A Pilot Study on the Prevalence of Micronutrient Imbalances in a Dutch General Population Cohort and the Effects of a Digital Lifestyle Program
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Measurements of Vitamins, Minerals, and Other Blood Biomarkers
2.3. Food Group and Supplement Consumption
2.4. Digital Lifestyle Program
2.5. Statistical Analysis
3. Results
3.1. Vitamin and Mineral Status
3.1.1. B Vitamins
3.1.2. Vitamin D
3.1.3. Iron Status
3.2. Consumption of Major Food Groups and Supplements
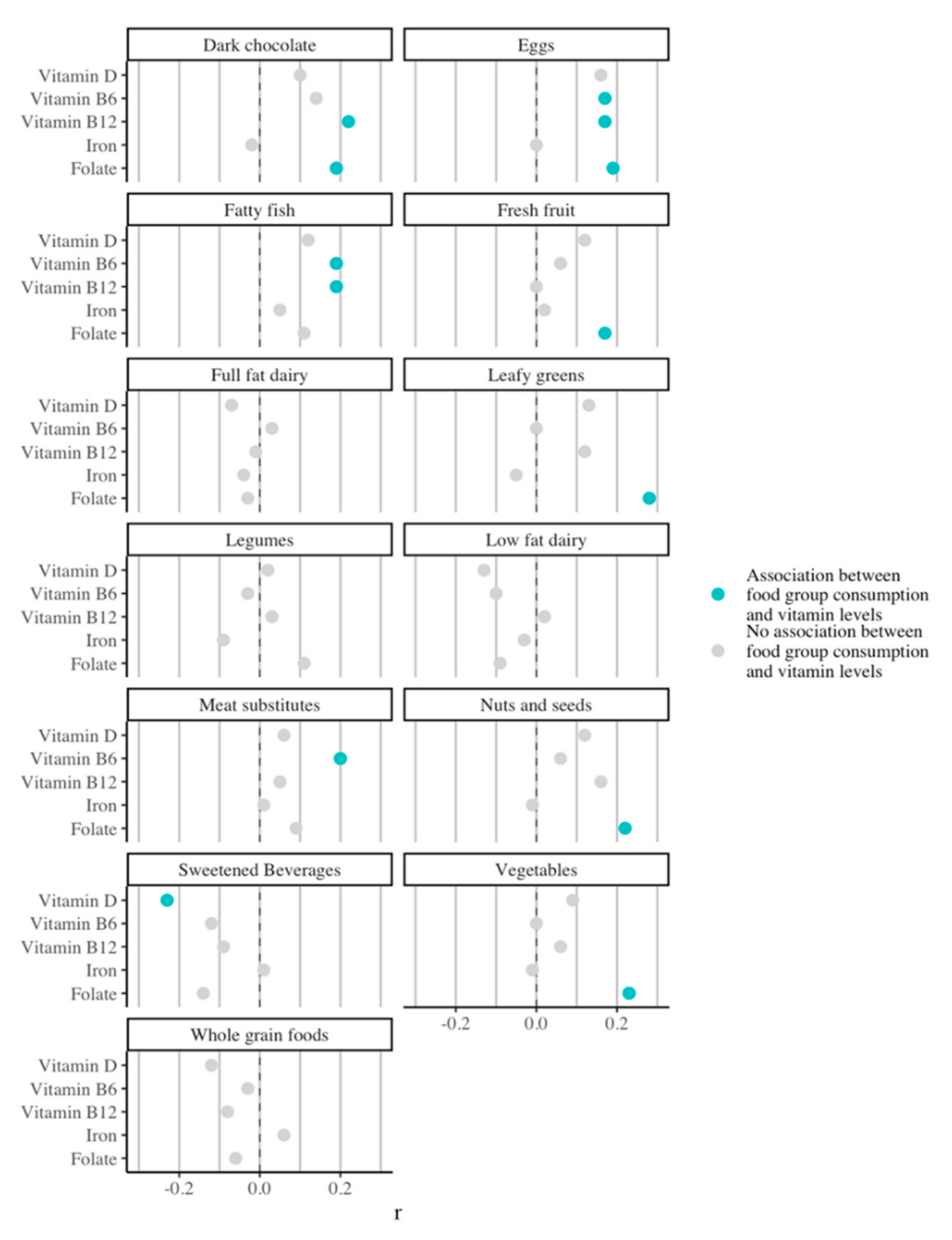
3.3. Impact of Food Group Consumption on Vitamin and Mineral Status
3.4. Effect of a Digital Lifestyle Intervention on Nutrient Status and Food Group Consumption
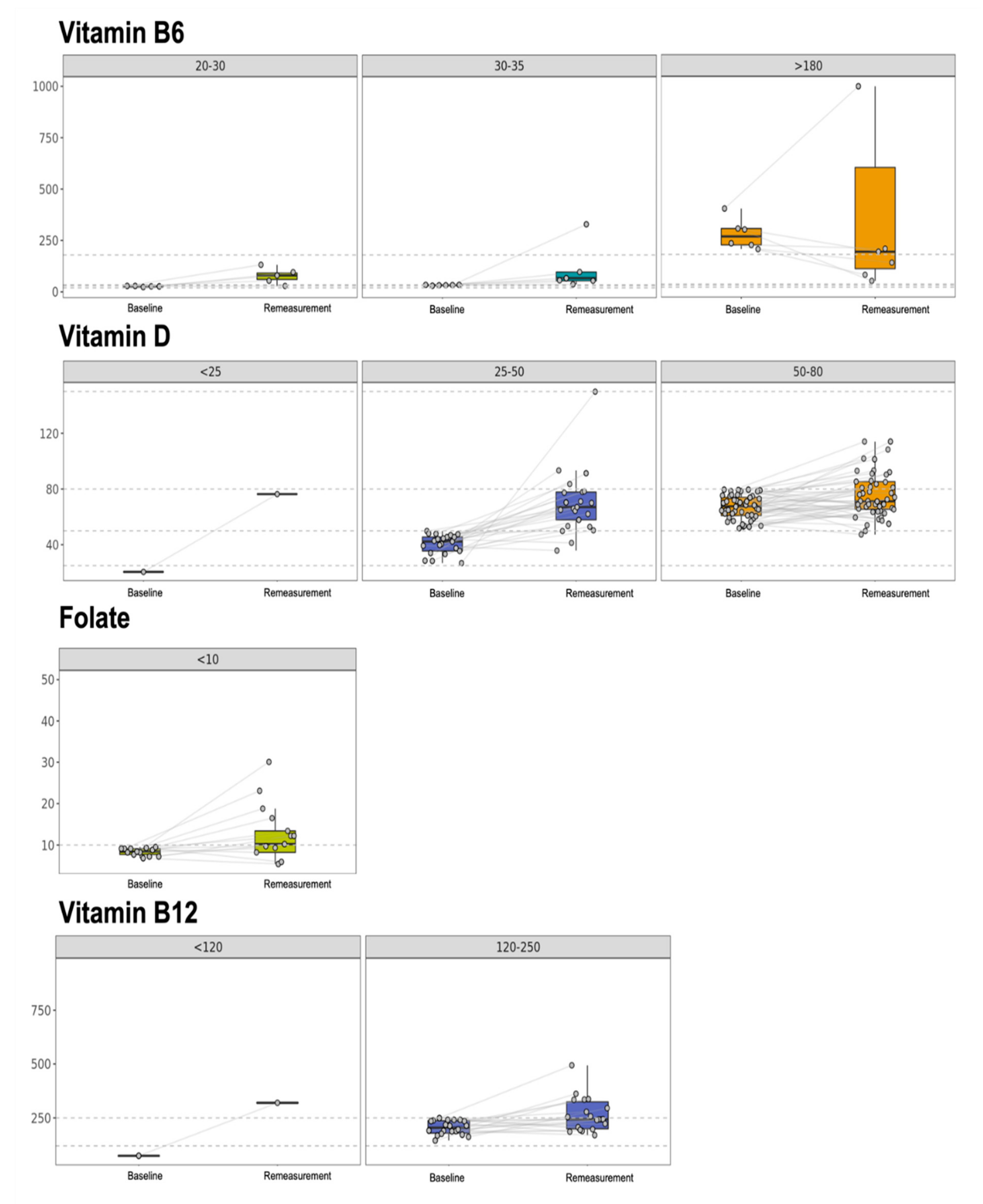
3.4.1. B Vitamins
3.4.2. Vitamin D
3.4.3. Iron Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Food Group | Lower Threshold (Portions) | Upper Threshold (Portions) |
|---|---|---|
| Shellfish | 1 per week | 3–6 per week |
| Vegetables | 3 per day | No upper limit |
| Legumes | 1 per day | No upper limit |
| Nuts and seeds | 1 per day | 2 per day |
| Soy * | 2 per week | 3 per day |
| Lean fish | 1 per week | 6 per week |
| Meat substitutes * | 1 per day | 6 per week |
| Whole grain foods | 2 per day | 4 per day |
| Low-fat dairy | 1 per day | 2 per day |
| Fresh fruit | 2 per day | 3 per day |
| Leafy greens | 1 per day | No upper limit |
| Herbs and spices | 1 per day | No upper limit |
| Coffee and tea | No lower limit | 3 per day |
| Fatty fish | 1 per week | 6 per week |
| Dark chocolate | No lower limit | 1 per day |
| Sweets | No lower limit | 3–6 per week |
| Sweetened beverages | No lower limit | 1–2 per week |
| Calorie-rich spreads | No lower limit | 3–6 per week |
| Red meat | No lower limit | 1–2 per week |
| Poultry | 1 per week | 3–6 per week |
| Take-out/fast food | No lower limit | <1 per week |
| Eggs | 2 per week | 1 per day |
| Full-fat dairy | No lower limit | 3–6 per week |
| Refined grains | No lower limit | 3–6 per week |
| Oils rich in saturated fat | No lower limit | 1 per day |
| Processed meat | No lower limit | 1–2 per week |
| Oils rich in unsaturated fat | No lower limit | 3 per day |
| (Added) salt | No lower limit | 1 per day |
| Water | 6 glasses per day | No upper limit |
Appendix B
References
- Trijsburg, L.; Talsma, E.F.; Crispim, S.P.; Garrett, J.; Kennedy, G.; de Vries, J.H.M.; Brouwer, I.D. Method for the Development of WISH, a Globally Applicable Index for Healthy Diets from Sustainable Food Systems. Nutrients 2021, 13, 93. [Google Scholar] [CrossRef]
