A Narrative Review of Human Clinical Trials to Improve Lactose Digestion and Tolerance by Feeding Bifidobacteria or Galacto-Oligosacharides
Abstract
1. Introduction
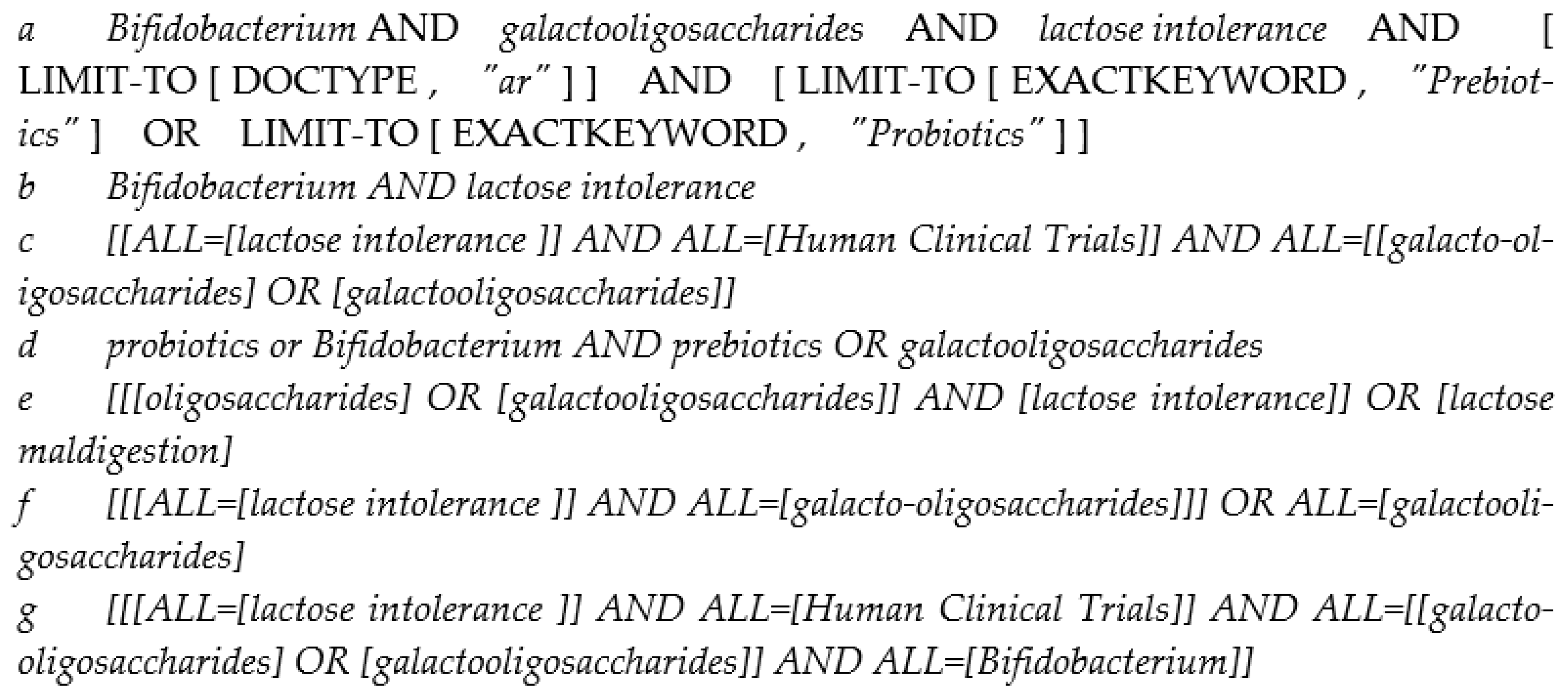
2. Materials and Methods
3. Results
3.1. Bifidobacterium as a Digestive Aid for People with Lactose Intolerance
3.2. Galacto-Oligosaccharides as a Digestive Aid for People with Lactose Intolerance
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Markowiak, P.; Śliżewska, K. Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients 2017, 9, 1021. [Google Scholar] [CrossRef] [PubMed]
- Garrido, D.; Ruiz-Moyano, S.; Jimenez-Espinoza, R.; Eom, H.-J.; Block, D.E.; Mills, D.A. Utilization of Galactooligosaccharides by Bifidobacterium longum subsp. infantis Isolates. Food Microbiol. 2013, 33, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Blekhman, R.; Goodrich, J.K.; Huang, K.; Sun, Q.; Bukowski, R.; Bell, J.T.; Spector, T.D.; Keinan, A.; Ley, R.E.; Gevers, D.; et al. Host Genetic Variation Impacts Microbiome Composition across Human Body Sites. Genome Biol. 2015, 16, 191. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Priebe, M.G.; Zhong, Y.; Huang, C.; Harmsen, H.J.M.; Raangs, G.C.; Antoine, J.-M.; Welling, G.W.; Vonk, R.J. Effects of Yogurt and Bifidobacteria Supplementation on the Colonic Microbiota in Lactose-Intolerant Subjects. J. Appl. Microbiol. 2008, 104, 595–604. [Google Scholar] [CrossRef] [PubMed]
- Rana, S.V.; Malik, A. Hydrogen Breath Tests in Gastrointestinal Diseases. Indian J. Clin. Biochem. 2014, 29, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Gasbarrini, A.; Corazza, G.R.; Gasbarrini, G.; Montalto, M.; Di Stefano, M.; Basilisco, G.; Parodi, A.; Usai-Satta, P.; Vernia, P.; Anania, C.; et al. Methodology and Indications of H2-Breath Testing in Gastrointestinal Diseases: The Rome Consensus Conference. Aliment. Pharmacol. Ther. 2009, 29 (Suppl. S1), 1–49. [Google Scholar]
- Firrman, J.; Liu, L.; Mahalak, K.; Hu, W.; Bittinger, K.; Moustafa, A.; Jones, S.M.; Narrowe, A.; Tomasula, P. An in Vitro Analysis of How Lactose Modifies the Gut Microbiota Structure and Function of Adults in a Donor-Independent Manner. Front. Nutr. 2023, 9, 1040744. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Aguilera, G.; Cárcamo, C.; Soto-Alarcón, S.; Gotteland, M. Improvement in Lactose Tolerance in Hypolactasic Subjects Consuming Ice Creams with High or Low Concentrations of Bifidobacterium bifidum 900791. Foods 2021, 10, 2468. [Google Scholar] [CrossRef]
- Masoumi, S.J.; Mehrabani, D.; Saberifiroozi, M.; Fattahi, M.R.; Moradi, F.; Najafi, M. The Effect of Yogurt Fortified with Lactobacillus acidophilus and Bifidobacterium sp. Probiotic in Patients with Lactose Intolerance. Food Sci. Nutr. 2021, 9, 1704–1711. [Google Scholar] [CrossRef]
