Associations between Serum Vitamin A and Metabolic Risk Factors among Eastern Chinese Children and Adolescents
Abstract
1. Introduction
2. Methods
2.1. Study Participants
2.2. Survey and Measurements
2.3. Diagnostic Criteria and Definitions
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Participants
3.2. Prevalence of Metabolic Diseases across Serum Vitamin A Quartiles in Children and Adolescents
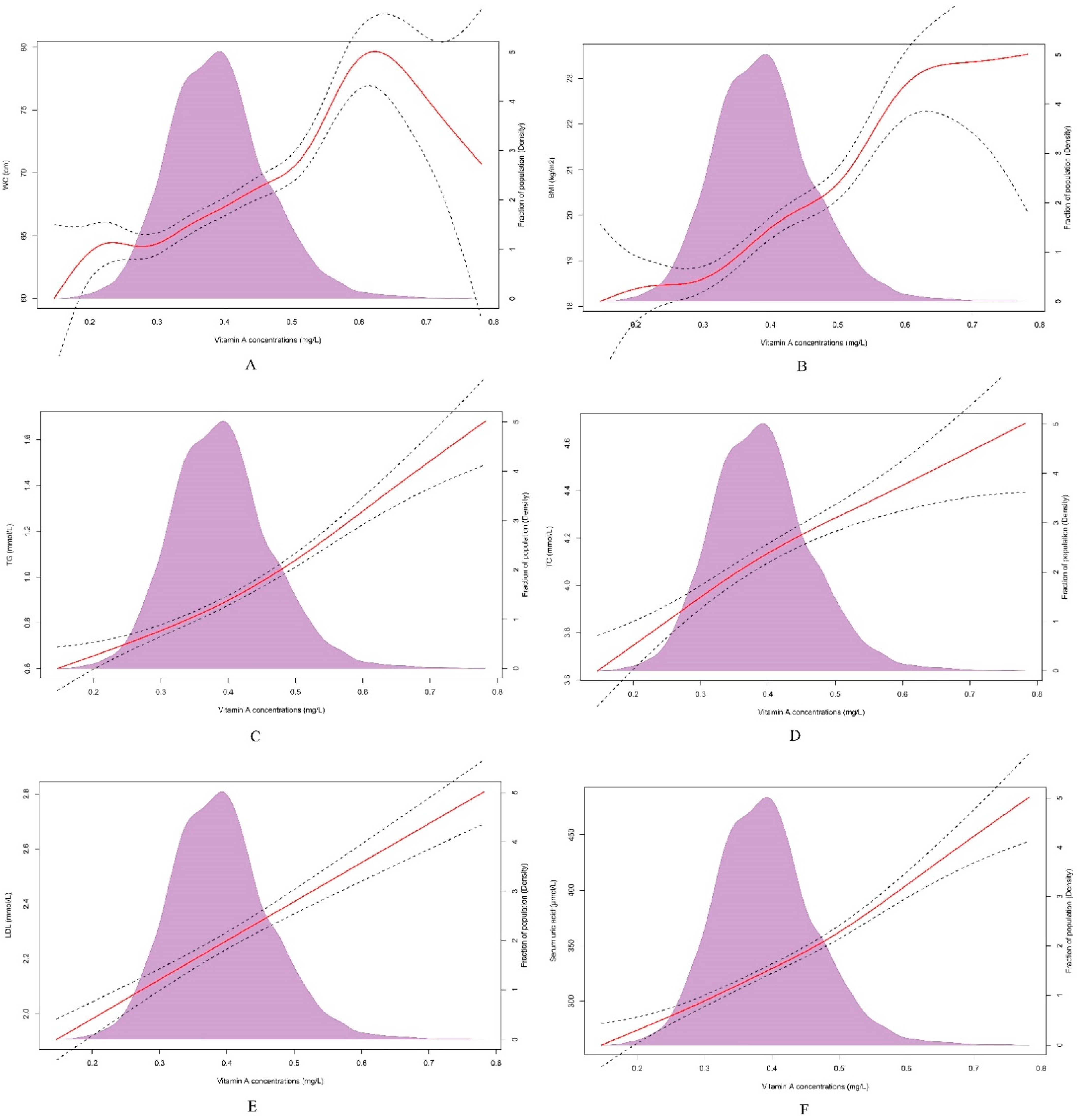
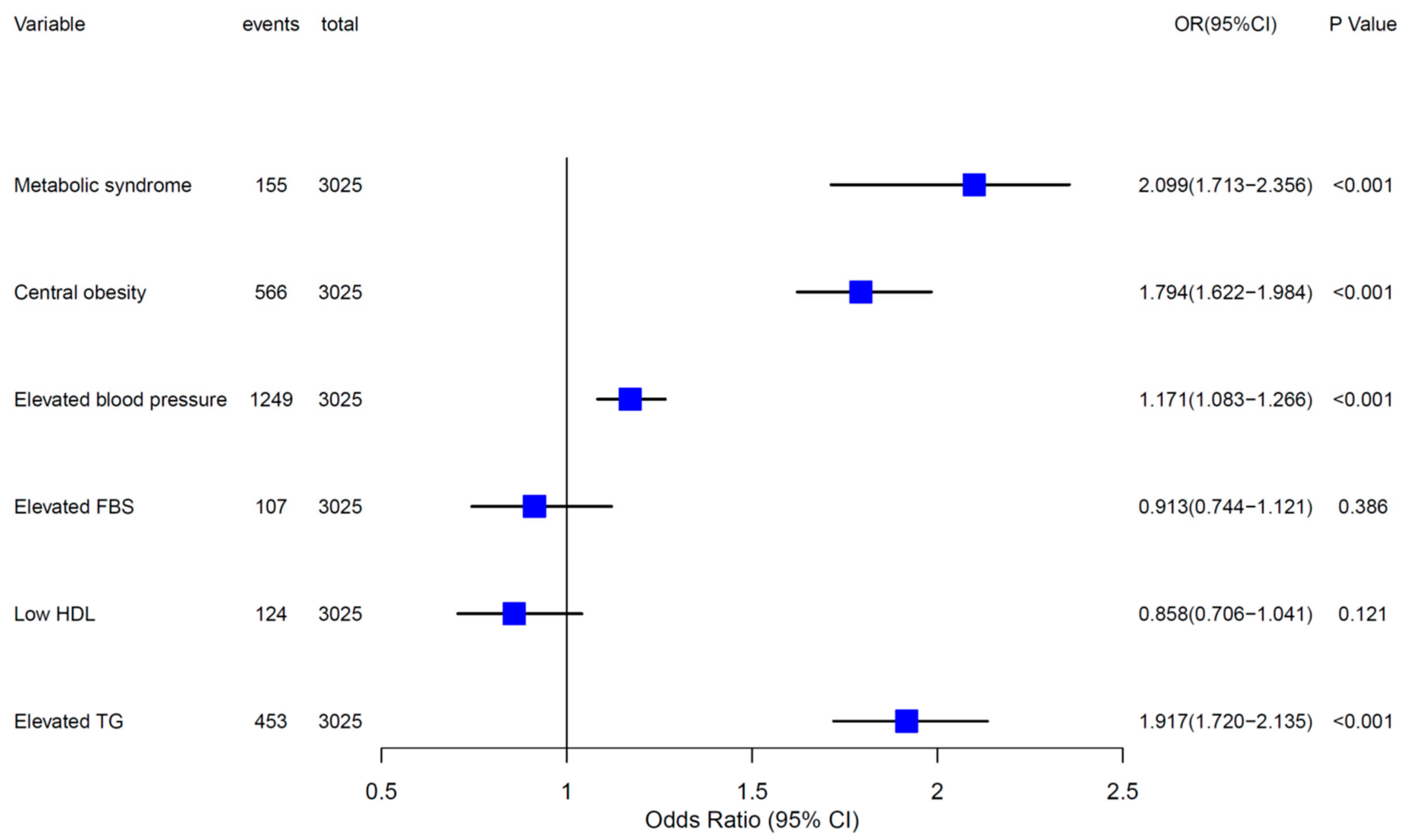
3.3. Associations of Serum Vitamin A with Metabolic Risk Factors in Children and Adolescents
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Conaway, H.H.; Henning, P.; Lerner, U.H. Vitamin a metabolism, action, and role in skeletal homeostasis. Endocr. Rev. 2013, 34, 766–797. [Google Scholar] [CrossRef] [PubMed]
- Larange, A.; Cheroutre, H. Retinoic Acid and Retinoic Acid Receptors as Pleiotropic Modulators of the Immune System. Annu. Rev. Immunol. 2016, 34, 369–394. [Google Scholar] [CrossRef] [PubMed]
- Tanumihardjo, S.A. Vitamin A: Biomarkers of nutrition for development. Am. J. Clin. Nutr. 2011, 94, 658S–665S. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosio, D.N.; Clugston, R.D.; Blaner, W.S. Vitamin A metabolism: An update. Nutrients 2011, 3, 63–103. [Google Scholar] [CrossRef]
- Stephensen, C.B. Vitamin A, infection, and immune function. Annu. Rev. Nutr. 2001, 21, 167–192. [Google Scholar] [CrossRef]