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Schoufour, J.; Wang, D.D.; Dhana, K.; Pan, A.; Liu, X.; Hu, F.B. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: Prospective cohort study. BMJ 2020, 368, l6669. [Google Scholar] [CrossRef] [Green Version]
- Fairfield, K.M.; Fletcher, R.H. Vitamins for Chronic Disease Prevention in Adults: Scientific Review. JAMA 2002, 287, 3116–3126. [Google Scholar] [CrossRef]
- Kearney, J. Food consumption trends and drivers. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2010, 365, 2793–2807. [Google Scholar] [CrossRef]
- Lotto, V.; Choi, S.-W.; Friso, S. Vitamin B6: A challenging link between nutrition and inflammation in CVD. Br. J. Nutr. 2011, 106, 183–195. [Google Scholar] [CrossRef] [Green Version]
- Gylling, B.; Myte, R.; Schneede, J.; Hallmans, G.; Häggström, J.; Johansson, I.; Ulvik, A.; Ueland, P.M.; Van Guelpen, B.; Palmqvist, R. Vitamin B-6 and colorectal cancer risk: A prospective population-based study using 3 distinct plasma markers of vitamin B-6 status. Am. J. Clin. Nutr. 2017, 105, 897–904. [Google Scholar] [CrossRef]
- Wang, H.; Chen, W.; Li, D.; Yin, X.; Zhang, X.; Olsen, N.; Zheng, S.G. Vitamin D and Chronic Diseases. Aging Dis. 2017, 8, 346–353. [Google Scholar] [CrossRef] [Green Version]
- Kaur, J.; Ferguson, S.L.; Freitas, E.; Miller, R.; Bemben, D.; Knehans, A.; Bemben, M. Association of Vitamin D Status with Chronic Disease Risk Factors and Cognitive Dysfunction in 50–70 Year Old Adults. Nutrients 2019, 11, 141. [Google Scholar] [CrossRef] [Green Version]
- Brachet, P.; Chanson, A.; Demigné, C.; Batifoulier, F.; Alexandre-Gouabau, M.-C.; Tyssandier, V.; Rock, E. Age-associated B vitamin deficiency as a determinant of chronic diseases. Nutr. Res. Rev. 2004, 17, 55–68. [Google Scholar] [CrossRef] [Green Version]
- Hiraoka, M.; Kagawa, Y. Genetic polymorphisms and folate status. Congenit. Anomalies 2017, 57, 142–149. [Google Scholar] [CrossRef] [Green Version]
- Surendran, S.; Adaikalakoteswari, A.; Saravanan, P.; Shatwaan, I.A.; Lovegrove, J.A.; Vimaleswaran, K.S. An update on vitamin B12-related gene polymorphisms and B12 status. Genes Nutr. 2018, 13, 2. [Google Scholar] [CrossRef] [Green Version]
- Krasniqi, E.; Boshnjaku, A.; Wagner, K.H.; Wessner, B. Association between Polymorphisms in Vitamin D Pathway-Related Genes, Vitamin D Status, Muscle Mass and Function: A Systematic Review. Nutrients 2021, 13, 3109. [Google Scholar] [CrossRef]
