The Impact of the Universal Infant Free School Meal Policy on Dietary Quality in English and Scottish Primary School Children: Evaluation of a Natural Experiment
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Source
2.3. Study Participants
2.4. Exposure Variables
2.5. Outcome Variables
2.6. Covariates
2.7. Statistical Analysis
3. Results
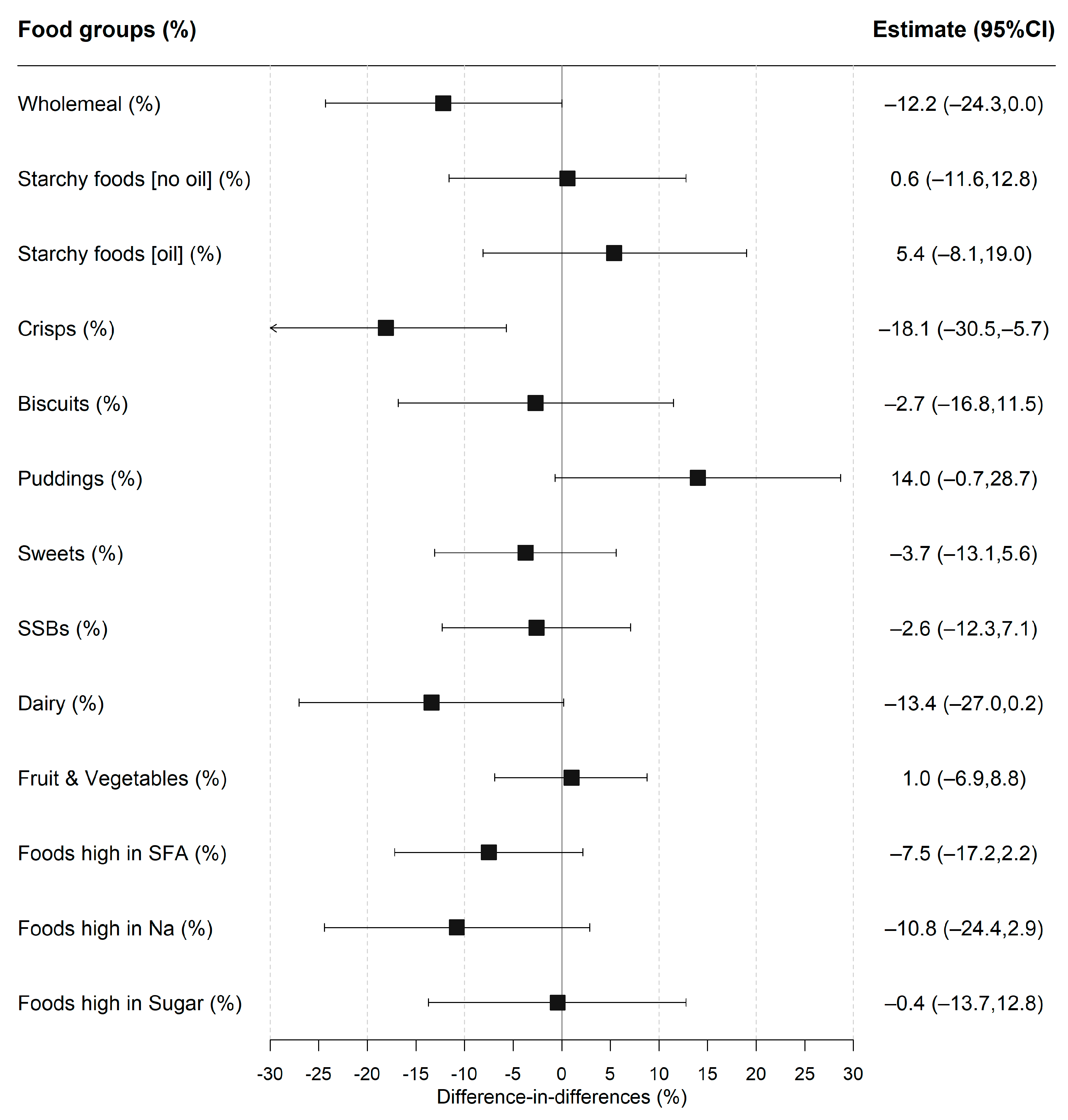
3.1. Policy Impact on Lunchtime Food Consumption Patterns
3.2. Policy Impact on Lunchtime Nutrient Intakes
3.3. Sensitivity Analyses
3.4. Policy Impact on Daily Nutrient Intakes
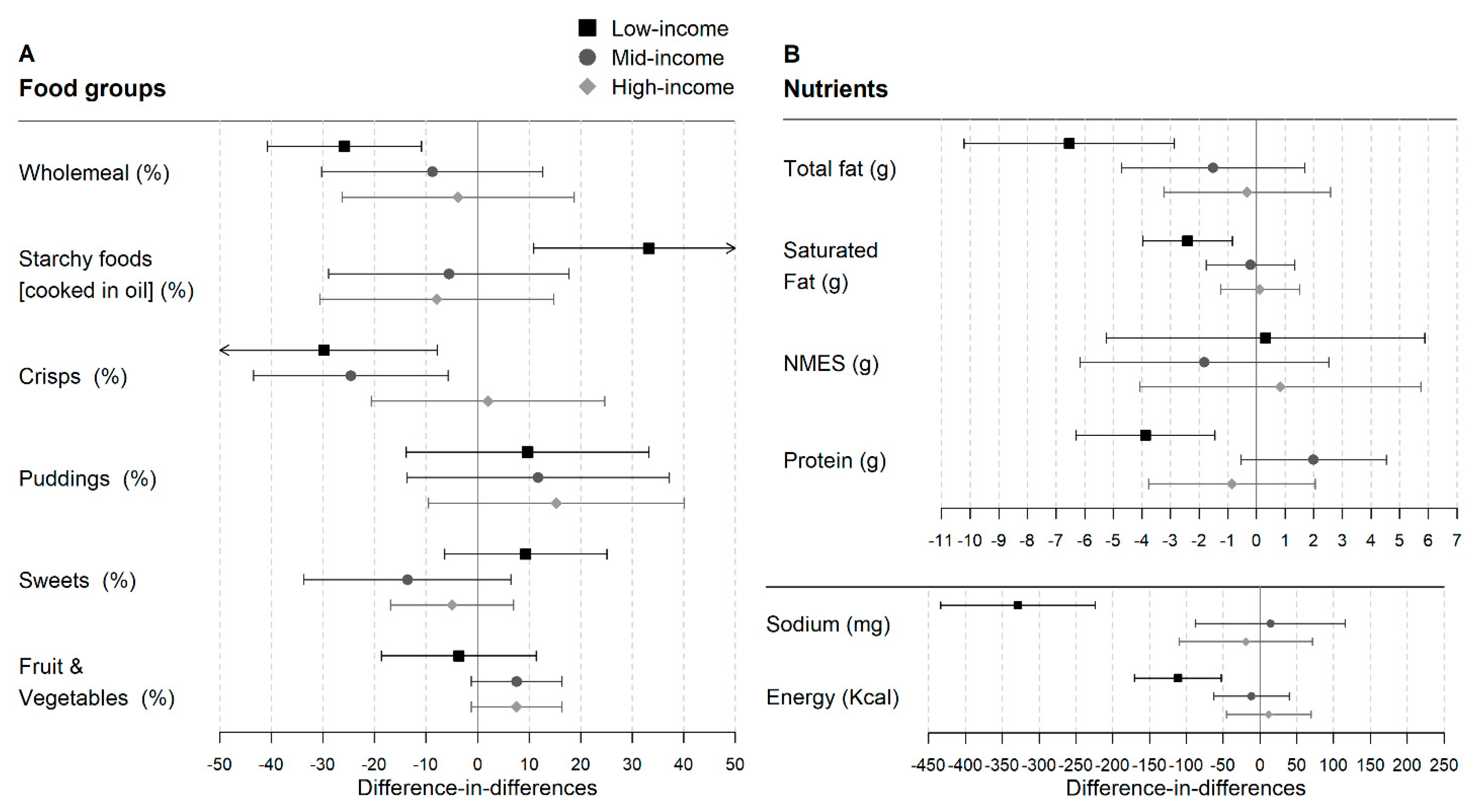
3.5. Differences between Income Groups
4. Discussion
4.1. Summary of Main Findings
4.2. Relationship to Previous Research
4.3. Strengths and Limitations
4.4. Implications for Policy and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Harrison, F.; Jennings, A.; Jones, A.; Welch, A.; van Sluijs, E.; Griffin, S.; Cassidy, A. Food and drink consumption at school lunchtime: The impact of lunch type and contribution to overall intake in British 9–10-year-old children. Public Health Nutr. 2013, 16, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.L.L.; Cleghorn, C.L.; Greenwood, D.C.; Cade, J.E. A comparison of British school meals and packed lunches from 1990 to 2007: Meta-analysis by lunch type. Br. J. Nutr. 2010, 104, 474–487. [Google Scholar] [CrossRef] [PubMed]
- Wyness, L.; Norris, C.; Clapham, M.; Davidson, I.; Wyness, L. School Meal Contribution to Nutrient Intake amongst 11–14 Years Old Scottish School Children. EC Nutr. 2016, 4, 836–844. [Google Scholar]
- Stevens, L.; Nelson, M. The contribution of school meals and packed lunch to food consumption and nutrient intakes in UK primary school children from a low income population. J. Hum. Nutr. Diet. 2011, 24, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Pearce, J.; Wood, L.; Nelson, M. Lunchtime food and nutrient intakes of secondary-school pupils; a comparison of school lunches and packed lunches following the introduction of mandatory food-based standards for school lunch. Public Health Nutr. 2013, 16, 1126–1131. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Evans, C.E.L.; Mandl, V.; Christian, M.S.; Cade, J.E. Impact of school lunch type on nutritional quality of English children’s diets. Public Health Nutr. 2016, 19, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Spence, S.; Matthews, J.N.S.; White, M.; Adamson, A.J. A repeat cross-sectional study examining the equitable impact of nutritional standards for school lunches in England in 2008 on the diets of 4-7y olds across the socio-economic spectrum. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 128. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.L.; Melia, K.E.; Rippin, H.L.; Hancock, N.; Cade, J. A repeated cross-sectional survey assessing changes in diet and nutrient quality of English primary school children’s packed lunches between 2006 and 2016. BMJ Open 2020, 10, e029688. [Google Scholar] [CrossRef] [PubMed]
- Holford, A.; Rabe, B. Going Universal-The Impact of Free School Lunches on Child Body Weight Outcomes; University of Essex: Colchester, UK, 2020. [Google Scholar]
- Taher, A.K.; Ensaff, H.; Evans, C.E.L. Cross-sectional associations between lunch-type consumed on a school day and British adolescents’ overall diet quality. Prev. Med. Rep. 2020, 19, 101133. [Google Scholar] [CrossRef] [PubMed]
- Craigie, A.M.; Lake, A.A.; Kelly, S.A.; Adamson, A.J.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef]
- Department of Education Schools, Pupils and Their Characteristics: January 2020. Available online: https://www.gov.uk/government/statistics/schools-pupils-and-their-characteristics-january-2020 (accessed on 9 May 2021).
- Office of National Statisitcs Households below Average Income: For Financial Years Ending 1995 to 2020. Available online: https://www.gov.uk/government/statistics/households-below-average-income-for-financial-years-ending-1995-to-2020 (accessed on 22 April 2021).
