Efficacy and Safety of a High-Energy, Low-Protein Formula Replacement Meal for Pre-Dialysis Chronic Kidney Disease Patients: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
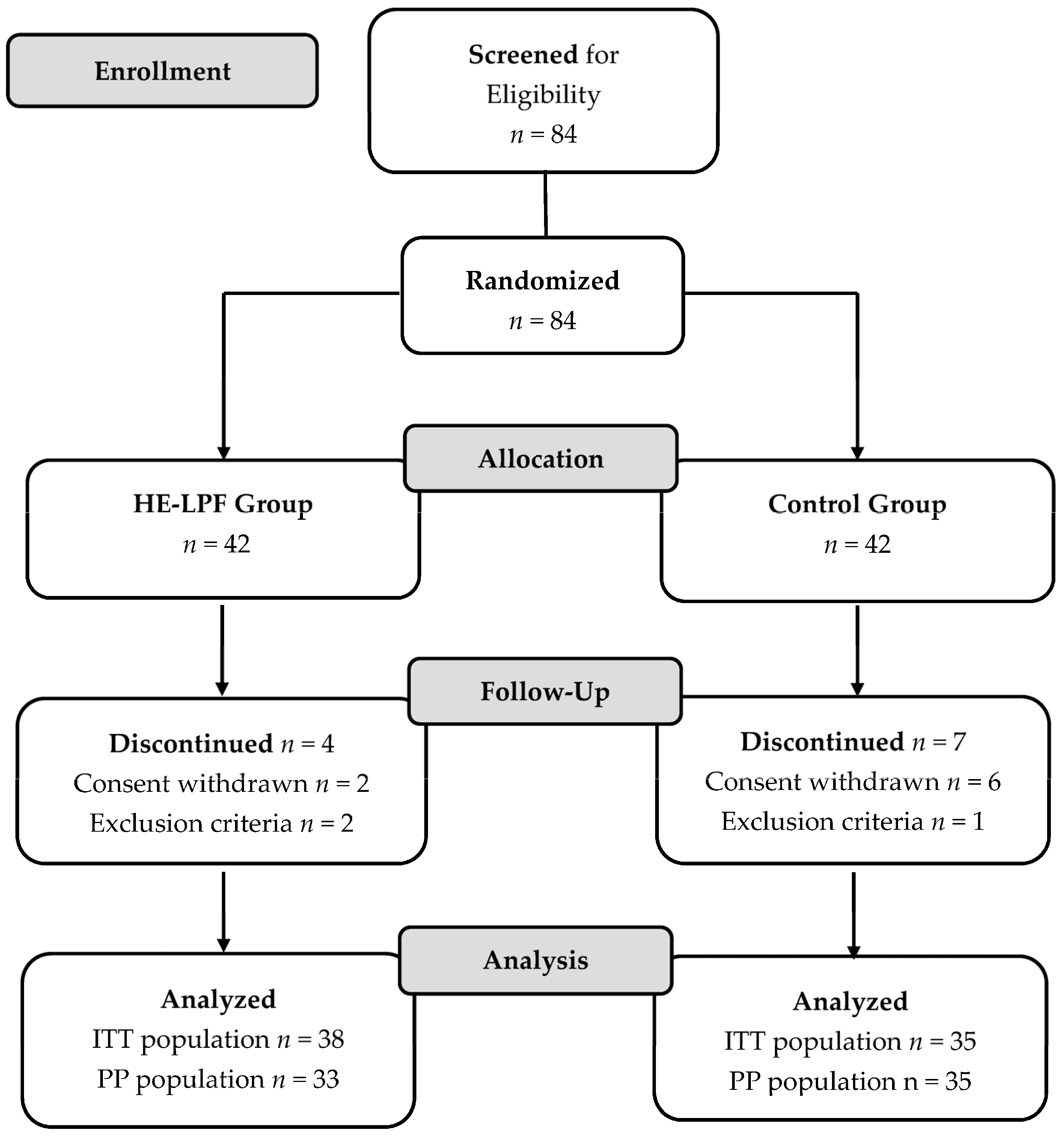
2.1. Study Design
2.2. Subjects
2.3. Dietary Management
2.4. Study Intervention
2.5. Efficacy Assessments
2.6. Safety and Adherence Assessments
2.7. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Efficacy Outcomes
3.3. Safety and Adherence Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kovesdy, C.P. Epidemiology of chronic kidney disease: An update 2022. Kidney Int. Suppl. 2022, 12, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.K.; Knicely, D.H.; Grams, M.E. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA 2019, 322, 1294–1304. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Jafar, T.H.; Nitsch, D.; Neuen, B.L.; Perkovic, V. Chronic kidney disease. Lancet 2021, 398, 786–802. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Fouque, D. Nutritional Management of Chronic Kidney Disease. N. Engl. J. Med. 2017, 377, 1765–1776. [Google Scholar] [CrossRef] [PubMed]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef] [PubMed]
- Kistler, B.M.; Moore, L.W.; Benner, D.; Biruete, A.; Boaz, M.; Brunori, G.; Chen, J.; Drechsler, C.; Guebre-Egziabher, F.; Hensley, M.K.; et al. The International Society of Renal Nutrition and Metabolism Commentary on the National Kidney Foundation and Academy of Nutrition and Dietetics KDOQI Clinical Practice Guideline for Nutrition in Chronic Kidney Disease. J. Ren. Nutr. 2021, 31, 116–120.e111. [Google Scholar] [CrossRef] [PubMed]
- Paes-Barreto, J.G.; Silva, M.I.; Qureshi, A.R.; Bregman, R.; Cervante, V.F.; Carrero, J.J.; Avesani, C.M. Can renal nutrition education improve adherence to a low-protein diet in patients with stages 3 to 5 chronic kidney disease? J. Ren. Nutr. 2013, 23, 164–171. [Google Scholar] [CrossRef]
- Cupisti, A.; Gallieni, M.; Avesani, C.M.; D’Alessandro, C.; Carrero, J.J.; Piccoli, G.B. Medical Nutritional Therapy for Patients with Chronic Kidney Disease not on Dialysis: The Low Protein Diet as a Medication. J. Clin. Med. 2020, 9, 3644. [Google Scholar] [CrossRef]
- Pisani, A.; Riccio, E.; Bellizzi, V.; Caputo, D.L.; Mozzillo, G.; Amato, M.; Andreucci, M.; Cianciaruso, B.; Sabbatini, M. 6-tips diet: A simplified dietary approach in patients with chronic renal disease. A clinical randomized trial. Clin. Exp. Nephrol. 2016, 20, 433–442. [Google Scholar] [CrossRef]
- Carrero, J.J.; Stenvinkel, P.; Cuppari, L.; Ikizler, T.A.; Kalantar-Zadeh, K.; Kaysen, G.; Mitch, W.E.; Price, S.R.; Wanner, C.; Wang, A.Y.; et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: A consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J. Ren. Nutr. 2013, 23, 77–90. [Google Scholar] [CrossRef]
