Patterns and Predictors of Low-Calorie Sweetener Consumption during Pregnancy: Findings from a National Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Sample Size Estimation
2.3. Assessments
2.3.1. LCS Consumption
2.3.2. Assessment of Covariates
2.4. Statistical Analysis
2.4.1. Latent Class Analysis
2.4.2. Predictors of LCS Consumption Patterns
3. Results
3.1. Participant Characteristics
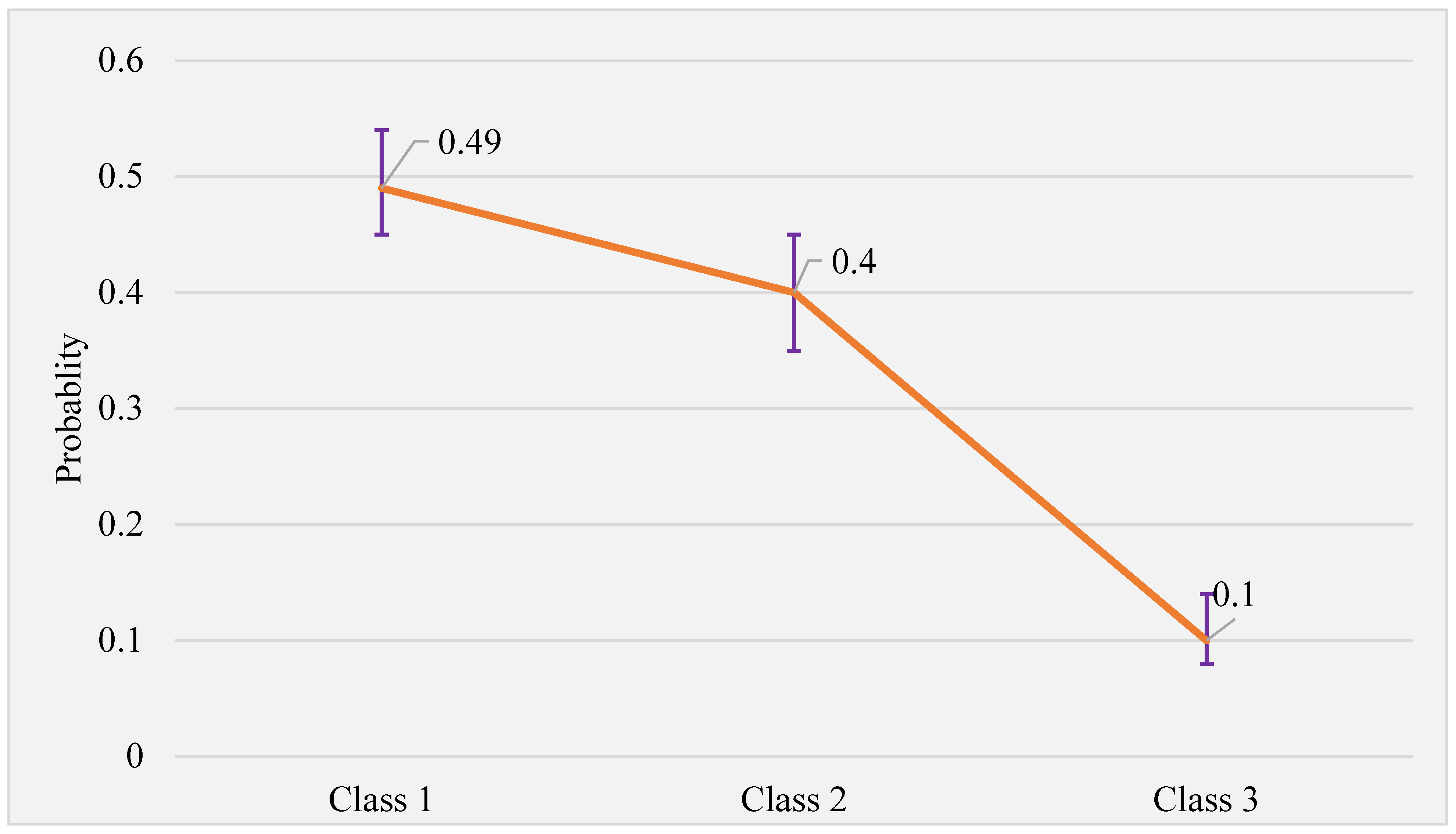
3.2. Latent Class Identification
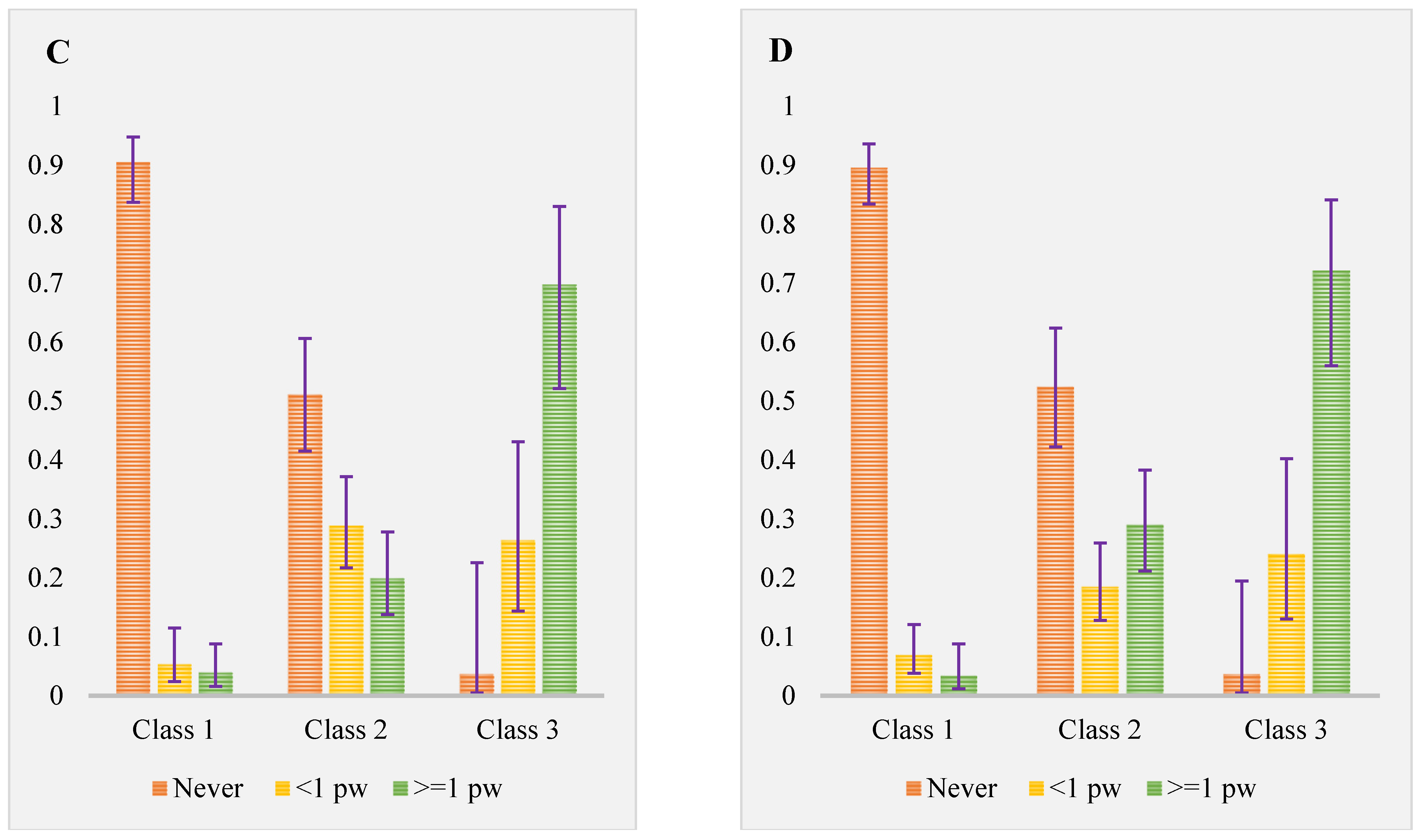
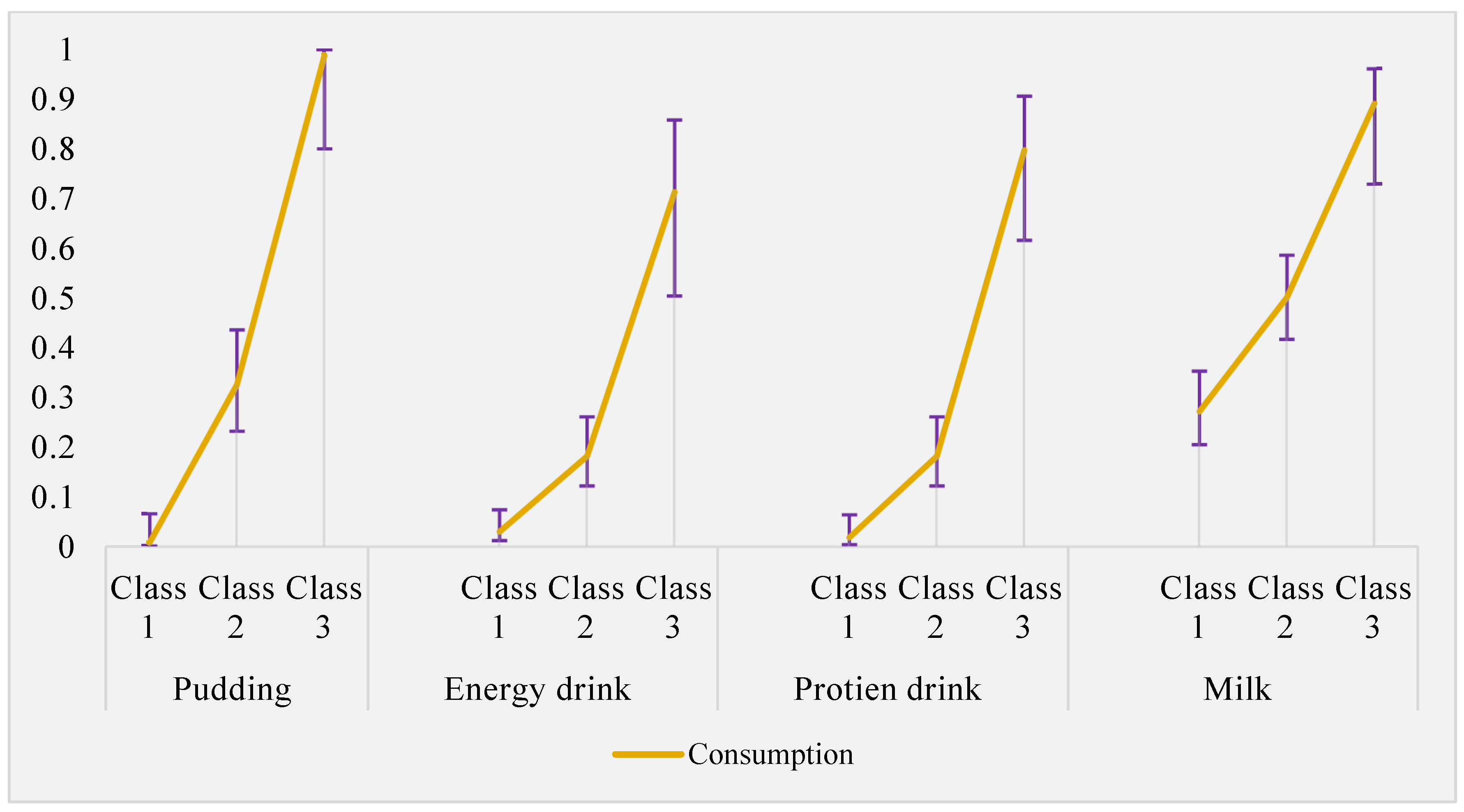
3.3. Latent Class Description
3.4. Prevalence, Reason for Consumption, and Safety Perception
3.5. Predictors of Moderate and Habitual LCS Consumption
4. Discussion
4.1. Prevalence of LCS Consumption
4.2. Predictors of Moderate and Habitual LCS Consumption
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hosseinpour-Niazi, S.; Aghayan, M.; Mirmiran, P.; Azizi, F. Does weight change modify the association between the consumption of sugar-sweetened beverages and 100% fruit juice and the risk of metabolic syndrome? Clin. Nutr. 2021, 40, 5261–5268. [Google Scholar] [CrossRef] [PubMed]
- Bradley, P. Diet composition and obesity. Lancet 2012, 379, 1100. [Google Scholar] [CrossRef] [PubMed]
- Benton, D. Can artificial sweeteners help control body weight and prevent obesity? Nutr. Res. Rev. 2005, 18, 63–76. [Google Scholar] [CrossRef]
