Family Household Characteristics and Stunting: An Update Scoping Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Study Characteristics
3.2. Stunting Prevalence
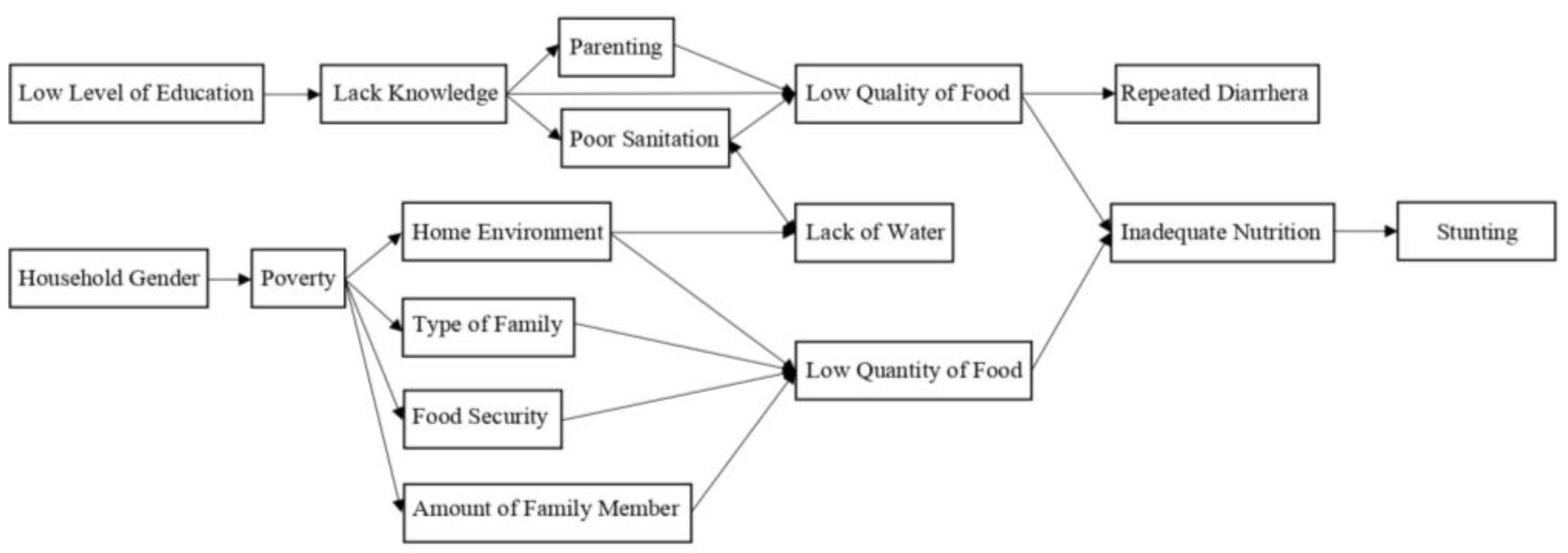
3.3. The Correlation between Family Household Characteristics and The Prevalence of Stunting
4. Discussion
4.1. Limitations
4.2. Implications for Clinical Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations Children’s Fund (UNICEF); World Health Organization; International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2021 Edition of the Joint Child Malnutrition Estimates; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Ministry of Health Indonesia. Situation of Stunted Toddler in Indonesia; Ministry of Health Indonesia: Jakarta, Indonesia, 2017. [Google Scholar]
- World Health Organization. Stunting in a Nutshell; World Heal Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Vaivada, T.; Akseer, N.; Akseer, S.; Somaskandan, A.; Stefopulos, M.; Bhutta, Z.A. Stunting in childhood: An overview of global burden, trends, determinants, and drivers of decline. Am. J. Clin. Nutr. 2020, 112 (Suppl. 2), 777S–791S. [Google Scholar] [CrossRef] [PubMed]
- Vonaesch, P.; Tondeur, L.; Breurec, S.; Bata, P.; Nguyen, L.B.L.; Frank, T.; Farra, A.; Rafaï, C.; Giles-Vernick, T.; Gody, J.C.; et al. Factors associated with stunting in healthy children aged 5 years and less living in Bangui (RCA). PLoS ONE 2017, 12, e0182363. [Google Scholar] [CrossRef] [PubMed]
- Beal, T.; Tumilowicz, A.; Sutrisna, A.; Izwardy, D.; Neufeld, L.M. A review of child stunting determinants in Indonesia. Matern. Child Nutr. 2018, 14, e12617. [Google Scholar] [CrossRef]
- Wirth, J.P.; Rohner, F.; Petry, N.; Onyango, A.W.; Matji, J.; Bailes, A.; de Onis, M.; Woodruff, B.A. Assessment of the WHO Stunting Framework using Ethiopia as a case study. Matern. Child Nutr. 2017, 13, e12310. [Google Scholar] [CrossRef] [PubMed]
- Imdad, A.; Yakoob, M.Y.; Bhutta, Z.A. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health 2011, 11, S25. [Google Scholar] [CrossRef] [PubMed]
- Ciptanurani, C.; Chen, H.-J. Household structure and concurrent stunting and overweight among young children in Indonesia. Public Health Nutr. 2021, 24, 2629–2639. [Google Scholar] [CrossRef]
- Sari, M.; Suhardin, S. Family determinants of stunting in Indonesia: A systematic review. Int. J. Psychosoc. Rehabil. 2020, 24, 815–822. [Google Scholar]
- Belayneh, M.; Loha, E.; Lindtjørn, B. Seasonal Variation of Household Food Insecurity and Household Dietary Diversity on Wasting and Stunting among Young Children in A Drought Prone Area in South Ethiopia: A Cohort Study. Ecol. Food Nutr. 2021, 60, 44–69. [Google Scholar] [CrossRef]
- Nshimyiryo, A.; Hedt-Gauthier, B.; Mutaganzwa, C.; Kirk, C.M.; Beck, K.; Ndayisaba, A.; Mubiligi, J.; Kateera, F.; El-Khatib, Z. Risk factors for stunting among children under five years: A cross-sectional population-based study in Rwanda using the 2015 Demographic and Health Survey. BMC Public Health 2019, 19, 175. [Google Scholar] [CrossRef]
- Habimana, S.; Biracyaza, E. Risk Factors of Stunting Among Children Under 5 Years of Age in The Eastern and Western Provinces of Rwanda: Analysis of Rwanda Demographic and Health Survey 2014/2015. Pediatr. Health Med. Ther. 2019, 10, 115–130. [Google Scholar] [CrossRef]