- Schrauben, S.J.; Apple, B.J.; Chang, A.R. Modifiable Lifestyle Behaviors and CKD Progression: A Narrative Review. Kidney360 2022, 3, 752–778. [Google Scholar] [CrossRef] [PubMed]
- MacLaughlin, H.L.; Friedman, A.N.; Ikizler, T.A. Nutrition in Kidney Disease: Core Curriculum 2022. Am. J. Kidney Dis. 2022, 79, 437–449. [Google Scholar] [CrossRef]
- Wu, H.L.; Sung, J.M.; Kao, M.D.; Wang, M.C.; Tseng, C.C.; Chen, S.T. Nonprotein calorie supplement improves adherence to low-protein diet and exerts beneficial responses on renal function in chronic kidney disease. J. Ren. Nutr. 2013, 23, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Kanazawa, Y.; Morita, S.; Sonoki, H.; Nakao, T. Effects of a novel nutritional formula specially developed for chronic kidney disease patients on protein-restricted diets: A randomized controlled trial. Ren. Replace. Ther. 2016, 2, 18. [Google Scholar] [CrossRef][Green Version]
- Montes-Delgado, R.; Guerrero Riscos, M.A.; García-Luna, P.P.; Martín Herrera, C.; Pereira Cunill, J.L.; Garrido Vázquez, M.; López Muñoz, I.; Suárez García, M.J.; Martín-Espejo, J.L.; Soler Junco, M.L.; et al. Treatment with low-protein diet and caloric supplements in patients with chronic kidney failure in predialysis. Comparative study. Rev. Clin. Esp. 1998, 198, 580–586. [Google Scholar] [PubMed]
- Satirapoj, B.; Prapakorn, J.; Punpanich, D.; Pongsuparbchon, C.; Supasyndh, O. The effect of ONCE Renal on minerals and electrolytes in predialysis patients with chronic kidney disease. Int. J. Nephrol. Renov. Dis. 2016, 9, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Mustad, V.A.; Hegazi, R.A.; Hustead, D.S.; Budiman, E.S.; Rueda, R.; Maki, K.; Powers, M.; Mechanick, J.I.; Bergenstal, R.M.; Hamdy, O. Use of a diabetes-specific nutritional shake to replace a daily breakfast and afternoon snack improves glycemic responses assessed by continuous glucose monitoring in people with type 2 diabetes: A randomized clinical pilot study. BMJ Open Diab. Res. Care 2020, 8, e001258. [Google Scholar] [CrossRef] [PubMed]
- Bowen, J.; Brindal, E.; James-Martin, G.; Noakes, M. Randomized Trial of a High Protein, Partial Meal Replacement Program with or without Alternate Day Fasting: Similar Effects on Weight Loss, Retention Status, Nutritional, Metabolic, and Behavioral Outcomes. Nutrients 2018, 10, 1145. [Google Scholar] [CrossRef]