- Sylvetsky, A.C.; Rother, K.I. Trends in the consumption of low-calorie sweeteners. Physiol. Behav. 2016, 164, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Swithers, S.E. Artificial sweeteners are not the answer to childhood obesity. Appetite 2015, 93, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Tandel, K.R. Sugar substitutes: Health controversy over perceived benefits. J. Pharmacol. Pharmacother. 2011, 2, 236–243. [Google Scholar] [CrossRef]
- Pepino, M.Y.J.P. Metabolic effects of non-nutritive sweeteners. Physiol. Behav. 2015, 152, 450–455. [Google Scholar] [CrossRef]
- Swithers, S.E. Artificial sweeteners produce the counterintuitive effect of inducing metabolic derangements. Trends Endocrinol. Metab. 2013, 24, 431–441. [Google Scholar] [CrossRef]
- Meng, Y.; Li, S.; Khan, J.; Dai, Z.; Li, C.; Hu, X.; Shen, Q.; Xue, Y. Sugar- and Artificially Sweetened Beverages Consumption Linked to Type 2 Diabetes, Cardiovascular Diseases, and All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 2636. [Google Scholar] [CrossRef]
- Zhang, X.; Li, X.; Liu, L.; Hong, F.; Zhao, H.; Chen, L.; Zhang, J.; Jiang, Y.; Zhang, J.; Luo, P. Dose-response association between sugar- and artificially sweetened beverage consumption and the risk of metabolic syndrome: A meta-analysis of population-based epidemiological studies. Public Health Nutr. 2021, 24, 3892–3904. [Google Scholar] [CrossRef]
- Azad, M.B.; Abou-Setta, A.M.; Chauhan, B.F.; Rabbani, R.; Lys, J.; Copstein, L.; Mann, A.; Jeyaraman, M.M.; Reid, A.E.; Fiander, M.; et al. Nonnutritive sweeteners and cardiometabolic health: A systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ 2017, 189, E929–E939. