Associations of Hormonal and Metabolic Parameters with Bone Mineralization in Young Adult Females
Abstract
1. Introduction
2. Materials and Methods
2.1. Participation in the Study
2.2. Basic Procedures
- A standard subject and physical examination was performed on all patients. Body mass index (BMI (kg/m2)) was calculated using anthropometric measurements (height (cm) and weight (kg)).
- Hormonal parameters were determined from fasting venous blood collected from the basilic vein in the morning between the 2nd and the 6th day of the follicular phase of the menstrual cycle: concentrations of androstendione, dihydroepiandrosterone sulphate (DHEA-S), testosterone (T), sex hormone binding protein (SHBG), 17-OH-progesterone, folliculotropic hormone (FSH), estradiol (E), thyrotropic hormone (TSH), free thyroxine (fT4) and cortisol. Based on the results, the free androgen index (FAI), free testosterone (FT) and bioavailable testosterone (BT) concentrations were calculated.
- 3.
- The metabolic activity of osteocytes was assessed by measuring the subjects’ serum sclerostin concentration. Sclerostin was measured by an enzyme-linked immunosorbent assay (Soluble Sclerostin (SOST) (Human) ELISA Kit, AVISCERA BIOSCIENCE, INC, Santa Clara, CA, USA; catalog number SK00385-01)). The assay’s properties: sensitivity (detection limit) ± 20 pg/mL, a broad detection range (125~4000 pg/mL), an intra-assay precision (Intra-CV) of 4–8% and an inter-assay precision (Inter-CV) of 6–10%.
- 4.
- All participants had their bone mineral density determined at lumbar spine (L1–L4) and for whole body by the dual-energy X-ray absorptiometry (DXA) technique (GE Lunar Prodigy Advance-Madison, WI, USA—z enCORE software version 8.8). Results were presented as BMD (g/cm2) and Z-score. According to the criteria, Z-score values >(−1.0) were stated as normal.