- Imdad, A.; Mayo-Wilson, E.; Herzer, K.; Bhutta, Z.A. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst. Rev. 2017, 3, CD008524. [Google Scholar] [CrossRef]
- Penniston, K.L.; Tanumihardjo, S.A. The acute and chronic toxic effects of vitamin A. Am. J. Clin. Nutr. 2006, 83, 191–201. [Google Scholar] [CrossRef]
- DeBoer, M.D. Obesity, systemic inflammation, and increased risk for cardiovascular disease and diabetes among adolescents: A need for screening tools to target interventions. Nutrition 2013, 29, 379–386. [Google Scholar] [CrossRef]
- Pan, X.F.; Wang, L.; Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 373–392. [Google Scholar] [CrossRef]
- Zimmet, P.; Alberti, G.; Kaufman, F.; Tajima, N.; Silink, M.; Arslanian, S.; Wong, G.; Bennett, P.; Shaw, J.; Caprio, S.; et al. The metabolic syndrome in children and adolescents. Lancet 2007, 369, 2059–2061. [Google Scholar] [CrossRef]
- DeBoer, M.D. Assessing and Managing the Metabolic Syndrome in Children and Adolescents. Nutrients 2019, 11, 1788. [Google Scholar] [CrossRef] [PubMed]
- Kit, B.K.; Kuklina, E.; Carroll, M.D.; Ostchega, Y.; Freedman, D.S.; Ogden, C.L. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999–2012. JAMA Pediatr. 