Barriers in the Management of Obesity in Mexican Children and Adolescents through the COVID-19 Lockdown—Lessons Learned and Perspectives for the Future
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Demographics
3.2. Lifestyles
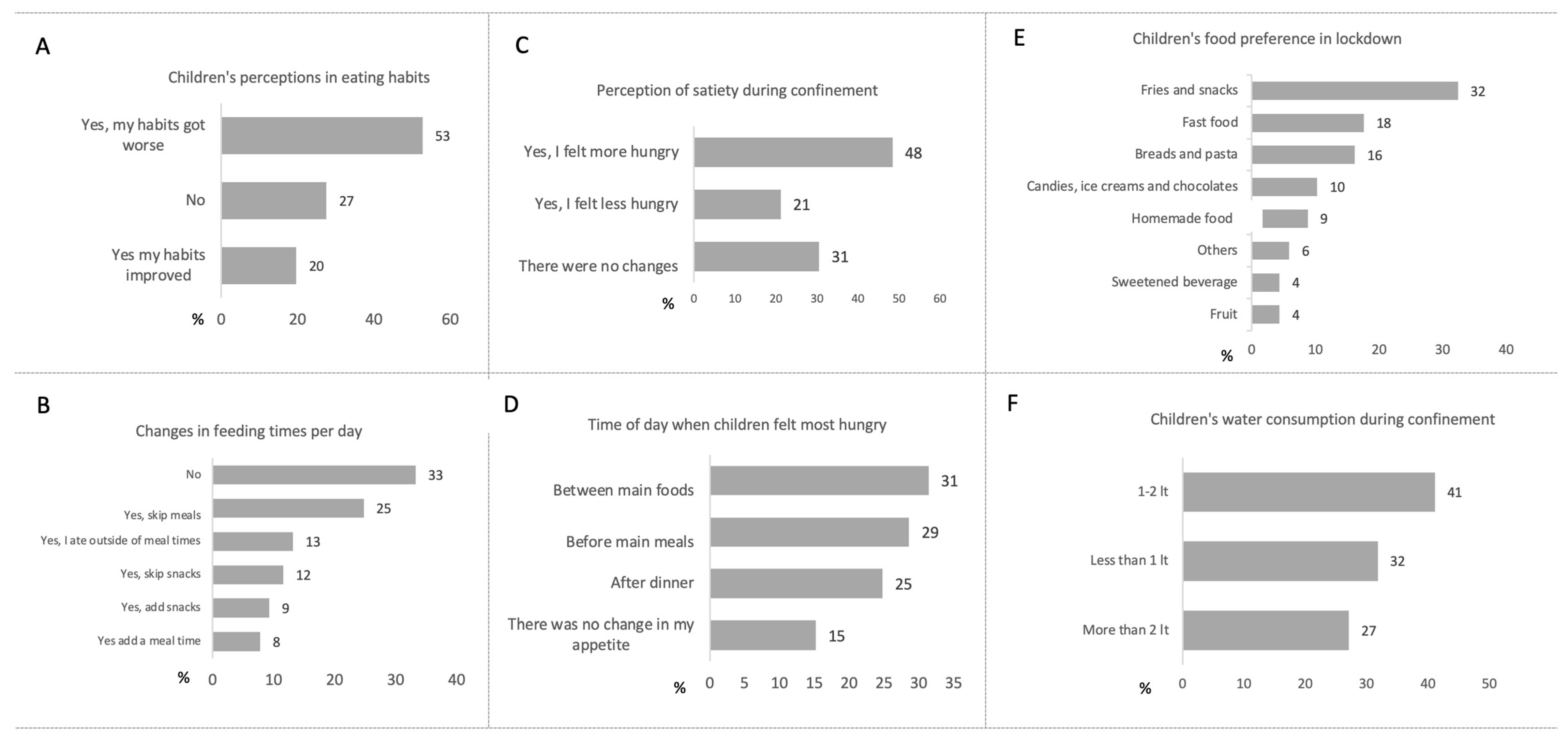
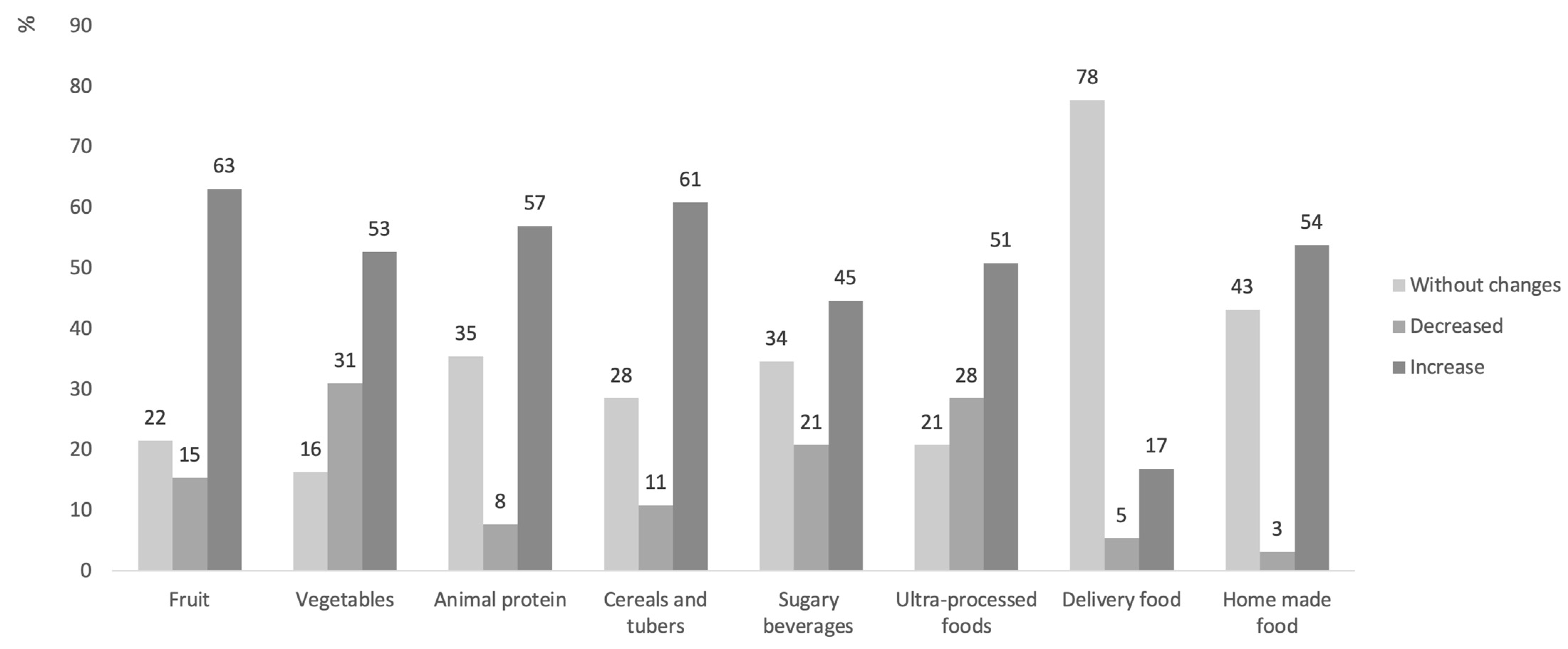
3.3. Food and Feeding
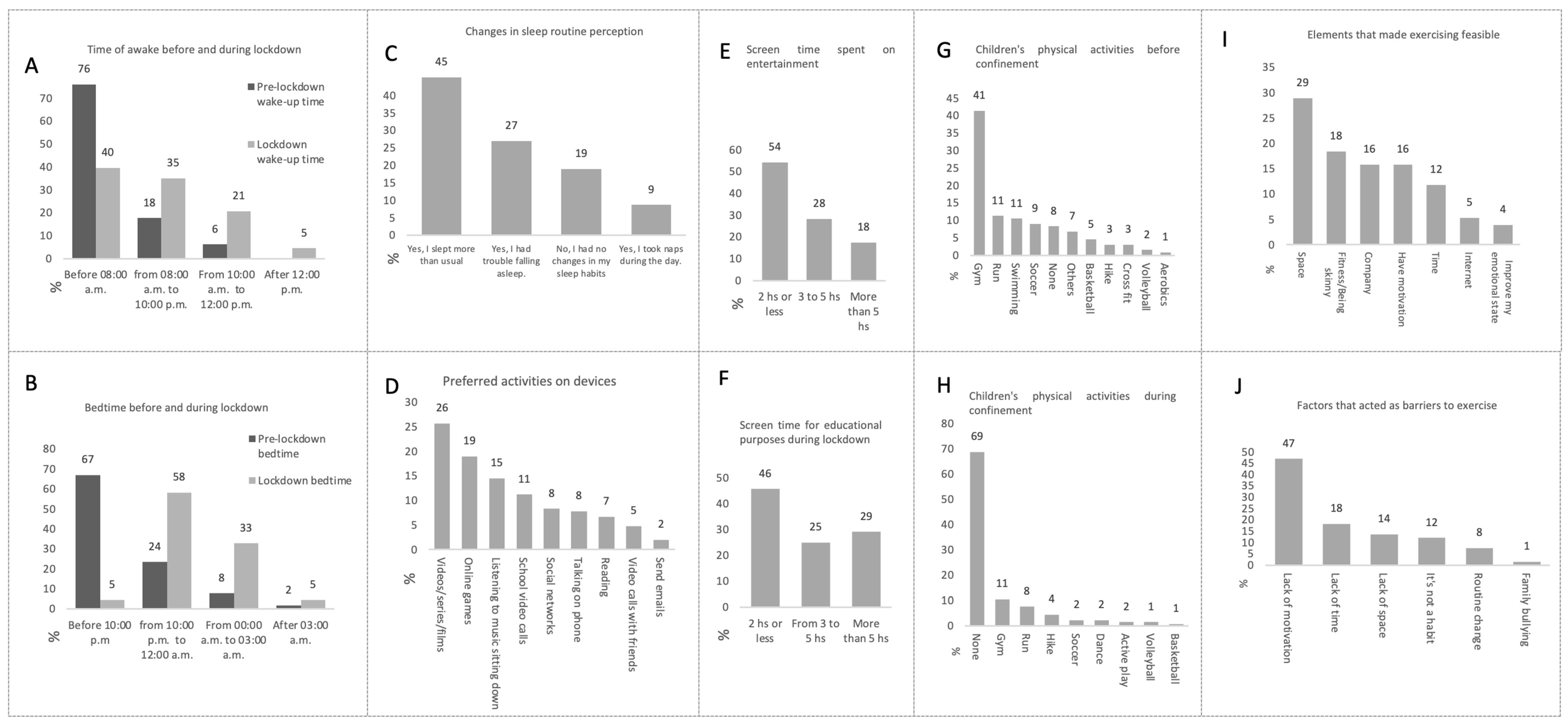
3.4. Sleep Patterns, Sedentary Lifestyle, and Physical Activity
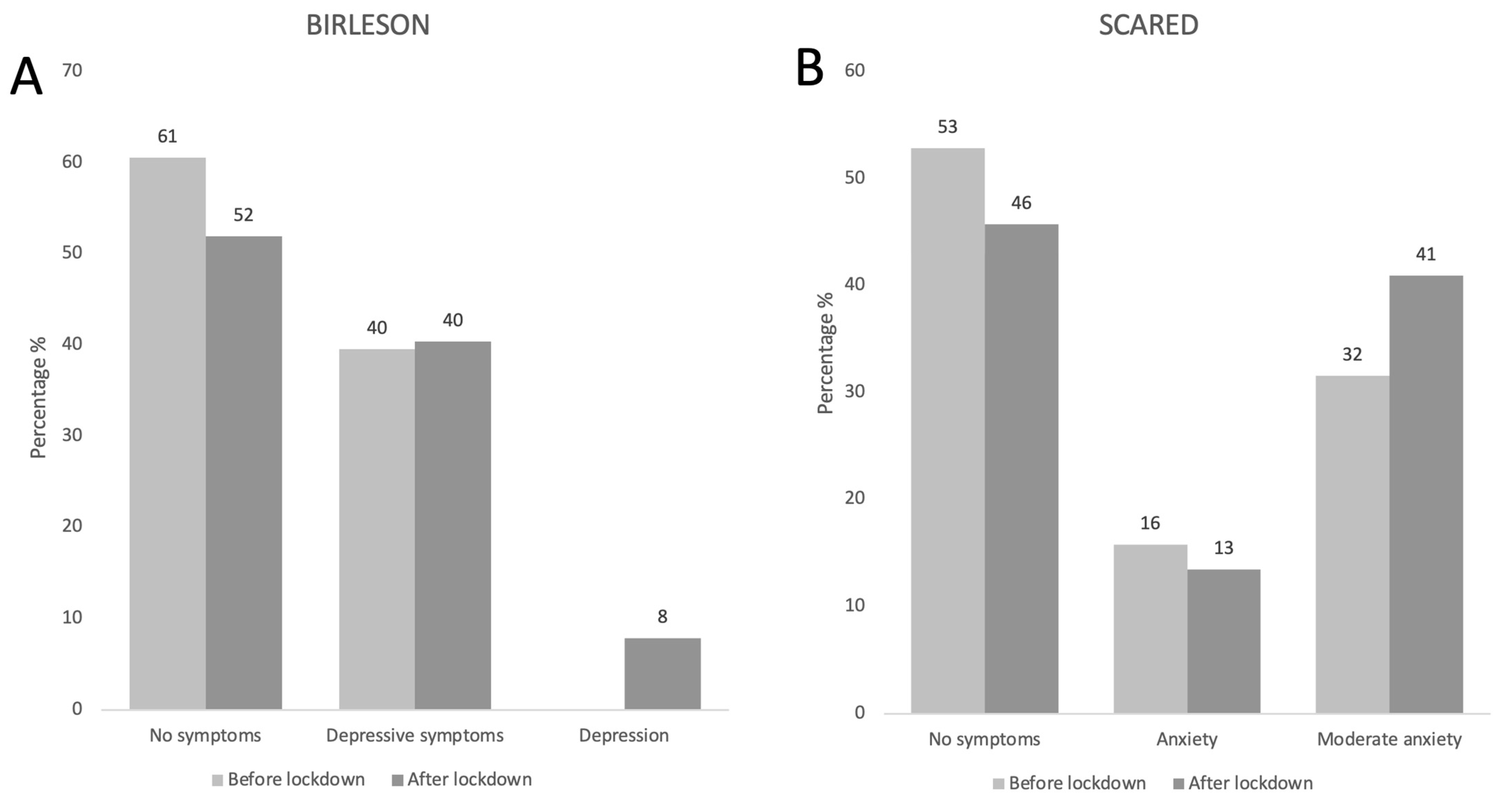
3.5. Mental Health
3.6. Changes in Body Composition, Metabolic Markers, and Anthropometric Measurements
3.7. e-Health
3.8. General Perception of the Pandemic and Lockdown
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470. [Google Scholar] [CrossRef]
- Araújo, L.A.d.; Veloso, C.F.; Souza, M.d.C.; Azevedo, J.M.C.d.; Tarro, G. The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. J. Pediatr. 2021, 97, 369–377. [Google Scholar] [CrossRef]