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Group
3.2. Hormone and Metabolic Parameters
3.3. Sclerostin
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martin, A.; Yu, J.; Xiong, J.; Khalid, A.B.; Katzenellenbogen, B.; Kim, S.H.; Katzenellenbogen, J.A.; Malaivijitnond, S.; Gabet, Y.; Krum, S.A.; et al. Estrogens and androgens inhibit association of RANKL with the pre-osteoblast membrane through post-translational mechanisms. J. Cell. Physiol. 2017, 232, 3798–3807. [Google Scholar] [CrossRef] [PubMed]
- Vanderschueren, D.; Gaytant, J.; Boonen, S.; Venken, K. Androgens and bone. Curr. Opin. Endocrinol. Diabetes 2008, 15, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Almeida, M.; Laurent, M.R.; Dubois, V.; Claessens, F.; O’Brien, C.A.; Bouillon, R.; Vanderschueren, D.; Manolagas, S.C. Estrogens and Androgens in Skeletal Physiology and Pathophysiology. Physiol. Rev. 2017, 97, 135–187. [Google Scholar] [CrossRef] [PubMed]
- Riggs, B.L.; Khosla, S.; Melton, L.J. Sex Steroids and the Construction and Conservation of the Adult Skeleton. Endocr. Rev. 2002, 23, 279–302. [Google Scholar] [CrossRef] [PubMed]
- Huitrón-Bravo, G.; Denova-Gutiérrez, E.; Talavera, J.O.; Moran-Villota, C.; Tamayo, J.; Omaña-Covarrubias, A.; Salmerón, J. Levels of serum estradiol and lifestyle factors related with bone mineral density in premenopausal Mexican women: A cross-sectional analysis. BMC Musculoskelet. Disord. 2016, 17, 437. [Google Scholar] [CrossRef]
- Wu, S.-M.; Shih, L.-H.; Lee, J.-Y.; Shen, Y.-J.; Lee, H.-H. Estrogen Enhances Activity of Wnt Signaling During Osteogenesis by Inducing Fhl1 Expression. J. Cell. Biochem. 2015, 116, 1419–1430. [Google Scholar] [CrossRef]