- Gulati, S.; Misra, A.; Tiwari, R.; Sharma, M.; Pandey, R.M.; Yadav, C.P. Effect of high-protein meal replacement on weight and cardiometabolic profile in overweight/obese Asian Indians in North India. Br. J. Nutr. 2017, 117, 1531–1540. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Maroni, B.J.; Steinman, T.I.; Mitch, W.E. A method for estimating nitrogen intake of patients with chronic renal failure. Kidney Int. 1985, 27, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Yue, H.; Zhou, P.; Xu, Z.; Liu, L.; Zong, A.; Qiu, B.; Liu, W.; Jia, M.; Du, F.; Xu, T. Effect of low-protein diet on kidney function and nutrition in nephropathy: A systematic review and meta-analysis of randomized controlled trials. Clin. Nutr. 2020, 39, 2675–2685. [Google Scholar] [CrossRef] [PubMed]
- Carrero, J.J. Mechanisms of altered regulation of food intake in chronic kidney disease. J. Ren. Nutr. 2011, 21, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Bjornsson, T.D. Use of Serum Creatinine Concentrations to Determine Renal Function1. Clin. Pharmacokinet. 1979, 4, 200–222. [Google Scholar] [CrossRef]
- Torreggiani, M.; Wang, A.Y.; Fois, A.; Piccoli, G.B. Personalized Low-Protein Diet Prescription in CKD Population: Merging Evidence From Randomized Trials With Observational Data. Semin. Nephrol. 2023, 43, 151402. [Google Scholar] [CrossRef] [PubMed]
- Hammad, S.; Pu, S.; Jones, P.J. Current Evidence Supporting the Link Between Dietary Fatty Acids and Cardiovascular Disease. Lipids 2016, 51, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Fazelian, S.; Moradi, F.; Agah, S.; Hoseini, A.; Heydari, H.; Morvaridzadeh, M.; Omidi, A.; Pizarro, A.B.; Ghafouri, A.; Heshmati, J. Effect of omega-3 fatty acids supplementation on cardio-metabolic and oxidative stress parameters in patients with chronic kidney disease: A systematic review and meta-analysis. BMC Nephrol. 2021, 22, 160. [Google Scholar] [CrossRef]
- Giannese, D.; D’Alessandro, C.; Panichi, V.; Pellegrino, N.; Cupisti, A. Nutritional Treatment as a Synergic Intervention to Pharmacological Therapy in CKD Patients. Nutrients 2023, 15, 2715. [Google Scholar] [CrossRef]
- Almeras, C.; Argilés, A. The general picture of uremia. Semin. Dial. 2009, 22, 329–333. [Google Scholar] [CrossRef]
- Kelly, O.J.; Huang, M.C.; Liao, H.Y.; Lin, C.C.; Tung, T.Y.; Cheng, R.W.; Wang, M.Y.; Yalawar, M.; Hwang, S.J. A Low-Protein Diet with a Renal-Specific Oral Nutrition Supplement Helps Maintain Nutritional Status in Patients with Advanced Chronic Kidney Disease. J. Pers. Med. 2021, 11, 1360. [Google Scholar] [CrossRef]
- Ekramzadeh, M.; Santoro, D.; Kopple, J.D. The Effect of Nutrition and Exercise on Body Composition, Exercise Capacity, and Physical Functioning in Advanced CKD Patients. Nutrients 2022, 14, 2129. [Google Scholar] [CrossRef]
| Parameter | HE-LPF Group (n = 38) | Control Group (n = 35) | p-Value |
|---|---|---|---|
| Male gender, n (%) | 22 (57.9) | 22 (62.9) | 0.665 |