- Sideli, L.; Lo Coco, G.; Bonfanti, R.C.; Borsarini, B.; Fortunato, L.; Sechi, C.; Micali, N. Effects of COVID-19 lockdown on eating disorders and obesity: A systematic review and meta-analysis. In European Eating Disorders Review; John Wiley and Sons Ltd.: Hoboken, NJ, USA, 2021; Volume 29, pp. 826–841. [Google Scholar]
- Fernández-Aranda, F.; Munguía, L.; Mestre-Bach, G.; Steward, T.; Etxandi, M.; Baenas, I.; Granero, R.; Sánchez, I.; Ortega, E.; Andreu, A.; et al. COVID Isolation Eating Scale (CIES): Analysis of the impact of confinement in eating disorders and obesity—A collaborative international study. In European Eating Disorders Review; John Wiley and Sons Ltd.: Hoboken, NJ, USA, 2020; pp. 871–883. [Google Scholar]
- Balakrishnan, V.; Zhen Ng, W.; Chong Soo, M.; Joo Han, G.; Jiat Lee, C. Infodemic and fake news-A comprehensive overview of its global magnitude during the COVID-19 pandemic in 2021: A scoping review. Int. J. Disaster Risk Reduct. 2022, 78, 2212–4209. [Google Scholar] [CrossRef]
- Pian, W.; Chi, J.; Ma, F. “Infodemic”: A systematic review using narrative synthesis. Inf. Process. Manag. 2021, 58, 102713. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Liu, C. Infodemic vs. Pandemic Factors Associated to Public Anxiety in the Early Stage of the COVID-19 Outbreak: A Cross-Sectional Study in China. Front Public Health 2021, 9, 723648. [Google Scholar] [CrossRef]
- Gray, K.L.; Birtles, H.; Reichelt, K.; James, I.A. The experiences of care home staff during the COVID-19 pandemic: A systematic review. Aging Ment. Health 2021, 26, 2080–2089. Available online: https://www.tandfonline.com/doi/abs/10.1080/13607863.2021.2013433 (accessed on 2 May 2023). [CrossRef]
- Bakaloudi, D.R.; Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Chourdakis, M. Impact of the first COVID-19 lockdown on body weight: A combined systematic review and a meta-analysis. Clin. Nutr. 2022, 41, 3046–3054. [Google Scholar] [CrossRef]
- Quagliariello, V.; Bonelli, A.; Caronna, A.; Conforti, G.; Iovine, M.; Carbone, A.; Berretta, M.; Botti, G.; Maurea, N. SARS-CoV-2 Infection and Cardioncology: From Cardiometabolic Risk Factors to Outcomes in Cancer Patients. Cancers 2020, 12, 3316. [Google Scholar] [CrossRef] [PubMed]
- Stavridou, A.; Kapsali, E.; Panagouli, E.; Thirios, A.; Polychronis, K.; Bacopoulou, F.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Obesity in children and adolescents during covid-19 pandemic. Children 2021, 8, 135. [Google Scholar] [CrossRef]
- Badesha, H.S.; Bagri, G.; Nagra, A.; Nijran, K.; Singh, G.; Aiyegbusi, O.L. Tackling childhood overweight and obesity after the COVID-19 pandemic. Lancet Child Adolesc. Health 2021, 5, 687–688. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.; Lu, X.; Xiao, T. The influence of neighborhood built environment on school-age children’s outdoor leisure activities and obesity: A case study of Shanghai central city in China. Front. Public Health 2023, 11, 1168077. [Google Scholar] [CrossRef]
- An, R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: A microsimulation model. J. Sport Health Sci. 2020, 9, 302–312. [Google Scholar] [CrossRef]
- Franckle, R.; Adler, R.; Davison, K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: A systematic review. Prev. Chronic Dis. 2014, 11, E101. [Google Scholar] [CrossRef] [PubMed]