- Hillman, R.S.; Steinberg, S.E. The Effects of Alcohol on Folate Metabolism. Annu. Rev. Med. 1982, 33, 345–354. [Google Scholar] [CrossRef]
- Tulchinsky, T.H. Micronutrient Deficiency Conditions: Global Health Issues. Public Health. Rev. 2010, 32, 243–255. [Google Scholar] [CrossRef] [Green Version]
- Johnson, M.A. If High Folic Acid Aggravates Vitamin B12 Deficiency What Should Be Done About It? Nutr. Rev. 2008, 65, 451–458. [Google Scholar] [CrossRef]
- Malouf, R.; Evans, J.G. Folic acid with or without vitamin B12 for the prevention and treatment of healthy elderly and demented people. Cochrane Database Syst. Rev. 2008, 4, CD004514. [Google Scholar] [CrossRef]
- Nielsen, J.B.; Leppin, A.; Gyrd-Hansen, D.E.; Jarbøl, D.E.; Søndergaard, J.; Larsen, P.V. Barriers to lifestyle changes for prevention of cardiovascular disease—A survey among 40–60-year old Danes. BMC Cardiovasc. Disord. 2017, 17, 245. [Google Scholar] [CrossRef] [Green Version]
- Thomas, K.; Krevers, B.; Bendtsen, P. Implementing healthy lifestyle promotion in primary care: A quasi-experimental cross-sectional study evaluating a team initiative. BMC Health Serv. Res. 2015, 15, 31. [Google Scholar] [CrossRef] [Green Version]
- Berry, L.L.; Flynn, A.G.; Seiders, K.; Haws, K.L.; Quach, S.Q. Physician Counseling of Overweight Patients About Preventive Health Behaviors. Am. J. Prev. Med. 2014, 46, 297–302. [Google Scholar] [CrossRef]
- DiFilippo, K.N.; Huang, W.-H.; Andrade, J.E.; Chapman-Novakofski, K.M. The use of mobile apps to improve nutrition outcomes: A systematic literature review. J. Telemed. Telecare 2015, 21, 243–253. [Google Scholar] [CrossRef] [PubMed]
- Paramastri, R.; Pratama, S.A.; Ho, D.K.N.; Purnamasari, S.D.; Mohammed, A.Z.; Galvin, C.J.; Hsu, Y.-H.E.; Tanweer, A.; Humayun, A.; Househ, M.; et al. Use of mobile applications to improve nutrition behaviour: A systematic review. Comput. Methods Programs Biomed. 2020, 192, 105459. [Google Scholar] [CrossRef] [PubMed]
- Fallaize, R.; Franco, R.Z.; Pasang, J.; Hwang, F.; A Lovegrove, J. Popular Nutrition-Related Mobile Apps: An Agreement Assessment Against a UK Reference Method. JMIR mHealth uHealth 2019, 7, e9838. [Google Scholar] [CrossRef]
- Kane, S.F.; Roberts, C.; Paulus, R. Hereditary Hemochromatosis: Rapid Evidence Review. Am. Fam. Physician 2021, 104, 263–270. [Google Scholar]
