Strategies to Reduce the Rate of Plate Waste in Hospitalized Patients: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Stage 1: Identifying the Research Questions
- What current strategies have been implemented to reduce the rate of plate waste in hospitals?
- What are the categories of strategies to reduce the rate of plate waste in hospitals?
- What are the impacts of the strategies on other parameters in addition to plate waste?
2.2. Stage 2: Identifying Relevant Studies
2.2.1. Search Terms
2.2.2. Databases
2.3. Stage 3: Selection of Studies
2.4. Stage 4: Data Extraction
2.5. Stage 5: Collating, Summarizing, and Reporting the Results
3. Results
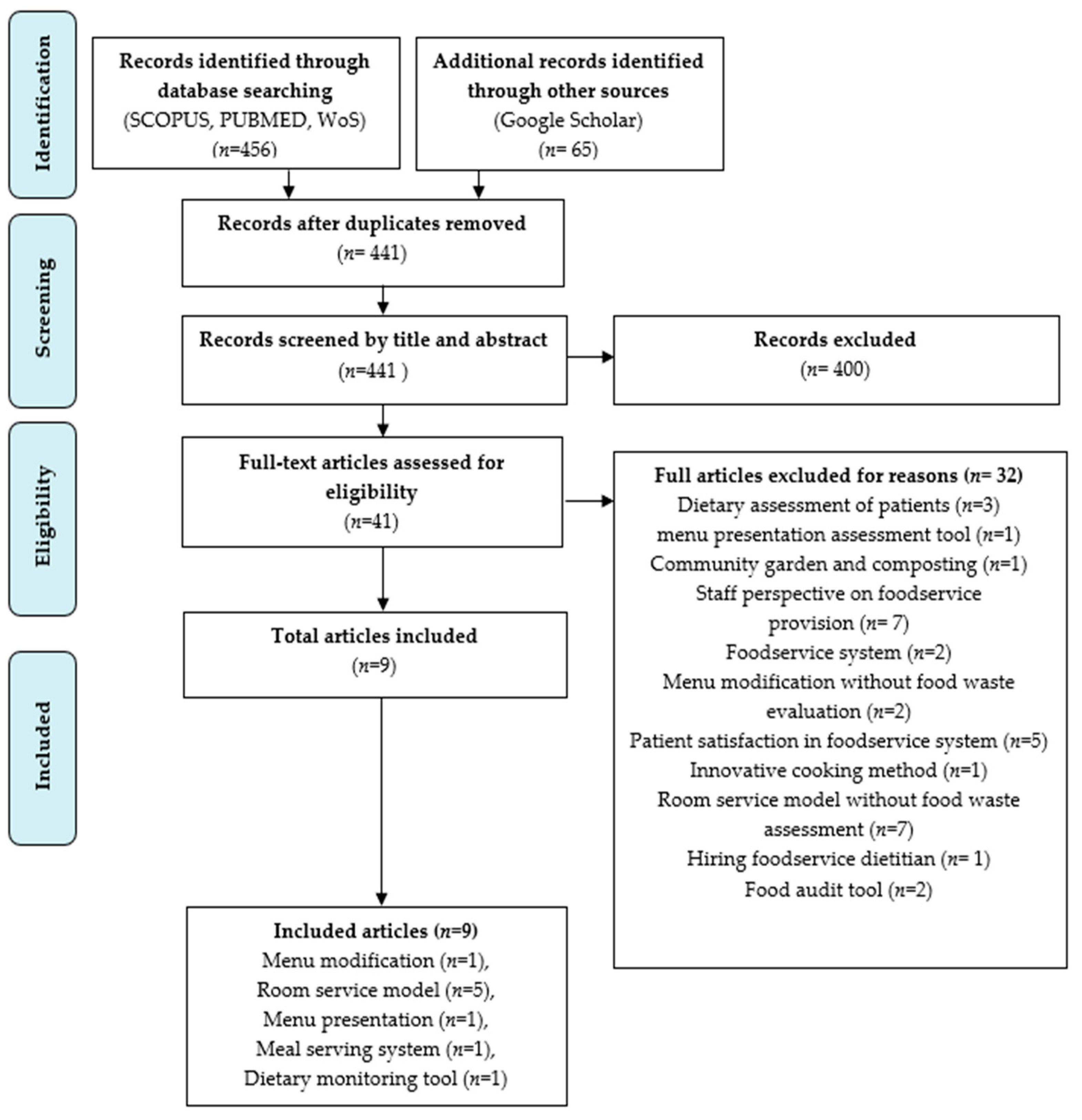
3.1. Selection of Sources of Evidence
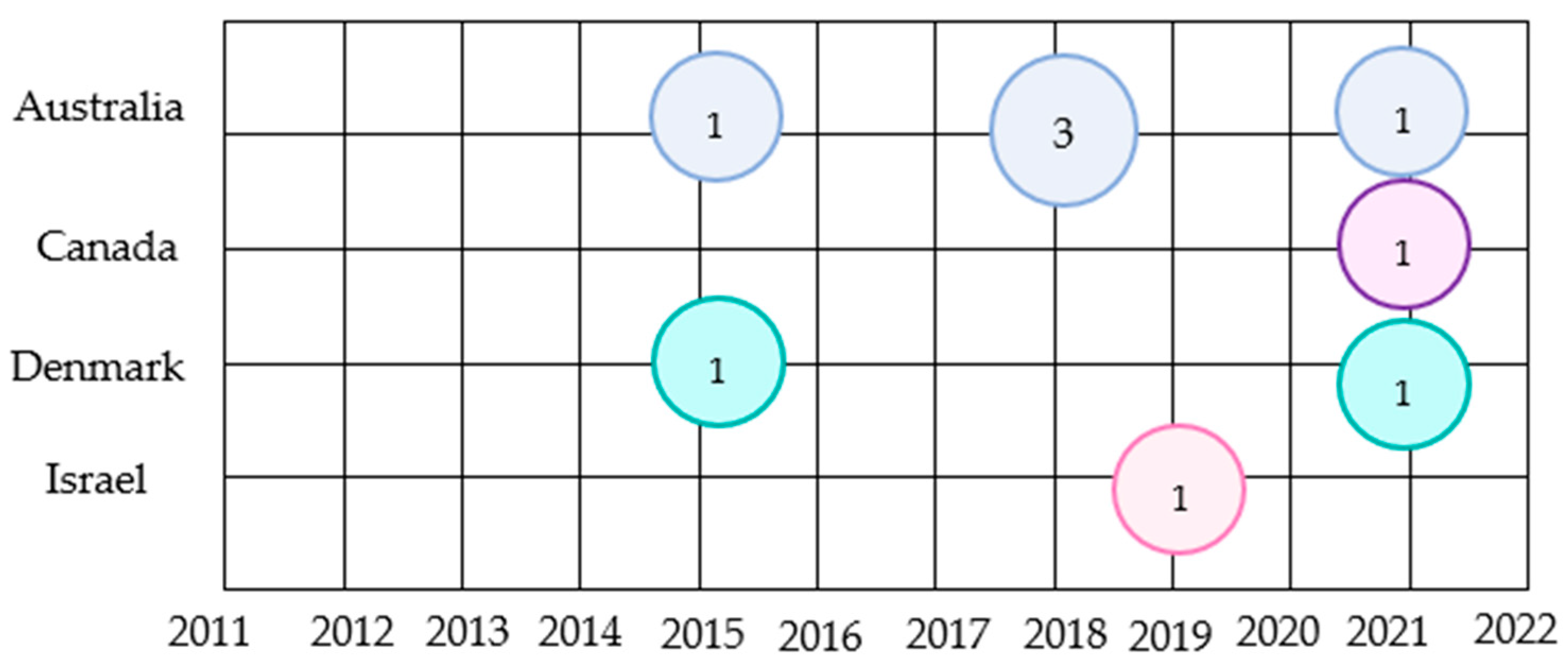
3.2. Study Characteristics and Patient Characteristics
3.3. Types of Strategies to Reduce the Rate of Plate Waste in Hospitals
| Author/Year/Country | Category of Strategy | Study Design | Patient’s Characteristics | Strategy | Pre-Intervention |
|---|---|---|---|---|---|
| Abou et al., 2021 (Canada) [34] | Room service model | Quasi-experimental study |
| Dining on Call (DOC) hospital foodservice
| Traditional foodservice
|
| Barrington et al., 2018 (Australia) [30] | Room service model | An observational point prevalence cohort study | For paper menu
| Patient-Directed Bedside Electronic Meal Ordering System (BMOS)
| Paper Menu (PM)
|
| Dynesen et al., 2021 (Denmark) [29] | Menu modification | A prospective cross-sectional study | Traditional trolley meal service
| Free Choice Menu (FCM).