- Botella, S.; Restituto, P.; Monreal, I.; Colina, I.; Calleja, A.; Varo, N. Traditional and Novel Bone Remodeling Markers in Premenopausal and Postmenopausal Women. J. Clin. Endocrinol. Metab. 2013, 98, E1740–E1748. [Google Scholar] [CrossRef]
- Khosla, S.; Oursler, M.J.; Monroe, D.G. Estrogen and the skeleton. Trends Endocrinol. Metab. 2012, 23, 576–581. [Google Scholar] [CrossRef]
- Walsh, J.S.; Henry, Y.M.; Fatayerji, D.; Eastell, R. Hormonal determinants of bone turnover before and after attainment of peak bone mass. Clin. Endocrinol. 2010, 72, 320–327. [Google Scholar] [CrossRef]
- Mohamad, N.V.; Soelaiman, I.-N.; Chin, K.-Y. A concise review of testosterone and bone health. Clin. Interv. Aging 2016, 11, 1317–1324. [Google Scholar] [CrossRef]
- Locatelli, V.; Bianchi, V.E. Effect of GH/IGF-1 on Bone Metabolism and Osteoporsosis. Int. J. Endocrinol. 2014, 2014, 235060. [Google Scholar] [CrossRef] [PubMed]
- Callewaert, F.; Sinnesael, M.; Gielen, E.; Boonen, S.; Vanderschueren, D. Skeletal sexual dimorphism: Relative contribution of sex steroids, GH–IGF1, and mechanical loading. J. Endocrinol. 2010, 207, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Conte, C.; Epstein, S.; Napoli, N. Insulin resistance and bone: A biological partnership. Acta Diabetol. 2018, 55, 305–314. [Google Scholar] [CrossRef]
- EMA. Evenity EPAR—EMA/571266/2019 EMEA/H/C/004465. 2020. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/roactemra (accessed on 18 February 2009).
- Hardy, R.; Zhou, H.; Seibel, M.J.; Cooper, M.S. Glucocorticoids and Bone: Consequences of Endogenous and Exogenous Excess and Replacement Therapy. Endocr. Rev. 2018, 39, 519–548. [Google Scholar] [CrossRef]