- Anstey, K. Expanding Eligibility for Free School Meals in England. Available online: https://cpag.org.uk/sites/default/files/files/policypost/CPAG-FSM-briefing-2020.pdf (accessed on 18 March 2021).
- Sellen, P.; Huda, N.; Gibson, S.; Oliver, L.L.; Huda, Z.; Gibson, S.; Oliver, L.L. Evaluation of Universal Infant Free School Meals; Education Policy Institue: London, UK, 2018. [Google Scholar]
- Kitchen, S.; Tanner, E.; Brown, V.; Natcen, C.P.; Crawford, C.; Dearden, L. Evaluation of the Free School Meals Pilot Impact Report; The Institute for Fiscal Studies: London, UK, 2012. [Google Scholar]
- Spence, S.; Matthews, J.N.S.; McSweeney, L.; Rowland, M.K.; Orango, P.; Adamson, A.J. Implementation of Universal Infant Free School Meals: A pilot study in NE England exploring the impact on Key Stage 1 pupil’s dietary intake. Public Health Nutr. 2020, 24, 3167–3175. [Google Scholar] [CrossRef]
- de Vocht, F.; Katikireddi, S.V.; McQuire, C.; Tilling, K.; Hickman, M.; Craig, P. Conceptualising natural and quasi experiments in public health. BMC Med. Res. Methodol. 2021, 21, 32. [Google Scholar] [CrossRef] [PubMed]
- NatCen Social Research. MRC Elsie Widdowson Laboratory National Diet and Nutrition Survey Years 1–9, 2008/09–2016/17; NatCen Social Research: London, UK, 2019. [Google Scholar]
- Public Health England; Food Standards Agency. Public Health England Appendix B Methodology for Years 10 and 11 of the NDNS RP. In National Diet and Nutrition Survey. Years 9 to 11 of the Rolling Programme (2016/2017–2018/2019); Food Standards Agency: London, UK, 2020. [Google Scholar]
- Department of Health and Social Care. Food Standards Agency Guide to Creating a Front of Pack (FoP) Nutrition Label for Pre-Packed Products Sold through Retail Outlets; Department of Health and Social Care: London, UK, 2016.