- United Nations Children’s Fund. The State of Children in Indonesia—Trends, Opportunities and Challenges for Realizing Children’s Rights; UNICEF Indonesia: Jakarta, Indonesia, 2020. [Google Scholar]
- World Health Organization. COVID-19 and the Social Determinants of Health and Health Equity: Evidence Brief; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Deatrick, J.A. Where Is “Family” in the Social Determinants of Health? Implications for Family Nursing Practice, Research, Education, and Policy. J. Fam. Nurs. 2017, 23, 423–433. [Google Scholar] [CrossRef]
- Government Regulation of the Republic of Indonesia. Implementation of Prosperous Family Development. Indonesia. 1994. Available online: https://peraturan.bpk.go.id/Home/Details/57208/pp-no-21-tahun-1994 (accessed on 10 October 2022).
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. Theory Pract. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Khalid, H.; Martin, E.G. Female-Headed Households Associated with Lower Childhood Stunting across Culturally Diverse Regions of Pakistan: Results from a Cross-Sectional Household Survey. Matern. Child Health J. 2017, 21, 1967–1984. [Google Scholar] [CrossRef] [PubMed]
- García Cruz, L.M.; González Azpeitia, G.; Reyes Súarez, D.; Santana Rodríguez, A.; Loro Ferrer, J.F.; Serra-Majem, L. Factors associated with stunting among children aged 0 to 59 months from the central region of Mozambique. Nutrients 2017, 9, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Bukusuba, J.; Kaaya, A.N.; Atukwase, A. Predictors of stunting in children aged 6 to 59 months: A case–control study in Southwest Uganda. Food Nutr Bull. 2017, 38, 542–553. [Google Scholar] [CrossRef] [PubMed]
- Masrul, M. Characteristics of Stunting Children with Background History of Family Demography and Maternal Reproductive In Pasaman And Pasaman Barat District, West Sumatera. J. Midwifery 2018, 3, 146–152. [Google Scholar] [CrossRef]
- Agho, K.E.; Mukabutera, C.; Mukazi, M.; Ntambara, M.; Mbugua, I.; Dowling, M.; Kamara, J.K. Moderate and severe household food insecurity predicts stunting and severe stunting among Rwanda children aged 6–59 months residing in Gicumbi district. Matern. Child Nutr. 2019, 15, e12767. [Google Scholar] [CrossRef] [PubMed]
- Khairani, N.; Effendi, S.U. Family characteristics as risk factors of stunting among children age 12–59 month. J. Aisyah J. Ilmu Kesehat. 2019, 4, 119–130. [Google Scholar] [CrossRef]
- Oktariyani Dasril, A. Karakteristik keluarga terhadap kejadian stunting pada anak. J. Sehat Mandiri 2019, 14, 48–56. [Google Scholar] [CrossRef]
- Sumiati Arsin, A.A.; Syafar, M. Determinants of stunting in children under five years of age in the Bone regency. Enferm. Clin. 2020, 30, 371–374. [Google Scholar] [CrossRef]
- Yaya, S.; Oladimeji, O.; Kolawole, E.; Bishwajit, G. Household structure, maternal characteristics and children’ s stunting in sub-Saharan Africa: Evidence from 35 countries. Int. Health 2019, 14, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Utami, R.A.; Setiawan, A.; Fitriyani, P. Identifying causal risk factors for stunting in children under five years of age in South Jakarta, Indonesia. Enferm. Clin. 2019, 29, 606–611. [Google Scholar] [CrossRef]
- Ariati, L.I.P. Faktor-faktor resiko penyebab terjadinya stunting pada balita usia 23–59 bulan. Oksitoksin J. Ilm Kebidanan 2019, 6, 28–37. [Google Scholar]