- Brink, E.; van Rossum, C.; Postma-Smeets, A.; Stafleu, A.; Wolvers, D.; van Dooren, C.; Toxopeus, I.; Buurma-Rethans, E.; Geurts, M.; Ocké, M. Development of healthy and sustainable food-based dietary guidelines for the Netherlands. Public Health. Nutr. 2019, 22, 2419–2435. [Google Scholar] [CrossRef] [Green Version]
- Fogg, B.J.J. A behavior model for persuasive design. Proceeding Persuasive ’09. In Proceedings of the 4th International Conference on Persuasive Technology, Claremont, CA, USA, 26–29 April 2009; Volume 40, pp. 1–7. [Google Scholar] [CrossRef]
- Van Oostrom, S.H.; Gijsen, R.; Stirbu, I.; Korevaar, J.C.; Schellevis, F.G.; Picavet, H.S.J.; Hoeymans, N. Time Trends in Prevalence of Chronic Diseases and Multimorbidity Not Only due to Aging: Data from General Practices and Health Surveys. PLoS ONE 2016, 11, e0160264. [Google Scholar] [CrossRef] [Green Version]
- Tynes, M.; Hepprich, M.; Timper, K. Regular intake of energy drinks and multivitamin supplements is associated with elevated plasma vitamin B6 levels in post-bariatric patients. Sci. Rep. 2021, 11, 17830. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products Nutrition and Allergies; Turck, D.; Bresson, J.-L.; Burlingame, B.; Dean, T.; Fairweather-Tait, S.; Neuhäuser-Berthold, M. Dietary reference values for vitamin B6. EFSA J. 2016, 14, e04485. [Google Scholar] [CrossRef]
- Institute of Medicine. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; The National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Mensink, G.B.M.; Fletcher, R.; Gurinović, M.; Huybrechts, I.; Lafay, L.; Serra-Majem, L.; Szponar, L.; Tetens, I.; Verkaik-Kloosterman, J.; Baka, A.; et al. Mapping low intake of micronutrients across Europe. Br. J. Nutr. 2013, 110, 755–773. [Google Scholar] [CrossRef] [Green Version]
- Borst, L.C.C.; Duk, M.J.; Tromp, E.A.M.; Hoevenaar-Blom, M.; Wielders, J.P.M. Vitamin D supplementation according to guidelines may be insufficient to correct preexisting deficiency in pregnancy. Ned Tijdschr Klin Chem Labgeneesk 2017, 42, 82–88. [Google Scholar]
- Govers, E. Should healthy people take a vitamin D supplement in winter months? BMJ 2016, 355, i6183. [Google Scholar] [CrossRef] [Green Version]
- Safiri, S.; Kolahi, A.-A.; Noori, M.; Nejadghaderi, S.A.; Karamzad, N.; Bragazzi, N.L.; Sullman, M.J.M.; Abdollahi, M.; Collins, G.S.; Kaufman, J.S.; et al. Burden of anemia and its underlying causes in 204 countries and territories, 1990–2019: Results from the Global Burden of Disease Study 2019. J. Hematol. Oncol. 2021, 14, 185. [Google Scholar] [CrossRef] [PubMed]