- Ministry of Housing, Communities & Local Government English Indices of Deprivation 2019. Available online: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed on 19 February 2021).
- van Buuren, S. Classification and regression trees. In Flexible Imputation of Missing Data; Chapman & Hall/CRC: London, UK, 2018. [Google Scholar]
- McCaffrey, D.F.; Griffin, B.A.; Almirall, D.; Slaughter, M.E.; Ramchand, R.; Burgette, L.F. A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat. Med. 2013, 32, 3388–3414. [Google Scholar] [CrossRef] [PubMed]
- Black, A.E. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int. J. Obes. 2000, 24, 1119–1130. [Google Scholar] [CrossRef]
- Börnhorst, C.; Huybrechts, I.; Hebestreit, A.; Vanaelst, B.; Molnár, D.; Bel-Serrat, S.; Mouratidou, T.; Moreno, L.A.; Pala, V.; Eha, M.; et al. Diet–obesity associations in children: Approaches to counteract attenuation caused by misreporting. Public Health Nutr. 2013, 16, 256–266. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Welsh Government. Welsh Government Healthy Eating in Maintained Schools Statutory Guidance for Local Authorities and Governing Bodies; Welsh Government: Cardiff, UK, 2014.
- Public Health England. Government Dietary Recommendations; Public Health England: London, UK, 2016.
- Holford, A. Take-up of Free School Meals: Price Effects and Peer Effects. Economica 2015, 82, 976–993. [Google Scholar] [CrossRef]
- McNeil, C.; Parkes, H.; Garthwaite, K.; Patrick, R. No Longer “Managing”: The Rise of Working Poverty and Fixing Britain’s Broken Social Settlemen. Available online: https://www.ippr.org/research/publications/no-longer-managing-the-rise-of-working-poverty-and-fixing-britain-s-broken-social-settlement (accessed on 7 January 2021).
- Dimbleby, H.; Vincent, J. The School Food Plan. Available online: https://www.schoolfoodmatters.org/campaigns/school-food-plan (accessed on 24 March 2021).
- Cohen, J.F.W.; Hecht, A.A.; McLoughlin, G.M.; Turner, L.; Schwartz, M.B. Universal School Meals and Associations with Student Participation, Attendance, Academic Performance, Diet Quality, Food Security, and Body Mass Index: A Systematic Review. Nutrients 2021, 13, 911. [Google Scholar] [CrossRef] [PubMed]
- USDA. Community Eligibility Provision. Available online: https://www.fns.usda.gov/cn/community-eligibility-provision (accessed on 3 January 2022).
