Choline Supplementation Does Not Promote Atherosclerosis in CETP-Expressing Male Apolipoprotein E Knockout Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Plasma Analysis of Trimethylamine N-Oxide
2.3. Lipoprotein Plasma Profiling
2.4. HDL Inflammatory Index (HII)
2.5. Measurement of Plasma Myeloperoxidase and Oxidized Phospholipids
2.6. Assessment of Atherosclerosis
2.7. Statistical Analysis
3. Results
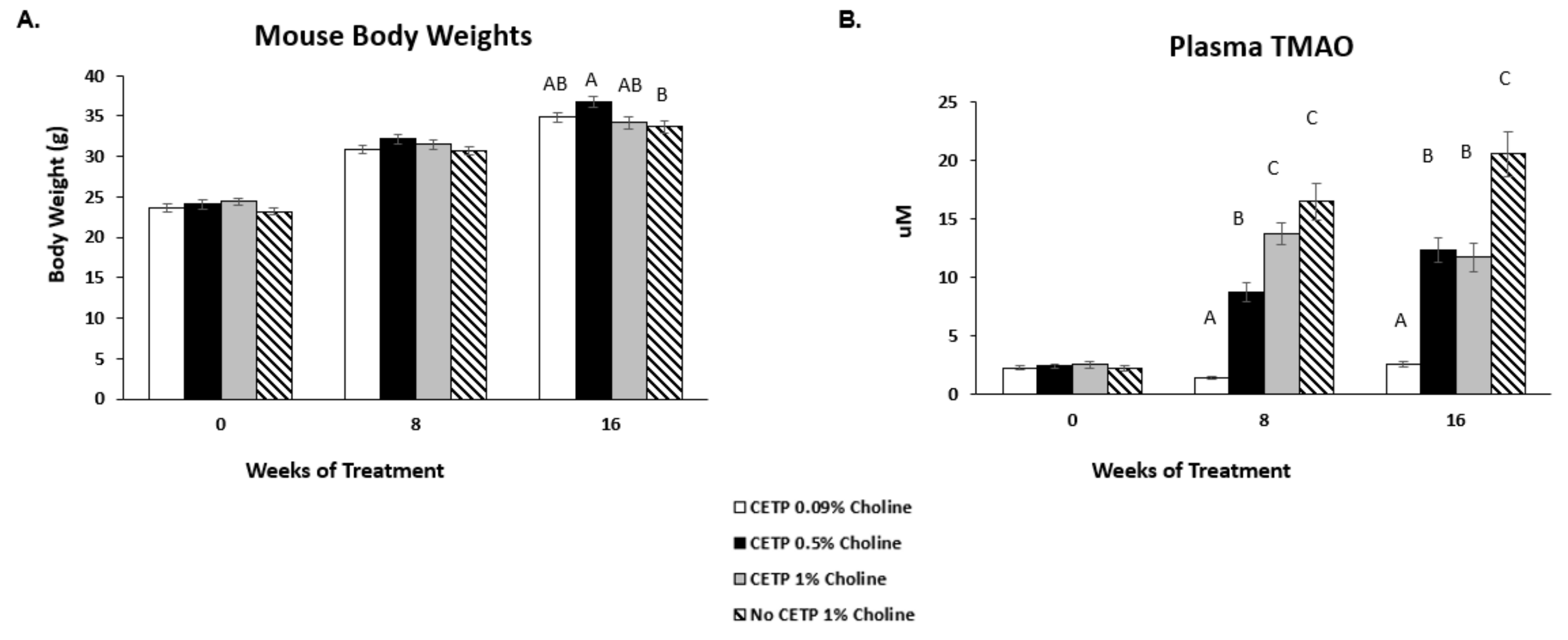
3.1. In Vivo Plasma Levels of TMAO
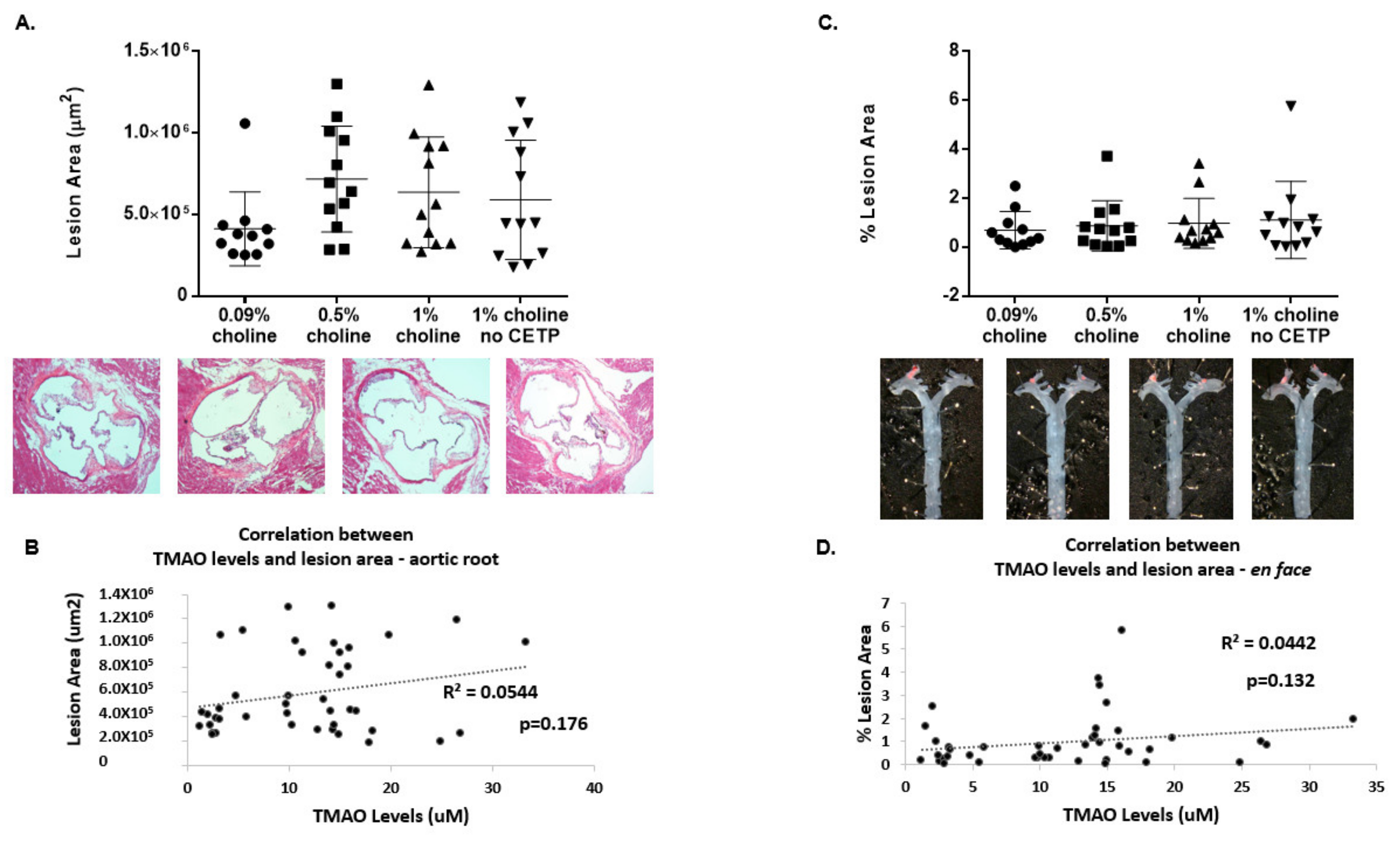
