Mediterranean Diet Adherence and Its Relationship to Metabolic Markers and Body Composition in Portuguese University Students
Highlights
- Mediterranean Diet and Cholesterol Levels: Students with higher adherence to the Mediterranean diet (MedDiet) exhibited significantly improved lipid profiles, higher HDL cholesterol, and better total/HDL cholesterol ratios.
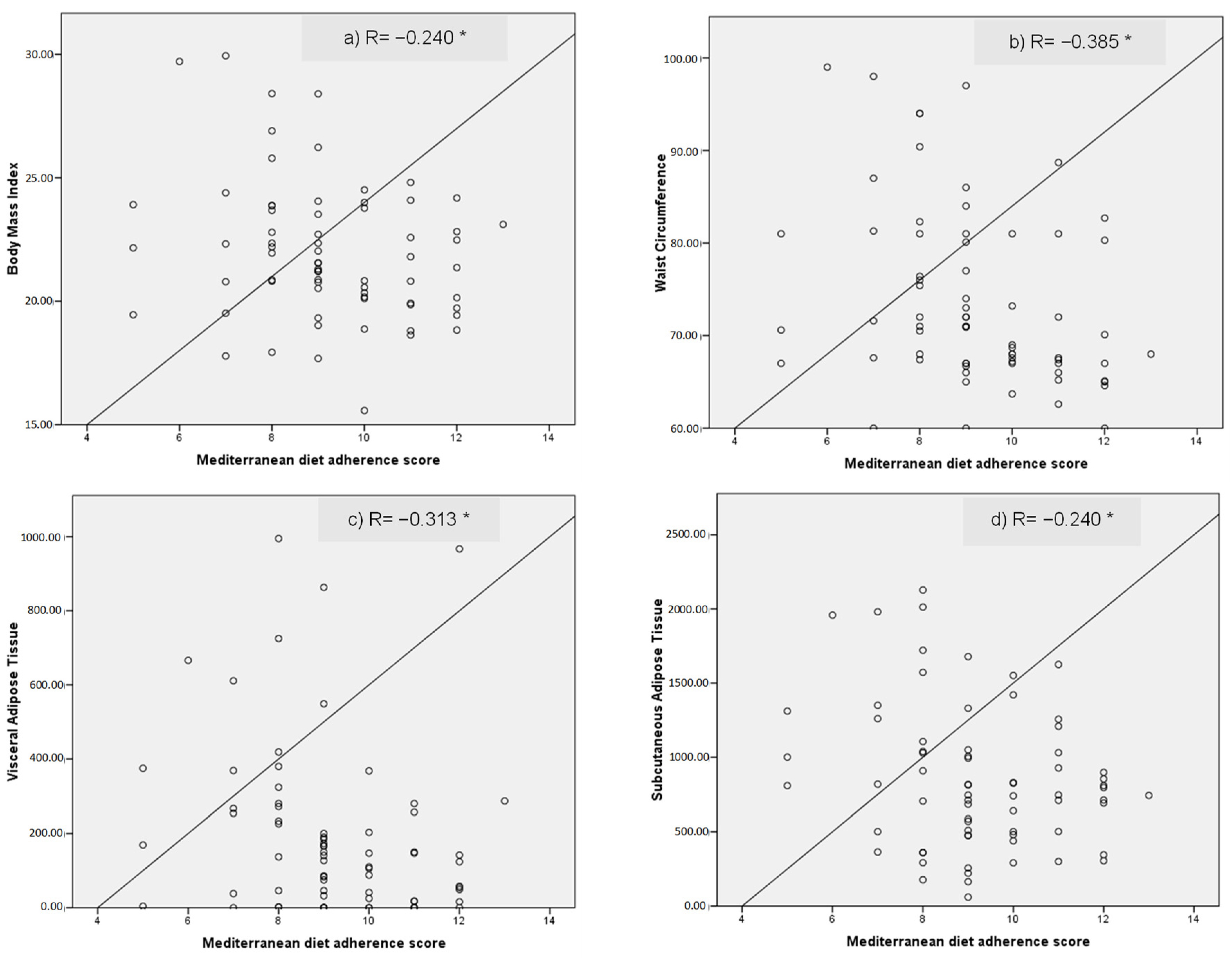
- Body Composition Benefits: Greater MedDiet adherence was associated with reduced visceral and subcutaneous fat, indicating healthier body composition patterns among university students.
