The Combination of School-Based and Family-Based Interventions Appears Effective in Reducing the Consumption of Sugar-Sweetened Beverages, a Randomized Controlled Trial among Chinese Schoolchildren
Abstract
:1. Introduction
2. Subjects and Methods
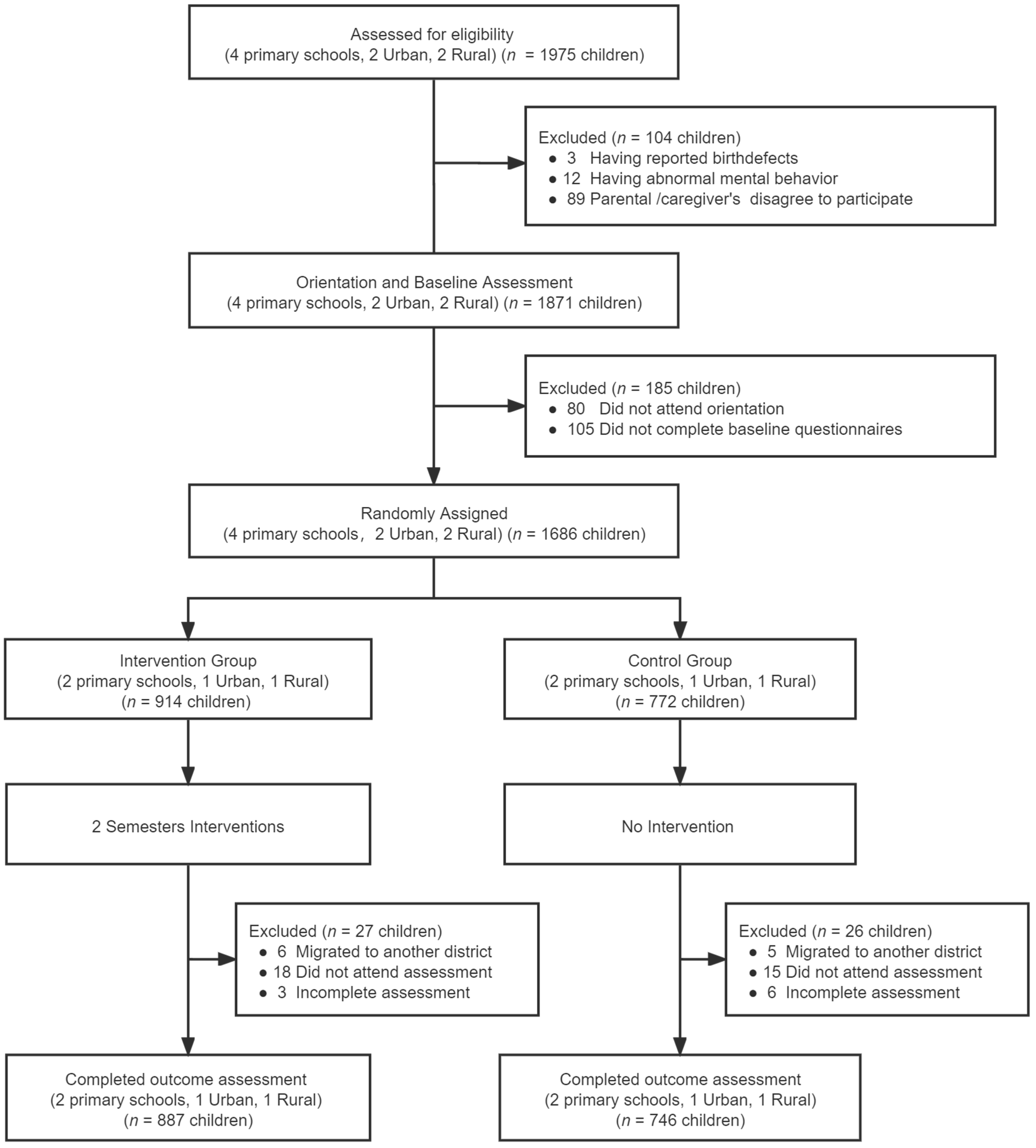
2.1. Study Subjects and Selection
2.2. Inclusion and Exclusion Criteria
2.3. Ethics Statement
2.4. Study Design
2.5. Knowledge about Sugar-Sweetened Beverages (SSBs)
2.6. Family Environment of SSBs
2.7. The Weekly SSBs Intake Frequency
2.8. Intervention
2.9. Quality Control
2.10. Data Management and Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics
3.2. Knowledge of SSBs
3.3. Family Influences with Parents and at Home
3.4. Frequency of SSBs Consumption
3.4.1. Frequency Distribution of SSBs Consumption
3.4.2. Frequency Difference in SSBs Consumption
3.5. Multivariate Regression Analysis of Factors on Improvement of SSBs Intake
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- CDC. Get the Facts: Sugar-Sweetened Beverages and Consumption. 2017. Available online: https://www.cdc.gov/nutrition/data-statistics/sugar-sweetened-beverages-intake.html (accessed on 28 December 2021).