- Almeida, C.C.; Lorena, S.L.S.; Pavan, C.R.; Akasaka, H.M.I.; Mesquita, M.A. Beneficial Effects of Long-Term Consumption of a Probiotic Combination of Lactobacillus casei Shirota and Bifidobacterium breve Yakult May Persist After Suspension of Therapy in Lactose-Intolerant Patients. Nutr. Clin. Pract. 2012, 27, 247–251. [Google Scholar] [CrossRef]
- Vitellio, P.; Celano, G.; Bonfrate, L.; Gobbetti, M.; Portincasa, P.; De Angelis, M. Effects of Bifidobacterium longum and Lactobacillus rhamnosus on Gut Microbiota in Patients with Lactose Intolerance and Persisting Functional Gastrointestinal Symptoms: A Randomised, Double-Blind, Cross-Over Study. Nutrients 2019, 11, 886. [Google Scholar] [CrossRef] [PubMed]
- Roškar, I.; Švigelj, K.; Štempelj, M.; Volfand, J.; Štabuc, B.; Malovrh, Š.; Rogelj, I. Effects of a Probiotic Product Containing Bifidobacterium animalis subsp. animalis IM386 and Lactobacillus plantarum MP2026 in Lactose Intolerant Individuals: Randomized, Placebo-Controlled Clinical Trial. J. Funct. Foods 2017, 35, 1–8. [Google Scholar] [CrossRef]
- Rasinkangas, P.; Forssten, S.D.; Marttinen, M.; Ibarra, A.; Bothe, G.; Junnila, J.; Uebelhack, R.; Donazzolo, Y.; Ouwehand, A.C. Bifidobacterium animalis subsp. lactis Bi-07 Supports Lactose Digestion In Vitro and in Randomized, Placebo- and Lactase-Controlled Clinical Trials. Am. J. Clin. Nutr. 2022, 116, 1580–1594. [Google Scholar] [CrossRef] [PubMed]
- Tianan, J.; Mustapha, A.; Savaiano, D.A. Improvement of Lactose Digestion in Humans by Ingestion of Unfermented Milk Containing Bifidobacterium longum. J. Dairy Sci. 1996, 79, 750–757. [Google Scholar]
- Savaiano, D.A.; Ritter, A.J.; Klaenhammer, T.R.; James, G.M.; Longcore, A.T.; Chandler, J.R.; Walker, W.A.; Foyt, H.L. Improving Lactose Digestion and Symptoms of Lactose Intolerance with a Novel Galacto-Oligosaccharide (RP-G28): A Randomized, Double-Blind Clinical Trial. Nutr. J. 2013, 12, 160. [Google Scholar] [CrossRef] [PubMed]
- Azcarate-Peril, M.A.; Roach, J.; Marsh, A.; Chey, W.D.; Sandborn, W.J.; Ritter, A.J.; Savaiano, D.A.; Klaenhammer, T.R. A Double-Blind, 377-Subject Randomized Study Identifies Ruminococcus, Coprococcus, Christensenella, and Collinsella as Long-Term Potential Key Players in the Modulation of the Gut Microbiome of Lactose Intolerant Individuals by Galacto-Oligosaccharides. Gut Microbes 2021, 13, 1957536. [Google Scholar] [CrossRef]
- Chey, W.; Sandborn, W.; Ritter, A.J.; Foyt, H.; Azcarate-Peril, M.A.; Savaiano, D.A. Galacto-Oligosaccharide RP-G28 Improves Multiple Clinical Outcomes in Lactose-Intolerant Patients. Nutrients 2020, 12, 1058. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.-Y.; Yen, C.-L.; Chen, S.-H. Management of Lactose Maldigestion by Consuming Milk Containing Lactobacilli. Dig. Dis. Sci. 1998, 43, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Gilliland, S.E. Lactobacillus acidophilus as a Dietary Adjunct for Milk to Aid Lactose Digestion in Humans. J. Dairy Sci. 1983, 66, 959–966. [Google Scholar] [CrossRef]