- von Hippel, P.T.; Powell, B.; Downey, D.B.; Rowland, N.J. The effect of school on overweight in childhood: Gain in body mass index during the school year and during summer vacation. Am. J. Public Health 2007, 97, 696–702. [Google Scholar] [CrossRef]
- Wang, Y.C.; Vine, S.; Hsiao, A.; Rundle, A.; Goldsmith, J. Weight-Related Behaviors When Children Are in School Versus on Summer Breaks: Does Income Matter? J. Sch. Health 2015, 85, 458–466. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/josh.12274 (accessed on 2 May 2023). [CrossRef]
- Técnico Diario, C. COVID-19 MÉXICO. Available online: https://www.gob.mx/cms/uploads/attachment/file/618867/CP_Salud_CTD_coronavirus_COVID-19__27feb21.pdf (accessed on 1 May 2023).
- Hampl, S.E.; Hassink, S.G.; Skinner, A.C.; Armstrong, S.C.; Barlow, S.E.; Bolling, C.F.; Edwards, K.C.A.; Eneli, I.; Hamre, R.; Joseph, M.M.; et al. CLINICAL PRACTICE GUIDELINE Guidance for the Clinician in Rendering Pediatric Care Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity. Available online: http://publications.aap.org/pediatrics/article-pdf/151/2/e2022060640/1451060/peds_2022060640.pdf (accessed on 16 July 2023).