- Qobadi, M.; Payton, M. Consumption of Sugar-Sweetened Beverages in Mississippi: Is There A Disparity? Behavioral Risk Factor Surveillance System, 2012. Int. J. Environ. Res. Public Health 2017, 14, 228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.; Xu, F.; Town, M.; Blanck, H.M. Prevalence of Sugar-Sweetened Beverage Intake Among Adults—23 States and the District of Columbia, 2013. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Han, E.; Powell, L.M. Consumption Patterns of Sugar-Sweetened Beverages in the United States. J. Acad. Nutr. Diet. 2013, 113, 43–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slining, M.M.; Mathias, K.C.; Popkin, B.M. Trends in Food and Beverage Sources among US Children and Adolescents: 1989–2010. J. Acad. Nutr. Diet. 2013, 113, 1683–1694. [Google Scholar] [CrossRef] [Green Version]
- Ng, S.W.; Ni Mhurchu, C.; Jebb, S.A.; Popkin, B.M. Patterns and trends of beverage consumption among children and adults in Great Britain, 1986–2009. Br. J. Nutr. 2012, 108, 536–551. [Google Scholar] [CrossRef] [Green Version]
- Barquera, S.; Campirano, F.; Bonvecchio, A.; Hernández-Barrera, L.; Rivera, A.J.; Popkin, B.M. Caloric beverage consumption patterns in Mexican children. Nutr. J. 2010, 9, 47. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Tao, W.; Mao, W.; Liu, A.; Liu, Z.; Zhang, B. Analysis on status of carbonated beverage consumption among the population over the age of 3 in nine provinces of China. Chin. J. Health Educ. 2015, 9, 819–822, 826. Available online: https://www.cnki.com.cn/Article/CJFDTotal-ZGJK201509002.htm (accessed on 28 December 2021). [CrossRef]
- Du, S.-M.; Hu, X.-Q.; Zhang, Q.; Wang, X.-J.; Pan, H.; Gao, J.-M.; Song, J.; Gao, C.-L.; He, Z.-F.; Ma, G.-S. Daily intake of plain water and beverages of primary and middle school students in four cities of China. Zhonghua Yu Fang Yi Xue Za Zhi Chin. J. Prev. Med. 2013, 47, 202–205. [Google Scholar]
- You, L.; Yang, T.; Bai, Y.; Chen, Y.; Zhang, Y.; Wang, P. Consumption pattern of liquid dairy products and soft beverages among pupils from nine areas in China. Chin. J. Sch. Health 2014, 35, 1772–1775. [Google Scholar]
- China National Health and Family Planning Commission. Report on Nutrition and Chronic Diseases of Chinese Residents, 3rd ed.; People’s Medical Publishing House: Beijing, China, 2015; pp. 11–15. ISBN 978-7-117-21915-0. [Google Scholar]
- Qin, Z.; Xu, F.; Ye, Q.; Zhou, H.; Li, C.; He, J.; Wang, Z.; Hong, X.; Hou, X. Sugar-sweetened beverages and school students’ hypertension in urban areas of Nanjing, China. J. Hum. Hypertens. 2018, 32, 392–396. [Google Scholar] [CrossRef]
- Malik, V.S.; Pan, A.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 1084–1102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, A.; Hu, F.B. Effects of carbohydrates on satiety: Differences between liquid and solid food. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; He, F.J.; Yin, Y.; Hashem, K.M.; MacGregor, A.G. Gradual reduction of sugar in soft drinks without substitution as a strategy to reduce overweight, obesity, and type 2 diabetes: A modelling study. Lancet Diabetes Endocrinol. 2016, 4, 105–114. [Google Scholar] [CrossRef]