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Noronha, J.C.; Khan, T.A.; McGlynn, N.; Back, S.; Grant, S.M.; Kendall, C.W.C.; Sievenpiper, J.L. The Effect of Non-Nutritive Sweetened Beverages on Postprandial Glycemic and Endocrine Responses: A Systematic Review and Network Meta-Analysis. Nutrients 2023, 15, 1050. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.S.H.; Zhu, R.; Kjølbæk, L.; Raben, A. Effect of Non- and Low-Caloric Sweeteners on Substrate Oxidation, Energy Expenditure, and Catecholamines in Humans—A Systematic Review. Nutrients 2023, 15, 2711. [Google Scholar] [PubMed]
- Cai, C.; Sivak, A.; Davenport, M.H. Effects of prenatal artificial sweeteners consumption on birth outcomes: A systematic review and meta-analysis. Public Health Nutr. 2021, 24, 5024–5033. [Google Scholar] [CrossRef]
- Wang, Q.P.; Lin, Y.Q.; Zhang, L.; Wilson, Y.A.; Oyston, L.J.; Cotterell, J.; Qi, Y.; Khuong, T.M.; Bakhshi, N.; Planchenault, Y.; et al. Sucralose Promotes Food Intake through NPY and a Neuronal Fasting Response. Cell Metab. 2016, 24, 75–90. [Google Scholar] [CrossRef]
- Suez, J.; Korem, T.; Zeevi, D.; Zilberman-Schapira, G.; Thaiss, C.A.; Maza, O.; Israeli, D.; Zmora, N.; Gilad, S.; Weinberger, A.; et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 2014, 514, 181–186. [Google Scholar] [CrossRef]
- Mennella, J.A.; Bobowski, N.K.; Reed, D.R. The development of sweet taste: From biology to hedonics. Rev. Endocr. Metab. Disord. 2016, 17, 171–178. [Google Scholar] [CrossRef]
- Concha, F.; Sambra, V.; Cáceres, P.; López-Arana, S.; Carvajal, B.; Gotteland, M. Maternal consumption and perinatal exposure to non-nutritive sweeteners: Should we be concerned? Front. Pediatr. 2023, 11, 1200990. [Google Scholar] [CrossRef]