- Pokorney, P.E.; Chandran, A.; Long, M.W. Impact of the Community Eligibility Provision on meal counts and participation in Pennsylvania and Maryland National School Lunch Programs. Public Health Nutr. 2019, 22, 3281–3287. [Google Scholar] [CrossRef] [PubMed]
- Schneider, K.R.; Oslund, J.; Liu, T. Impact of the community eligibility provision program on school meal participation in Texas. Public Health Nutr. 2021, 24, 6534–6542. [Google Scholar] [CrossRef] [PubMed]
- Chambers, S.; Boydell, N.; Ford, A.; Eadie, D. Learning from the implementation of Universal Free School Meals in Scotland using Normalisation Process Theory: Lessons for policymakers to engage multiple stakeholders. Food Policy 2020, 95, 101936. [Google Scholar] [CrossRef] [PubMed]
- Food for Life. State of the Nation: Children’s Food in England, 2019; Food for Life: Bristol, UK, 2019. [Google Scholar]
- Guy’s and St Thomas’ Charity. Cookwise Serving up Children’s Health; Guy’s & St Thomas’ Foundation: London, UK, 2020. [Google Scholar]


| Pre-UIFSM (2010–2014) 1 | Post-UIFSM (2014–2017) | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Intervention Group: Infants (n = 281) | Control Group: Juniors (n = 239) | p Value 2 | Intervention Group: Infants (n = 172) | Control Group: Juniors (n = 162) | p Value 3 | |
| Age | Mean (SD) | 5.6 (1.0) | 9.1 (1.0) | <0.001 b | 5.7 (1.0) | 9.4 (1.0) | <0.001 b |
| Sex | n (%) | 0.28 a | 0.45 a | ||||
| Female | 137 (49.9) | 107 (44.3) | 88 (50.0) | 72 (45.4) | |||
| Ethnicity | n (%) | 0.98 a | 0.70 a | ||||
| Ethnic minorities | 52 (20.2) | 43 (20.1) | 30 (20.0) | 27 (18.1) | |||
| Household income (£) | Mean (SD) | 30,648.3 (19,539.5) | 26,601.9 (18,800.4) | 0.03 b | 31,479.6 (20,798.4) | 28,976.4 (18,465.9) | 0.28 a |
| IMD (quintiles) | n (%) | 0.07 a | 0.44 a | ||||
| Least deprived | 62 (19.1) | 42 (19.4) | 40 (20.8) | 42 (27.6) | |||
| 2 | 49 (17.4) | 41 (14.9) | 29 (17.7) | 29 (18.3) | |||
| 3 | 60 (23.2) | 44 (16.5) | 33 (21.0) | 27 (13.5) | |||
| 4 | 64 (24.0) | 52 (21.2) | 34 (19.1) | 32 (20.9) | |||
| Most deprived | 46 (16.3) | 60 (28.1) | 36 (21.4) | 32 (19.7) | |||
| Region | n (%) | 0.03 a | 0.16 a | ||||
| England: North | 57 (21.9) | 62 (31.3) | 44 (24.0) | 37 (20.5) | |||
| England: Central | 44 (13.4) | 42 (17.8) | 28 (16.7) | 25 (14.1) | |||
| England: South | 126 (55.3) | 83 (40.9) | 87 (51.8) | 77 (49.1) | |||
| Scotland | 54 (9.5) | 52 (10.0) | 13 (7.6) | 23 (16.3) | |||
| School lunch type | n (%) | 0.68 a | <0.001 a | ||||
| School meal | 139 (47.4) | 121 (49.6) | 141 (80.5) | 78 (48.8) | |||
| Packed lunch | 142 (52.6) | 118 (50.4) | 31 (19.5) | 84 (51.2) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parnham, J.C.; Chang, K.; Millett, C.; Laverty, A.A.; von Hinke, S.; Pearson-Stuttard, J.; de Vocht, F.; White, M.; Vamos, E.P. The Impact of the Universal Infant Free School Meal Policy on Dietary Quality in English and Scottish Primary School Children: Evaluation of a Natural Experiment. Nutrients 2022, 14, 1602. https://doi.org/10.3390/nu14081602
Parnham JC, Chang K, Millett C, Laverty AA, von Hinke S, Pearson-Stuttard J, de Vocht F, White M, Vamos EP. The Impact of the Universal Infant Free School Meal Policy on Dietary Quality in English and Scottish Primary School Children: Evaluation of a Natural Experiment. Nutrients. 2022; 14(8):1602. https://doi.org/10.3390/nu14081602
Chicago/Turabian StyleParnham, Jennie C., Kiara Chang, Christopher Millett, Anthony A. Laverty, Stephanie von Hinke, Jonathan Pearson-Stuttard, Frank de Vocht, Martin White, and Eszter P. Vamos. 2022. "The Impact of the Universal Infant Free School Meal Policy on Dietary Quality in English and Scottish Primary School Children: Evaluation of a Natural Experiment" Nutrients 14, no. 8: 1602. https://doi.org/10.3390/nu14081602
APA StyleParnham, J. C., Chang, K., Millett, C., Laverty, A. A., von Hinke, S., Pearson-Stuttard, J., de Vocht, F., White, M., & Vamos, E. P. (2022). The Impact of the Universal Infant Free School Meal Policy on Dietary Quality in English and Scottish Primary School Children: Evaluation of a Natural Experiment. Nutrients, 14(8), 1602. https://doi.org/10.3390/nu14081602