| Age (years), mean (SD) | 56.4 (12.9) | 53.5 (10.2) | 0.230 |
| eGFR (mL/min/1.73 m2), mean (SD) | 16.0 (8.5) | 17.3 (9.5) | 0.585 |
| CKD stage, n (%) | 0.314 | ||
| Stage 3 | 3 (7.9) | 5 (14.3) | |
| Stage 4 | 12 (31.6) | 15 (42.9) | |
| Stage 5 | 23 (60.5) | 15 (42.9) | |
| Primary cause of CKD, n (%) | 0.246 | ||
| Diabetic nephropathy | 11 (28.9) | 13 (37.1) | |
| Glomerular nephropathy | 9 (23.7) | 2 (5.7) | |
| Vascular nephropathy/HTN | 11 (28.9) | 12 (34.3) | |
| Polycystic kidney disease | 5 (13.2) | 5 (14.3) | |
| Other | 2 (5.3) | 3 (8.6) | |
| Comorbidities, n (%) | |||
| Diabetes | 11 (28.9) | 13 (37.1) | 0.457 |
| Hypertension | 11 (28.9) | 12 (34.3) | 0.812 |
| Concomitant medications, n (%) | |||
| ACE inhibitors/ARBs | 9 (23.7) | 9 (25.3) | 1.000 |
| Keto-analogues | 12 (31.6) | 12 (34.3) | 1.000 |
| Body weight (kg), mean (SD) | 62.7 (11.6) | 66.5 (11.1) | 0.185 |
| Body mass index (kg/m2), mean (SD) | 23.3 (3.8) | 24.1 (3.2) | 0.258 |
| Grip strength (kg), mean (SD) | 28.6 (10.6) | 32.8 (11.4) | 0.092 |
| Vital signs | |||
| Systolic blood pressure (mm Hg), mean (SD) | 136.6 (22.1) | 135.9 (16.5) | 0.732 |
| Diastolic blood pressure (mm Hg), mean (SD) | 76.0 (14.9) | 80 (12.8) | 0.208 |
| Heart rate (bpm), mean (SD) | 75.9 (12.1) | 78.6 (11.8) | 0.281 |
| Respiratory rate (bpm), mean (SD) | 19.0 (5.9) | 18.1 (5.5) | 0.458 |
| Parameter | HE-LPF Group (n = 38) | Control Group (n = 35) | p-Value |
|---|---|---|---|
| Body weight change (kg) | |||
| Change from baseline to Week 2 a | 0.1 (1.4) | 0.1 (1.4) | 0.921 |
| Change from baseline to Week 4 a | 0.0 (1.8) | 0.1 (1.3) | 0.685 |
| Body weight (kg) | 0.153 | ||
| Baseline | 62.7 (11.6) | 66.5 (11.1) | |
| Week 2 | 62.8 (11.7) | 66.6 (11.2) | |
| Week 4 | 62.7 (11.5) | 66.6 (11.0) | |
| Body mass index (kg/m2) | 0.266 | ||
| Baseline | 23.3 (3.8) | 24.1 (3.2) | |
| Week 2 | 23.3 (3.8) | 24.2 (3.3) | |
| Week 4 | 23.2 (3.8) | 24.2 (3.2) | |
| Body fat (%) | 0.157 | ||
| Baseline | 20.8 (6.8) | 23.1 (8.1) | |
| Week 2 | 20.9 (7.5) | 23.3 (8.2) | |
| Week 4 | 20.0 (8.3) | 22.9 (8.0) | |
| Fat mass (kg) | 0.087 | ||
| Baseline | 13.0 (5.4) | 15.3 (6.5) | |
| Week 2 | 13.1 (6.1) | 15.5 (6.7) | |
| Week 4 | 12.4 (6.2) | 15.2 (6.5) | |
| Muscle mass (kg) | 0.472 | ||
| Baseline | 46.0 (8.7) | 47.5 (8.7) | |
| Week 2 | 45.9 (8.9) | 47.3 (8.4) | |
| Week 4 | 46.2 (9.0) | 47.6 (8.4) | |
| Fat free mass (kg) | 0.460 | ||
| Baseline | 48.6 (9.0) | 50.3 (9.1) | |
| Week 2 | 48.6 (9.3) | 50.1 (8.7) | |
| Week 4 | 48.8 (9.4) | 50.4 (8.7) | |
| Extracellular water (kg) | 0.459 | ||
| Baseline | 14.0 (2.4) | 14.4 (2.3) | |
| Week 2 | 13.9 (2.6) | 14.3 (2.2) | |
| Week 4 | 14.0 (2.5) | 14.4 (2.2) | |
| Waist circumference (cm) | 0.269 | ||