- BMI and Waist Circumference Reduction: Higher adherence to MedDiet correlated with a lower Body Mass Index (BMI) and smaller waist circumference, suggesting a positive effect on weight management.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Participants’ Characterization and Instruments
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mistretta, A.; Marventano, S.; Antoci, M.; Cagnetti, A.; Giogianni, G.; Nolfo, F.; Rametta, S.; Pecora, G.; Marranzano, M. Mediterranean diet adherence and body composition among Southern Italian adolescents. Obes. Res. Clin. Pract. 2017, 11, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Zulet Fraile, P.; Lizancos Castro, A.; Andía Melero, V.; González Antigüedad, C.; Monereo Megías, S.; Calvo Revilla, S. Relación de La Composición Corporal Medida Por DEXA Con El Estilo de Vida y La Satisfacción Con La Imagen Corporal En Estudiantes Universitarios. Nutr. Hosp. 2019, 36, 919–925. [Google Scholar] [CrossRef] [PubMed]
- Cobo-Cuenca, A.I.; Garrido-Miguel, M.; Soriano-Cano, A.; Ferri-Morales, A.; Martínez-Vizcaíno, V.; Martín-Espinosa, N.M. Adherence to the Mediterranean Diet and Its Association with Body Composition and Physical Fitness in Spanish University Students. Nutrients 2019, 11, 2830. [Google Scholar] [CrossRef] [PubMed]
- Galan-Lopez, P.; Sánchez-Oliver, A.J.; Ries, F.; González-Jurado, J.A. Mediterranean Diet, Physical Fitness and Body Composition in Sevillian Adolescents: A Healthy Lifestyle. Nutrients 2019, 11, 2009. [Google Scholar] [CrossRef] [PubMed]
- UNESCO—Falconry, a Living Human Heritage. Available online: https://ich.unesco.org/en/RL/falconry-a-living-human-heritage-01708 (accessed on 9 March 2023).
- Galan-Lopez, P.; Ries, F.; Gisladottir, T.; Domínguez, R.; Sánchez-Oliver, A.J. Healthy Lifestyle: Relationship between Mediterranean Diet, Body Composition and Physical Fitness in 13 to 16-Year Old Icelandic Students. Int. J. Environ. Res. Public Health 2018, 15, 2632. [Google Scholar] [CrossRef]
- Silveira, E.A.; Barbosa, L.S.; Rodrigues, A.P.S.; Noll, M.; De Oliveira, C. Body fat percentage assessment by skinfold equation, bioimpedance and densitometry in older adults. Arch. Public Health 2020, 78, 65. [Google Scholar] [CrossRef]
- Murphy, R.A.; Reinders, I.; Register, T.C.; Ayonayon, H.N.; Newman, A.B.; Satterfield, S.; Goodpaster, B.H.; Simonsick, E.M.; Kritchevsky, S.B.; Harris, T.B. Associations of BMI and adipose tissue area and density with incident mobility limitation and poor performance in older adults. Am. J. Clin. Nutr. 2014, 99, 1059–1065. [Google Scholar] [CrossRef]
- Ortega, F.B.; Sui, X.; Lavie, C.J.; Blair, S.N. Body Mass Index, the Most Widely Used But Also Widely Criticized Index: Would a Gold-Standard Measure of Total Body Fat Be a Better Predictor of Cardiovascular Disease Mortality? Mayo Clin. Proc. 2016, 91, 443–455. [Google Scholar] [CrossRef]
- Ferreira-Pêgo, C.; Rodrigues, J.; Costa, A.; Sousa, B. Adherence to the Mediterranean Diet in Portuguese University Students. Biomed. Biopharm. Res. J. 2019, 16, 41–49. [Google Scholar] [CrossRef]
- Leri, M.; Scuto, M.; Ontario, M.L.; Calabrese, V.; Calabrese, E.J.; Bucciantini, M.; Stefani, M. Healthy Effects of Plant Polyphenols: Molecular Mechanisms. Int. J. Mol. Sci. 2020, 21, 1250. [Google Scholar] [CrossRef]