- Adams, P.C.; Reboussin, D.M.; Barton, J.; McLaren, C.E.; Eckfeldt, J.H.; McLaren, G.D.; Dawkins, F.W.; Acton, R.T.; Harris, E.L.; Gordeuk, V.R.; et al. Hemochromatosis and Iron-Overload Screening in a Racially Diverse Population. N. Engl. J. Med. 2005, 352, 1769–1778. [Google Scholar] [CrossRef] [Green Version]
- Bozzini, C.; Girelli, D.; Olivieri, O.; Martinelli, N.; Bassi, A.; De Matteis, G.; Tenuti, I.; Lotto, V.; Friso, S.; Pizzolo, F.; et al. Prevalence of Body Iron Excess in the Metabolic Syndrome. Diabetes Care 2005, 28, 2061–2063. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sachinidis, A.; Doumas, M.; Imprialos, K.; Stavropoulos, K.; Katsimardou, A.; Athyros, V.G. Dysmetabolic Iron Overload in Metabolic Syndrome. Curr. Pharm. Des. 2020, 26, 1019–1024. [Google Scholar] [CrossRef]
- Laine, F.; Ruivard, M.; Loustaud-Ratti, V.; Bonnet, F.; Calès, P.; Bardou-Jacquet, E.; Sacher-Huvelin, S.; Causse, X.; Beusnel, C.; Renault, A.; et al. Metabolic and hepatic effects of bloodletting in dysmetabolic iron overload syndrome: A randomized controlled study in 274 patients. Hepatology 2017, 65, 465–474. [Google Scholar] [CrossRef]
- Anderson, G.J.; Bardou-Jacquet, E. Revisiting hemochromatosis: Genetic vs. phenotypic manifestations. Ann. Transl. Med. 2021, 9, 731. [Google Scholar] [CrossRef]
- Hess, J.M.; Cifelli, C.J.; Agarwal, S.; Fulgoni, V.L. Comparing the cost of essential nutrients from different food sources in the American diet using NHANES 2011–2014. Nutr. J. 2019, 18, 68. [Google Scholar] [CrossRef] [Green Version]
- Elia, M.; Normand, C.; Laviano, A.; Norman, K. A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in community and care home settings. Clin. Nutr. 2016, 35, 125–137. [Google Scholar] [CrossRef] [Green Version]
- Reinert, A.; Rohrmann, S.; Becker, N.; Linseisen, J. Lifestyle and diet in people using dietary supplements. Eur. J. Nutr. 2007, 46, 165–173. [Google Scholar] [CrossRef]
- Chen, F.; Du, M.; Blumberg, J.B.; Chui, K.K.H.; Ruan, M.; Rogers, G.; Shan, Z.; Zeng, L.; Zhang, F.F. Association Among Dietary Supplement Use, Nutrient Intake, and Mortality Among U.S. Adults. Ann. Intern. Med. 2019, 170, 604–613. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force. Screening for Vitamin D Deficiency in Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2021, 325, 1436–1442. [Google Scholar] [CrossRef] [PubMed]