| Baseline | 84.4 (10.5) | 86.1 (9.3) | |
| Week 4 | 83.6 (9.9) | 87.0 (9.8) | |
| Grip strength (kg) | 0.129 | ||
| Baseline | 28.6 (10.6) | 32.8 (11.4) | |
| Week 2 | 29.0 (10.4) | 32.6 (12.3) | |
| Week 4 | 28.5 (10.4) | 32.6 (11.9) |
| Parameter | HE-LPF Group | Control Group | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 2 | Week 4 | Baseline | Week 2 | Week 4 | ||
| ITT Population | |||||||
| Energy (kcal/day) | 1560 (318) | 1702 (400) | 1756 (339) | 1671 (303) | 1651 (317) | 1569 (323) | 0.531 |
| Energy (kcal/kg BW/day) | 25.4 (6.2) | 27.6 (6.6) | 28.6 (6.8) | 25.6 (5.5) | 25.4 (6.0) | 24.1 (5.6) | 0.093 |
| Protein (g/kg BW/day) | 0.78 (0.20) | 0.76 (0.21) | 0.80 (0.21) | 0.80 (0.21) | 0.82 (0.23) | 0.74 (0.20) | 0.898 |
| Protein (% of energy) | 12.2 (2.4) | 10.9 (1.6) | 11.1 (1.8) | 12.4 (2.3) | 12.8 (3.2) | 12.3 (2.9) | 0.021 * |
| CHO (% of energy) | 51.2 (6.3) | 51.2 (6.0) | 51.5 (5.7) | 53.2 (6.9) | 52.5 (6.1) | 52.9 (7.3) | 0.216 |
| Fat (% of energy) | 36.6 (5.2) | 38.0 (5.6) | 37.3 (5.0) | 34.4 (6.1) | 34.7 (5.3) | 34.8 (5.8) | 0.010 * |
| SFA (g) | 15.3 (4.5) | 18.2 (4.6) | 18.4 (4.8) | 15.8 (5.2) | 15.2 (4.5) | 15.1 (4.4) | 0.032 * |
| MUFA (g) | 17.3 (5.9) | 25.3 (6.3) | 25.3 (5.6) | 18.9 (7.1) | 17.6 (5.6) | 16.8 (4.8) | <0.001 * |
| PUFA (g) | 25.5 (8.3) | 27.2 (9.1) | 27.8 (8.7) | 25.3 (8.7) | 25.1 (9.2) | 23.0 (7.2) | 0.160 |
| EPA (mg) | 68 (130) | 231 (236) | 134 (112) | 49 (60) | 70 (153) | 108 (179) | 0.005 * |
| DHA (mg) | 168 (233) | 313 (402) | 176 (175) | 109 (78) | 173 (240) | 246 (320) | 0.307 |
| Fiber (g) | 12.2 (4.0) | 12.2 (3.8) | 12.4 (4.6) | 13.5 (5.6) | 14.0 (6.0) | 12.3 (4.5) | 0.264 |
| Sodium (mg) | 1526 (910) | 1343 (574) | 1472 (733) | 1533 (568) | 1525 (711) | 1393 (613) | 0.787 |
| Potassium (mg) | 1383 (362) | 1458 (436) | 1462 (545) | 1596 (542) | 1570 (535) | 1347 (431) | 0.443 |
| Calcium (mg) | 329 (147) | 431 (177) | 427 (142) | 402 (238) | 392 (225) | 365 (187) | 0.753 |
| Phosphorus (mg) | 592 (158) | 655 (194) | 696 (219) | 674 (185) | 674 (224) | 616 (171) | 0.845 |
| Magnesium (mg) | 143 (37) | 173 (59) | 167 (51) | 173 (70) | 164 (58) | 146 (50) | 0.999 |
| PP Population | |||||||
| Energy (kcal/day) | 1600 (292) | 1754 (382) | 1817 (287) | 1671 (303) | 1651 (317) | 1569 (323) | 0.153 |
| Energy (kcal/kg BW/day) | 26.0 (6.2) | 28.4 (6.6) | 29.5 (6.6) | 25.6 (5.5) | 25.4 (6.0) | 24.1 (5.6) | 0.028 * |
| Protein (g/kg BW/day) | 0.78 (0.20) | 0.77 (0.22) | 0.82 (0.20) | 0.80 (0.21) | 0.82 (0.23) | 0.74 (0.20) | 0.952 |
| Protein (% of energy) | 11.9 (2.0) | 10.6 (1.4) | 11.0 (1.3) | 12.4 (2.3) | 12.8 (3.2) | 12.3 (2.9) | 0.007 * |
| CHO (% of energy) | 51.9 (5.8) | 51.2 (6.0) | 51.6 (4.5) | 53.2 (6.9) | 52.5 (6.1) | 52.9 (7.3) | 0.326 |