- Davis, L.M.; Martínez, I.; Walter, J.; Goin, C.; Hutkins, R.W. Barcoded pyrosequencing reveals that consumption of galactooligosaccharides results in a highly specific bifidogenic response in humans. PLoS ONE 2011, 6, e25200. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, T.; Kimura, K.; Hatano, H. Diverse galactooligosaccharides consumption by bifidobacteria: Implications of β-galactosidase—LacS operon. Biosci. Biotechnol. Biochem. 2015, 79, 664–672. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Inclusion Criterion | Exclusion Criteria |
|---|---|---|
| Participants | No age limit | Gastrointestinal disorder other than LI, antibiotic treatments |
| Intervention | Bifidobacterium or galacto-oligosaccharides | - |
| Outcomes | Reduced hydrogen breath test [HBT] results, decreased abdominal discomfort scores, reduced fecal urgency, and improved lactose tolerance | - |
| Study design | Human clinical trials, randomized controlled trials (RCT’s) | In vivo and in vitro experiments |
| Variable Studied | Total Number of Studies | Outcomes Studied | Number of Studies with Favorable Outcomes | Number of Studies with No Significant Outcomes | Number of Studies with No Favorable Outcomes |
|---|---|---|---|---|---|
| Lactose intolerance and Bifidobacterium | 74 | 8 | 5 | 3 | 0 |
| Lactose intolerance and Galacto-oligosaccharide | 48 | 3 | 3 | 0 | 0 |
| S. No. | Ref No. | Subjects | Intervention | Days of Intervention | Symptoms Evaluated | Hydrogen Breath Test (HBT) | Fecal Analysis | |||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Control/Placebo | Lactose Maldigesters | Control/Placebo | Experimental Group | ||||||
| 1 | [4] | 11 | 0 | 11 | None | B. longum and B. animalis | 2 weeks | All symptoms of LI | Conducted during each visit | Analyzed for fecal microbiota and β-galactosidase activity |
| 2 | [9] | 45 | Acute phase = 45 Chronic phase = 16 | Acute phase = 45 Chronic phase = 13 | No Bifidobacterium (negative control)/lactase (positive control) | B. bifidum 900,791 | Acute phase: same-day analysis Chronic phase: 4 weeks of placebo/Bifidobacterium | Nausea, vomiting, abdominal pain, abdominal distension, increased rectal gas, borborygmi, and diarrhea | Conducted during each visit | None |
| 3 | [10] | 55 | 28 | 27 | L. bulgaricus and S. thermophiles | L. acidophilus and Bifidobacterium sp. | 1 week | Diarrhea, abdominal pain, flatulence, vomiting and nausea, bloating, and flatulence | Conducted during each visit | None |
| 4 | [11] | 27 | 27 | 27 | Lactase ingestion | L. casei and B. breve | 4 weeks | Abdominal pain, flatulence, stool consistency, and abdominal distention | Conducted during each visit | None |
| 5 | [12] | 23 | 23 | 23 | Placebo with maltodextrins | B. longum BB536 + L. rhamnosus HN001 + vitamin B6 (ZR) | 30 days | Bloating, abdominal pain, and bowel movements | For screening | Analyzed to identify the bacterial microbiome |