- Yu, P.; Chen, Y.; Zhao, A.; Bai, Y.; Zheng, Y.; Zhao, W.; Zhang, Y. Consumption of sugar-sweetened beverages and its association with overweight among young children from China. Public Health Nutr. 2016, 19, 2336–2346. [Google Scholar] [CrossRef] [Green Version]
- Keller, K.L.; Kirzner, J.; Pietrobelli, A.; St-Onge, M.-P.; Faith, M.S. Increased Sweetened Beverage Intake Is Associated with Reduced Milk and Calcium Intake in 3- to 7-Year-Old Children at Multi-Item Laboratory Lunches. J. Am. Diet. Assoc. 2009, 109, 497–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gui, Z.-H.; Zhu, Y.-N.; Cai, L.; Sun, F.-H.; Ma, Y.-H.; Jing, J.; Chen, Y.-J. Sugar-Sweetened Beverage Consumption and Risks of Obesity and Hypertension in Chinese Children and Adolescents: A National Cross-Sectional Analysis. Nutrients 2017, 9, 1302. [Google Scholar] [CrossRef] [Green Version]
- Bernabé, E.; Vehkalahti, M.; Sheiham, A.; Aromaa, A.; Suominen, A.L. Sugar-sweetened beverages and dental caries in adults: A 4-year prospective study. J. Dent. 2014, 42, 952–958. [Google Scholar] [CrossRef]
- Scharf, R.J.; DeBoer, M.D. Sugar-Sweetened Beverages and Children’s Health. Annu. Rev. Public Health 2016, 37, 273–293. [Google Scholar] [CrossRef] [Green Version]
- Malik, V.S.; Hu, F.B. Sugar-Sweetened Beverages and Cardiometabolic Health: An Update of the Evidence. Nutrients 2019, 11, 1840. [Google Scholar] [CrossRef] [Green Version]
- Xi, B.; Shuangshuang, L.; Reilly, K.H.; Li, S.; Zheng, R.; Barrio-Lopez, M.T.; Martinez-Gonzalez, M.A.; Zhou, D. Sugar-sweetened beverages and risk of hypertension and CVD: A dose–response meta-analysis. Br. J. Nutr. 2015, 113, 709–717. [Google Scholar] [CrossRef] [Green Version]
- Rahman, A.A.; Jomaa, L.; Kahale, L.; Adair, P.; Pine, C. Effectiveness of behavioral interventions to reduce the intake of sugar-sweetened beverages in children and adolescents: A systematic review and meta-analysis. Nutr. Rev. 2017, 76, 88–107. [Google Scholar] [CrossRef]
- Mazarello Paes, V.; Hesketh, K.; O’Malley, C.; Moore, H.; Summerbell, C.; Griffin, S.; van Sluijs, E.M.F.; Ong, K.K.; Lakshman, R. Determinants of sugar-sweetened beverage consumption in young children: A systematic review. Obes. Rev. J. Int. Assoc. Study Obes. 2015, 16, 903–913. [Google Scholar] [CrossRef] [Green Version]
- Mensink, F.; Schwinghammer, S.A.; Smeets, A. The Healthy School Canteen Programme: A Promising Intervention to Make the School Food Environment Healthier. J. Environ. Public Health 2012, 2012, 415746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vartanian, L.R.; Schwartz, M.B.; Brownell, K.D. Effects of Soft Drink Consumption on Nutrition and Health: A Systematic Review and Meta-Analysis. Am. J. Public Health 2007, 97, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Sichieri, R.; Trotte, A.P.; De Souza, R.A.; Veiga, G.V. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009, 12, 197–202. [Google Scholar] [CrossRef] [Green Version]