- Castro-Barquero, S.; Lamuela-Raventós, R.M.; Doménech, M.; Estruch, R. Relationship between Mediterranean Dietary Polyphenol Intake and Obesity. Nutrients 2018, 10, 1523. [Google Scholar] [CrossRef]
- da Silva, T.R.; Martins, C.C.; Ferreira, L.L.; Spritzer, P.M. Mediterranean diet is associated with bone mineral density and muscle mass in postmenopausal women. Climacteric 2019, 22, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Kalkuz, S.; Demircan, A. Effects of the Mediterranean diet adherence on body composition, blood parameters and quality of life in adults. Postgrad. Med. J. 2021, 97, 798–802. [Google Scholar] [CrossRef] [PubMed]
- Sood, S.; Feehan, J.; Itsiopoulos, C.; Wilson, K.; Plebanski, M.; Scott, D.; Hebert, J.R.; Shivappa, N.; Mousa, A.; George, E.S.; et al. Higher Adherence to a Mediterranean Diet Is Associated with Improved Insulin Sensitivity and Selected Markers of Inflammation in Individuals Who Are Overweight and Obese without Diabetes. Nutrients 2022, 14, 4437. [Google Scholar] [CrossRef] [PubMed]
- Hernáez, Á.; Castañer, O.; Goday, A.; Ros, E.; Pintó, X.; Estruch, R.; Salas-Salvadó, J.; Corella, D.; Arós, F.; Serra-Majem, L.; et al. The Mediterranean diet decreases LDL atherogenicity in high cardiovascular risk individuals: A randomized controlled trial. Mol. Nutr. Food Res. 2017, 61, 1601015. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 2019, CD009825. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Chrysoula, L.; Leonida, I.; Kotzakioulafi, E.; Theodoridis, X.; Chourdakis, M. Impact of the level of adherence to the Mediterranean diet on blood pressure: A systematic review and meta-analysis of observational studies. Clin. Nutr. 2021, 40, 5771–5780. [Google Scholar] [CrossRef]
- Manzano-Carrasco, S.; Felipe, J.L.; Sanchez-Sanchez, J.; Hernandez-Martin, A.; Gallardo, L.; Garcia-Unanue, J. Physical Fitness, Body Composition, and Adherence to the Mediterranean Diet in Young Football Players: Influence of the 20 mSRT Score and Maturational Stage. Int. J. Environ. Res. Public Health 2020, 17, 3257. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. Bull. World Health Organ. 2001, 70, 373–374. [Google Scholar]
- Instituto da Gestão do Fundo Social Europeu Nomenclatura Das Unidades Territoriais Para Fins Estatísticos (NUTS). Available online: http://www.igfse.pt/st_glossario.asp?startAt=2&categoryID=309 (accessed on 15 January 2023).
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Sepp, H.; Brage, S.; Becker, W.; Jakes, R.; Hennings, M.; Wareham, N.J. Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish adults. Public Health Nutr. 2006, 9, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Garrow, J.S.; Webster, J. Quetelet’s index (W/H2) as a measure of fatness. Int. J. Obes. 1985, 9, 147–153. [Google Scholar] [PubMed]
- Martínez-González, M.Á.; Corella, D.; Salas-Salvadó, J.; Ros, E.; Covas, M.I.; Fiol, M.; Wärnberg, J.; Arós, F.; Ruíz-Gutiérrez, V.; Lamuela-Raventós, R.M.; et al. Cohort Profile: Design and methods of the PREDIMED study. Int. J. Epidemiol. 2012, 41, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Mediterranean Diet Adherence in the Mediterranean Healthy Eating, Aging and Lifestyle (MEAL) Study Cohort—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/28562120/ (accessed on 9 March 2023).