| Fat (% of energy) | 36.2 (5.0) | 38.2 (5.5) | 37.4 (4.3) | 34.4 (6.1) | 34.7 (5.3) | 34.8 (5.8) | 0.013 * |
| SFA (g) | 15.4 (4.1) | 18.6 (4.2) | 18.9 (4.2) | 15.8 (5.2) | 15.2 (4.5) | 15.1 (4.4) | 0.008 * |
| MUFA (g) | 17.5 (5.4) | 26.0 (5.6) | 26.1 (4.6) | 18.9 (7.1) | 17.6 (5.6) | 16.8 (4.8) | <0.001 * |
| PUFA (g) | 26.2 (8.1) | 28.6 (8.2) | 28.7 (8.4) | 25.3 (8.7) | 25.1 (9.2) | 23.0 (7.2) | 0.045 * |
| EPA (mg) | 58 (118) | 233 (242) | 145 (116) | 49 (60) | 70 (153) | 108 (179) | 0.008 * |
| DHA (mg) | 142 (205) | 311 (412) | 193 (182) | 109 (78) | 173 (240) | 246 (320) | 0.371 |
| Fiber (g) | 12.5 (4.1) | 12.8 (3.7) | 13.0 (4.0) | 13.5 (5.6) | 14.0 (6.0) | 12.3 (4.5) | 0.563 |
| Sodium (mg) | 1508 (885) | 1376 (590) | 1521 (757) | 1533 (568) | 1525 (711) | 1393 (613) | 0.914 |
| Potassium (mg) | 1404 (325) | 1512 (421) | 1539 (536) | 1596 (542) | 1570 (535) | 1347 (431) | 0.835 |
| Calcium (mg) | 322 (137) | 446 (185) | 449 (129) | 402 (238) | 392 (225) | 365 (187) | 0.536 |
| Phosphorus (mg) | 596 (156) | 676 (196) | 718 (217) | 674 (185) | 674 (224) | 616 (171) | 0.821 |
| Magnesium (mg) | 142 (31) | 179 (60) | 176 (47) | 173 (70) | 164 (58) | 146 (50) | 0.621 |
| Parameter | HE-LPF Group (n = 38) | Control Group (n = 35) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 2 | Week 4 | Baseline | Week 2 | Week 4 | ||
| Renal function | |||||||
| eGFR (mL/min/1.73 m2) | 16.0 (8.5) | 15.9 (8.3) | 15.2 (8.2) | 17.3 (9.5) | 16.7 (9.1) | 17.4 (9.5) | 0.480 |
| BUN (mg/dL) | 58.4 (22.8) | 56.6 (22.4) | 58.6 (22.3) | 54.8 (29.7) | 57.7 (31.9) | 56.9 (29.8) | 0.818 |
| Creatinine (mg/dL) | 4.7 (2.2) | 4.8 (2.4) | 4.9 (2.4) | 4.9 (3.1) | 5.0 (3.1) | 5.0 (3.3) | 0.797 |
| Serum electrolytes | |||||||
| Sodium (mEq/L) | 138.9 (3.7) | 138.9 (3.7) | 139.1 (3.3) | 138.7 (3.5) | 138.6 (3.1) | 138.6 (3.1) | 0.635 |
| Chloride (mEq/L) a | 106.3 (4.5) | 105.9 (5.0) | 106.4 (4.0) | 106.9 (6.7) | 105.4 (4.2) | 105.6 (4.3) | 0.806 |
| Potassium (mEq/L) | 4.8 (0.7) | 4.7 (0.7) | 4.8 (0.6) | 4.6 (0.5) | 4.6 (0.4) | 4.7 (0.5) | 0.264 |
| Calcium (mg/dL) | 8.8 (0.9) | 8.7 (0.7) | 8.8 (0.8) | 9.0 (1.0) | 8.9 (0.9) | 9.0 (0.9) | 0.213 |
| Phosphorus (mg/dL) | 4.3 (0.7) | 4.3 (1.0) | 4.3 (0.7) | 4.2 (1.1) | 4.3 (1.3) | 4.3 (1.2) | 0.774 |
| Magnesium (mg/dL) | 2.2 (0.4) | — | 2.3 (0.3) | 2.2 (0.3) | — | 2.2 (0.4) | 0.902 |
| Plasma protein | |||||||
| Albumin (g/dL) | 4.2 (0.3) | 4.1 (0.3) | 4.2 (0.3) | 4.2 (0.3) | 4.1 (0.3) | 4.1 (0.3) | 0.780 |
| Prealbumin (g/L) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.0) | 0.3 (0.1) | 0.554 |
| Total protein (g/dL) | 7.0 (0.6) | 6.9 (0.6) | 7.0 (0.5) | 6.9 (0.6) | 6.8 (0.6) | 6.8 (0.5) | 0.337 |