- Masereka, E.M.; Kiconco, A.; Katsomyo, E.; Munguiko, C. The Prevalence and Determinants of Stunting among Children 6–59 Months of Age in One of the Sub-Counties in the Rwenzori Sub-Region, Western Uganda. Open J. Nurs. 2020, 10, 239–251. [Google Scholar] [CrossRef][Green Version]
- Simelane, M.S.; Chemhaka, G.B.; Zwane, E. A multilevel analysis of individual, household and community level factors on stunting among children aged 6-59 months in Eswatini: A secondary analysis of the Eswatini 2010 and 2014 Multiple Indicator Cluster Surveys. PLoS ONE 2020, 15, e0241548. [Google Scholar] [CrossRef]
- Jayanti, R.; Yanuaringsih, G.P.; Olivia, N.; Jundapri, K.; Ariandini, S.; Munir, R. Determinants of Stunting in Indonesian Toddlers. Indian J. Forensic Med. Toxicol. 2021, 15, 3954. [Google Scholar]
- Susanto, T.; Rasni, H.; Susumaningrum, L.A. Prevalence of malnutrition and stunting among under-five children: A cross-sectional study family of quality of life in agricultural areas of Indonesia. Med. J. Nutr. Metab. 2021, 14, 147–161. [Google Scholar] [CrossRef]
- Tanzil, L.; Hafriani, H. Faktor-faktor yang mempengaruhi terjadinya stunting pada balita usia 24–59 bulan. J. Kebidanan Malahayati 2021, 7, 25–31. [Google Scholar] [CrossRef]
- Saeni, R.H.; Arief, E. Family Biopsychosocial Characteristics on Stunting Events in Children in Stunting Locus Areas Tapalang Barat District. Int. J. Health Sci. Res. 2022, 12, 30–39. [Google Scholar] [CrossRef]
- Stewart, C.P.; Iannotti, L.; Dewey, K.G.; Michaelsen, K.F.; Onyango, A.W. Contextualising complementary feeding in a broader framework for stunting prevention. Matern. Child Nutr. 2013, 9 (Suppl. 2), 27–45. [Google Scholar] [CrossRef]
- Huriah, T.; Nurjannah, N. Risk factors of stunting in developing countries: A scoping review. Open Access Maced. J. Med. Sci. 2020, 8, 155–160. [Google Scholar] [CrossRef]
- Geberselassie, S.B.; Abebe, S.M.; Melsew, Y.A.; Mutuku, S.M.; Wassie, M.M. Prevalence of stunting and its associated factors among children 6-59 months of age in Libo-Kemekem district, Northwest Ethiopia; A community based cross sectional study. PLoS ONE 2018, 13, e0195361. [Google Scholar] [CrossRef] [PubMed]
- Thurstans, S.; Opondo, C.; Seal, A.; Wells, J.; Khara, T.; Dolan, C.; Briend, A.; Myatt, M.; Garenne, M.; Sear, R.; et al. Boys are more likely to be undernourished than girls: A systematic review and meta-analysis of sex differences in undernutrition. BMJ Glob. Health 2020, 5, e004030. [Google Scholar] [CrossRef] [PubMed]
- Tahangnacca, M.; Amiruddin, R.; Ansariadi Syam, A. Model of stunting determinants: A systematic review. Enfermería Clínica 2020, 30, 241–245. Available online: https://www.sciencedirect.com/science/article/pii/S113086212030187X (accessed on 16 November 2022). [CrossRef]
- Islam, M.S.; Zafar Ullah, A.N.; Mainali, S.; Imam, M.A.; Hasan, M.I. Determinants of stunting during the first 1000 days of life in Bangladesh: A review. Food Sci. Nutr. 2020, 8, 4685–4695. [Google Scholar] [CrossRef]
- Rohmawati, N. Risk factors stunting incidence in children aged 6-36 months in jember regency. UNEJ e-Proceeding 2018, 1, 128–136. [Google Scholar]