- Østbye, T.; Malhotra, R.; Stroo, M.; Lovelady, C.; Brouwer, R.; Zucker, N.; Fuemmeler, B. The effect of the home environment on physical activity and dietary intake in preschool children. Int. J. Obes. 2013, 37, 1314–1321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zahid, A.; Davey, C.; Reicks, M. Beverage Intake among Children: Associations with Parent and Home-Related Factors. Int. J. Environ. Res. Public Health 2017, 14, 929. [Google Scholar] [CrossRef] [Green Version]
- Hill, J.O. Can a small-changes approach help address the obesity epidemic? A report of the Joint Task Force of the American Society for Nutrition, Institute of Food Technologists, and International Food Information Council. Am. J. Clin. Nutr. 2009, 89, 477–484. [Google Scholar] [CrossRef] [Green Version]
- Sirasa, F.; Mitchell, L.; Azhar, A.; Chandrasekara, A.; Harris, N. A six-week healthy eating intervention with family engagement improves food knowledge and preferences but not dietary diversity among urban preschool children in Sri Lanka. Public Health Nutr. 2021, 24, 4328–4338. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhu, Y.; Peng, Q.; Ji, Y.; Yuan, H.; Peng, H. Effect of the application of weekly behavior records in comprehensive intervention on KAP of sugary beverages among pupils. Chin. J. Health Educ. 2021, 37, 63–66. [Google Scholar] [CrossRef]
- Gillies, C.; Blanchet, R.; Gokiert, R.; Farmer, A.; Thorlakson, J.; Hamonic, L.; Willows, N.D. School-based nutrition interventions for Indigenous children in Canada: A scoping review. BMC Public Health 2020, 20, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nezami, B.T.; Lytle, L.A.; Tate, D.F. A randomized trial to reduce sugar-sweetened beverage and juice intake in preschool-aged children: Description of the Smart Moms intervention trial. BMC Public Health 2016, 16, 837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- White, A.H.; James, S.A.; Paulson, S.W.; Beebe, L.A. Sugar Sweetened Beverage Consumption among Adults with Children in the Home. Front. Nutr. 2018, 5, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vinke, P.; Blijleven, K.; Luitjens, M.; Corpeleijn, E. Young Children’s Sugar-Sweetened Beverage Consumption and 5-Year Change in BMI: Lessons Learned from the Timing of Consumption. Nutrients 2020, 12, 2486. [Google Scholar] [CrossRef] [PubMed]
- Teo, C.; Chin, Y.; Lim, P.; Masrom, S.; Shariff, Z. Impacts of a School-Based Intervention That Incorporates Nutrition Education and a Supportive Healthy School Canteen Environment among Primary School Children in Malaysia. Nutrients 2021, 13, 1712. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Bleich, S.N.; Gortmaker, S.L. Increasing Caloric Contribution From Sugar-Sweetened Beverages and 100% Fruit Juices Among US Children and Adolescents, 1988–2004. Pediatrics 2008, 121, e1604–e1614. [Google Scholar] [CrossRef]
- Bogart, L.M.; Elliott, M.N.; Ober, A.J.; Klein, D.J.; Hawes-Dawson, J.; Cowgill, B.O.; Uyeda, K.; Schuster, M.A. Home Sweet Home: Parent and Home Environmental Factors in Adolescent Consumption of Sugar-Sweetened Beverages. Acad. Pediatr. 2017, 17, 529–536. [Google Scholar] [CrossRef]
- Fernández-Alvira, J.M.; Mouratidou, T.; Bammann, K.; Hebestreit, A.; Barba, G.; Sieri, S.; Reisch, L.; Eiben, G.; Hadjigeorgiou, C.; Kovacs, E.; et al. Parental education and frequency of food consumption in European children: The IDEFICS study. Public Health Nutr. 2012, 16, 487–498. [Google Scholar] [CrossRef] [Green Version]