3.2. Lack of TMAO Effect on Aortic Lesions
3.3. Effects of Increased TMAO on Plasma Lipid Profile
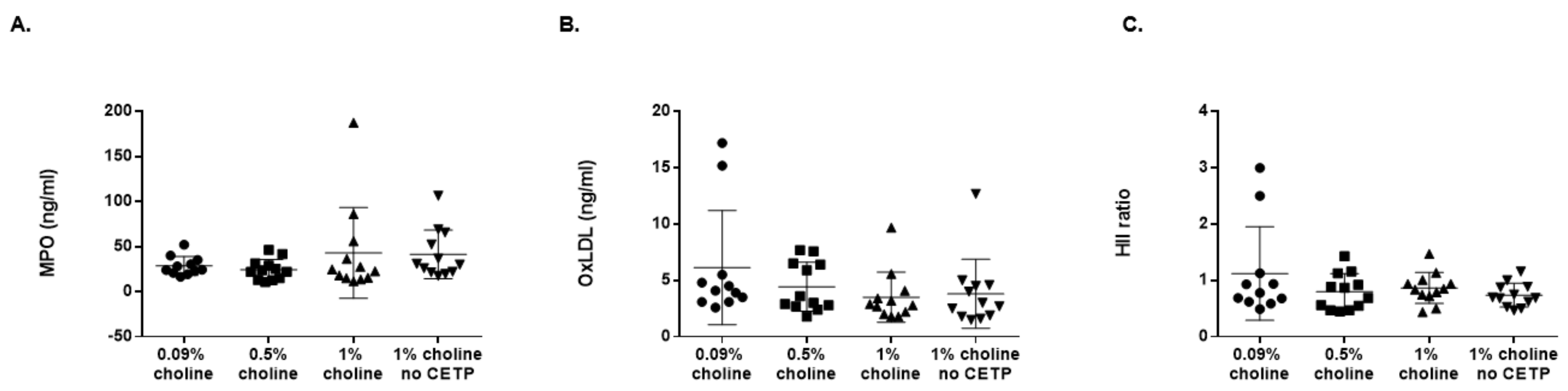
3.4. Effects of TMAO on MPO, OxLDL and HDL Antioxidant Capacity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Koeth, R.A.; Wang, Z.; Levison, B.S.; Buffa, J.A.; Org, E.; Sheehy, B.T.; Britt, E.B.; Fu, X.; Wu, Y.; Li, L.; et al. Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013, 19, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Klipfell, E.; Bennett, B.J.; Koeth, R.; Levison, B.S.; DuGar, B.; Feldstein, A.E.; Britt, E.B.; Fu, X.; Chung, Y.-M.; et al. Gut Flora Metabolism of Phosphatidylcholine Promotes Cardiovascular Disease. Nature 2011, 472, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Patterson, K.Y.; Bhagwat, S.A.; Williams, J.R.; Howe, J.C.; Holden, J.M.; Zeisel, S.H.; Dacosta, K.A.; Mar, M.-H. USDA Database for the Choline Content of Common Foods, Release Two; Nutrient Data Laboratory, Beltsville Human Nutrition Research Center, ARS, USDA: Beltsville, MD, USA, 2008.