| Traditional trolley meal service (trolley)
|
| Farrer et al., 2015 (Australia) [36] | Meal-serving system | A pilot study | Molded meals (treatment group)
| Molded smooth pureed meals
| Non-molded smooth pureed meals Served in the standard format |
| Navarro et al., 2019 (Israel) [35] | Meal presentation | A randomized intervention study | White napkin (control group)
| The addition of an orange napkin (experimental group) Cost approximately USD 0.05 for each napkin for the hospital meal tray | White napkin (control group) Received usual food trays with a white napkin |
| Neaves et al., 2021 (Australia) [32] | Room service model | A retrospective analysis | Thaw retherm service model
| On-demand room service model
| Bought-in, thaw-retherm foodservice model and cook-fresh
|
| McCray et al., 2018a (Australia) [33] | Roomservice model | A retrospective analysis | Traditional foodservice model
| Room service (RS)
| Traditional Model (TM)
|
| McCray et al., 2018b (Australia) [31] | Room service model | An observational point prevalence | Traditional paper menu ordering system (TM)
| Bedside meal ordering system (BMOS) model
| Traditional paper menu system (TM)
|
| Ofei et al., 2015 (Denmark) [28] | Dietary intake monitoring tool | A prospective observational cohort study | A trolley meal delivery system with dietary intake monitoring system (DIMS) technology
| Utilize a trolley meal delivery system with dietary intake monitoring system (DIMS) technology
| Trolley meal delivery system
|
| Author/Year/Country | Parameter | Findings | ||||
|---|---|---|---|---|---|---|
| Abou et al., 2021 (Canada) [34] |
| Tray waste | Patient Satisfaction | Food cost and labor cost per meal per day | ||
|
|
| ||||
| Barrington et al., 2018 (Australia) [30] |
| Plate waste | Dietary intake | Patient meal experience | ||
|
|
| ||||
| Dynesen et al., 2021 (Denmark) [29] |
| Plate waste | Nutritional intake | Portion Size | ||
|
|
| ||||
| Farrer et al., 2015 (Australia) [36] |
| Plate Waste | Patient Satisfaction | |||
| No statistical significance was seen in the hedonic rating of patient satisfaction with meals in the molded form as compared to the control group (p = 0.31) | |||||
| McCray et al., 2018a (Australia) [33] |
| Plate waste | Patient Satisfaction | Nutritional intake | Food cost | |
|
|
|
| |||
| McCray et al., 2018b (Australia) [31] |
| Plate waste | Patient Satisfaction | Nutritional intake | Nutrition assistant role and satisfaction | Food cost |
|
|
|
|
| ||
| Navarro et al., 2019 (Israel) [35] |
| Plate Waste | Patient Satisfaction | |||
|
| |||||
| Neaves et al., 2021 (Australia) [32] |
| Plate waste | Patient Satisfaction | Nutritional intake | Meal quality | Food cost |
|
|
|
|
| ||
| Ofei et al., 2015 (Denmark) [28] |
| Plate waste | Nutritional intake | |||
|
| |||||
3.4. The Impacts of the Strategies on Other Parameters and to Plate Waste
3.4.1. Method to Estimate Plate Waste
3.4.2. Patient Satisfaction
3.4.3. Nutritional Intake
3.4.4. Meal Quality
3.4.5. Food Cost
3.4.6. Portion Size
3.4.7. Nutrition Assistant Role and Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Visser-Amundson, A. A Multi-Stakeholder Partnership to Fight Food Waste in the Hospitality Industry: A Contribution to the United Nations Sustainable Development Goals 12 and 17. J. Sustain. Tour. 2020, 30, 2448–2475. [Google Scholar] [CrossRef]
- Kasavan, S.; Mohamed, A.F.; Halim, S.A. Drivers of food waste generation: Case study of island-based hotels in Langkawi, Malaysia. Waste Manag. 2019, 91, 72–79. [Google Scholar] [CrossRef] [PubMed]
- European Environmental Agency. What Are the Sources of Food Waste in Europe? 2016. Available online: https://www.eea.europa.eu/media/infographics/wasting-food−1/image/image_view_fullscreen (accessed on 26 October 2022).