- Acero, D.; Zoellner, J.; Davy, B.; Hedrick, V. Changes in Non-Nutritive Sweetener Consumption Patterns in Response to a Sugar-Sweetened Beverage Reduction Intervention. Nutrients 2020, 12, 3428. [Google Scholar] [CrossRef]
- Battram, D.S.; Piché, L.; Beynon, C.; Kurtz, J.; He, M. Sugar-Sweetened Beverages: Children’s Perceptions, Factors of Influence, and Suggestions for Reducing Intake. J. Nutr. Educ. Behav. 2016, 48, 27–34. [Google Scholar] [CrossRef]
- Fulkerson, J.A.; Friend, S.; Horning, M.; Flattum, C.; Draxten, M.; Neumark-Sztainer, D.; Gurvich, O.; Garwick, A.; Story, M.; Kubik, M.Y. Family Home Food Environment and Nutrition-Related Parent and Child Personal and Behavioral Outcomes of the Healthy Home Offerings via the Mealtime Environment (HOME) Plus Program: A Randomized Controlled Trial. J. Acad. Nutr. Diet. 2017, 118, 240–251. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.L.; Lemon, S.C.; Clausen, K.; Whyte, J.; Rosal, M.C. Design and methods for a community-based intervention to reduce sugar-sweetened beverage consumption among youth: H2GO! study. BMC Public Health 2016, 16, 1150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popkin, B.M.; Hawkes, C. Sweetening of the global diet, particularly beverages: Patterns, trends, and policy responses. Lancet Diabetes Endocrinol. 2016, 4, 174–186. [Google Scholar] [CrossRef] [Green Version]
- Leonard, K.; Masatu, M.C. Outpatient process quality evaluation and the Hawthorne Effect. Soc. Sci. Med. 2006, 63, 2330–2340. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Retained in Trial (1633) | Dropped Out (53) | χ2/t | p |
|---|---|---|---|---|
| Sex | ||||
| Male | 875/53.6 | 29/54.7 | 0.03 | 0.87 |
| Female | 758/46.4 | 24/45.3 | ||
| Age (years) | ||||
| 9 | 1044/63.9 | 33/62.3 | 0.06 | 0.80 |
| 10 | 589/36.1 | 20/37.7 | ||
| Area | ||||
| Rural | 891/54.6 | 31/58.5 | 0.32 | 0.57 |
| Urban | 742/45.4 | 22/41.5 | ||
| BMI * | 17.21 ± 2.93 | 17.22 ± 2.96 | −0.05 | 0.96 |
| Frequency of SSBs consumption | 4.81 ± 4.24 | 4.45 ± 4.48 | −0.94 | 0.35 |
| Father’s education level | ||||
| High school | 674/41.3 | 23/43.4 | 0.10 | 0.76 |
| University or above | 959/58.7 | 30/56.6 | ||
| Mother’s education level | ||||
| High school | 722/44.2 | 25/47.1 | 0.18 | 0.67 |
| University or above | 911/55.8 | 28/52.8 | ||
| Father’s BMI | ||||
| <24 kg/m2 | 733/44.9 | 22/41.5 | 0.24 | 0.63 |
| ≥24 kg/m2 | 900/55.1 | 31/58.5 | ||
| Mother’s BMI | ||||
| <24 kg/m2 | 1360/83.3 | 42/79.2 | 0.60 | 0.44 |
| ≥24 kg/m2 | 273/16.7 | 11/20.8 |
| Characteristics | Total (1633) | Intervention Group (887) | Control Group (746) | χ2/t | p |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 875/53.6 | 480/54.1 | 395/52.9 | 0.20 | 0.65 |
| Female | 758/46.4 | 407/45.9 | 351/47.1 | ||
| Age (years) | |||||
| 9 | 1044/63.9 | 584/65.8 | 460/61.7 | 3.07 | 0.08 |
| 10 | 589/36.1 | 303/34.2 | 286/38.3 | ||
| Area | |||||
| Rural | 891/54.6 | 516/58.2 | 375/50.3 | 10.22 | 0.00 |
| Urban | 742/45.4 | 371/41.8 | 371/49.7 | ||
| BMI | 17.19 ± 2.99 | 17.11 ± 2.97 | 17.28 ± 3.01 | −1.12 | 0.26 |