- Institute of Medicine. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline; The National Academies Press: Washington, DC, USA, 1998; p. 592. [Google Scholar]
- Li, Z.; Vance, D.E. Thematic Review Series: Glycerolipids. Phosphatidylcholine and choline homeostasis. J. Lipid Res. 2008, 49, 1187–1194. [Google Scholar] [CrossRef] [PubMed]
- Van der Veen, J.N.; Kennelly, J.P.; Wan, S.; Vance, J.E.; Vance, D.E.; Jacobs, R.L. The critical role of phosphatidylcholine and phosphatidylethanolamine metabolism in health and disease. Biochim. Biophys. Acta Biomembr. 2017, 1859, 1558–1572. [Google Scholar] [CrossRef]
- James, S.J.; Melnyk, S.; Pogribna, M.; Pogribny, I.P.; Caudill, M.A. Elevation in S-Adenosylhomocysteine and DNA Hypomethylation: Potential Epigenetic Mechanism for Homocysteine-Related Pathology. J. Nutr. 2002, 132, 2361S–2366S. [Google Scholar] [CrossRef]
- Fungwe, T.; Cagen, L.; Wilcox, H.; Heimberg, M. Regulation of hepatic secretion of very low density lipoprotein by dietary cholesterol. J. Lipid Res. 1992, 33, 179–191. [Google Scholar] [CrossRef]
- Zeisel, S.H. Metabolic crosstalk between choline/1-carbon metabolism and energy homeostasis. Clin. Chem. Lab. Med. CCLM 2012, 51, 467–475. [Google Scholar] [CrossRef]
- Olthof, M.R.; Brink, E.J.; Katan, M.B.; Verhoef, P. Choline supplemented as phosphatidylcholine decreases fasting and postmethionine-loading plasma homocysteine concentrations in healthy men. Am. J. Clin. Nutr. 2005, 82, 111–117. [Google Scholar] [CrossRef]
- Aldana-Hernandez, P.; Leonard, K.-A.; Zhao, Y.-Y.; Curtis, J.M.; Field, C.J.; Jacobs, R.L. Dietary Choline or Trimethylamine N-oxide Supplementation Does Not Influence Atherosclerosis Development in Ldlr-/- and Apoe-/- Male Mice. J. Nutr. 2020, 150, 249–255. [Google Scholar] [CrossRef]
- Collins, H.L.; Drazul-Schrader, D.; Sulpizio, A.C.; Koster, P.D.; Williamson, Y.; Adelman, S.J.; Owen, K.; Sanli, T.; Bellamine, A. L-Carnitine intake and high trimethylamine N-oxide plasma levels correlate with low aortic lesions in ApoE−/− transgenic mice expressing CETP. Atherosclerosis 2016, 244, 29–37. [Google Scholar] [CrossRef]
- Lindskog Jonsson, A.; Caesar, R.; Akrami, R.; Reinhardt, C.; Hallenius, F.F.; Boren, J.; Backhead, F. Impact of Gut Microbiota and Diet on the Development of Atherosclerosis in Apoe-/- Mice. Arterioscler. Thromb. Vasc. Biol. 2018, 38, 2318–2326. [Google Scholar] [CrossRef]
- Tanigawa, H.; Billheimer, J.T.; Tohyama, J.-I.; Zhang, Y.; Rothblat, G.; Rader, D.J. Expression of Cholesteryl Ester Transfer Protein in Mice Promotes Macrophage Reverse Cholesterol Transport. Circulation 2007, 116, 1267–1273. [Google Scholar] [CrossRef]
- Patel, P.J.; Khera, A.V.; Jafri, K.; Wilensky, R.L.; Rader, D.J. The Anti-Oxidative Capacity of High-Density Lipoprotein Is Reduced in Acute Coronary Syndrome But Not in Stable Coronary Artery Disease. J. Am. Coll. Cardiol. 2011, 58, 2068–2075. [Google Scholar] [CrossRef]
- Navab, M.; Hama, S.Y.; Hough, G.P.; Subbanagounder, G.; Reddy, S.T.; Fogelman, A.M. A cell-free assay for detecting HDL that is dysfunctional in preventing the formation of or inactivating oxidized phospholipids. J. Lipid Res. 2001, 42, 1308–1317. [Google Scholar] [CrossRef]
- Tangirala, R.K.; Rubin, E.M.; Palinski, W. Quantitation of atherosclerosis in murine models: Correlation between lesions in the aortic origin and in the entire aorta, and differences in the extent of lesions between sexes in LDL receptor-deficient and apolipoprotein E-deficient mice. J. Lipid Res. 1995, 36, 2320–2328. [Google Scholar] [CrossRef]