- Archibald, A.J.; Dolinsky, V.W.; Azad, M.B. Early-Life Exposure to Non-Nutritive Sweeteners and the Developmental Origins of Childhood Obesity: Global Evidence from Human and Rodent Studies. Nutrients 2018, 10, 194. [Google Scholar] [CrossRef]
- Probst, Y.C.; Dengate, A.; Jacobs, J.; Louie, J.C.; Dunford, E.K. The major types of added sugars and non-nutritive sweeteners in a sample of Australian packaged foods. Public Health Nutr. 2017, 20, 3228–3233. [Google Scholar] [CrossRef]
- Sylvetsky, A.C.; Figueroa, J.; Rother, K.I.; Goran, M.I.; Welsh, J.A. Trends in Low-Calorie Sweetener Consumption among Pregnant Women in the United States. Curr. Dev. Nutr. 2019, 3, nzz004. [Google Scholar] [CrossRef]
- Conway, M.C.; Cawley, S.; Geraghty, A.A.; Walsh, N.M.; O’Brien, E.C.; McAuliffe, F.M. The consumption of low-calorie sweetener containing foods during pregnancy: Results from the ROLO study. Eur. J. Clin. Nutr. 2022, 76, 227–234. [Google Scholar] [CrossRef]
- WHO. Use of Non-Sugar Sweeteners: WHO Guideline; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- Tein, J.Y.; Coxe, S.; Cham, H. Statistical Power to Detect the Correct Number of Classes in Latent Profile Analysis. Struct. Equ. Model. 2013, 20, 640–657. [Google Scholar] [CrossRef]
- Malek, L.; Umberger, W.; Makrides, M.; Zhou, S.J. Adherence to the Australian dietary guidelines during pregnancy: Evidence from a national study. Public Health Nutr. 2016, 19, 1155–1163. [Google Scholar] [CrossRef]
- Food Standards Australia New Zealand. Consumption of Intense Sweeteners in Australia and New Zealand; Food Standards Australia New Zealand: Canberra, Australia, 2003.