| Frequency of SSBs consumption | 4.86 ± 4.80 | 4.55 ± 4.99 | 5.24 ± 4.54 | −2.42 | 0.02 |
| Father’s education level | |||||
| High school | 674/41.3 | 363/40.9 | 311/41.7 | 0.10 | 0.76 |
| University or above | 959/58.7 | 524/59.1 | 435/58.3 | ||
| Mother’s education level | |||||
| High school | 722/44.2 | 395/44.5 | 327/43.8 | 0.08 | 0.80 |
| University or above | 911/55.8 | 492/55.5 | 419/56.2 | ||
| Father’s BMI | |||||
| <24 kg/m2 | 733/44.9 | 395/44.5 | 338/45.3 | 0.10 | 0.77 |
| ≥24 kg/m2 | 900/55.1 | 492/55.5 | 408/54.7 | ||
| Mother’s BMI | |||||
| <24 kg/m2 | 1360/83.3 | 724/81.6 | 636/85.3 | 3.84 | 0.05 |
| ≥24 kg/m2 | 273/16.7 | 163/18.4 | 110/14.7 |
| Knowledge | Before the Intervention | χ2 | p | After the Intervention | χ2 | p | ||
|---|---|---|---|---|---|---|---|---|
| Intervention Group (n = 887) | Control Group (n = 746) | Intervention Group (n = 887) | Control Group (n = 746) | |||||
| 1. Definition of added sugar. | 183/20.6 | 180/24.1 | 2.87 | 0.10 | 618/69.7 | 209/28.0 | 281.31 | 0.00 |
| 2. Definition of SSBs. | 190/21.4 | 170/22.8 | 0.44 | 0.51 | 593/66.9 | 197/26.4 | 265.44 | 0.00 |
| 3. SSBs are bad for health. | 789/89.0 | 671/89.9 | 0.42 | 0.52 | 874/98.5 | 678/90.9 | 50.30 | 0.00 |
| 4. SSBs may cause tooth decay. | 734/82.8 | 612/82.0 | 0.14 | 0.74 | 865/97.5 | 662/88.7 | 51.46 | 0.00 |
| 5. SSBs may cause childhood overweight and obesity. | 613/69.1 | 542/72.7 | 2.46 | 0.13 | 839/94.6 | 582/78.0 | 98.51 | 0.00 |
| 6. SSBs can increase type 2 diabetes in children and in later life. | 377/42.5 | 328/44.0 | 0.35 | 0.58 | 733/82.6 | 456/61.1 | 94.72 | 0.00 |
| 7. Carbonated drinks may increase risks of bone in children. | 362/40.8 | 325/43.6 | 1.26 | 0.27 | 736/83.0 | 475/63.7 | 78.79 | 0.00 |
| 8. Fruit and/or vegetable beverage are not a substitute for fruits and vegetables. | 500/56.4 | 425/57.0 | 0.06 | 0.84 | 774/87.3 | 500/67.0 | 96.75 | 0.00 |
| 9. Milk beverages are not substitute for milk. | 305/34.4 | 273/36.6 | 0.87 | 0.38 | 613/69.1 | 358/48.0 | 74.98 | 0.00 |
| 10. SSBs are one of the high-sugar foods. | 765/82.2 | 622/83.4 | 2.60 | 0.11 | 848/95.6 | 659/88.3 | 30.04 | 0.00 |
| Adequate knowledge about SSBs * | 301/33.9 | 276/37.0 | 1.66 | 0.21 | 786/88.6 | 400/53.6 | 249.60 | 0.00 |
| Family Environment with Parents | Before the Intervention | χ2 | p | After the Intervention | χ2 | p | ||
|---|---|---|---|---|---|---|---|---|
| Intervention Group (n = 887) | Control Group (n = 746) | Intervention Group (n = 887) | Control Group (n = 746) | |||||
| Parents have been warned about harms of SSBs | ||||||||
| Yes | 563/63.5 | 447/59.9 | 2.17 | 0.15 | 788/88.8 | 477/63.9 | 143.89 | 0.00 |
| No | 324/36.5 | 299/40.1 | 99/11.2 | 269/36.1 | ||||
| My home always has SSBs a | ||||||||
| Yes | 218/24.6 | 163/21.8 | 1.69 | 0.20 | 96/10.8 | 167/22.4 | 40.10 | 0.00 |
| No | 669/75.4 | 583/78.2 | 791/89.2 | 579/77.6 | ||||
| My parents restricted me from drinking SSBs b | ||||||||
| Yes | 502/56.6 | 422/56.6 | 0.00 | 1.00 | 756/85.2 | 424/56.8 | 162.98 | 0.00 |
| No | 385/43.4 | 324/43.4 | 131/14.8 | 322/43.2 | ||||
| My parents restricted me from sugary snacks c | ||||||||
| Yes | 468/52.8 | 385/51.6 | 0.22 | 0.66 | 737/83.1 | 411/55.1 | 152.10 | 0.00 |
