| LDL cholesterol | −0.065 | 0.071 | −0.074 | 0.040 |
| HDL cholesterol | 0.041 | 0.253 | −0.005 | 0.896 |
| Triglycerides | −0.060 | 0.100 | −0.036 | 0.324 |
| No Incident Hypolipidemic Treatment | Incident Hypolipidemic Treatment | p-Value | |
|---|---|---|---|
| Total | 2743 (88.7) | 349 (11.3) | |
| Woman (%) | 1598 (58.3) | 172 (49.3) | 0.001 |
| Age (years) | 55.4 ± 10.0 | 59.4 ± 9.3 | <0.001 |
| Swiss-born (%) | 1788 (65.2) | 217 (62.2) | 0.268 |
| Educational level (%) | <0.001 | ||
| High | 684 (24.9) | 64 (18.3) | |
| Middle | 801 (29.2) | 85 (24.4) | |
| Low | 1258 (45.9) | 200 (57.3) | |
| Living alone (%) | 1149 (41.9) | 150 (43.0) | 0.697 |
| Smoking status (%) | 0.012 | ||
| Never | 1200 (43.8) | 131 (37.5) | |
| Former | 1021 (37.2) | 130 (37.3) | |
| Current | 522 (19.0) | 88 (25.2) | |
| BMI (kg/m2) | 25.3 ± 4.3 | 27.0 ± 4.5 | <0.001 |
| BMI categories (%) | <0.001 | ||
| Normal | 1441 (52.5) | 119 (34.1) | |
| Overweight | 970 (35.4) | 159 (45.6) | |
| Obese | 332 (12.1) | 71 (20.3) | |
| Hypertension (%) | 839 (30.6) | 169 (48.4) | <0.001 |
| Diabetes (%) | 131 (4.8) | 49 (14.0) | <0.001 |
| Mediterranean diet score | |||
| Trichopoulou | 4.0 ± 1.5 | 4.1 ± 1.5 | 0.205 |
| Vormund | 4.8 ± 1.9 | 4.8 ± 1.8 | 0.402 |
| Trichopoulou | p-Value | Vormund | p-Value | |
|---|---|---|---|---|
| Untreated (n = 2991) | ||||
| 5- to 10-year changes | ||||
| Total cholesterol | 0.001 | 0.941 | 0.052 | 0.005 |
| LDL cholesterol | −0.000 | 0.995 | 0.043 | 0.020 |
| HDL cholesterol | 0.014 | 0.450 | 0.022 | 0.234 |
| Triglycerides | 0.021 | 0.245 | 0.038 | 0.036 |
| Treated (n = 629) | ||||
| 5- to 10-year changes | ||||
| Total cholesterol | 0.020 | 0.625 | 0.030 | 0.453 |
| LDL cholesterol | 0.012 | 0.771 | 0.011 | 0.779 |
| HDL cholesterol | −0.005 | 0.900 | 0.020 | 0.612 |
| Triglycerides | 0.040 | 0.319 | 0.071 | 0.076 |
| Trichopoulou | p-Value | Vormund | p-Value | |
|---|---|---|---|---|
| Untreated (n = 2991) | ||||
| 5- to 10-year changes | ||||
| Total cholesterol | 0.000 | 0.986 | 0.031 | 0.085 |
| LDL cholesterol | −0.007 | 0.693 | 0.026 | 0.142 |
| HDL cholesterol | 0.022 | 0.238 | 0.026 | 0.167 |
| Triglycerides | 0.010 | 0.583 | 0.004 | 0.839 |
| Treated (n = 629) | ||||
| 5- to 10-year changes | ||||
| Total cholesterol | 0.033 | 0.411 | 0.024 | 0.557 |
| LDL cholesterol | 0.040 | 0.328 | 0.130 | 0.750 |
| HDL cholesterol | −0.017 | 0.678 | 0.000 | 0.987 |
| Triglycerides | 0.003 | 0.950 | 0.036 | 0.381 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flatscher, M.; Garnier, A.; Marques-Vidal, P.; Kraege, V. Impact of Mediterranean Diet on Lipid Composition in the Colaus-PsyColaus Study. Nutrients 2023, 15, 4659. https://doi.org/10.3390/nu15214659
Flatscher M, Garnier A, Marques-Vidal P, Kraege V. Impact of Mediterranean Diet on Lipid Composition in the Colaus-PsyColaus Study. Nutrients. 2023; 15(21):4659. https://doi.org/10.3390/nu15214659
Chicago/Turabian StyleFlatscher, Mélisande, Antoine Garnier, Pedro Marques-Vidal, and Vanessa Kraege. 2023. "Impact of Mediterranean Diet on Lipid Composition in the Colaus-PsyColaus Study" Nutrients 15, no. 21: 4659. https://doi.org/10.3390/nu15214659
APA StyleFlatscher, M., Garnier, A., Marques-Vidal, P., & Kraege, V. (2023). Impact of Mediterranean Diet on Lipid Composition in the Colaus-PsyColaus Study. Nutrients, 15(21), 4659. https://doi.org/10.3390/nu15214659