- Fulkerson, J.A.; Friend, S.; Horning, M.; Flattum, C.; Draxten, M.; Neumark-Sztainer, D.; Gurvich, O.; Garwick, A.; Story, M.; Kubik, M.Y. Family Home Food Environment and Nutrition-Related Parent and Child Personal and Behavioral Outcomes of the Healthy Home Offerings via the Mealtime Environment (HOME) Plus Program: A Randomized Controlled Trial. J. Acad. Nutr. Diet. 2018, 118, 240–251. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Rolland, B.; Haesebaert, F.; Zante, E.; Benyamina, A.; Haesebaert, J.; Franck, N. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: Survey study. JMIR Public Health Surveill 2020, 6, e19630. [Google Scholar] [CrossRef] [PubMed]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Ruiz-Roso, M.B.; de Carvalho Padilha, P.; Mantilla-Escalante, D.C.; Ulloa, N.; Brun, P.; Acevedo-Correa, D.; Arantes Ferreira Peres, W.; Martorell, M.; Aires, M.T.; de Oliveira Cardoso, L.; et al. Covid-19 confinement and changes of adolescent’s dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 2020, 12, 1807. [Google Scholar] [CrossRef]
- Di Pierro, F.; Khan, A.; Iqtadar, S.; Mumtaz, S.U.; Chaudhry, M.N.A.; Bertuccioli, A.; Derosa, G.; Maffioli, P.; Togni, S.; Riva, A.; et al. Quercetin as a possible complementary agent forearly-stage COVID-19: Concluding results of a randomized clinical trial. Front. Pharmacol. 2023, 13, 1096853. [Google Scholar] [CrossRef]
- Vlieg-Boerstra, B.; de Jong, N.; Meyer, R.; Agostoni, C.; De Cosmi, V.; Grimshaw, K.; Milani, G.P.; Muraro, A.; Elberink, H.O.; Pali-Schöll, I.; et al. Nutrient supplementation for prevention of viral respiratory tract infections in healthy subjects: A systematic review and meta-analysis. Allergy 2022, 77, 1373–1388. [Google Scholar] [CrossRef] [PubMed]
- Adams, E.L.; Caccavale, L.J.; Smith, D.; Bean, M.K. Food Insecurity, the Home Food Environment, and Parent Feeding Practices in the Era of COVID-19. Obesity 2020, 28, 2056–2063. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, A.B.; van Tilburg, W.A.P.; Igou, E.R.; Wisman, A.; Donnelly, A.E.; Mulcaire, J.B. Eaten up by boredom: Consuming food to escape awareness of the bored self. Front Psychol. 2015, 6, 369. [Google Scholar] [CrossRef] [PubMed]
- Ruíz-Roso, M.B.; de Carvalho Padilha, P.; Matilla-Escalante, D.C.; Brun, P.; Ulloa, N.; Acevedo-Correa, D.; Arantes Ferreira Peres, W.; Martorell, M.; Rangel Bousquet Carrilho, T.; de Oliveira Cardoso, L.; et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during covid-19 pandemic: An observational study. Nutrients 2020, 12, 2289. [Google Scholar] [CrossRef] [PubMed]
- Cellini, N.; Di Giorgio, E.; Mioni, G.; Di Riso, D. Sleep and Psychological Difficulties in Italian School-Age Children During COVID-19 Lockdown. J. Pediatr. Psychol. 2021, 46, 153–167. [Google Scholar] [CrossRef] [PubMed]
- Vrabec, A.; Yuhas, M.; Deyo, A.; Kidwell, K. Social jet lag and eating styles in young adults. Chronobiol Int. 2022, 39, 1277–1284. [Google Scholar] [CrossRef]
- Zhu, B.; Wang, Y.; Yuan, J.; Mu, Y.; Chen, P.; Srimoragot, M.; Li, Y.; Park, C.G.; Reutrakul, S. Associations between sleep variability and cardiometabolic health: A systematic review. Sleep Med. Reviews 2022, 66, 101688. [Google Scholar] [CrossRef]