| No | 419/47.2 | 361/48.4 | 150/16.9 | 335/44.9 | ||||
| My parents often drink SSBs d | ||||||||
| Yes | 276/31.1 | 180/24.1 | 9.83 | 0.00 | 57/6.4 | 204/27.3 | 132.06 | 0.00 |
| No | 611/68.9 | 566/75.9 | 830/93.6 | 542/72.7 | ||||
| My parents often eat sugary snacks e | ||||||||
| Yes | 182/20.5 | 157/21.0 | 0.07 | 0.81 | 40/4.5 | 169/22.7 | 119.53 | 0.00 |
| No | 705/79.5 | 589/79.0 | 847/95.5 | 577/77.3 | ||||
| Frequency of SSBs Consumption (Times/Week) | Intervention Group (n = 887) | χ2 | p | Control Group (n = 746) | χ2 | p | |||
|---|---|---|---|---|---|---|---|---|---|
| Before the Intervention | After the Intervention | Before the Intervention | After the Intervention | ||||||
| Carbonated beverages | <1 | 552/62.2 | 622/70.1 | 17.44 | 0.00 | 427/57.2 | 408/54.7 | 3.03 | 0.388 |
| 1~3 | 314/35.4 | 248/28.0 | 306/41.0 | 324/43.4 | |||||
| ≥4 | 21/2.4 | 17/1.9 | 13/1.7 | 14/1.9 | |||||
| Fruit and/or vegetable beverages | <1 | 509/57.4 | 675/76.1 | 86.45 | 0.00 | 374/50.1 | 403/54.0 | 4.15 | 0.25 |
| 1~3 | 352/39.7 | 200/22.5 | 351/47.1 | 321/43.0 | |||||
| ≥4 | 26/2.9 | 12/1.4 | 21/2.8 | 22/2.9 | |||||
| Sweetened tea beverages | <1 | 693/78.1 | 731/82.4 | 9.81 | 0.02 | 522/70.0 | 520/69.7 | 6.57 | 0.09 |
| 1~3 | 175/19.7 | 148/16.7 | 203/27.2 | 217/29.1 | |||||
| ≥4 | 19/2.1 | 8/0.9 | 21/2.8 | 9/1.2 | |||||
| Lactobacillus/milk beverages | <1 | 459/51.7 | 607/68.4 | 60.79 | 0.00 | 342/45.8 | 363/48.7 | 2.57 | 0.46 |
| 1~3 | 338/38.1 | 226/25.5 | 316/42.4 | 302/40.5 | |||||
| ≥4 | 90/10.1 | 54/6.1 | 88/11.8 | 81/10.9 | |||||
| Sports/energy beverages | <1 | 605/68.2 | 660/74.4 | 12.55 | 0.01 | 459/61.5 | 424/56.8 | 5.95 | 0.11 |
| 1~3 | 254/28.6 | 212/23.9 | 263/35.3 | 293/39.3 | |||||
| ≥4 | 28/3.2 | 15/1.7 | 24/3.2 | 29/3.9 | |||||
| Plant-protein beverages | <1 | 672/75.8 | 716/80.7 | 7.87 | 0.05 | 526/70.5 | 516/69.2 | 0.88 | 0.83 |
| 1~3 | 184/20.7 | 142/16.0 | 192/25.7 | 196/26.3 | |||||
| ≥4 | 31/3.5 | 29/3.3 | 28/3.8 | 34/4.6 | |||||
| Brewed beverages | <1 | 764/86.1 | 804/90.6 | 14.43 | 0.00 | 602/80.7 | 608/81.5 | 1.93 | 0.59 |
| 1~3 | 91/10.3 | 72/8.1 | 120/16.1 | 122/16.4 | |||||
| ≥4 | 32/3.6 | 11/1.2 | 24/3.2 | 16/2.1 | |||||
| Coffee beverages | <1 | 827/93.2 | 849/95.7 | 6.16 | 0.10 | 686/92.0 | 690/92.5 | 0.21 | 0.98 |
| 1~3 | 55/6.2 | 35/3.9 | 51/6.8 | 48/6.4 | |||||
| ≥4 | 5/0.6 | 3/0.3 | 9/1.2 | 8/1.1 | |||||
| Any SSBs | <1 | 177/20.0 | 300/33.8 | 61.98 | 0.00 | 111/14.9 | 119/16.0 | 6.90 | 0.08 |
| 1~3 | 333/37.5 | 308/34.7 | 253/33.9 | 208/27.9 | |||||
| ≥4 | 377/42.5 | 279/31.5 | 382/51.2 | 419/56.2 | |||||
| Frequency of SSBs Consumption | Intervention Group (n = 887) | t | p | Control Group (n = 746) | t | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before the Intervention | After the Intervention | Mean Change | Before the Intervention | After the Intervention | Mean Change | |||||
| Carbonated beverages | 0.61 ± 1.18 | 0.49 ± 1.01 | −0.12 ± 1.39 | 2.46 | 0.01 | 0.62 ± 0.94 | 0.73 ± 1.21 | 0.11 ± 1.23 | −2.48 | 0.01 |
| Fruit and/or vegetable beverages | 0.73 ± 1.19 | 0.39 ± 0.89 | −0.33 ± 1.40 | 7.14 | 0.00 | 0.83 ± 1.24 | 0.82 ± 1.20 | −0.01 ± 1.63 | 0.16 | 0.88 |