- González-Rodríguez, M.; Redruello-Requejo, M.; Samaniego-Vaesken, M.L.; Montero-Bravo, A.; Puga, A.M.; Partearroyo, T.; Varela-Moreiras, G. Low- and No-Calorie Sweetener (LNCS) Presence and Consumption among the Portuguese Adult Population. Nutrients 2021, 13, 4186. [Google Scholar] [CrossRef]
- Drewnowski, A.; Rehm, C.D. Socio-demographic correlates and trends in low-calorie sweetener use among adults in the United States from 1999 to 2008. Eur. J. Clin. Nutr. 2015, 69, 1035–1041. [Google Scholar] [CrossRef]
- Sylvetsky, A.C.; Welsh, J.A.; Brown, R.J.; Vos, M.B. Low-calorie sweetener consumption is increasing in the United States. Am. J. Clin. Nutr. 2012, 96, 640–646. [Google Scholar] [CrossRef]
- Catenacci, V.A.; Pan, Z.; Thomas, J.G.; Ogden, L.G.; Roberts, S.A.; Wyatt, H.R.; Wing, R.R.; Hill, J.O. Low/No calorie sweetened beverage consumption in the National Weight Control Registry. Obesity 2014, 22, 2244–2251. [Google Scholar] [CrossRef]
- Sylvetsky, A.C.; Jin, Y.; Clark, E.J.; Welsh, J.A.; Rother, K.I.; Talegawkar, S.A. Consumption of Low-Calorie Sweeteners among Children and Adults in the United States. J. Acad. Nutr. Diet. 2017, 117, 441–448.e2. [Google Scholar] [CrossRef]
- Grech, A.; Kam, C.O.; Gemming, L.; Rangan, A. Diet-Quality and Socio-Demographic Factors Associated with Non-Nutritive Sweetener Use in the Australian Population. Nutrients 2018, 10, 833. [Google Scholar] [CrossRef]
- American Heart Association. American Heart Association Recommendations for Physical Activity in Adults and Kids; American Heart Association: Dallas, TX, USA, 2018. [Google Scholar]
- Australin Bureau of Statstics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2016; Australin Bureau of Statstics: Canberra, Australia, 2016.
- National Health and Medical Research Council. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013.
- Palatnik, A.; Moosreiner, A.; Olivier-Van Stichelen, S. Consumption of non-nutritive sweeteners during pregnancy. Am. J. Obstet. Gynecol. 2020, 223, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Qin, P.; Li, Q.; Zhao, Y.; Chen, Q.; Sun, X.; Liu, Y.; Li, H.; Wang, T.; Chen, X.; Zhou, Q.; et al. Sugar and artificially sweetened beverages and risk of obesity, type 2 diabetes mellitus, hypertension, and all-cause mortality: A dose-response meta-analysis of prospective cohort studies. Eur. J. Epidemiol. 2020, 35, 655–671. [Google Scholar] [CrossRef] [PubMed]
- Sotres-Alvarez, D.; Herring, A.H.; Siega-Riz, A.M. Latent Class Analysis Is Useful to Classify Pregnant Women into Dietary Patterns. J. Nutr. 2010, 140, 2253–2259. [Google Scholar] [CrossRef] [PubMed]
- Sinha, P.; Calfee, C.S.; Delucchi, K.L. Practitioner’s Guide to Latent Class Analysis: Methodological Considerations and Common Pitfalls. Crit. Care Med. 2021, 49, e63–e79. [Google Scholar] [CrossRef] [PubMed]
- Vermunt, J.K.; Magidson, J.; Hagenaars, J.A.; McCutcheon, A.L. Applied Latent Class Analysis; Cambridge University Press: Cambridge, UK, 2002. [Google Scholar]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. Multidiscip. J. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Dziak, J.J.; Coffman, D.L.; Lanza, S.T.; Li, R.; Jermiin, L.S. Sensitivity and specificity of information criteria. Brief. Bioinform. 2020, 21, 553–565. [Google Scholar] [CrossRef]
- Szwajcer, E.M.; Hiddink, G.J.; Koelen, M.A.; van Woerkum, C.M. Nutrition-related information-seeking behaviours before and throughout the course of pregnancy: Consequences for nutrition communication. Eur. J. Clin. Nutr. 2005, 59 (Suppl. S1), S57–S65. [Google Scholar] [CrossRef]
- Ross, A.; Willson, V.L. Hierarchical multiple regression analysis using at least two sets of variables (in two blocks). In Basic and Advanced Statistical Tests; Brill: Leiden, The Netherlands, 2017; pp. 59–74. [Google Scholar]
- Johnston, R.; Jones, K.; Manley, D. Confounding and collinearity in regression analysis: A cautionary tale and an alternative procedure, illustrated by studies of British voting behaviour. Qual. Quant. 2018, 52, 1957–1976. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Apparent Consumption of Selected Foodstuffs, Australia. Available online: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/apparent-consumption-selected-foodstuffs-australia/latest-release#non-alcoholic-beverages (accessed on 15 June 2023).