- Karam, J.; Bibiloni, M.d.M.; Serhan, M.; Tur, J.A. Adherence to Mediterranean Diet among Lebanese University Students. Nutrients 2021, 13, 1264. [Google Scholar] [CrossRef]
- García-Meseguer, M.J.; Burriel, F.C.; García, C.V.; Serrano-Urrea, R. Adherence to Mediterranean diet in a Spanish university population. Appetite 2014, 78, 156–164. [Google Scholar] [CrossRef]
- Baydemir, C.; Ozgur, E.G.; Balci, S. Evaluation of adherence to Mediterranean diet in medical students at Kocaeli University, Turkey. J. Int. Med. Res. 2018, 46, 1585–1594. [Google Scholar] [CrossRef]
- Tuttolomondo, A.; Simonetta, I.; Daidone, M.; Mogavero, A.; Ortello, A.; Pinto, A. Metabolic and Vascular Effect of the Mediterranean Diet. Int. J. Mol. Sci. 2019, 20, 4716. [Google Scholar] [CrossRef]
- Carr, S.S.; Hooper, A.J.; Sullivan, D.R.; Burnett, J.R. Non-HDL-cholesterol and apolipoprotein B compared with LDL-cholesterol in atherosclerotic cardiovascular disease risk assessment. Pathology 2019, 51, 148–154. [Google Scholar] [CrossRef]
- Bendall, C.L.; Mayr, H.; Opie, R.; Bes-Rastrollo, M.; Itsiopoulos, C.; Thomas, C.J. Central obesity and the Mediterranean diet: A systematic review of intervention trials. Crit. Rev. Food Sci. Nutr. 2018, 58, 3070–3084. [Google Scholar] [CrossRef]
- Boivin, A.; Brochu, G.; Marceau, S.; Marceau, P.; Hould, F.-S.; Tchernof, A. Regional differences in adipose tissue metabolism in obese men. Metabolism 2007, 56, 533–540. [Google Scholar] [CrossRef]
- Sam, S. Differential effect of subcutaneous abdominal and visceral adipose tissue on cardiometabolic risk. Horm. Mol. Biol. Clin. Investig. 2018, 33, 20180014. [Google Scholar] [CrossRef]
- Lotta, L.A.; Abbasi, A.; Sharp, S.J.; Sahlqvist, A.-S.; Waterworth, D.; Brosnan, J.M.; Scott, R.A.; Langenberg, C.; Wareham, N.J. Definitions of Metabolic Health and Risk of Future Type 2 Diabetes in BMI Categories: A Systematic Review and Network Meta-analysis. Diabetes Care 2015, 38, 2177–2187. [Google Scholar] [CrossRef]
- Scaglioni, S.; De Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors Influencing Children’s Eating Behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef]
- The Influence of Peers’ and Siblings’ on Children’s and Adolescents’ Healthy Eating Behavior. A Systematic Literature Review—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/31927070/ (accessed on 16 March 2023).