- Hardy, R.; Cooper, M.S. Adrenal gland and bone. Arch. Biochem. Biophys. 2010, 503, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Bedford, J.L.; Barr, S.I. The Relationship Between 24-h Urinary Cortisol and Bone in Healthy Young Women. Int. J. Behav. Med. 2010, 17, 207–215. [Google Scholar] [CrossRef]
- Ardawi, M.-S.M.; Al-Kadi, H.A.; Rouzi, A.A.; Qari, M.H. Determinants of serum sclerostin in healthy pre- and postmenopausal women. J. Bone Miner. Res. 2011, 26, 2812–2822. [Google Scholar] [CrossRef]
- Slemenda, C.; Longcope, C.; Peacock, M.; Hui, S.; Johnston, C.C. Sex steroids, bone mass, and bone loss: A prospective study of pre-, peri-, and postmenopausal women. J. Clin. Invest. 1996, 97, 14–21. [Google Scholar] [CrossRef]
- Wang, T.; He, C. Pro-inflammatory cytokines: The link between obesity and osteoarthritis. Acta Diabetol. 2018. [Google Scholar] [CrossRef]
- He, Z.; Rankinen, T.; Leon, A.S.; Skinner, J.S.; Tchernof, A.; Bouchard, C. Plasma steroids, body composition, and fat distribution: Effects of age, sex, and exercise training. Int. J. Obes. 2018, 42, 1366–1377. [Google Scholar] [CrossRef]
- Ragnarsson, O.; Trimpou, P.; Oleröd, G.; Landin-Wilhelmsen, K. Urinary free cortisol and androgens in the population—Hormone interactions and the relationship with body composition and bone status. Steroids 2016, 115, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Khosla, S.; Melton, L.J.; Atkinson, E.J.; O’Fallon, W.M.; Klee, G.G.; Riggs, B.L. Relationship of Serum Sex Steroid Levels and Bone Turnover Markers with Bone Mineral Density in Men and Women: A Key Role for Bioavailable Estrogen. J. Clin. Endocrinol. Metab. 1998, 83, 2266–2274. [Google Scholar]