- Azad, M.B.; Sharma, A.K.; de Souza, R.J.; Dolinsky, V.W.; Becker, A.B.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; Lefebvre, D.L.; Sears, M.R. Association Between Artificially Sweetened Beverage Consumption During Pregnancy and Infant Body Mass Index. JAMA Pediatr. 2016, 170, 662–670. [Google Scholar] [CrossRef]
- Alharthi, S.A.S.; Alaisayi, K.H.A.; Alalawi, L.Y.S.; Alamri, R.O.S.; Abu-Elfotuh, K.; Alenazi, T.S.; Amirthalingam, P.; Albariqi, H.A.H.; Mohammed, A.A.; Alsubayti, N.; et al. The consumption pattern and perception of using artificial sweeteners among the public in Tabuk region, Saudi Arabia. Front. Public Health 2023, 11, 1166868. [Google Scholar] [CrossRef]
- Farhat, G.; Dewison, F.; Stevenson, L. Knowledge and Perceptions of Non-Nutritive Sweeteners within the UK Adult Population. Nutrients 2021, 13, 444. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.M.; McGowan, C.A.; Mahony, R.; Foley, M.E.; McAuliffe, F.M. Low glycaemic index diet in pregnancy to prevent macrosomia (ROLO study): Randomised control trial. BMJ Br. Med. J. 2012, 345, e5605. [Google Scholar] [CrossRef] [PubMed]
- Hill, S.E.; Prokosch, M.L.; Morin, A.; Rodeheffer, C.D. The effect of non-caloric sweeteners on cognition, choice, and post-consumption satisfaction. Appetite 2014, 83, 82–88. [Google Scholar] [CrossRef]
- Goran, M.I.; Plows, J.F.; Ventura, E.E. Effects of consuming sugars and alternative sweeteners during pregnancy on maternal and child health: Evidence for a secondhand sugar effect. Proc. Nutr. Soc. 2019, 78, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Donazar-Ezcurra, M.; Lopez-del Burgo, C.; Martinez-Gonzalez, M.A.; Basterra-Gortari, F.J.; de Irala, J.; Bes-Rastrollo, M. Soft drink consumption and gestational diabetes risk in the SUN project. Clin. Nutr. 2018, 37, 638–645. [Google Scholar] [CrossRef]
- Andrade, C. The Limitations of Online Surveys. Indian J. Psychol. Med. 2020, 42, 575–576. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Births, Australia; ABS: Canberra, Australia, 2021.
- Molin, E.; Mokhtarian, P.; Kroesen, M. Multimodal travel groups and attitudes: A latent class cluster analysis of Dutch travelers. Transp. Res. Part A Policy Pract. 2016, 83, 14–29. [Google Scholar] [CrossRef]

| Characteristics | Category | Overall | Low-Calorie Sweetener Consumption Pattern | |||
|---|---|---|---|---|---|---|
| Infrequent or Non-Consumer (n = 209) | Moderate Consumer (n = 169) | Habitual Consumer (n = 44) | p-Value | |||
| Age (year) | 30.0 ± 4.6 | 30.7 ± 4.3 | 29.5 ± 4.9 | 29.0 ± 4.8 | 0.013 | |
| BMI (kg/m2) | 27.1 ± 6.5 | 27.3 ± 6.5 | 27.4 ± 6.6 | 24.8 ± 5.5 | 0.052 | |
| Diet quality score | 47.2 ± 16.2 | 48.8 ± 15.7 | 45.4 ± 15.9 | 46.2 ± 18.6 | 0.124 | |
| Educational level | Secondary | 82 (19.4) | 41 (19.6) | 34 (20.1) | 7 (15.9) | 0.037 |
| Post-secondary but no tertiary | 148 (35.1) | 65 (31.1) | 72 (42.6) | 11 (25.0) | ||
| Tertiary | 192 (45.5) | 103 (49.3) | 63 (32.3) | 26 (59.1) | ||
| Employment status | Not working | 77 (18.3) | 50 (23.9) | 22 (13.0) | 5 (11.4) | 0.011 |
| Working | 345 (81.7) | 159 (76.1) | 147 (87.0) | 39 (88.6) | ||
| General medical condition | No | 338 (80.1) | 160 (76.5) | 140 (82.8) | 38 (86.4) | 0.025 |