- Benson, I. WRAP Running Month of Restaurant Food Waste Action. 2019. Available online: https://resource.co/article/wrap-runningmonth-restaurant-food-waste-action (accessed on 26 October 2022).
- Garcia-Garcia, G.; Woolley, E.; Rahimifard, S. A framework for a more efficient approach to food waste management. Int. J. Food Eng. 2015, 1, 65–72. [Google Scholar] [CrossRef]
- Zaki, A.H. Waste not, Want not—It’s Time We Get Serious about Food Waste. New Straits Times. 2019. Available online: https://www.nst.com.my/lifestyle/sunday-vibes/2019/09/525506/waste-not-want-not-%E2%80%93-its-time-we-get-serious-about-food-waste (accessed on 27 October 2022).
- Kasavan, S.; Nurul Izzati, M.A.; Masarudin, N.A. Quantification of solid waste in school canteens—A case study from a Hulu Selangor Municipality, Selangor. Plan. Malays. 2020, 18, 160–171. [Google Scholar] [CrossRef]
- Razalli, N.H.; Cheah, C.F.; Mohammad, N.M.A.; Manaf, Z.A. Plate waste study among hospitalised patients receiving texture-modified diet. Nutr. Res. Pract. 2021, 15, 655–671. [Google Scholar] [CrossRef]
- Chemah, T.C.; Nur Adilah, Z.; Sabaianah, B.; Zurinawati, M.; Aslinda Mohd, S. Plate Waste in Public Hospitals Foodservice Management in Selangor, Malaysia. Indian J. Sci. Technol. 2018, 11, 1–5. [Google Scholar] [CrossRef]
- Goonan, S.; Mirosa, M.; Spence, H. Getting a taste for food waste: A mixed methods ethnographic study into hospital food waste before patient consumption conducted at three New Zealand foodservice facilities. J. Acad. Nutr. Diet. 2014, 114, 63–71. [Google Scholar] [CrossRef]
- Alshqaqeeq, F.; Twomey, J.M.; Overcash, M.R. Food waste in hospitals. Int. J. Technol. Manag. 2018, 17, 186–196. [Google Scholar]
- Shahar, S.; Chee, K.Y.; Chik, W.; Pa, W.C. Food intakes and preferences of hospitalised geriatric patients. BMC Geriatr. 2002, 2, 1–6. [Google Scholar] [CrossRef]
- Aminuddin, N.; Vijayakumaran, R.; Abdul Razak, S. Patient Satisfaction with Hospital Foodservice and its Impact on Plate Waste in Public Hospitals in East Malaysia. Hosp. Pract. Resear. 2018, 3, 90–97. [Google Scholar] [CrossRef]
- Norshariza, J.; Siti Farrah Zaidah, M.; Basmawati, B.; Leow, C.; Lina, I.; Norafidza, A.; Khalizah, J.; John Kong, J.P.; Lim, S.M. Evaluation of Factors Affecting Food Wastage among Hospitalized Patients on Therapeutic Diet at Ministry of Health (MOH) Hospitals. Asian J. Diet. 2019, 1, 111–120. [Google Scholar]
- American Hospital Association. Fast Facts on U.S. Hospitals, 2019. Available online: https://www.aha.org/statistics/2020-01-07-archived-fast-facts-us-hospitals-2019 (accessed on 14 October 2022).