| Variable | n | Average | Median | Q1 | Q4 | SD * |
|---|---|---|---|---|---|---|
| Age [years] | 111 | 23.80 | 24.00 | 23.00 | 25.00 | 1.793 |
| Body weight [kg] | 111 | 63.48 | 61.00 | 56.00 | 68.00 | 11.854 |
| Height [cm] | 111 | 168.21 | 168.00 | 164.00 | 173.00 | 5.967 |
| BMI [kg/m2] | 111 | 22.39 | 21.00 | 19.50 | 23.50 | 4.223 |
| BMD Total [g/cm2] | 111 | 1.14 | 1.13 | 1.06 | 1.21 | 0.096 |
| BMD L1–L4 [g/cm2] | 111 | 1.20 | 1.19 | 1.11 | 1.29 | 0.122 |
| BMD L1–L4 z-score | 111 | 0.22 | 0.10 | −0.50 | 0.80 | 1.001 |
| BMC [g] | 111 | 2390.55 | 2407.00 | 2220.00 | 2624.00 | 351.032 |
| MS-R [kg] | 111 | 27.96 | 28.30 | 24.70 | 31.30 | 4.395 |
| MS-L [kg] | 111 | 26.38 | 26.30 | 23.10 | 30.40 | 4.781 |
| FLR | 111 | 0.50 | 0.45 | 0.38 | 0.58 | 0.180 |
| A/G | 111 | 0.79 | 0.79 | 0.63 | 0.93 | 0.202 |
| VF [g] | 111 | 273.44 | 161.00 | 60.00 | 309.00 | 355.636 |
| Glucose [mg/dL] | 109 | 88.44 | 89.00 | 83.00 | 93.30 | 7.616 |
| Insulin [µIU/mL] | 106 | 10.43 | 9.36 | 7.10 | 12.90 | 5.267 |
| HOMA2 IR | 106 | 1.34 | 1.20 | 0.91 | 1.64 | 0.666 |
| Estradiol [pg/mL] | 111 | 38.55 | 33.21 | 22.10 | 50.60 | 27.827 |
| Testosterone [ng/mL] | 111 | 0.37 | 0.35 | 0.25 | 0.47 | 0.174 |
| FT [ng/mL] | 105 | 0.00 | 0.00 | 0.00 | 0.01 | 0.005 |
| BAT [ng/mL] | 105 | 0.12 | 0.08 | 0.05 | 0.14 | 0.140 |
| FAI | 105 | 2.08 | 1.40 | 0.76 | 2.56 | 2.415 |
| Cortisol [ng/mL] | 111 | 17.99 | 17.60 | 12.00 | 22.70 | 7.572 |
| TSH [μIU/mL] | 111 | 2.11 | 1.76 | 1.19 | 2.80 | 1.411 |
| Sclerostin [pg/mL] | 111 | 2136.37 | 125.00 | 125.00 | 263.00 | 4989.928 |
| Variable | Group A | Group B | Value p | ||||
|---|---|---|---|---|---|---|---|
| n | Mean | Q1–Q4 | n | Mean | Q1–Q4 | ||
| (SD/Median) | (SD/Median) | ||||||