- Bruins, M.J.; Bird, J.K.; Aebischer, C.P.; Eggersdorfer, M. Considerations for Secondary Prevention of Nutritional Deficiencies in High-Risk Groups in High-Income Countries. Nutrients 2018, 10, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferraro, S.; Panzeri, A.; Panteghini, M. Tackling serum folate test in European countries within the health technology assessment paradigm: Request appropriateness, assays and health outcomes. Clin. Chem. Lab. Med. 2017, 55, 1262–1275. [Google Scholar] [CrossRef] [Green Version]
- Wolffenbuttel, B.; Wouters, H.; de Jong, W.; Huls, G.; van der Klauw, M.M. Association of vitamin B12, methylmalonic acid, and functional parameters. Neth. J. Med. 2020, 78, 10–24. [Google Scholar]
- Fleming, T.; Bavin, L.; Lucassen, M.; Stasiak, K.; Hopkins, S.; Merry, S. Beyond the Trial: Systematic Review of Real-World Uptake and Engagement with Digital Self-Help Interventions for Depression, Low Mood, or Anxiety. J. Med. Internet Res. 2018, 20, e199. [Google Scholar] [CrossRef]
- Meyerowitz-Katz, G.; Ravi, S.; Arnolda, L.; Feng, X.; Maberly, G.; Astell-Burt, T. Rates of Attrition and Dropout in App-Based Interventions for Chronic Disease: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, e20283. [Google Scholar] [CrossRef]

| Marker (Unit) | Reference Range |
|---|---|
| Vitamin B6 (nmol/L) | Deficiency: <20 Low: 20–30 Normal: 30–180 High: >180 |
| Folate (nmol/L) | Low: <10 Normal: ≥10 |
| Vitamin B12 (pmol/L) | Deficiency: <120 Low: 120–250 Normal: ≥250 |
| Vitamin D (nmol/L) | Deficiency: <25 Insufficiency: 50–80 Normal: 80–180 Elevated: >180 |
| Iron (µmol/L) | Deficiency: <10 Normal: 10–30 High: ≥30 |
| Hemoglobin (mmol/L) | Men: 8.5–11 Women: 7.5–10 |
| Ferritin (µg/L) | Men: 30–400 Women: 15–150 |
| Transferrin (g/L) | 2.0–3.6 |
| Transferrin saturation (%) | 15–45 |
| Marker or Characteristic | Baseline Status, Total Cohort (n = 348) |
|---|---|
| Demographics | |
| Sex (% female) | 56% |
| Age (years, SD) | 44.6 (11.1) |
| Vitamin B6 | |
| Mean (SD), in nmol/L | 74.5 (59.6) |
| Deficient | 3 (0.9%) |
| Risk of deficiency | 26 (7.5%) |
| Normal | 282 (81%) |
| Excess | 16 (4.6%) |
| Folate | |
| Mean (SD), in nmol/L | 18.9 (9.9) |
| Deficient | 52 (14.9%) |
| Normal | 296 (85.1%) |
| Vitamin B12 | |
| Mean (SD), in pmol/L | 371 (193) |
| Deficient | 2 (0.6%) |
| Insufficient | 80 (23%) |
| Normal | 266 (76.4%) |
| Vitamin D | |
| Mean (SD), in nmol/L | 68 (25) |
| Deficient | 4 (1.1%) |
| Insufficient | 79 (22.7%) |
| Suboptimal | 178 (51.2%) |
| Normal | 84 (24.1%) |
| Excessive | 3 (0.9%) |
| Iron status | |