- Iaccarino Idelson, P.; Scalfi, L.; Valerio, G. Adherence to the Mediterranean Diet in children and adolescents: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 283–299. [Google Scholar] [CrossRef]
- Mendonça, N.; Gregório, M.J.; Salvador, C.; Henriques, A.R.; Canhão, H.; Rodrigues, A.M. Low Adherence to the Mediterranean Diet Is Associated with Poor Socioeconomic Status and Younger Age: A Cross-Sectional Analysis of the EpiDoC Cohort. Nutrients 2022, 14, 1239. [Google Scholar] [CrossRef]
- Kastorini, C.-M.; Milionis, H.J.; Esposito, K.; Giugliano, D.; Goudevenos, J.A.; Panagiotakos, D.B. The Effect of Mediterranean Diet on Metabolic Syndrome and Its Components: A Meta-Analysis of 50 Studies and 534,906 Individuals. J. Am. Coll. Cardiol. 2011, 57, 1299–1313. [Google Scholar] [CrossRef]
- Agnoli, C.; Sieri, S.; Ricceri, F.; Giraudo, M.T.; Masala, G.; Assedi, M.; Panico, S.; Mattiello, A.; Tumino, R.; Giurdanella, M.C.; et al. Adherence to a Mediterranean diet and long-term changes in weight and waist circumference in the EPIC-Italy cohort. Nutr. Diabetes 2018, 8, 22. [Google Scholar] [CrossRef]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. Ser. A 2018, 73, 318–326. [Google Scholar] [CrossRef]
- Ventriglio, A.; Sancassiani, F.; Contu, M.P.; Latorre, M.; Di Slavatore, M.; Fornaro, M.; Bhugra, D. Mediterranean Diet and Its Benefits on Health and Mental Health: A Literature Review. Clin. Pract. Epidemiol. Ment. Health 2020, 16, 156–164. [Google Scholar] [CrossRef]
- Bazzocchi, A.; Ponti, F.; Albisinni, U.; Battista, G.; Guglielmi, G. DXA: Technical aspects and application. Eur. J. Radiol. 2016, 85, 1481–1492. [Google Scholar] [CrossRef] [PubMed]
- Rumbo-Rodríguez, L.; Sánchez-SanSegundo, M.; Ferrer-Cascales, R.; García-D’urso, N.; Hurtado-Sánchez, J.A.; Zaragoza-Martí, A. Comparison of Body Scanner and Manual Anthropometric Measurements of Body Shape: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6213. [Google Scholar] [CrossRef] [PubMed]
- Chiriacò, M.; Tubili, C.; Bo, S.; Parillo, M.; Vetrani, C.; Mazzotti, A.; Pistis, D.; Marelli, G.; Grandone, I.; Natali, A. Critical evaluation of the questionnaires assessing adherence to the Mediterranean diet that are based on servings. Nutr. Metab. Cardiovasc. Dis. NMCD 2023, 33, 724–736. [Google Scholar] [CrossRef] [PubMed]
| Total Population (n = 70) | Low Adherence (n = 23) | High Adherence (n = 47) | p-Value | |
|---|---|---|---|---|
| Sex, % (n) | ||||
| Male | 25.70 (18) | 39.10 (9) | 19.10 (9) | 0.072 c |
| Female | 74.30 (52) | 60.90 (14) | 80.9 (38) | |
| Age, years | 23.00 (7.00) | 24.00 (7.00) | 23.00 (7.00) | 0.598 b |
| Height, m | 1.67 (0.08) | 1.68 (0.72) | 1.66 (0.85) | 0.500 a |
| Mass, kg | 59.40 (14.00) | 63.80 (20.80) | 57.10 (13.60) | 0.138 b |