- Aryastami, N.K.; Shankar, A.; Kusumawardani, N.; Besral, B.; Jahari, A.B.; Achadi, E. Low birth weight was the most dominant predictor associated with stunting among children aged 12–23 months in Indonesia. BMC Nutr. 2017, 3, 16. [Google Scholar] [CrossRef]
- Titaley, C.R.; Ariawan, I.; Hapsari, D.; Muasyaroh, A.; Dibley, M.J. Determinants of the Stunting of Children Under Two Years Old in Indonesia: A Multilevel Analysis of the 2013 Indonesia Basic Health Survey. Nutrients 2019, 11, 1106. [Google Scholar] [CrossRef]
- Wendt, A.; Hellwig, F.; Saad, G.E.; Faye, C.; Mokomane, Z.; Boerma, T.; Barros, A.J.D.; Victora, C. Are children in female-headed households at a disadvantage? An analysis of immunization coverage and stunting prevalence: In 95 low- and middle-income countries. SSM Popul. Health 2021, 15, 100888. [Google Scholar] [CrossRef]
- Wondimu, H.; Delelegn, W.; Dejene, K. What do female-headed households’ livelihood strategies in Jimma city, South west Ethiopia look like from the perspective of the sustainable livelihood approach? Cogent. Soc. Sci. 2022, 8, 2075133. [Google Scholar] [CrossRef]
- Rahayuwati, L.; Nurhidayah, I.; Hidayati, N.O.; Hendrawati, S.; Agustina, H.S.; Ekawati, R. Analysis of factor affecting nutrition status on children. J. Keperawatan Padjadjaran 2019, 7, 119–133. [Google Scholar] [CrossRef][Green Version]
- Rahayuwati, L.; Nurhidayah, I.; Hidayati, N.O.; Hendrawati, S.; Agustina, H.S.; Ekawati, R.; Setiawan, A.S. Analysis of factors affecting the prevalence of stunting on children under five years. EurAsian J. Biosci. 2020, 14, 6565–6575. [Google Scholar]
- Yani, D.I.; Hidayat, Y.F.; Amrullah, A.A. Erratum to: Knowledge, attitude, and practice of cough etiquette in patients with Tuberculosis in the community health centers. Belitung Nurs. J. 2020, 6, 186. [Google Scholar] [CrossRef]
- Vilcins, D.; Sly, P.D.; Jagals, P. Environmental Risk Factors Associated with Child Stunting: A Systematic Review of the Literature. Ann. Glob. Health 2018, 84, 551–562. [Google Scholar] [CrossRef]
- Pun, V.C.; Dowling, R.; Mehta, S. Ambient and household air pollution on early-life determinants of stunting—A systematic review and meta-analysis. Environ. Sci. Pollut. Res. 2021, 28, 26404–26412. [Google Scholar] [CrossRef]
- Juniarti, N.; Nurapipah, M.; Yani, D.I.; Sari, C.W.M. Influencing factors of community empowerment for domestic waste prevention and management among people living in river basin: A scoping review. Indian J. Public Health 2021, 65, 302–306. Available online: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85116977073&doi=10.4103%2Fijph.IJPH_1281_20&partnerID=40&md5=057efb0b74165317ebb5b67fe5fc3a5e (accessed on 20 November 2022). [PubMed]
- Frankenberger, T.; McCaston, M. The Household Livelihood Security Concept: Food Nutrition and Agriculture; FAO: Rome, Italy, 1998. [Google Scholar]
- Palmer, R.C.; Ismond, D.; Rodriquez, E.J.; Kaufman, J.S. Social Determinants of Health: Future Directions for Health Disparities Research. Am. J. Public Health 2019, 109, S70–S71. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Fleury, M.-J.; Xiang, Y.-T.; Li, M.; D’Arcy, C. Resilience and protective factors among people with a history of child maltreatment: A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 453–475. [Google Scholar] [CrossRef]