- Sokouti, M.; Shafiee-Kandjani, A.R.; Sokouti, M.; Sokouti, B. A meta-analysis of systematic reviews and meta-analyses to evaluate the psychological consequences of COVID-19. BMC Psychol. 2023, 11, 279. [Google Scholar] [CrossRef] [PubMed]
- Rouhani, P.; Lotfi, K.; Anjom-Shoae, J.; Hajhashemi, Z.; Mokhtari, E.; Heidari, Z.; Saneei, P. Association between patterns of nutrient intake and circulating vitamin D with sleep status among Iranian adults. Sci. Rep. 2023, 13, 15318. [Google Scholar] [CrossRef] [PubMed]
- Quek, Y.H.; Tam, W.W.S.; Zhang, M.W.B.; Ho, R.C.M. Exploring the association between childhood and adolescent obesity and depression: A meta-analysis. Obes. Rev. 2017, 18, 742–754. [Google Scholar] [CrossRef]
- Suchomlinov, A.; Konstantinov, V.V.; Purlys, P. Associations between depression, height and bodymass index in adolescent and adult population of Penza city and oblast, Russia. J. Biosoc. Sci. 2021, 53, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Wu, Y.; Fan, S.; Dal Santo, T.; Li, L.; Jiang, X.; Li, K.; Wang, Y.; Tasleem, A.; Krishnan, A.; et al. Comparison of mental health symptoms before and during the covid-19 pandemic: Evidence from a systematic review and meta-analysis of 134 cohorts. BMJ 2023, 380, e074224. [Google Scholar] [CrossRef]
- Abawi, O.; Welling, M.S.; van den Eynde, E.; van Rossum, E.F.; Halberstadt, J.; van den Akker, E.L.; van der Voorn, B. COVID-19 related anxiety in children and adolescents with severe obesity: A mixed-methods study. Clin. Obes. 2020, 10, e12412. [Google Scholar] [CrossRef]
- Linardon, J.; Shatte, A.; Tepper, H.; Fuller-Tyszkiewicz, M. A survey study of attitudes toward, and preferences for, e-therapy interventions for eating disorder psychopathology. Int. J. Eat. Disord. 2020, 53, 907–916. [Google Scholar] [CrossRef] [PubMed]
- Traore, S.S.; Bo, Y.; Kou, G.; Lyu, Q. Socioeconomic inequality in overweight/obesity among US children: NHANES 2001 to 2018. Front. Pediatric. 2023, 11, 1082558. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Lijuan, W.; Huan, C.; Hao, L.; Yuan, C. Study on the relationship between the distribution and substitution of 24-hour activity time and the body mass index of children: Based on a component analysis model School of Physical Education and Sport Training. Sports Sci. 2022, 42, 77–84. [Google Scholar] [CrossRef]

| Patients | Range | Mean | SD | |
|---|---|---|---|---|
| Age (years) | 8–12 | 32% | 13 | 3 |
| 12–18 | 68% | |||
| Sex (M: W) | 61: 68 | 47%: 52% | ||
| Overweight | 25% | |||
| Obesity | 75% | |||
| Parents/guardians | ||||
| Age (years) | 18–35 | 34% | 40 | 8 |
| 36–60 | 64% | |||
| 60 and over | 3% | |||
| Relationship | Grandmother | 3% | ||
| Grandfather | 1% | |||
| Mother | 87% | |||
| Father | 6% | |||
| Aunt | 3% | |||
| Others | 1% | |||
| Educational level | Non | 1% | ||
| Elementary school | 8% | |||
| Junior high school | 38% | |||
| High school or equivalent | 31% | |||
| Degree | 19% | |||
| Other | 1% | |||
| Marital status | Single | 17% | ||
| Concubinage | 29% | |||
| Married | 41% | |||
