The Individual Nutrition Education Needs among Patients with Type 2 Diabetes at the Public Health Centers in Padang, Indonesia: A Cross-Sectional Study
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
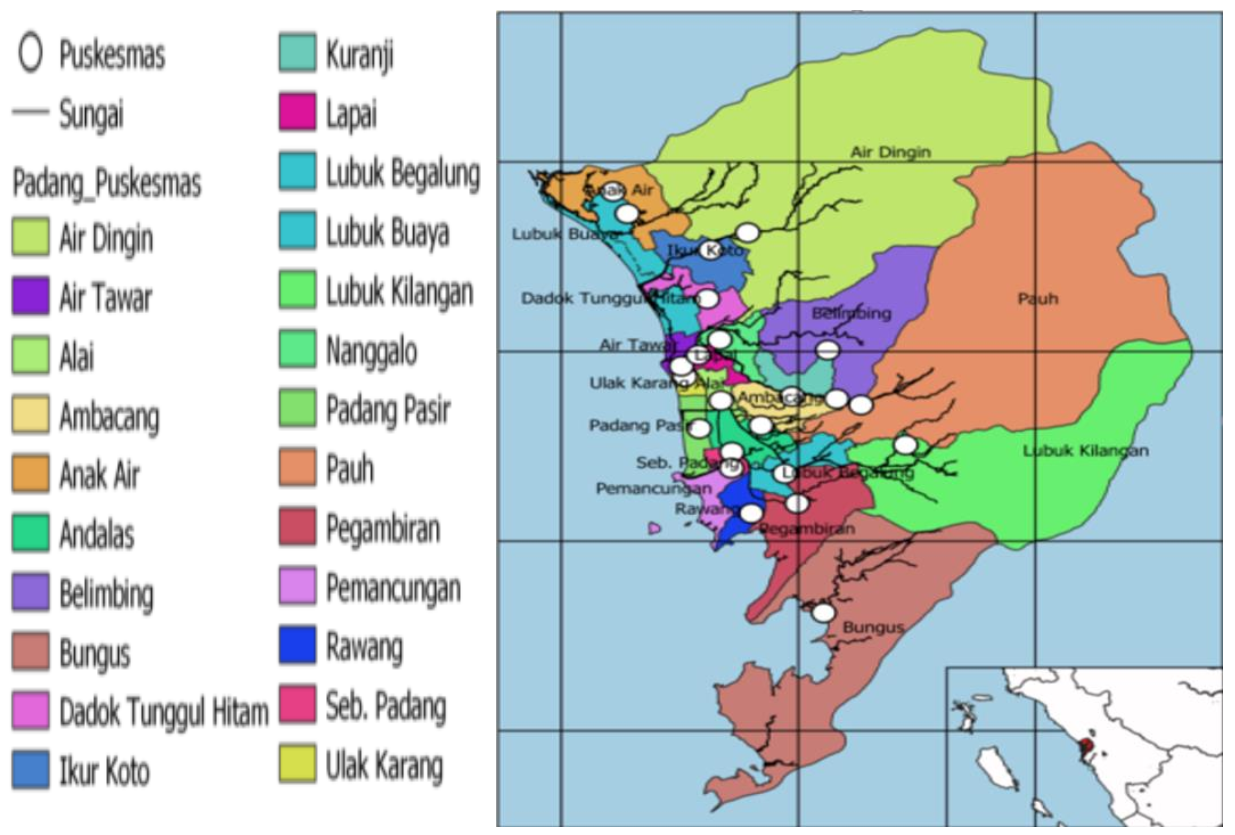
2.2. Respondents, Sampling and Study Location
2.3. Study Site and Sampling Procedure
2.4. Questionnaires
2.5. Data Analyses
3. Results
| Nutritionists Practices Component | n | % |
|---|---|---|
| Attendance | ||
| 134 45 | 74.9 25.1 |
| Frequency | ||
| 107 7 20 | 59.8 3.9 11.1 |
| Duration | ||
| 108 26 | 60.3 14.5 |
| Main provider | ||
| 103 89 20 | 57.5 49.7 11.2 |
| General understanding towards education sessions | ||
| 131 3 | 73.2 1.7 |
| Satisfaction of education session | ||
| 117 18 | 65.4 10.1 |
| Nutrition education materials | ||
| 84 43 37 14 4 | 46.9 24.0 21.0 7.8 2.3 |
| Satisfaction towards the tool kits | ||
| 112 22 | 62.6 12.3 |
| Recommended toolkits | ||
| 36 26 18 11 | 20.4 14.2 10.1 6.1 |
| Coverage of nutrition education topics | ||
| 51 48 47 41 37 37 33 25 19 17 17 14 9 8 6 6 4 2 1 1 | 28.5 26.8 26.3 22.9 20.7 20.7 19.8 14.0 10.6 9.5 9.5 7.8 5.0 4.5 3.4 3.4 2.2 1.2 0.6 0.6 |
| Common nutrition assessments | ||
| 131 114 116 103 64 55 | 73.2 63.7 64.8 57.5 35.8 30.7 |
| Perception of patients who did not routinely attend individual nutrition education | ||
| 19 15 6 3 1 1 | 42.3 33.3 13.3 6.7 2.2 2.2 |
| Items | n | % |
|---|---|---|
| The need for individual nutrition education | ||
| 159 19 | 88.8 10.6 |
| Perception that individual nutrition education is not needed (n = 179) | ||
| 12 4 2 | 7.2 2.3 1.1 |
| Common questions asked during education sessions | ||
| 45 10 10 9 9 9 7 4 2 2 12 | 25.1 5.6 5.6 5.0 5.0 5.0 3.9 2.3 1.1 1.1 7.2 |
| Respondents who actively participated during an education session | ||
| 118 61 | 66.0 34.0 |
| Able to follow the education | ||
| 148 31 | 82.7 17.3 |
| Perception of reasons for not following the education | ||
| 20 4 2 1 1 | 11.1 2.3 1.1 0.6 0.6 |
| Recommended topics | ||
| 45 20 23 1 1 11 2 1 7 7 | 25.1 11.2 9.5 0.6 0.6 6.1 1.1 0.6 3.9 3.9 |
| Perceived improvement in glucose control | ||
| 137 42 | 76.5 23.5 |
| Perceived benefits of education | ||
| 93 50 18 2 | 51.9 27.9 10.0 1.1 |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation (IDF) 9th Edition 2019. Available online: https://www.diabetesatlas.org. (accessed on 20 July 2021).