- Susanti, R.D.; Juniarti, N.; Yani, D.I.; Nurhasanah, N. Culture versus Technology: Bridging the Gap to Improve COVID-19 Prevention and Care based on the COVID-19 Task Force Perspectives. Open Access Maced. J. Med. Sci. 2021, 9, 92–100. [Google Scholar] [CrossRef]

| Components | Author | Frequency |
|---|---|---|
| Publishing Year | ||
| 2017 | [19,20,21] | 3 |
| 2018 | [22] | 1 |
| 2019 | [12,23,24,25,26,27,28,29] | 8 |
| 2020 | [30,31] | 2 |
| 2021 | [9,11,32,33,34] | 5 |
| 2022 | [35] | 1 |
| Country | ||
| Ethiopia | [11] | 1 |
| Indonesia | [9,22,24,25,26,28,29,32,33,34,35] | 11 |
| Kwaluseni | [31] | 1 |
| Mozambique | [20] | 1 |
| Pakistan | [19] | 1 |
| Rwanda | [12,23] | 2 |
| Sub-saharan Africa | [27] | 1 |
| Uganda | [21,30] | 2 |
| Study Method | ||
| Case control | [20,21,22,32,34,35] | 6 |
| Cohort Study | [11] | 1 |
| Cross Sectional Study | [9,12,19,23,24,25,26,28,29,30,33] | 9 |
| Survey | [27,31] | 2 |
| Sampling Technique | ||
| Random Sampling | ||
| Cluster Sampling | [19,26,27,28] | 4 |
| Random sampling | [12,21,29] | 3 |
| Systematic Sampling | [30,31] | 2 |
| Two stage sampling | [11,23] | 2 |
| Non Random Sampling | ||
| Accidental Sampling | [24] | 1 |
| Consecutive Sampling | [20,33] | 2 |
| Purposive Sampling | [9,22,32,34,35] | 5 |
| Total Population Sampling | [25] | 1 |
| Sample Size | ||
| <50 | [34] | 1 |
| <200 | [21,22,25,26,28,32,35] | 7 |
| <1000 | [11,20,29,30,33] | 5 |
| <10,000 | [12,19,23,24,31] | 5 |
| >10,000 | [9,27] | 2 |
| Respondent’s Age (Children) | ||
| Infants | ||
| 0–6 months | [12,20,22,27,33] | 5 |
| 6–12 months | [11,12,20,21,22,26,27,30,31,33] | 10 |
| Toddler (1–3 years) | [9,11,12,19,20,21,22,26,27,29,30,31,32,33,34,35] | 17 |
| Preschool (3–5 years) | [9,11,12,19,20,21,24,26,27,30,31,32,33,34,35] | 15 |
| Under five years old | [23,28,29] | 3 |
| School (above 5 years) | [25] | 1 |
| Components | Author | Frequency |
|---|---|---|
| Stunting Prevalence (n (%)) | ||
| ≤25% | ||
| 949 (4.8%) (stunting & overweight) | [9] | 1 |
| 512–593 (20%–24%) (different years (2010 and 2014) | [31] | 1 |
| 31 (25%) | [25] | 1 |
| 26%–50% | ||
| 32 (31.37%) | [24] | 1 |
| 36 (32.4%) | [29] | 1 |
| 54 (32.73%) | [26] | 1 |
| 56 (33%) | [21] | 1 |
| 73.751 (34%) | [27] | 1 |
| 102 (36%) | [20] | 1 |
| 74 (38.5%) | [28] | 1 |
| 1.355 (37%) | [12] | 1 |
| 1.408 (43%) | [11] | 1 |
| 167 (44.9%) | [30] | 1 |
| 198 (46.7%) | [33] | 1 |
| 57 (50%) | [35] | 1 |
| 60 (50%) | [32] | 1 |
| 20 (50%) | [34] | 1 |
| >51% | ||
| 94 (51%) | [22] | 1 |
| 5.140 (71%) | [19] | 1 |
| Not Mentioned | [23] | 1 |
| Stunting Assessment Method | ||
| KMS Data (Indonesian Local Card) | [22,24,32,35] | 4 |
| Demographic and Health Survey (DHS) | [12,27] | 2 |
| Height/ Length Assessment | [23,25,26,30] | 4 |
| Height for age score | [9,11,19,20,21,29,31,33] | 8 |
| Not Mentioned | [28,34] | 2 |
| Family Household Variables | Author | Statistic Test | p-Value | Correlation Score | Correlation |
|---|---|---|---|---|---|
| Individual Level Factors | |||||
| Sex of child | [20] | Binary Logistic Regression (Crude Odds Ratio) | 0.001 | 4.01 | Significantly correlated |
| [21] | Chi-square | 0.016 | n/a | Significantly correlated | |
| [12] | Chi-square | <0.01 | n/a | Significantly correlated | |
| [27] | Chi-square | <0.001 | n/a | Significantly correlated | |
| [31] | Chi-square | <0.001 | 15.61 | Significantly correlated | |
| [9] | Chi-square | >0.05 | 0.89 | Not correlated | |