| Divorcee | 5% | |||
| Separated | 9% | |||
| Number of family members at home | 2–4 members | 57% | ||
| 5–9 members | 38% | |||
| over 10 | 5% | |||
| Mean | SD | p | ||
|---|---|---|---|---|
| BMI | pre | 26 | 4 | <0.001 |
| post | 29 | 5 | ||
| BMI z-score | pre | 1.83 | 0.38 | 0.01 |
| post | 1.96 | 0.39 | ||
| BMI percentile | pre | 96 | 3 | 0.01 |
| post | 97 | 3 | ||
| Waist (cm) | pre | 88 | 14 | <0.001 |
| post | 97 | 13 | ||
| WHtR (cm) | pre | 0.58 | 0.1 | 0.03 |
| post | 0.60 | 0.1 | ||
| Fat mass (%) | pre | 32 | 10 | <0.001 |
| post | 34 | 10 | ||
| Lean mass (%) | pre | 71 | 8 | <0.008 |
| post | 66 | 11 | ||
| Adiposity percentage (%) | pre | 23 | 18 | 0.002 |
| post | 32 | 23 | ||
| Uric acid (mg/dL) | pre | 5.6 | 1 | 0.16 |
| post | 5.9 | 1 | ||
| ALT (IU/L) | pre | 38 | 36 | 0.23 |
| post | 27 | 20 | ||
| AST (IU/L) | pre | 31 | 26 | 0.10 |
| post | 22 | 8 | ||
| Total cholesterol (mg/dL) | pre | 165 | 33 | 0.40 |
| post | 156 | 32 | ||
| HDL cholesterol (mg/dL) | pre | 39 | 6 | 0.17 |
| post | 36 | 10 | ||
| LDL cholesterol (mg/dL) | pre | 112 | 35 | 0.53 |
| post | 106 | 32 | ||
| Triglycerides (mg/dL) | pre | 156 | 74 | 0.81 |
| post | 161 | 67 | ||
| Fasting glucose (mg/dL) | pre | 89 | 7 | 0.047 |
| post | 93 | 6 | ||
| Hemoglobin A1c (%) | pre | 5.7 | 0.4 | 0.33 |
| post | 5.8 | 0.3 | ||
| Basal insuline (mg/dL) | pre | 23 | 16 | 0.29 |
| post | 17 | 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arellano-Alvarez, P.; Muñoz-Guerrero, B.; Ruiz-Barranco, A.; Garibay-Nieto, N.; Hernandez-Lopez, A.M.; Aguilar-Cuarto, K.; Pedraza-Escudero, K.; Fuentes-Corona, Z.; Villanueva-Ortega, E. Barriers in the Management of Obesity in Mexican Children and Adolescents through the COVID-19 Lockdown—Lessons Learned and Perspectives for the Future. Nutrients 2023, 15, 4238. https://doi.org/10.3390/nu15194238
Arellano-Alvarez P, Muñoz-Guerrero B, Ruiz-Barranco A, Garibay-Nieto N, Hernandez-Lopez AM, Aguilar-Cuarto K, Pedraza-Escudero K, Fuentes-Corona Z, Villanueva-Ortega E. Barriers in the Management of Obesity in Mexican Children and Adolescents through the COVID-19 Lockdown—Lessons Learned and Perspectives for the Future. Nutrients. 2023; 15(19):4238. https://doi.org/10.3390/nu15194238
Chicago/Turabian StyleArellano-Alvarez, Paulina, Brenda Muñoz-Guerrero, Alejandra Ruiz-Barranco, Nayely Garibay-Nieto, Ana María Hernandez-Lopez, Karina Aguilar-Cuarto, Karen Pedraza-Escudero, Zendy Fuentes-Corona, and Erendira Villanueva-Ortega. 2023. "Barriers in the Management of Obesity in Mexican Children and Adolescents through the COVID-19 Lockdown—Lessons Learned and Perspectives for the Future" Nutrients 15, no. 19: 4238. https://doi.org/10.3390/nu15194238
APA StyleArellano-Alvarez, P., Muñoz-Guerrero, B., Ruiz-Barranco, A., Garibay-Nieto, N., Hernandez-Lopez, A. M., Aguilar-Cuarto, K., Pedraza-Escudero, K., Fuentes-Corona, Z., & Villanueva-Ortega, E. (2023). Barriers in the Management of Obesity in Mexican Children and Adolescents through the COVID-19 Lockdown—Lessons Learned and Perspectives for the Future. Nutrients, 15(19), 4238. https://doi.org/10.3390/nu15194238