| Sweetened tea beverages | 0.42 ± 1.15 | 0.27 ± 0.74 | −0.14 ± 1.29 | 3.27 | 0.00 | 0.53 ± 1.13 | 0.49 ± 1.08 | −0.04 ± 1.35 | 0.87 | 0.38 |
| Lactobacillus/milk beverages | 1.20 ± 1.90 | 0.78 ± 1.55 | −0.43 ± 2.20 | 5.74 | 0.00 | 1.34 ± 1.90 | 1.26 ± 1.68 | −0.08 ± 2.42 | 0.91 | 0.36 |
| Sports/energy beverages | 0.58 ± 1.19 | 0.44 ± 1.02 | −0.14 ± 1.37 | 2.93 | 0.00 | 0.66 ± 1.19 | 0.78 ± 1.30 | −0.12 ± 1.56 | −2.04 | 0.04 |
| Plant-protein beverages | 0.52 ± 1.25 | 0.45 ± 1.21 | −0.07 ± 1.72 | 1.24 | 0.21 | 0.63 ± 1.43 | 0.67 ± 1.36 | 0.05 ± 1.94 | −0.66 | 0.51 |
| Brewed beverages | 0.37 ± 1.27 | 0.20 ± 0.81 | −0.16 ± 1.48 | 3.30 | 0.00 | 0.36 ± 1.18 | 0.28 ± 0.76 | −0.11 ± 1.53 | 1.06 | 0.29 |
| Coffee beverages | 0.12 ± 0.61 | 0.07 ± 0.89 | −0.04 ± 0.68 | 1.87 | 0.06 | 0.18 ± 0.82 | 0.16 ± 0.72 | −0.02 ± 1.01 | 0.58 | 0.56 |
| Any SSBs | 4.55 ± 4.99 | 3.11 ± 3.22 | −1.44 ± 6.65 | 6.41 | 0.00 | 5.24 ± 4.54 | 5.25 ± 4.24 | 0.01 ± 6.26 | −0.04 | 0.97 |
| Variables | Number (n = 1504) | Median Difference before and after Intervention a (25th, 75th Percentiles) | Β (95% CI) | p |
|---|---|---|---|---|
| Group | ||||
| Control Group | 710 | 0.00 (−3.00, 3.00) | 1 | |
| Intervention Group | 794 | −1.00 (−4.00, 1.25) | −1.77 (−2.45, −1.09) | 0.00 |
| Area | ||||
| Rural | 819 | 0.00 (−3.00, 3.00) | 1 | |
| Urban | 685 | −1.00 (−4.00, 2.00) | −2.05 (−2.77, −1.32) | 0.00 |
| Parental educational | ||||
| Parental education level is university or above | 697 | 0.00 (−3.00, 3.00) | 1 | |
| One parent’s education level is university or above | 286 | −1.00 (−4.00, 2.00) | −0.95 (−1.88, −0.01) | 0.04 |
| Parental education level is high school or blow | 521 | −1.00 (−4.00, 2.00) | −1.19 (−1.99, −0.38) | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, C.; Hong, X.; Wang, W.; Zhou, H.; Wu, J.; Xu, H.; Zhou, N.; Zhao, J. The Combination of School-Based and Family-Based Interventions Appears Effective in Reducing the Consumption of Sugar-Sweetened Beverages, a Randomized Controlled Trial among Chinese Schoolchildren. Nutrients 2022, 14, 833. https://doi.org/10.3390/nu14040833
Wang C, Hong X, Wang W, Zhou H, Wu J, Xu H, Zhou N, Zhao J. The Combination of School-Based and Family-Based Interventions Appears Effective in Reducing the Consumption of Sugar-Sweetened Beverages, a Randomized Controlled Trial among Chinese Schoolchildren. Nutrients. 2022; 14(4):833. https://doi.org/10.3390/nu14040833
Chicago/Turabian StyleWang, Chenchen, Xin Hong, Weiwei Wang, Hairong Zhou, Jie Wu, Hao Xu, Nan Zhou, and Jinkou Zhao. 2022. "The Combination of School-Based and Family-Based Interventions Appears Effective in Reducing the Consumption of Sugar-Sweetened Beverages, a Randomized Controlled Trial among Chinese Schoolchildren" Nutrients 14, no. 4: 833. https://doi.org/10.3390/nu14040833
APA StyleWang, C., Hong, X., Wang, W., Zhou, H., Wu, J., Xu, H., Zhou, N., & Zhao, J. (2022). The Combination of School-Based and Family-Based Interventions Appears Effective in Reducing the Consumption of Sugar-Sweetened Beverages, a Randomized Controlled Trial among Chinese Schoolchildren. Nutrients, 14(4), 833. https://doi.org/10.3390/nu14040833