| [11] | Logistic linear | >0.05 | 1.52 | Not correlated | |
| History of diarrhoea | [12] | Chi-square | <0.01 | n/a | Significantly correlated |
| Age of child | [19] | Logistic regression (Odds Ratio) | 0.96 | 1 | Not correlated |
| [21] | Chi-square | 0.798 | n/a | Not Correlated | |
| [22] | n/a | 0.640 | n/a | Not Correlated | |
| [23] | Chi-square | 0.0001 | 1.78 | Significantly correlated | |
| [12] | Chi-square | <0.01 | n/a | Significantly correlated | |
| [27] | Chi-square | <0.001 | n/a | Significantly correlated | |
| [33] | Product Moment Test | >0.05 | 0.027 | Not correlated | |
| [28] | Chi-square | 3.92 | 1.348 | Not correlated | |
| [31] | Chi-square | <0.001 | 51.26 | Significantly correlated | |
| [11] | Logistic linear | >0.05 | 1.43 | Not correlated | |
| Birth place of child | [21] | Chi-square | 1.0 | n/a | Not correlated |
| Family Level Factors | |||||
| Household headship | |||||
| Gender of house hold headship | [19] | Logistic regression (Odds Ratio) | <0.01 | 0.74 | Significantly correlated |
| [21] | Chi-square | 1.00 | n/a | Not correlated | |
| [27] | Chi-square | <0.001 | n/a | Significantly correlated | |
| [9] | Chi-square | >0.05 | 0.83 | Not correlated | |
| Education of household Headship | [19] | Logistic regression (Odds Ratio) | 0.01 | 0.56 | Significantly correlated |
| [22] | Chi-square | 0.003 | n/a | Significantly correlated | |
| [28] | Chi-square | 0.000 | 4.596 | Significantly correlated | |
| [9] | Chi-square | >0.05 | 0.68 | Not correlated | |
| Age of household headship | [28] | Pearson | 0.132 | 0.069 | Not correlated |
| [9] | Chi-square | >0.05 | 0.82 | Not correlated | |
| Primary Caregiver | |||||
| Age of parent | [33] | Product Moment Test | >0.05 | 0.049 | Not correlated |
| Type of Family | [20] | Binary Logistic Regression (Crude Odds Ratio) | 18.36 | 0.001 | Significantly correlated |
| [22] | Chi-square | 0.017 | n/a | Significantly correlated | |
| [27] | Chi-square | <0.001 | n/a | Significantly correlated | |
| [28] | Chi-square | 0.059 | 1.841 | Not correlated | |
| [9] | Chi-square | >0.05 | 0.98 | Not correlated | |
| Sex of primary caregiver | [21] | Chi-square | 0.378 | n/a | Not correlated |
| Education of primary caregiver | [21] | Chi-square | 0.126 | n/a | Not correlated |
| [23] | Chi-square | 0.937 | 1.42 | Not correlated | |
| [12] | Chi-square | <0.01 | n/a | Significantly correlated | |
| [24] | Chi-square | 0.455 | n/a | Not correlated | |
| [25] | Chi-square | 0.00 | n/a | Significantly correlated | |
| [27] | Chi-square | <0.001 | n/a | Significantly correlated | |
| [28] | Chi-square | 0.006 | 2.440 | Significantly correlated | |
| [29] | Chi-square | 0.048 | n/a | Significantly correlated | |
| [31] | Chi-square | <0.001 | 59.53 | Significantly correlated | |
| [34] | Chi-square | 0.000 | 22.667 | Significantly correlated | |
| [11] | Logistic linear | >0.05 | 0.19 | Not correlated | |
| Relationship of primary caregiver to child | [21] | Chi-square | 0.693 | n/a | Not correlated |
| [23] | Chi-square | 0.01 | 0.82 | Significantly correlated | |
| Mother’s height | [24] | Chi-square | 0.257 | n/a | Not correlated |
| [34] | Chi-square | 0.84 | 1.08 | Not correlated | |
| Mother’s knowledge | [24] | Chi-square | 0.003 | n/a | Significantly correlated |