| CRP (mg/dL) | 0.2 (0.2) | — | 0.2 (0.3) | 0.1 (0.2) | — | 0.3 (0.7) | 0.752 |
| Metabolic markers | |||||||
| Cholesterol (mg/dL) | 163.6 (38.1) | — | 162.3 (37.5) | 165.2 (41.3) | — | 162.8 (40.7) | 0.907 |
| Triglyceride (mg/dL) | 109.8 (52.5) | — | 126.2 (95.9) | 134.5 (55.9) | — | 125.6 (51.8) | 0.401 |
| LDL-C (mg/dL) | 90.3 (30.7) | — | 86.3 (25.5) | 94.9 (32.6) | — | 93.3 (32.5) | 0.412 |
| Uric acid (mg/dL) | 6.2 (1.9) | — | 6.0 (1.8) | 6.2 (1.9) | — | 5.8 (1.8) | 0.778 |
| HbA1c (%) | 5.8 (0.6) | — | 5.8 (0.6) | 6.1 (1.3) | — | 6.0 (1.2) | 0.208 |
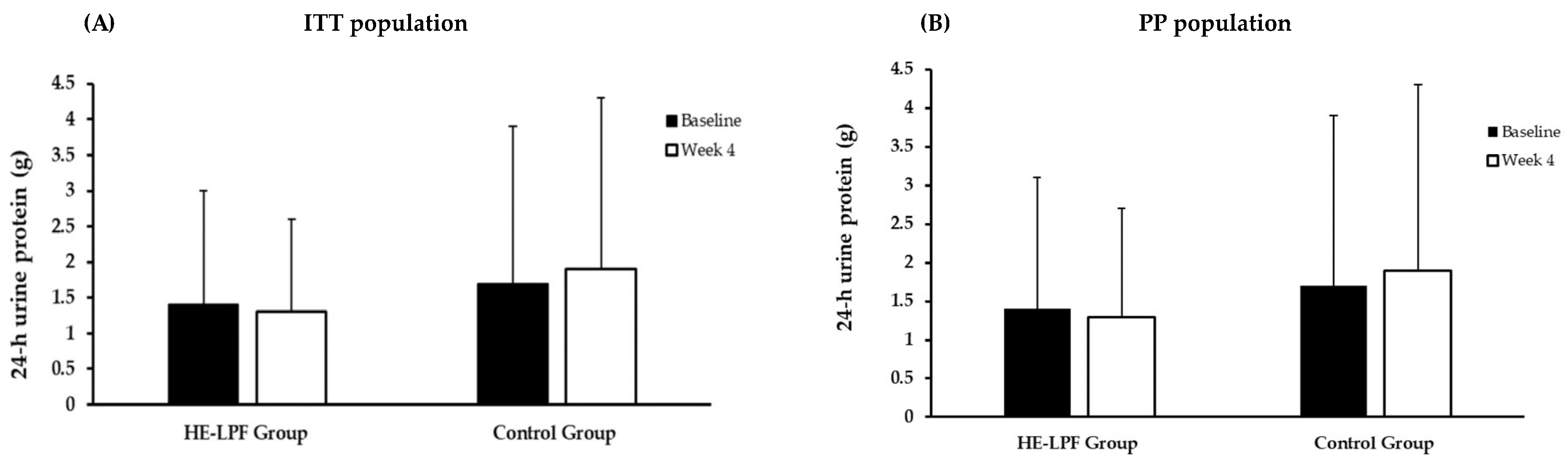
| 24 h urine collection | |||||||
| 24 h urine protein (g) | 1.4 (1.6) | 1.5 (1.7) | 1.3 (1.3) | 1.7 (2.2) | 1.6 (1.7) | 1.9 (2.4) | 0.411 |
| 24 h UUN (g) | 6.7 (2.8) | 6.7 (2.3) | 6.5 (2.3) | 7.1 (3.9) | 6.7 (2.6) | 7.4 (3.4) | 0.434 |
| Dietary protein intake (g/day) | 55.5 (18.5) | 55.7 (15.6) | 54.0 (15.6) | 59.2 (25.5) | 56.5 (16.9) | 61.2 (22.5) | 0.314 |
| Dietary protein intake (g/kg BW/day) | 0.89 (0.26) | 0.89 (0.20) | 0.86 (0.22) | 0.89 (0.38) | 0.86 (0.25) | 0.93 (0.32) | 0.835 |
| Parameter | HE-LPF Group (n = 33) | Control Group (n = 35) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 2 | Week 4 | Baseline | Week 2 | Week 4 | ||
| Renal function | |||||||
| eGFR (mL/min/1.73 m2) | 16.4 (8.8) | 16.3 (8.6) | 15.8 (8.5) | 17.3 (9.5) | 16.7 (9.1) | 17.4 (9.5) | 0.656 |
| BUN (mg/dL) | 57.2 (21.4) | 54.0 (20.8) | 56.8 (21.1) | 54.8 (29.7) | 57.7 (31.9) | 56.9 (29.8) | 0.944 |
| Creatinine (mg/dL) | 4.6 (2.3) | 4.7 (2.5) | 4.8 (2.5) | 4.9 (3.1) | 5.0 (3.1) | 5.0 (3.3) | 0.728 |
| Serum electrolytes | |||||||
| Sodium (mEq/L) | 139.5 (2.9) | 139.6 (3.1) | 139.6 (3.0) | 138.7 (3.5) | 138.6 (3.1) | 138.6 (3.1) | 0.188 |
| Chloride (mEq/L) a | 106.7 (3.9) | 106.3 (4.5) | 106.8 (3.9) | 106.9 (6.7) | 105.4 (4.2) | 105.6 (4.3) | 0.510 |
| Potassium (mEq/L) | 4.7 (0.7) | 4.7 (0.7) | 4.8 (0.6) | 4.6 (0.5) | 4.6 (0.4) | 4.7 (0.5) | 0.543 |
| Calcium (mg/dL) | 8.8 (0.9) | 8.7 (0.7) | 8.8 (0.8) | 9.0 (1.0) | 8.9 (0.9) | 9.0 (0.9) | 0.255 |
| Phosphorus (mg/dL) | 4.3 (0.7) | 4.3 (1.0) | 4.3 (0.7) | 4.2 (1.1) | 4.3 (1.3) | 4.3 (1.2) | 0.906 |
| Magnesium (mg/dL) | 2.3 (0.4) | 2.3 (0.4) | 2.2 (0.3) | 2.2 (0.4) | 0.595 | ||
| Plasma protein | |||||||
| Albumin (g/dL) | 4.2 (0.3) | 4.1 (0.3) | 4.2 (0.3) | 4.2 (0.3) | 4.1 (0.3) | 4.1 (0.3) | 0.826 |
| Prealbumin (g/L) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.0) | 0.3 (0.1) | 0.280 |
| Total protein (g/dL) | 7.0 (0.6) | 6.9 (0.6) | 7.0 (0.6) | 6.9 (0.6) | 6.8 (0.6) | 6.8 (0.5) | 0.333 |
| CRP (mg/dL) | 0.2 (0.2) | 0.2 (0.3) | 0.1 (0.2) | 0.3 (0.7) | 0.907 | ||
| Metabolic markers | |||||||