| FM [kg] | 95 | 20.20 | 14.34–22.93 | 16 | 23.89 | 15.53–32.19 | >0.1 |
| (8.76/18.17) | (11.89/17.93) | ||||||
| LBM [kg] | 95 | 41.03 | 38.04–43.61 | 16 | 40.58 | 36.09–45.78 | >0.1 |
| (4.40/41.29) | (4.78/39.43) | ||||||
| Glucose [mg/dl] | 93 | 88.26 | 83.50–93.20 | 16 | 89.48 | 82.30–94.90 | >0.1 |
| (7.68/89.00) | (7.37/89.10) | ||||||
| Insulin [µIU/mL] | 90 | 10.10 | 6.80–12.60 | 16 | 12.30 | 8.26–14.10 | >0.1 |
| (4.87/9.15) | (7.03/12.15) | ||||||
| HOMA2 IR | 90 | 1.30 | 0.88–1.59 | 16 | 1.59 | 1.06–1.85 | >0.1 |
| (0.62/1.18) | (0.87/1.56) | ||||||
| Estradiol [pg/mL] | 95 | 40.91 | 23.20–53.40 | 16 | 24.54 | 13.66–33.21 | 0.0189 |
| (29.00/35.30) | (12.75/25.80) | ||||||
| Testosterone [ng/mL] | 95 | 0.38 | 0.25–0.48 | 16 | 0.37 | 0.25–0.47 | >0.1 |
| (0.18/0.36) | (0.18/0.34) | ||||||
| FT [ng/mL] | 90 | 0.00 | 0.00–0.01 | 15 | 0.00 | 0.00–0.01 | >0.1 |
| (0.18/0.36) | (0.01/0.00) | ||||||
| BAT [ng/mL] | 90 | 0.12 | 0.05–0.14 | 15 | 0.11 | 0.02–0.22 | >0.1 |
| (0.14/0.08) | (0.13/0.05) | ||||||
| FAI | 90 | 1.95 | 0.81–2.56 | 15 | 2.87 | 0.37–5.23 | >0.1 |
| (1.83/1.42) | (4.61/0.79) | ||||||
| Sclerostin [pg/mL] | 95 | 1950.59 | 125.00–244.00 | 16 | 3239.45 | 125.00–1228.12 | >0.1 |
| (4740.95/125.0) | (6342.35/125.00) | ||||||
| Cortisol [ng/mL] | 95 | 17.24 | 11.70–21.63 | 16 | 22.49 | 18.65–25.17 | 0.0070 |
| (7.42/16.00) | (7.12/22.89) | ||||||
| Variable | n | R | p |
|---|---|---|---|
| FLR | 111 | 0.2042 | 0.0315 |
| VF [g] | 111 | 0.1586 | 0.0963 |
| Glucose [mg/dL] | 109 | 0.1120 | 0.2460 |
| Insulin [µIU/mL] | 106 | −0.0497 | 0.6122 |
| HOMA2 IR | 106 | −0.0422 | 0.6668 |
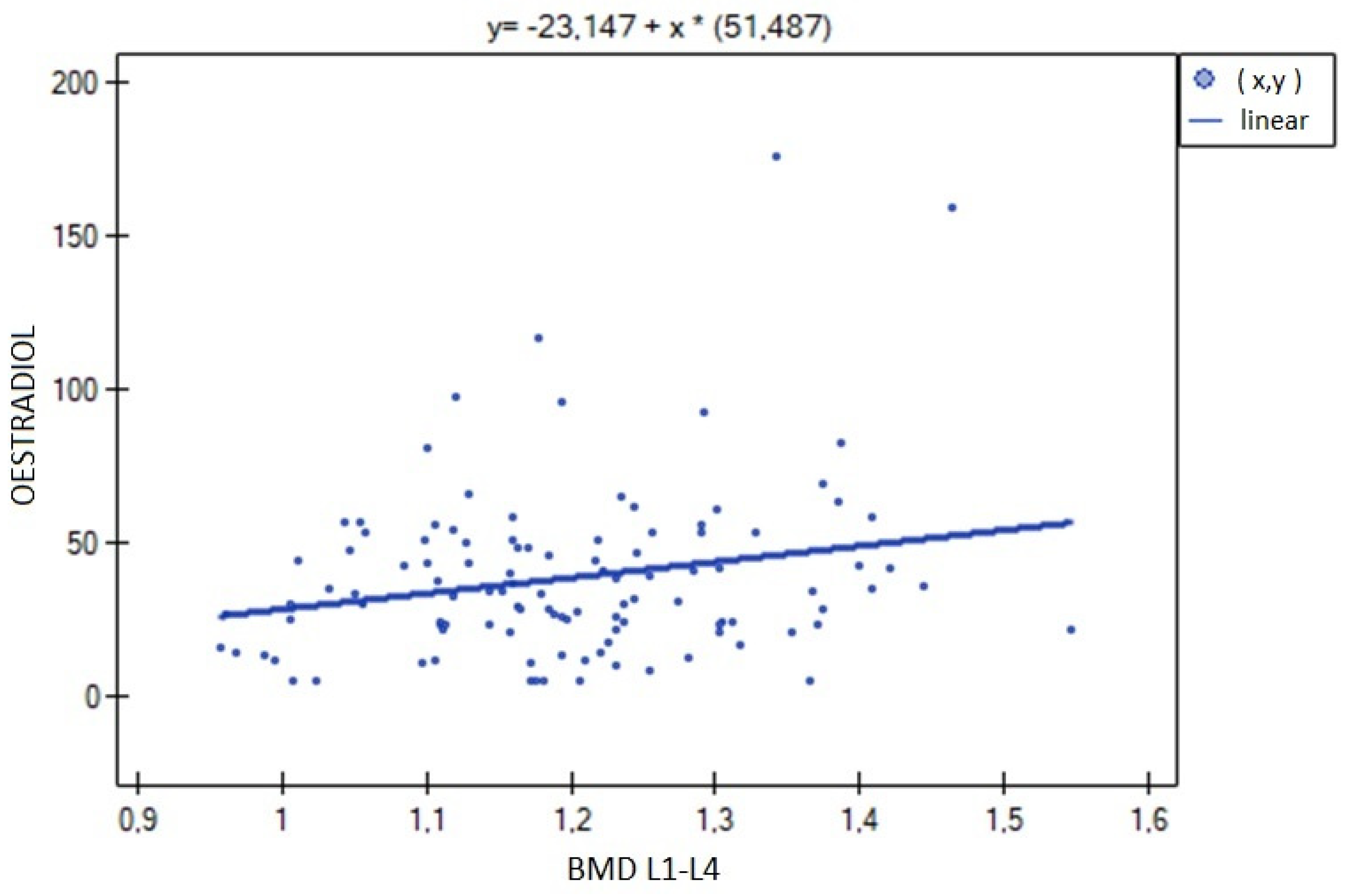
| Estradiol [pg/mL] | 111 | 0.1239 | 0.1949 |
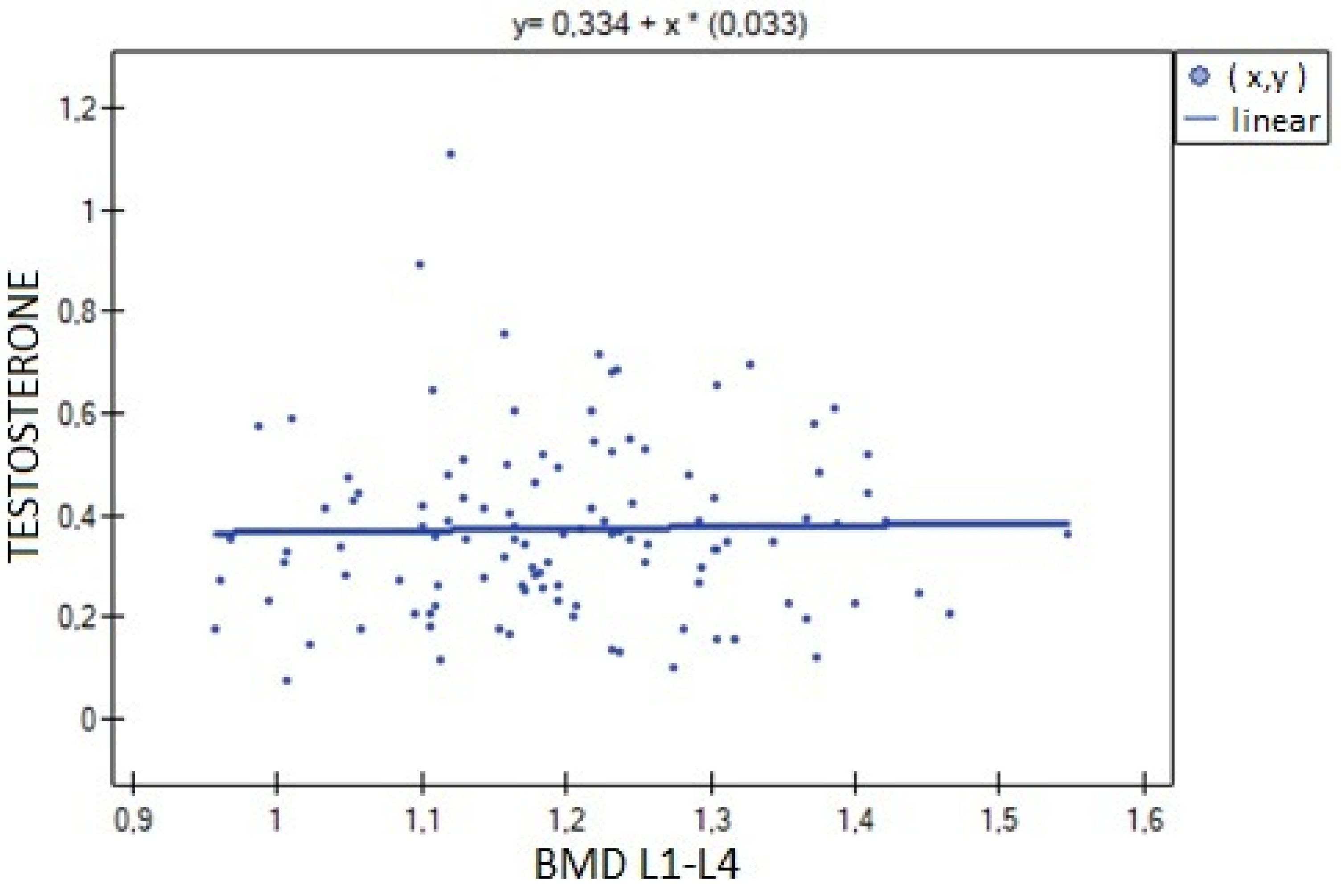