- National Health Survey by Indonesian Ministry of Health. Indonesian Basic Data-Riset Kesehatan Dasar (RISKESDAS); Indonesian Ministry of Health: Jakarta, Indonesia, 2013. [Google Scholar]
- Shamsudin, J.; Harith, S.; Razak, S.A.; Zainal, N.A. A tailored dietary counselling via diet management tool (DMT) helps dietitian improves short term glycaemic control among type 2 diabetes patients. Int. Arch. Med. 2015, 8, 1–9. [Google Scholar] [CrossRef]
- Świątoniowska, N.; Sarzyńska, K.; Szymańska-Chabowska, A.; Jankowska-Polańska, B. The role of education in type 2 diabetes treatment. Diabetes Res. Clin. Pract. 2019, 151, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Shan, P.-F.; Li, Q.; Khamaisi, M.; Qiang, G.-F. Type 2 Diabetes Mellitus and Macrovascular Complications. Int. J. Endocrinol. 2017, 2017, 4301461. [Google Scholar] [CrossRef] [PubMed]
- Ricci-Cabello, I.; Ruiz-Pérez, I.; Rojas-García, A.; Pastor, G.; Rodríguez-Barranco, M.; Gonçalves, D.C. Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: A systematic review, meta-analysis and meta-regression. BMC Endocr. Disord. 2014, 14, 60. [Google Scholar] [CrossRef] [PubMed]
- Evert, A.B.; Boucher, J.L.; Cypress, M.; Dunbar, S.A.; Franz, M.J.; Mayer-Davis, E.J.; Neumiller, J.J.; Nwankwo, R.; Verdi, C.L.; Urbanski, P.; et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014, 37 (Suppl. S1), S120–S143. [Google Scholar] [CrossRef] [PubMed]
- Hendrie, G.A.; Coveney, J.; Cox, D. Exploring nutrition knowledge and the demographic variation in knowledge levels in an Australian community sample. Public Health Nutr. 2008, 11, 1365–1371. [Google Scholar] [CrossRef] [PubMed]
- Islam, N.S.; Wyatt, L.C.; Taher, M.; Riley, L.; Tandon, S.D.; Tanner, M.; Mukherji, B.R.; Trinh-Shevrin, C. A Culturally Tailored Community Health Worker Intervention Leads to Improvement in Patient-Centered Outcomes for Immigrant Patients with Type 2 Diabetes. Clin. Diabetes 2018, 36, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Muchiri, J.; Gericke, G.; Rheeder, P. Impact of nutrition education on diabetes knowledge and attitudes of adults with type 2 diabetes living in a resource-limited setting in South Africa: A randomised controlled trial. J. Endocrinol. Metab. Diabetes S. Afr. 2016, 21, 26–34. [Google Scholar] [CrossRef][Green Version]
- Van Smoorenburg, A.N.; Hertroijs, D.F.; Dekkers, T.; Elissen, A.M.; Melles, M. Patients’ perspective on self-management: Type 2 diabetes in daily life. BMC Health Serv. Res. 2019, 19, 605. [Google Scholar] [CrossRef] [PubMed]
- Hemmati Maslakpak, M.; Razmara, S.; Niazkhani, Z. Effects of Face-to-Face and Telephone-Based Family-Oriented Education on Self-Care Behavior and Patient Outcomes in Type 2 Diabetes: A Randomized Controlled Trial. J. Diabetes Res. 2017, 2017, 8404328. [Google Scholar] [CrossRef] [PubMed]
- Puri, I.Y.; Mohd Yusof, B.N.; Abu Zaid, Z.; Ismail, A.; Haron, H.; Lipoeto, N.I. Currents Nutritional Practices of Nutritionists in the Management of Type 2 Diabetes Patients at Public Health Centres in Padang, Indonesia. Nutrients 2021, 13, 1975. [Google Scholar] [CrossRef]
- Arifin, B.; van Asselt, A.D.I.; Setiawan, D.; Atthobari, J.; Postma, M.J.; Cao, Q. Diabetes distress in Indonesian patients with type 2 diabetes: A comparison between primary and tertiary care. BMC Health Serv. Res. 2019, 19, 773. [Google Scholar] [CrossRef] [PubMed]
- Ariane, C.P. Buku Pintar Kade Posbindu, 1st ed.; Kementrian Kesehatan Republik Indonesia, Indonesian Ministry of Health: Jakarta, Indonesia, 2019. [Google Scholar]