- Alshqaqeeq, F.; Twomey, J.; Overcash, M.; Sadkhi, A. A study of food waste in St. Francis Hospital. Int. J. Healthc. Manag. 2017, 13, 1–9. [Google Scholar] [CrossRef]
- Budiningsari, D.; Shahar, S.; Abdul Manaf, Z.; Susetyowati, S. Needs assessment for patient’s food intake monitoring among Indonesian healthcare professionals. Int. Nurs. Rev. 2018, 65, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Kontogianni, M.D.; Anna, K.; Bersimis, F.; Sulz, I.; Schindler, K.; Hiesmayr, M.; Chourdakis, M. Exploring factors influencing dietary intake during hospitalization: Results from analyzing Nutrition Day’s database (2006–2013). Clin. Nutr. ESPEN 2020, 38, 263–270. [Google Scholar] [CrossRef]
- Keller, H.; Allard, J.; Vesnaver, E.; Laporte, M.; Gramlich, L.; Bernier, P.; Davidson, B.; Duerksen, D.; Jeejeebhoy, K.; Payette, H. Barriers to food intake in acute care hospitals: A report of the Canadian Malnutrition Task Force. J. Hum. Nutr. Diet. 2015, 28, 546–557. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. JBI Evid. Implement. 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Williams, P.; Walton, K. Plate waste in hospitals and strategies for change. E-Spen. Eur. E J. Clin. Nutr. Metab. 2011, 6, e235–e241. [Google Scholar] [CrossRef]
- Daudt, H.M.; van Mossel, C.; Scott, S.J. Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med. Res. Methodol. 2013, 13, 48. [Google Scholar] [CrossRef] [PubMed]
- Pham, M.T.; Rajić, A.; Greig, J.D.; Sargeant, J.M.; Papadopoulos, A.; McEwen, S.A. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res. Synth. Methods 2014, 5, 371–385. [Google Scholar] [CrossRef] [PubMed]
- Khalil, H.; Peters, M.; Godfrey, C.M.; McInerney, P.; Soares, C.B.; Parker, D. An evidence-based approach to scoping reviews. Worldviews Evid.-Based Nurs. 2016, 13, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Ofei, K.T.; Holst, M.; Rasmussen, H.H.; Mikkelsen, B.E. Effect of meal portion size choice on plate waste generation among patients with different nutritional status. An investigation using Dietary Intake Monitoring System (DIMS). Appetite 2015, 91, 157–164. [Google Scholar] [CrossRef]
- Dynesen, A.W.; Snitkjær, P.; Andreasen, L.S.; Elgaard, L.; Aaslyng, M.D. Eat what you want and when you want. Effect of a free choice menu on the energy and protein intake of geriatric medical patients. Clin. Nutr. ESPEN 2021, 46, 288–296. [Google Scholar] [CrossRef]
- Barrington, V.; Maunder, K.; Kelaart, A. Engaging the patient: Improving dietary intake and meal experience through bedside terminal meal ordering for oncology patients. J. Hum. Nutr. Diet. 2018, 31, 803–809. [Google Scholar] [CrossRef]
- McCray, S.; Maunder, K.; Norris, R.; Moir, J.; MacKenzie-Shalders, K. Bedside Menu Ordering System increases energy and protein intake while decreasing plate waste and food costs in hospital patients. Clin. Nutr. ESPEN 2018, 26, 66–71. [Google Scholar] [CrossRef]
- Neaves, B.; Bell, J.J.; McCray, S. Impact of room service on nutritional intake, plate and production waste, meal quality and patient satisfaction and meal costs: A single site pre-post evaluation. Nutr. Diet. 2022, 79, 187–196. [Google Scholar] [CrossRef]
- McCray, S.; Maunder, K.; Barsha, L.; Mackenzie-Shalders, K. Room service in a public hospital improves nutritional intake and increases patient satisfaction while decreasing food waste and cost. J. Hum. Nutr. Diet. 2018, 31, 734–741, 18. [Google Scholar] [CrossRef]
- Abou El Hassan, D.; Lewis, R.; Howe, N.; Vlietstra, E. Dining on Call: Outcomes of a hospital patient dining model. In Healthcare Management Forum; SAGE Publications: Los Angeles, CA, USA, 2021; Volume 34, pp. 336–339. [Google Scholar]
- Navarro, D.A.; Shapiro, Y.; Birk, R.; Boaz, M. Orange napkins increase food intake and satisfaction with hospital food service: A randomized intervention. Nutrition 2019, 67, 100008. [Google Scholar] [CrossRef]