| Testosterone [ng/mL] | 111 | 0.0600 | 0.5312 |
| FT [ng/mL] | 105 | 0.2294 | 0.0185 |
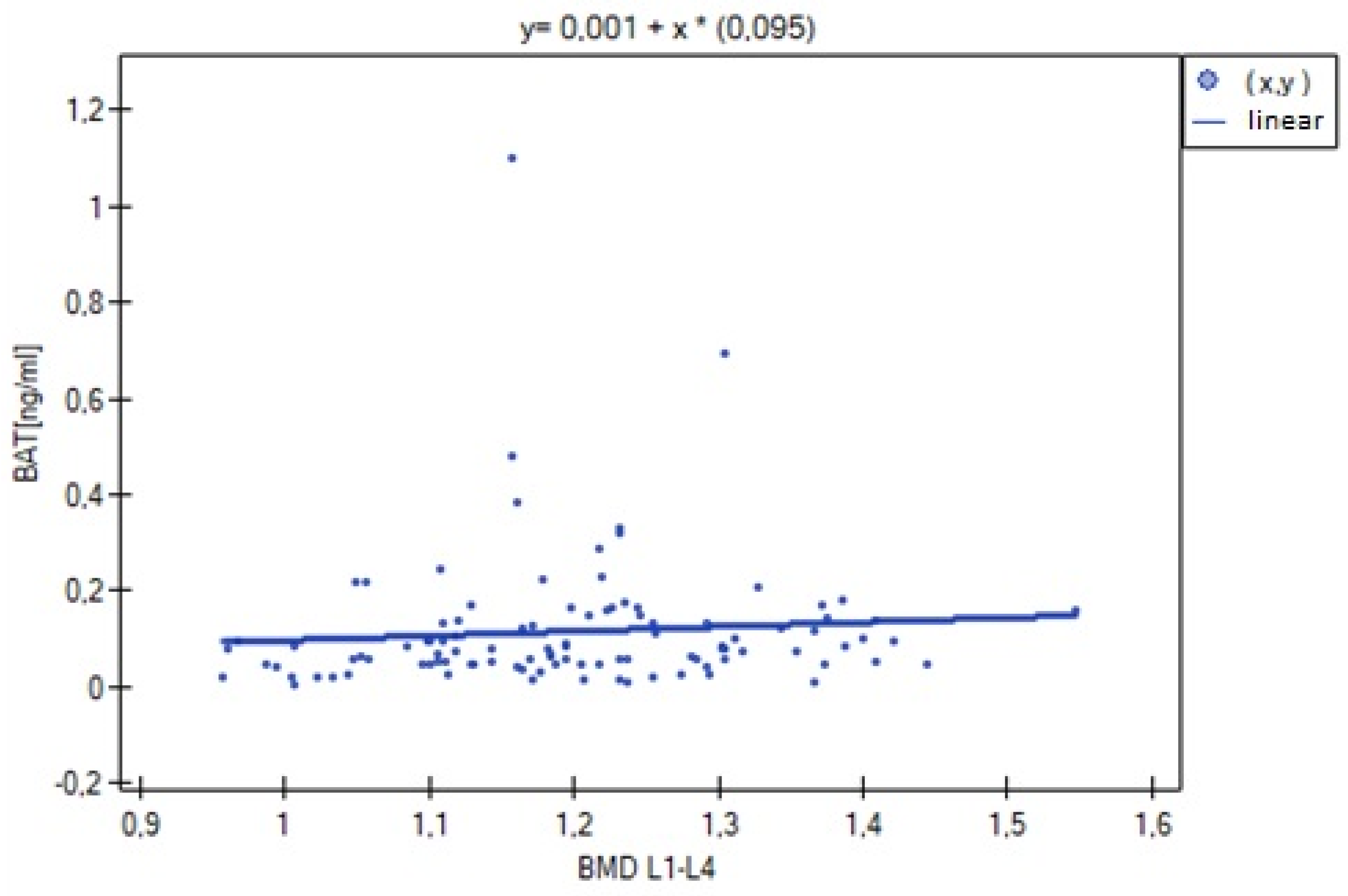
| BAT [ng/mL] | 105 | 0.2002 | 0.0405 |
| FAI | 105 | 0.2157 | 0.0270 |
| Cortisol [ng/mL] | 111 | −0.2633 | 0.0052 |
| Sclerostin [pg/mL] | 111 | 0.0204 | 0.8314 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patalong-Wójcik, M.; Golara, A.; Sokołowska, A.; Zając, K.; Kozłowski, M.; Krzyścin, M.; Brodowska, A.; Syrenicz, I.; Cymbaluk-Płoska, A.; Sowińska-Przepiera, E. Associations of Hormonal and Metabolic Parameters with Bone Mineralization in Young Adult Females. Nutrients 2023, 15, 2482. https://doi.org/10.3390/nu15112482
Patalong-Wójcik M, Golara A, Sokołowska A, Zając K, Kozłowski M, Krzyścin M, Brodowska A, Syrenicz I, Cymbaluk-Płoska A, Sowińska-Przepiera E. Associations of Hormonal and Metabolic Parameters with Bone Mineralization in Young Adult Females. Nutrients. 2023; 15(11):2482. https://doi.org/10.3390/nu15112482
Chicago/Turabian StylePatalong-Wójcik, Martyna, Anna Golara, Alicja Sokołowska, Katarzyna Zając, Mateusz Kozłowski, Mariola Krzyścin, Agnieszka Brodowska, Igor Syrenicz, Aneta Cymbaluk-Płoska, and Elżbieta Sowińska-Przepiera. 2023. "Associations of Hormonal and Metabolic Parameters with Bone Mineralization in Young Adult Females" Nutrients 15, no. 11: 2482. https://doi.org/10.3390/nu15112482
APA StylePatalong-Wójcik, M., Golara, A., Sokołowska, A., Zając, K., Kozłowski, M., Krzyścin, M., Brodowska, A., Syrenicz, I., Cymbaluk-Płoska, A., & Sowińska-Przepiera, E. (2023). Associations of Hormonal and Metabolic Parameters with Bone Mineralization in Young Adult Females. Nutrients, 15(11), 2482. https://doi.org/10.3390/nu15112482