| Cholesterol (mg/dL) | 161.5 (37.0) | — | 159.5 (32.4) | 165.2 (41.3) | — | 162.8 (40.7) | 0.702 |
| Triglyceride (mg/dL) | 108.6 (55.2) | — | 112.9 (70.8) | 134.5 (55.9) | — | 125.6 (51.8) | 0.158 |
| LDL-C (mg/dL) | 89.2 (30.0) | — | 86.4 (24.7) | 94.9 (32.6) | — | 93.3 (32.5) | 0.384 |
| Uric acid (mg/dL) | 5.9 (1.6) | — | 5.8 (1.8) | 6.2 (1.9) | — | 5.8 (1.8) | 0.775 |
| HbA1c (%) | 5.8 (0.6) | — | 5.8 (0.6) | 6.1 (1.3) | — | 6.0 (1.2) | 0.214 |
| 24 h urine collection | |||||||
| 24 h urine protein (g) | 1.4 (1.7) | 1.5 (1.7) | 1.3 (1.4) | 1.7 (2.2) | 1.6 (1.7) | 1.9 (2.4) | 0.444 |
| 24 h UUN (g) | 6.9 (2.7) | 6.9 (2.3) | 6.7 (2.3) | 7.1 (3.9) | 6.7 (2.6) | 7.4 (3.4) | 0.656 |
| Dietary protein intake (g/day) | 56.7 (17.9) | 56.9 (15.5) | 55.3 (15.4) | 59.2 (25.5) | 56.5 (16.9) | 61.2 (22.5) | 0.510 |
| Dietary protein intake (g/kg BW/day) | 0.91 (0.25) | 0.91 (0.20) | 0.88 (0.22) | 0.89 (0.38) | 0.86 (0.25) | 0.93 (0.32) | 0.910 |
| Parameters | HE-LPF Group (n = 38) | Control Group (n = 35) | Overall (n = 73) |
|---|---|---|---|
| Diarrhea | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Abdominal distension | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Constipation | 3 (7.9) | 2 (5.7) | 5 (6.8) |
| Nausea | 2 (5.3) | 1 (2.9) | 3 (4.1) |
| Vomiting | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, W.-C.; Hsieh, H.-M.; Chen, J.-P.; Tsai, S.-F.; Chiu, H.-F.; Chung, M.-C.; Huang, S.-T.; Chen, Y.-Y.; Chen, C.-H. Efficacy and Safety of a High-Energy, Low-Protein Formula Replacement Meal for Pre-Dialysis Chronic Kidney Disease Patients: A Randomized Controlled Trial. Nutrients 2023, 15, 4506. https://doi.org/10.3390/nu15214506
Yang W-C, Hsieh H-M, Chen J-P, Tsai S-F, Chiu H-F, Chung M-C, Huang S-T, Chen Y-Y, Chen C-H. Efficacy and Safety of a High-Energy, Low-Protein Formula Replacement Meal for Pre-Dialysis Chronic Kidney Disease Patients: A Randomized Controlled Trial. Nutrients. 2023; 15(21):4506. https://doi.org/10.3390/nu15214506
Chicago/Turabian StyleYang, Wen-Ching, Hui-Min Hsieh, Jun-Peng Chen, Shang-Feng Tsai, Hsien-Fu Chiu, Mu-Chi Chung, Shih-Ting Huang, Yun-Yu Chen, and Cheng-Hsu Chen. 2023. "Efficacy and Safety of a High-Energy, Low-Protein Formula Replacement Meal for Pre-Dialysis Chronic Kidney Disease Patients: A Randomized Controlled Trial" Nutrients 15, no. 21: 4506. https://doi.org/10.3390/nu15214506
APA StyleYang, W.-C., Hsieh, H.-M., Chen, J.-P., Tsai, S.-F., Chiu, H.-F., Chung, M.-C., Huang, S.-T., Chen, Y.-Y., & Chen, C.-H. (2023). Efficacy and Safety of a High-Energy, Low-Protein Formula Replacement Meal for Pre-Dialysis Chronic Kidney Disease Patients: A Randomized Controlled Trial. Nutrients, 15(21), 4506. https://doi.org/10.3390/nu15214506