| Mean iron (SD), in µmol/L | 20.4 (6.9) |
| Iron deficiency anemia | 3 (0.9%) |
| Overt iron deficiency | 14 (4%) |
| Normal iron + low ferritin | 12 (3.4%) |
| Normal iron | 304 (87.4%) |
| Iron overload High iron and ferritin | 3 (0.9%) 30 (8.6%) |
| Isolated high ferritin | 40 (11.5%) |
| Marker | Before Lifestyle Intervention (n) a | After Lifestyle Intervention (n) a | p-Value b |
|---|---|---|---|
| Vitamin B6 | n = 29 | n = 5 | |
| Mean (SD), in mmol/L | 27.2 (2.1) | 78.2 (39.4) | 0.04 |
| Improved | - | 4 (80%) | |
| Normalized | - | 4 (80%) | |
| Folate | n = 52 | n = 12 | |
| Mean (SD), in mmol/L | 8.3 (1.7) | 12.7 (6.8) | 0.05 |
| Improved | - | 8 (67%) | |
| Normalized | - | 7 (58%) | |
| Vitamin B12 | n = 82 | n = 20 | |
| Mean (SD), in mmol/L | 205 (32) | 264 (78) | 0.006 |
| Improved | - | 14 (70%) | |
| Normalized | - | 9 (45%) | |
| Vitamin D | n = 68 | n = 22 | |
| Mean (SD), in mmol/L | 40 (6) | 68 (24) | <0.001 |
| Improved | - | 19 (86.4%) | |
| Normalized | - | 3 (13.6%) | |
| Iron status c | n = 45 | n = 12 | |
| Mean (SD), in mmol/L | 34.6 | 23.2 | <0.001 |
| Improved | - | 10 (83.3%) | |
| Normalized | - | 9 (75%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castela Forte, J.; Gannamani, R.; Folkertsma, P.; Kanthappu, S.; van Dam, S.; Wolffenbuttel, B.H.R. A Pilot Study on the Prevalence of Micronutrient Imbalances in a Dutch General Population Cohort and the Effects of a Digital Lifestyle Program. Nutrients 2022, 14, 1426. https://doi.org/10.3390/nu14071426
Castela Forte J, Gannamani R, Folkertsma P, Kanthappu S, van Dam S, Wolffenbuttel BHR. A Pilot Study on the Prevalence of Micronutrient Imbalances in a Dutch General Population Cohort and the Effects of a Digital Lifestyle Program. Nutrients. 2022; 14(7):1426. https://doi.org/10.3390/nu14071426
Chicago/Turabian StyleCastela Forte, José, Rahul Gannamani, Pytrik Folkertsma, Saro Kanthappu, Sipko van Dam, and Bruce H. R. Wolffenbuttel. 2022. "A Pilot Study on the Prevalence of Micronutrient Imbalances in a Dutch General Population Cohort and the Effects of a Digital Lifestyle Program" Nutrients 14, no. 7: 1426. https://doi.org/10.3390/nu14071426
APA StyleCastela Forte, J., Gannamani, R., Folkertsma, P., Kanthappu, S., van Dam, S., & Wolffenbuttel, B. H. R. (2022). A Pilot Study on the Prevalence of Micronutrient Imbalances in a Dutch General Population Cohort and the Effects of a Digital Lifestyle Program. Nutrients, 14(7), 1426. https://doi.org/10.3390/nu14071426