- Getz, G.S.; Reardon, C.A. Diet, Microbes, and Murine Atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2018, 38, 2269–2271. [Google Scholar] [CrossRef]
- Ding, L.; Chang, M.; Guo, Y.; Zhang, L.; Xue, C.; Yanagita, T.; Zhang, T.; Wang, Y. Trimethylamine-N-oxide (TMAO)-induced atherosclerosis is associated with bile acid metabolism. Lipids Health Dis. 2018, 17, 1–8. [Google Scholar] [CrossRef]
- Chen, M.-L.; Zhu, X.-H.; Lang, H.-D.; Yi, L.; Mi, M.-T. Trimethylamine-N-Oxide induces vascular inflammation by activating the NLRP3 inflammasome through the SIRT3-SOD2-mtROS signaling pathway. J. Am. Heart Assoc. 2017, 6, e006347. [Google Scholar] [CrossRef]
- Butteiger, D.N.; Hibberd, A.A.; McGraw, N.J.; Napawan, N.; Hall-Porter, J.M.; Krul, E.S. Soy Protein Compared with Milk Protein in a Western Diet Increases Gut Microbial Diversity and Reduces Serum Lipids in Golden Syrian Hamsters. J. Nutr. 2016, 146, 697–705. [Google Scholar] [CrossRef]
- Panasevich, M.R.; Schuster, C.M.; Phillips, K.E.; Meers, G.M.; Chintapalli, S.V.; Wankhade, U.D.; Shankar, K.; Butteiger, D.N.; Krul, E.S.; Thyfault, J.P.; et al. Soy compared with milk protein in a Western diet changes fecal microbiota and decreases hepatic steatosis in obese OLETF rats. J. Nutr. Biochem. 2017, 46, 125–136. [Google Scholar] [CrossRef]
- Muralidharan, J.; Galiè, S.; Hernández-Alonso, P.; Bulló, M.; Salas-Salvadó, J. Plant-Based Fat, Dietary Patterns Rich in Vegetable Fat and Gut Microbiota Modulation. Front. Nutr. 2019, 6, 157. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Zhang, S.; Tian, M.; Chen, J.; Chen, F.; Guan, W. Different Sources of High Fat Diet Induces Marked Changes in Gut Microbiota of Nursery Pigs. Front. Microbiol. 2020, 11, 859. [Google Scholar] [CrossRef] [PubMed]
- Obregon-Tito, A.J.; Tito, R.Y.; Metcalf, J.L.; Sankaranarayanan, K.; Clemente, J.C.; Ursell, L.K.; Xu, Z.Z.; Van Treuren, W.; Knight, R.; Gaffney, P.; et al. Subsistence strategies in traditional societies distinguish gut microbiomes. Nat. Commun. 2015, 6, 6505. [Google Scholar] [CrossRef] [PubMed]
- Daugherty, A.; Rateri, D.L. Development of experimental designs for atherosclerosis studies in mice. Methods 2005, 36, 129–138. [Google Scholar] [CrossRef]
- Daugherty, A.; Rateri, D.L. Do Vivarium Conditions Influence Atherosclerotic Lesion Size? Arterioscler. Thromb. Vasc. Biol. 2012, 32, 2339–2340. [Google Scholar] [CrossRef][Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collins, H.L.; Adelman, S.J.; Butteiger, D.N.; Bortz, J.D. Choline Supplementation Does Not Promote Atherosclerosis in CETP-Expressing Male Apolipoprotein E Knockout Mice. Nutrients 2022, 14, 1651. https://doi.org/10.3390/nu14081651
Collins HL, Adelman SJ, Butteiger DN, Bortz JD. Choline Supplementation Does Not Promote Atherosclerosis in CETP-Expressing Male Apolipoprotein E Knockout Mice. Nutrients. 2022; 14(8):1651. https://doi.org/10.3390/nu14081651
Chicago/Turabian StyleCollins, Heidi L., Steven J. Adelman, Dustie N. Butteiger, and Jonathan D. Bortz. 2022. "Choline Supplementation Does Not Promote Atherosclerosis in CETP-Expressing Male Apolipoprotein E Knockout Mice" Nutrients 14, no. 8: 1651. https://doi.org/10.3390/nu14081651
APA StyleCollins, H. L., Adelman, S. J., Butteiger, D. N., & Bortz, J. D. (2022). Choline Supplementation Does Not Promote Atherosclerosis in CETP-Expressing Male Apolipoprotein E Knockout Mice. Nutrients, 14(8), 1651. https://doi.org/10.3390/nu14081651