| [34] | Chi-square | 0.006 | 28 | Significantly correlated | |
| Mother’s marital stutus | [27] | Chi-square | <0.001 | n/a | Not correlated |
| [31] | Chi-square | 0.195 | 3.27 | Not correlated | |
| Mother’s age | [27] | Chi-square | <0.001 | n/a | Significantly correlated |
| [28] | Pearson | 0.109 | 0.065 | Not correlated | |
| [31] | Chi-square | 0.390 | 6.30 | Not correlated | |
| [11] | Logistic linear | >0.05 | 0.97 | Not correlated | |
| Mother’s occupation | [20] | Binary Logistic Regression | 0.304 | 0.23 | Not correlated |
| [28] | Chi-square | 0.005 | 1.045 | Significantly correlated | |
| [29] | Chi-square | 0.797 | n/a | Not correlated | |
| [34] | Chi-square | 0.744 | 1.238 | Not correlated | |
| [11] | Logistic linear | <0.001 | 0.09 | Significantly correlated | |
| Socio-Cultural Orientation | |||||
| Famliy wealth/socio-economic status | [19] | Logistic regression (Odds Ratio) | <0.01 | 0.35–0.78 | Significantly correlated |
| [21] | Chi-square | 0.510 | n/a | Not correlated | |
| [22] | Chi-square | 0.081 | n/a | Not correlated | |
| [23] | Chi-square | 0.088 | 1.43 | Not correlated | |
| [12] | Chi-square | <0.01 | n/a | Significantly correlated | |
| [24] | Chi-square | 0.320 | n/a | Not correlated | |
| [25] | Chi-square | 0.00 | n/a | Significantly correlated | |
| [27] | Chi-square | <0.001 | n/a | Significantly correlated | |
| [28] | Chi-square | 0.000 | 3778 | Significantly correlated | |
| [29] | Chi-square | 0.000 | n/a | Significantly correlated | |
| [31] | Chi-square | <0.001 | 48.30 | Significantly Correlated | |
| [32] | Chi-square | 0.004 | 9.33 | Significantly Correlated | |
| [9] | Chi-square | >0.05 | 0.73 | Not correlated | |
| [34] | Chi-square | 0.001 | 13.22 | Significantly correlated | |
| [11] | Logistic linear | >0.05 | 4.01 | Not correlated | |
| Family Ethnicity | [19] | Logistic regression (Odds Ratio) | 0.02 | 1.35 | Significantly correlated |
| [21] | Chi-square | 0.759 | n/a | Not correlated | |
| Area of residence | [20] | Binary Logistic Regression (Crude Odds Ratio) | 0.001 | 137.95 | Significantly correlated |
| [12] | Chi-square | <0.01 | n/a | Significantly correlated | |
| [27] | Chi-square | <0.001 | n/a | Significantly correlated | |
| [31] | Chi-square | 0.012 | 6.38 | Significantly correlated | |
| Number of family members | [22] | t-test | 0.240 | n/a | Not correlated |
| [12] | Chi-square | 0.73 | n/a | Not correlated | |
| [24] | Chi-square | 0.245 | n/a | Not correlated | |
| [26] | Chi-square | 0.557 | n/a | Not correlated | |
| [9] | Chi-square | <0.01 | 0.59 | Significantly correlated | |
| Number of children | [31] | Chi-square | <0.001 | 20.63 | Significantly correlated |
| [9] | Chi-square | <0.05 | 0.52 | Significantly correlated | |
| Number of dependent adult | [9] | Chi-square | >0.05 | 0.66 | Not correlated |
| Siblings under 5 years old | [20] | Binary Logistic Regression (Crude Odds Ratio) | 0.001 | 41.75 | Significantly correlated |
| Family System Factors | |||||
| Family awareness nutrition | [33] | Product Moment Test | >0.05 | −0.048 | Not correlated |
| [11] | Logistic linear | >0.05 | 1.07 | Not correlated | |
| Food consumption score | [21] | Chi-square | 0.040 | n/a | Significantly correlated |
| Food security status | [21] | Chi-square | 0.021 | n/a | Significantly correlated |