| BMI, kg/m2 | 21.99 (2.79) | 23.10 (3.34) | 21.44 (2.32) | 0.018 a |
| Waist Circumference, cm | 70.95 (14.00) | 76.00 (16.50) | 68.00 (7.30) | 0.004 b |
| Liquid Ingestion, L/day | 2.00 (1.00) | 2.00 (1.00) | 2.00 (1.00) | 0.749 b |
| Monthly Family Income, % (n) | ||||
| Under EUR 1000 | 8.60 (6) | 8.70 (2) | 8.50 (4) | 1.000 d |
| EUR 1000–3000 | 65.70 (46) | 65.20 (15) | 66.00 (31) | |
| EUR > 3000 | 25.70 (18) | 26.10 (6) | 25.50 (12) | |
| Smoking Status, % (n) | ||||
| Smoker | 11.40 (8) | 17.40 (4) | 8.50 (4) | 0.564 d |
| Ex-Smoker | 11.40 (8) | 13.00 (3) | 10.60 (5) | |
| Non-Smoker | 77.10 (54) | 69.60 (16) | 80.90 (38) | |
| Academic course, % (n) | ||||
| Health | 62.90 (44) | 60.90 (14) | 63.80 (30) | 0.810 c |
| Other | 37.1 (26) | 39.10 (9) | 36.20 (17) | |
| Home Living, % (n) | ||||
| Parents’ home | 48.60 (34) | 56.50 (13) | 44.70 (21) | 0.590 c |
| With other students | 17.10 (12) | 13.00 (3) | 19.10 (9) | |
| Partner | 18.60 (13) | 21.70 (5) | 17.00 (8) | |
| Alone | 15.70 (11) | 8.70 (2) | 19.10 (9) |
| Total Population (n = 70) | Low Adherence (n = 23) | High Adherence (n = 47) | p-Value | |
|---|---|---|---|---|
| Hemoglobin A1c, % | 5.23 (0.40) | 5.19 (0.39) | 5.26 (0.40) | 0.530 a |
| Triglycerides, mg/dL | 93.50 (68.00) | 89.00 (73.00) | 98.00 (70.00) | 0.822 b |
| Total Cholesterol, mg/dL | 169.24 (32.09) | 167.30 (36.57) | 170.19 (30.04) | 0.726 a |
| HDL, mg/dL | 60.77 (15.61) | 53.87 (9.90) | 64.15 (22.00) | 0.009 a |
| Glucose, mg/dL | 89.50 (15.00) | 94.00 (14.00) | 88.00 (12.00) | 0.057 b |
| LDL, mg/dL | 82.00 (27.45) | 90.50 (40.00) | 81.00 (28.00) | 0.210 a |
| VLDL, mg/dL | 19.00 (13.00) | 17.50 (14.00) | 20.00 (14.00) | 0.523 a |
| TC/HDL ratio, mg/dL | 2.75 (0.84) | 3.06 (1.07) | 2.65 (0.74) | 0.017 a |
| Non-HDL, mg/dL | 105.00 (30.00) | 111.50 (44.00) | 105.00 (26.00) | 0.460 a |
| Systolic Blood Pressure, mm Hg | 110.00 (12.06) | 113.13 (10.57) | 108.47 (12.55) | 0.130 a |
| Diastolic Blood Pressure, mm Hg | 70.50 (14.00) | 70.00 (13.00) | 71.00 (15.00) | 0.131 b |
| Heart Rate, bpm | 68.00 (14.00) | 66.00 (13.00) | 69.00 (17.00) | 0.381 b |
| Total Population (n = 70) | Low Adherence (n = 23) | High Adherence (n = 47) | p-Value | |
|---|---|---|---|---|
| Total BMD, % | 1.94 (0.24) | 1.86 (0.23) | 1.98 (0.24) | 0.060 a |
| Total BMC, % | 3.88 (0.33) | 3.81 (0.29) | 3.91 (0.35) | 0.229 a |
| Fat Mass, % | 27.88 (6.90) | 28.76 (7.88) | 27.45 (6.41) | 0.460 a |
| Lean Mass, % | 68.23 (6.73) | 67.41 (7.72) | 68.63 (6.24) | 0.481 a |
| Fat-Free Mass, % | 72.11 (6.89) | 71.22 (7.88) | 72.54 (6.39) | 0.455 a |
| VAT, cm3 | 141.50 (238.00) | 267.00 (334.00) | 106.00 (155.00) | 0.005 a |
| SAT, cm3 | 858.37 (485.16) | 1076.61 (603.05) | 751.58 (379.03) | 0.008 b |
| Mean (SD) | p-Value a | |