| Diabetes mellitus | 17 (4.0) | 5 (2.4) | 9 (5.3) | 3 (6.8) | ||
| Other | 67 (15.9) | 44 (21.1) | 20 (11.8) | 3 (6.8) | ||
| Parity | Primigravida | 169 (40.0) | 79 (37.8) | 71 (42.0) | 19 (43.2) | 0.387 |
| One | 178(42.2) | 98 (46.9) | 64 (37.8) | 16 (36.4) | ||
| Two or more | 75 (17.8) | 32 (15.3) | 34 (20.1) | 9 (20.4) | ||
| Pregnancy stage | First trimester | 81 (19.2) | 37 (17.7) | 32 (18.9) | 12 (27.3) | 0.419 |
| Second trimester | 132 (31.3) | 64 (30.6) | 52 (30.8) | 16 (36.4) | ||
| Third trimester | 209 (49.5) | 108 (51.7) | 85 (50.3) | 16 (36.4) | ||
| Pregnancy complication | None | 282 (66.8) | 151 (72.2) | 107 (63.3) | 24 (54.5) | 0.142 |
| GDM | 44 (10.4) | 18 (8.6) | 19 (11.2) | 7 (15.9) | ||
| Other | 96 (22.7) | 40 (19.1) | 43 (25.4) | 13 (29.5) | ||
| Pre-pregnancy supplement use (Yes) | Yes | 230 (54.5) | 106 (50.7) | 94 (55.6) | 30 (68.2) | 0.100 |
| Pregnancy supplement use | Do not use | 36 (8.5) | 22 (10.5) | 11 (6.5) | 3 (6.8) | 0.500 |
| Use but do not contain I and F | 41 (9.7) | 23 (11.0) | 15 (8.9) | 3 (6.8) | ||
| Use I and F containing supp | 345 (81.7) | 164 (78.5) | 143 (84.6) | 38 (86.4) | ||
| Pre-pregnancy Alcohol use (Yes) | Yes | 284 (67.3) | 146 (69.8) | 115 (68.0) | 23 (52.3) | 0.075 |
| Pregnancy alcohol use (Yes) | Yes | 28 (6.6) | 9 (4.3) | 14 (8.3) | 5 (11.4) | 0.125 |
| Smoking habit | Never smoker | 387 (91.7) | 194 (92.8) | 154 (84.6) | 39 (88.6) | 0.198 |
| Past smoker | 29 (6.9) | 10 (4.3) | 14 (8.3) | 5 (11.4) | ||
| Current smoker | 6 (1.4) | 5 (2.4) | 1 (0.6) | - | ||
| Moderate physical activity during the current pregnancy | ≤2/week | 324 (77.8) | 165 (78.9) | 131 (77.5) | 28 (63.6) | 0.178 |
| 3–4/week | 77 (18.2) | 37 (17.1) | 28 (16.6) | 12 (27.3) | ||
| ≥5/week | 21 (5.0) | 7 (3.3) | 10 (5.9) | 4 (9.1) | ||
| IRSAD | First quintile (Disadvantaged) | 78 (20.2) | 38 (18.2) | 32 (18.9) | 8 (18.2) | 0.027 |
| Second quintile | 79 (20.5) | 37 (17.7) | 39 (23.1) | 3 (6.8) | ||
| Third quintile | 79 (20.5) | 34 (16.3) | 39 (23.1) | 6 (13.6) | ||
| Fourth quintile | 73 (18.9) | 36 (17.2) | 27 (15.9) | 10 (22.7) | ||
| Fifth quintile (Advantaged) | 77 (19.9) | 38 (18.2) | 23 (13.6) | 16 (36.4) | ||
| Model | LL | df | AIC | BIC | L2 | Entropy R2 |
|---|---|---|---|---|---|---|
| 1 Class | −4459.041 | 23 | 8964.083 | 9057.118 | 4148.479 | - |
| 2 Classes | −4069.316 | 47 | 8232.631 | 8422.746 | 3369.027 | 0.632 |
| 3 Classes | −3970.422 | 71 | 8082.844 | 8370.039 | 3171.240 | 0.716 |
| 4 Classes | −3931.431 | 91 | 8044.862 | 8412.958 | 3093.258 | 0.683 |
| 5 Classes | −3895.562 | 113 | 8017.125 | 8474.210 | 3021.520 | 0.687 |
| Variable | Category | LCS Consumption | |||
|---|---|---|---|---|---|
| Infrequent or Non-Consumer (n = 209) | Moderate Consumer (n = 169) | Habitual Consumer (n = 44) | p-Value | ||
| Are you aware of any adverse effects of LCS? | No | 106 (50.7) | 85 (50.3) | 26 (59.1) | 0.413 |
| Not sure | 49 (23.4) | 30 (17.7) | 7 (15.9) | ||
| Yes | 54 (25.8) | 54 (31.9) | 11 (25.0) | ||
| Are you concerned that LCS may affect your or your baby’s health? | No | 82 (39.2) | 79 (46.7) | 22 (50.0) | 0.314 |
| Not sure | 69 (33.0) | 56 (33.1) | 11 (25.0) | ||
| Yes | 58 (27.8) | 34 (20.1) | 11 (25.0) | ||