- Farrer, O.; Olsen, C.; Mousley, K.; Teo, E. Does presentation of smooth pureed meals improve patients consumption in an acute care setting: A pilot study. Nutr. Diet. 2015, 73, 405–409. [Google Scholar] [CrossRef]
- Sherwin, A.J.; Nowson, C.A.; McPhee, J.; Alexander, J.L.; Wark, J.D.; Flicker, L. Nutrient intake at meals in residential care facilities for the aged: Validated visual estimation of plate waste. Aust J. Nutr. Diet. 1998, 55, 188–193. [Google Scholar]
- Comstock, E.M.; St Pierre, R.G.; Mackiernan, Y.D. Measuring individual plate waste in school lunches. Visual estimation and children’s ratings vs. actual weighing of plate waste. J. Am. Diet. Assoc. 1981, 79, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Graves, K.; Shannon, B. Using visual plate waste measurement to assess school lunch food behaviour. J. Am. Diet. Assoc. 1983, 82, 163–165. [Google Scholar]
- Hiesmayr, M.; Schindler, K.; Pernicka, E.; Schuh, C.; Schoeniger-Hekeler, A.; Bauer, P.; Laviano, A.; Lovell, A.; Mouhieddine, M.; Schuetz, T.; et al. Decreased food intake is a risk factor for mortality in hospitalised patients: The Nutrition Day survey 2006. Clin. Nutr. 2009, 28, 484–491. [Google Scholar] [CrossRef]
- Kandiah, J.; Stinnett, L.; Lutton, D. Visual plate waste in hospitalized patients: Length of stay and diet order. J. Am. Diet. Assoc 2006, 106, 1663–1666. [Google Scholar] [CrossRef]
- Capra, S.; Wright, O.; Sardie, M.; Bauer, J.; Askew, D. The acute hospital foodservice patient satisfaction questionnaire: The development of a valid and reliable tool to measure patient satisfaction with acute care hospital foodservices. Foodserv. Res. Int. 2005, 16, 1–14. [Google Scholar] [CrossRef]
- Pullen, K.; Collins, R.; Stone, T.; Carter, H.; Sadler, H.; Collinson, A. Are energy and protein requirements met in hospital? J. Hum. Nutr. Diet. 2018, 31, 178–187. [Google Scholar] [CrossRef]
- do Rosario, V.A.; Walton, K. Hospital Food Service. In Handbook of Eating and Drinking: Interdisciplinary Perspectives; Springer International Publishing: Cham, Switzerland, 2019; pp. 1–27. [Google Scholar]
- Hartwell, H.J.; Shepherd, P.A.; Edwards, J.S.A.; Johns, N. What do patients value in the hospital meal experience? Appetite 2016, 96, 293–298. [Google Scholar] [CrossRef]
- Sao Joao, E.A.; Spowart, J.; Taylor, A. Employee training contributes to service quality and therefore sustainability. Tour. Leis. 2019, 8, 1–15. [Google Scholar]
- Vijayakumaran, R.K.; Eves, A.; Margaret, L. Understanding Patients’ Meal Experiences through Staff’s Role: Study on Malaysian Public Hospitals. Hosp. Pract. Resear. 2018, 3, 50–58. [Google Scholar] [CrossRef]
- Vijayakumaran, R.K.; Eves, A.; Lumbers, M. Patients Emotions during Meal Experience: Understanding through Critical Incident Technique. Int. J. Hosp. Res 2016, 5, 113–121. [Google Scholar]
| Searched Terms | |
|---|---|
| Concept | strategy OR policy OR guidelines OR procedure AND food service OR meal service AND |
| Context | hospital food waste AND hospital plate waste |
| Population | AND hospitalized patients |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manimaran, S.; Razalli, N.H.; Abdul Manaf, Z.; Mat Ludin, A.F.; Shahar, S. Strategies to Reduce the Rate of Plate Waste in Hospitalized Patients: A Scoping Review. Nutrients 2023, 15, 301. https://doi.org/10.3390/nu15020301
Manimaran S, Razalli NH, Abdul Manaf Z, Mat Ludin AF, Shahar S. Strategies to Reduce the Rate of Plate Waste in Hospitalized Patients: A Scoping Review. Nutrients. 2023; 15(2):301. https://doi.org/10.3390/nu15020301
Chicago/Turabian StyleManimaran, Sangeetha, Nurul Huda Razalli, Zahara Abdul Manaf, Arimi Fitri Mat Ludin, and Suzana Shahar. 2023. "Strategies to Reduce the Rate of Plate Waste in Hospitalized Patients: A Scoping Review" Nutrients 15, no. 2: 301. https://doi.org/10.3390/nu15020301
APA StyleManimaran, S., Razalli, N. H., Abdul Manaf, Z., Mat Ludin, A. F., & Shahar, S. (2023). Strategies to Reduce the Rate of Plate Waste in Hospitalized Patients: A Scoping Review. Nutrients, 15(2), 301. https://doi.org/10.3390/nu15020301