- Aday, L.A.; Cornelius, L.J. Designing and Conducting Health Surveys: A Comprehensive Guide; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- Rusdiana Savira, M.; Amelia, R. The effect of diabetes self-management education on Hba1c level and fasting blood sugar in type 2 diabetes mellitus patients in primary health care in binjai city of north Sumatera, Indonesia. Open Access Maced. J. Med. Sci. 2018, 6, 715–718. [Google Scholar] [CrossRef]
- Vasconcelos, C.; Cabral, M.; Ramos, E. The Impact of a Community-Based Food Education Program on Nutrition-Related Knowledge in Middle-Aged and Older Patients with Type 2 Diabetes: Results of a Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 2403. [Google Scholar] [CrossRef] [PubMed]
- Almeda-valdes, P.; Martagón, A.J.; Galán-ramírez, G.A.; Aguilar-salinas, C.A. Empowerment of patients with type 2 diabetes: Current perspectives. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 1311. [Google Scholar]
- Badedi, M.; Solan, Y.; Darraj, H.; Sabai, A.; Mahfouz, M.; Alamodi, S.; Alsabaani, A. Factors Associated with Long-Term Control of Type 2 Diabetes Mellitus. J. Diabetes Res. 2016, 2016, 2109542. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y. Effectiveness of Systematic Health Education Model for Type 2. Int. J. Endocrinol. 2018, 2018, 6530607. [Google Scholar] [CrossRef] [PubMed]
- Sami, W.; Ansari, T.; Butt, N.S.; Rashid, M.; Hamid, A. Effect of diet on type 2 diabetes mellitus: A review. Int. J. Health Sci. 2017, 11, 65. [Google Scholar]
- Viswanathan, V.; Krishnan, D.; Kalra, S. Insights on Medical Nutrition Therapy for Type 2 Diabetes Mellitus: An Indian Perspective. Adv. Ther. 2019, 36, 520–547. [Google Scholar] [CrossRef] [PubMed]
| Items | n | % |
|---|---|---|
| Sex | ||
| 42 137 | 23.5 76.5 |
| Age, years | ||
| Mean SD | (57.51 ± 9.61) | |
| 103 76 | 57.8 42.5 |
| Educational level | ||
| 82 74 23 | 45.9 41.3 12.8 |
| Employment | ||
| 88 46 45 | 49.2 25.7 25.1 |
| Participating Public Health Care (PUSKESMAS) | ||
| 37 21 18 17 17 16 14 12 11 10 6 | 20.7 11.7 10.1 9.5 9.5 8.9 7.8 6.7 6.1 5.6 3.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puri, I.Y.; Yusof, B.-N.M.; Zaid, Z.A.; Ismail, A.; Haron, H.; Lipoeto, N.I. The Individual Nutrition Education Needs among Patients with Type 2 Diabetes at the Public Health Centers in Padang, Indonesia: A Cross-Sectional Study. Nutrients 2022, 14, 1105. https://doi.org/10.3390/nu14051105
Puri IY, Yusof B-NM, Zaid ZA, Ismail A, Haron H, Lipoeto NI. The Individual Nutrition Education Needs among Patients with Type 2 Diabetes at the Public Health Centers in Padang, Indonesia: A Cross-Sectional Study. Nutrients. 2022; 14(5):1105. https://doi.org/10.3390/nu14051105
Chicago/Turabian StylePuri, Ice Yolanda, Barakatun-Nisak Mohd Yusof, Zalina Abu Zaid, Amin Ismail, Hasnah Haron, and Nur Indrawaty Lipoeto. 2022. "The Individual Nutrition Education Needs among Patients with Type 2 Diabetes at the Public Health Centers in Padang, Indonesia: A Cross-Sectional Study" Nutrients 14, no. 5: 1105. https://doi.org/10.3390/nu14051105
APA StylePuri, I. Y., Yusof, B.-N. M., Zaid, Z. A., Ismail, A., Haron, H., & Lipoeto, N. I. (2022). The Individual Nutrition Education Needs among Patients with Type 2 Diabetes at the Public Health Centers in Padang, Indonesia: A Cross-Sectional Study. Nutrients, 14(5), 1105. https://doi.org/10.3390/nu14051105