| Reason for consumption | Did not consume or no reason | 116 (55.5) | 33 (19.5) | 4 (9.1) | <0.001 |
| Weight loss and/or DM | 38 (18.2) | 62 (36.7) | 18 (40.9) | ||
| Other | 55 (26.3) | 74 (43.8) | 22 (50.0) | ||
| Variables | Category | Moderate Consumption | Habitual Consumption | ||
|---|---|---|---|---|---|
| aRRR a | 95% CI | aRRR a | 95% CI | ||
| Age | - | 0.93 | 0.88–0.98 | 0.92 | 0.84–1.01 |
| Employment status | Not working | Ref | |||
| Working | 3.25 | 1.67–6.33 | 2.71 | 0.85–8.60 | |
| Educational level | Secondary | Ref | |||
| Above secondary but not tertiary | 1.29 | 0.69–2.41 | 0.79 | 0.25–2.50 | |
| Degree and above | 0.77 | 0.41–1.45 | 1.37 | 0.46–4.07 | |
| General medical condition | No | Ref | |||
| Yes-DM | 2.14 | 0.56–8.16 | 3.06 | 0.45–20.54 | |
| Yes, other | 0.45 | 0.23–0.88 | 0.20 | 0.05–0.80 | |
| Pre-pregnancy alcohol use | No | Ref | |||
| Yes | 0.81 | 0.49–1.32 | 0.65 | 0.29–1.45 | |
| BMI | - | 0.99 | 0.95–1.02 | 0.89 | 0.83–0.97 |
| Diet quality | - | 0.98 | 0.97–0.99 | 0.98 | 0.95–1.00 |
| SSB consumption | ≤once/week | Ref | |||
| ≥2 times/week | 1.34 | 0.82–2.19 | 3.17 | 1.39–7.21 | |
| Moderate physical activity during current pregnancy | No or <2/week | Ref | |||
| 3–4/week | 1.04 | 0.57–1.91 | 1.98 | 0.79–4.92 | |
| ≥5/week | 1.74 | 0.58–5.18 | 3.92 | 0.93–16.51 | |
| Pregnancy supplement use | Not at all | Ref | |||
| Use, don’t contain I and F | 2.29 | 0.76–6.85 | 4.07 | 0.54–30.29 | |
| Use, contain I and F | 2.71 | 1.13–6.47 | 3.77 | 0.80–17.74 | |
| Parity | Primigravida | Ref | |||
| One | 0.90 | 0.54–1.49 | 0.89 | 0.37–2.13 | |
| Two or more | 1.93 | 0.96–3.89 | 3.06 | 0.94–9.93 | |
| Pregnancy duration | First trimester | Ref | |||
| Second trimester | 0.96 | 0.49–1.87 | 0.85 | 0.30–2.38 | |
| Third trimester | 0.80 | 0.43–1.49 | 0.38 | 0.14–1.04 | |
| Pregnancy complication | None | Ref | |||
| Other | 1.73 | 0.98–3.06 | 3.11 | 1.26–7.67 | |
| GDM | 1.27 | 0.55–2.95 | 3.53 | 1.03–12.10 | |
| LCS safety concern about the baby | No | Ref | |||
| Not sure | 0.85 | 0.50–1.44 | 0.56 | 0.22–1.43 | |
| Yes | 0.61 | 0.34–1.10 | 0.57 | 0.22–1.51 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gebremichael, B.; Lassi, Z.S.; Begum, M.; Mittinty, M.; Zhou, S.-J. Patterns and Predictors of Low-Calorie Sweetener Consumption during Pregnancy: Findings from a National Survey. Nutrients 2023, 15, 4196. https://doi.org/10.3390/nu15194196
Gebremichael B, Lassi ZS, Begum M, Mittinty M, Zhou S-J. Patterns and Predictors of Low-Calorie Sweetener Consumption during Pregnancy: Findings from a National Survey. Nutrients. 2023; 15(19):4196. https://doi.org/10.3390/nu15194196
Chicago/Turabian StyleGebremichael, Bereket, Zohra S. Lassi, Mumtaz Begum, Murthy Mittinty, and Shao-Jia Zhou. 2023. "Patterns and Predictors of Low-Calorie Sweetener Consumption during Pregnancy: Findings from a National Survey" Nutrients 15, no. 19: 4196. https://doi.org/10.3390/nu15194196
APA StyleGebremichael, B., Lassi, Z. S., Begum, M., Mittinty, M., & Zhou, S.-J. (2023). Patterns and Predictors of Low-Calorie Sweetener Consumption during Pregnancy: Findings from a National Survey. Nutrients, 15(19), 4196. https://doi.org/10.3390/nu15194196