| 6 | [13] | 44 | 22 | 22 | Placebo | B. animalis IM386 and L. plantarum MP2026 | 6 weeks | Diarrhea, abdominal pain, vomiting, and flatulence or rumble | Conducted during each visit | None |
| 7 | [14] | 34 (BoosterAlpha) + 33 (Booster Omega) | 34 (Booster Alpha) + 33 (Booster Omega) | 34 (Booster Alpha) + 33 (Booster Omega) | Booster alpha: (placebo) milk Booster Omega: (control) lactose + water | B. animalis subsp. lactis Bi-07 | Booster alpha—101 days Booster omega—195 days | Bowel movements, vomiting, and stool consistency | Conducted during each visit | For quantification of Bifidobacterium in feces |
| 8 | [15] | 15 | 15 | 15 | Low-fat milk with no probiotic | B. longum B6 grown on lactose/B. longum B6 grown on lactose + glucose/B. longum ATCC 15,708 grown on lactose medium | 15 days | Abdominal pain, diarrhea, flatulence, bloating, and abdominal rumbling | Conducted during each visit | None |
| 14 | [16] | 61 | 19 | 42 | Placebo (corn syrup) | RP-G28 | 35 days | Abdominal pain, diarrhea, flatulence, bloating and cramping, symptoms reduced post-RP-G28 intervention | Conducted during each visit | None |
| 15 | [17] | 368 | 121 | Lower dose of RP-G28 = 126 Higher dose of RP-G28 = 121 | Placebo (powdered corn syrup) | Low GOS (10–15 g/day) and high GOS treatments (15–20 g/day) | 30 days | Analyzed for screening | Conducted for screening | Collected to analyze the fecal microbiota |
| 16 | [18] | 368 | 121 | Lower dose of RP-G28 = 126 Higher dose of RP-G28 = 121 | Placebo (powdered corn syrup) | Low GOS (10–15 g/day) and high GOS treatments (15–20 g/day) | 30 days | Abdominal pain, cramping, bloating, and gas movement | Conducted during each visit | Collected to analyze the fecal microbiota |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mysore Saiprasad, S.; Moreno, O.G.; Savaiano, D.A. A Narrative Review of Human Clinical Trials to Improve Lactose Digestion and Tolerance by Feeding Bifidobacteria or Galacto-Oligosacharides. Nutrients 2023, 15, 3559. https://doi.org/10.3390/nu15163559
Mysore Saiprasad S, Moreno OG, Savaiano DA. A Narrative Review of Human Clinical Trials to Improve Lactose Digestion and Tolerance by Feeding Bifidobacteria or Galacto-Oligosacharides. Nutrients. 2023; 15(16):3559. https://doi.org/10.3390/nu15163559
Chicago/Turabian StyleMysore Saiprasad, Sindusha, Olivia Grace Moreno, and Dennis A. Savaiano. 2023. "A Narrative Review of Human Clinical Trials to Improve Lactose Digestion and Tolerance by Feeding Bifidobacteria or Galacto-Oligosacharides" Nutrients 15, no. 16: 3559. https://doi.org/10.3390/nu15163559
APA StyleMysore Saiprasad, S., Moreno, O. G., & Savaiano, D. A. (2023). A Narrative Review of Human Clinical Trials to Improve Lactose Digestion and Tolerance by Feeding Bifidobacteria or Galacto-Oligosacharides. Nutrients, 15(16), 3559. https://doi.org/10.3390/nu15163559