| [23] | Chi-square | 0.006 | 1.68 | Significantly correlated | |
| [21] | Chi-square | 0.004 | 0.23 | Significantly correlated | |
| [11] | Logistic linear | >0.05 | 0.72 | Not correlated | |
| Family wellness | [33] | Product Moment Test | >0.05 | −0.055 | Not correlated |
| Knowledge of nutrition | [28] | Chi-square | 0.001 | 2.971 | Significantly correlated |
| Atttude toward nutrition | [28] | Chi-square | 0.001 | 2.971 | Significantly correlated |
| Behavior toward nutrition | [28] | Chi-square | 0.001 | 2.890 | Significantly correlated |
| Nutritional parenting | [28] | Chi-square | 0.000 | 3.896 | Significantly correlated |
| Family Quality of Life | [33] | Product Moment Test | <0.01 | 0.209 | Significantly correlated |
| Family interaction | [33] | Product Moment Test | <0.01 | 0.203 | Significantly correlated |
| Parenting | [33] | Product Moment Test | <0.01 | 0.175 | Significantly correlated |
| [25] | Chi-square | 0.007 | n/a | Significantly correlated | |
| Emotional welfare | [33] | Product Moment Test | <0.01 | 0.193 | Significantly correlated |
| Physical welfare | [33] | Product Moment Test | <0.01 | 0.216 | Significantly correlated |
| Family support | [33] | Product Moment Test | <0.01 | 0.136 | Significantly correlated |
| [35] | Chi-square | 0.49 | 0.49 | Not correlated | |
| Environment Factors | |||||
| Type of home: Straw and wood | [20] | Binary Logistic Regression (Crude Odds Ratio) | 0.002 | 3.27 | Significantly correlated |
| Exposure to cigarette smoke | [35] | Chi-square | 0.09 | 0.31 | Not correlated |
| Type of floor: soil | [20] | Binary Logistic Regression (Crude Odds Ratio) | 0.001 | 0.05 | Significantly correlated |
| Cooking fuel: wood | [20] | Binary Logistic Regression (Crude Odds Ratio) | 0.001 | 45.5 | Significantly correlated |
| Water access | [23] | Chi-square | 0.040 | 1.52 | Significantly correlated |
| [12] | Chi-square | <0.01 | n/a | Significantly correlated | |
| Sanitation facility | [12] | Chi-square | 0.052 | 0.40 | Not correlated |
| [30] | Chi-square | <0.01 | n/a | Significantly correlated | |
| [31] | Chi-square | <0.001 | 32.79 | Significantly correlated | |
| Source of drinking water | [21] | Chi-square | 0.004 | 0.92 | Significantly correlated |
| [31] | Chi-square | 0.020 | 5.45 | Significantly correlated | |
| Household electricity | [31] | Chi-square | <0.001 | 15.48 | Significantly correlated |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yani, D.I.; Rahayuwati, L.; Sari, C.W.M.; Komariah, M.; Fauziah, S.R. Family Household Characteristics and Stunting: An Update Scoping Review. Nutrients 2023, 15, 233. https://doi.org/10.3390/nu15010233
Yani DI, Rahayuwati L, Sari CWM, Komariah M, Fauziah SR. Family Household Characteristics and Stunting: An Update Scoping Review. Nutrients. 2023; 15(1):233. https://doi.org/10.3390/nu15010233
Chicago/Turabian StyleYani, Desy Indra, Laili Rahayuwati, Citra Windani Mambang Sari, Maria Komariah, and Sherllina Rizqi Fauziah. 2023. "Family Household Characteristics and Stunting: An Update Scoping Review" Nutrients 15, no. 1: 233. https://doi.org/10.3390/nu15010233
APA StyleYani, D. I., Rahayuwati, L., Sari, C. W. M., Komariah, M., & Fauziah, S. R. (2023). Family Household Characteristics and Stunting: An Update Scoping Review. Nutrients, 15(1), 233. https://doi.org/10.3390/nu15010233