|---|---|---|
| Gender | ||
| Male | 8.78 (1.63) | 0.221 |
| Female | 9.38 (1.85) | |
| Academic course | ||
| Health | 9.25 (1.87) | 0.898 |
| Other | 9.19 (1.72) | |
| Student Worker | ||
| Yes | 9.21 (1.98) | 0.904 |
| No | 9.26 (1.59) | |
| Grade Level | ||
| Bachelor’s | 9.33 (1.86) | 0.543 |
| Master’s | 8.82 (1.43) | |
| PhD | 9.57 (2.30) | |
| Year Coursing—Bachelor’s | ||
| 1st | 8.33 (1.75) | 0.051 |
| 2nd | 10.20 (2.17) | |
| 3rd | 9.83 (1.63) | |
| 4th | 8.36 (1.86) | |
| Type of housing | ||
| Family | 9.12 (1.84) | 0.620 |
| Friends/Partner/Alone | 9.33 (1.79) | |
| Residence | ||
| Urban | 9.07 (1.71) | 0.104 |
| Rural | 10.00 (2.13) | |
| Monthly Family Income | ||
| Up to EUR 1000 | 8.67 (1.51) | 0.697 |
| EUR 1000–3000 | 9.33 (1.71) | |
| EUR > 3000 | 9.17 (2.15) | |
| Smoking Status. % (n) | ||
| Smoker | 8.25 (1.74) | 0.224 |
| Ex-Smoker | 9.00 (2.00) | |
| Non-Smoker | 9.41 (1.74) | |
| PAL | ||
| Low | 9.18 (2.27) | 0.413 |
| Medium | 9.47 (1.78) | |
| High | 8.76 (1.25) |
| Recommendation | Compliance by Sex | Compliance by Course | Compliance by Living Arrangement | Compliance by Income Level | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | p-Value a | Health | Other | p-Value a | Friends | Family | p-Value a | EUR < 1000 | EUR 1000–3000 | EUR > 3000 | p-Value a | ||
| 1. Do you use olive oil as a main culinary fat? | Yes | 94.40 | 94.20 | 0.973 | 95.50 | 92.30 | 0.584 | 100.00 | 88.90 | 0.045 | 100.00 | 93.50 | 94.40 | 0.811 |
| 2. How much olive oil do you consume in a given day (including the oil used for frying. salads. out-of-house meals. etc.)? | ≥4 tbsp | 22.20 | 34.60 | 0.329 | 36.40 | 23.10 | 0.247 | 38.20 | 25.00 | 0.233 | 83.30 | 28.30 | 22.20 | 0.015 |
| 3. How many vegetable servings do you consume per day? (1 serving: 200 g consider side dishes as half a serving)) | ≥2 (≥1 portion raw or as a salad) | 72.20 | 73.10 | 0.944 | 72.70 | 73.10 | 0.975 | 67.60 | 77.80 | 0.341 | 100.00 | 76.10 | 55.60 | 0.074 |
| 4. How many fruit units (including natural fruit juices) do you consume per day? | ≥3 | 61.10 | 48.10 | 0.340 | 50.00 | 53.80 | 0.756 | 55.90 | 47.20 | 0.469 | 16.70 | 58.70 | 44.40 | 0.121 |
| 5. How many servings of red meat. hamburger. or meat products (ham. sausage. etc.) do you consume per day? (1 serving: 100–150 g) | <1 | 66.70 | 86.50 | 0.062 | 81.80 | 80.80 | 0.913 | 76.50 | 86.10 | 0.300 | 100.00 | 80.40 | 77.80 | 0.459 |
| 6. How many servings of butter. margarine. or cream you consume per day? (1 serving: 12 g) | <1 | 72.20 | 80.80 | 0.446 | 77.30 | 80.80 | 0.730 | 73.50 | 83.30 | 0.318 | 66.70 | 71.70 | 100.00 | 0.035 |
| 7. How many sweet or carbonated beverages do you drink per day? | <1 | 88.90 | 92.30 | 0.655 | 90.90 | 92.30 | 0.840 | 88.20 | 94.40 | 0.354 | 66.70 | 93.50 | 94.40 | 0.076 |
| 8. How much wine do you drink per week? | ≥7 glasses | 5.60 | 7.70 | 0.762 | 6.80 | 7.70 | 0.891 | 8.80 | 5.60 | 0.596 | 0.00 | 4.30 | 16.70 | 0.177 |
| 9. How many servings of legumes do you consume per week? (1 serving: 150 g) | ≥3 | 66.70 | 59.60 | 0.596 | 47.70 | 84.60 | 0.002 | 44.10 | 77.80 | 0.004 | 66.70 | 58.70 | 66.70 | 0.809 |
| 10. How many servings of fish or shellfish do you consume per week? (1 serving of 100–150 g of fish or 4–5 units or 200 g of shellfish) | ≥3 | 27.80 | 73.10 | 0.001 | 72.70 | 42.30 | 0.012 | 70.60 | 52.80 | 0.126 | 33.30 | 67.40 | 55.60 | 0.229 |
| 11. How many times per week do you consume commercial sweets or pastries (not homemade). such as cakes. cookies. biscuits. or custard? | <3 | 88.90 | 67.30 | 0.076 | 72.70 | 73.10 | 0.975 | 61.80 | 83.30 | 0.043 | 33.30 | 78.30 | 72.20 | 0.066 |
| 12. How many servings of nuts (including peanuts) do you consume per week? (1 serving 30 g) | ≥3 | 55.60 | 55.80 | 0.987 | 56.80 | 53.80 | 0.809 | 47.10 | 63.90 | 0.157 | 33.30 | 63.00 | 44.40 | 0.207 |
| 13. Do you preferentially consume chicken. turkey. or rabbit meat instead of veal. pork. hamburger. or sausage? | Yes | 61.10 | 73.10 | 0.340 | 77.30 | 57.70 | 0.084 | 79.40 | 61.10 | 0.095 | 50.00 | 71.70 | 72.20 | 0.535 |
| 14. How many times per week do you consume vegetables. pasta. rice. or other dishes seasoned with sofrito (sauce made with tomato and onion. leek. or garlic and simmered with olive oil)? | ≥2 | 83.30 | 86.50 | 0.738 | 81.80 | 92.30 | 0.226 | 88.20 | 88.30 | 0.558 | 100.00 | 82.60 | 88.90 | 0.470 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopes, S.; Fontes, T.; Menezes, R.; Rodrigues, L.M.; Ferreira-Pêgo, C. Mediterranean Diet Adherence and Its Relationship to Metabolic Markers and Body Composition in Portuguese University Students. Nutrients 2023, 15, 2330. https://doi.org/10.3390/nu15102330
Lopes S, Fontes T, Menezes R, Rodrigues LM, Ferreira-Pêgo C. Mediterranean Diet Adherence and Its Relationship to Metabolic Markers and Body Composition in Portuguese University Students. Nutrients. 2023; 15(10):2330. https://doi.org/10.3390/nu15102330
Chicago/Turabian StyleLopes, Sofia, Tatiana Fontes, Regina Menezes, Luís Monteiro Rodrigues, and Cíntia Ferreira-Pêgo. 2023. "Mediterranean Diet Adherence and Its Relationship to Metabolic Markers and Body Composition in Portuguese University Students" Nutrients 15, no. 10: 2330. https://doi.org/10.3390/nu15102330
APA StyleLopes, S., Fontes, T., Menezes, R., Rodrigues, L. M., & Ferreira-Pêgo, C. (2023). Mediterranean Diet Adherence and Its Relationship to Metabolic Markers and Body Composition in Portuguese University Students. Nutrients, 15(10), 2330. https://doi.org/10.3390/nu15102330