2015, 169, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Canas, J.A.; Beydoun, H.A.; Chen, X.; Shroff, M.R.; Zonderman, A.B. Serum antioxidant concentrations and metabolic syndrome are associated among U.S. adolescents in recent national surveys. J. Nutr. 2012, 142, 1693–1704. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Peng, R.; Cao, J.; Kang, Y.; Qu, P.; Liu, Y.; Xiao, X.; Li, T. Serum vitamin A status is associated with obesity and the metabolic syndrome among school-age children in Chongqing, China. Asia Pac. J. Clin. Nutr. 2016, 25, 563–570. [Google Scholar] [PubMed]
- Guerendiain, M.; Mayneris-Perxachs, J.; Montes, R.; López-Belmonte, G.; Martín-Matillas, M.; Castellote, A.I.; Martín-Bautista, E.; Martí, A.; Martínez, J.A.; Moreno, L.; et al. Relation between plasma antioxidant vitamin levels, adiposity and cardio-metabolic profile in adolescents: Effects of a multidisciplinary obesity programme. Clin. Nutr. 2017, 36, 209–217. [Google Scholar] [CrossRef]
- National Health and Family Planning Commission of People’s Republic of China. Method for Vitamin A Deficiency Screening; WS/T 553-2017; National Health and Family Planning Commission of People’s Republic of China: Beijing, China, 2018.
- National Health and Family Planning Commission of People’s Republic of China. Screening for Overweight and Obesity among School-Age Children and Adolescents; WST 586-2018; National Health and Family Planning Commission of People’s Republic of China: Beijing, China, 2018.
- Cook, S.; Weitzman, M.; Auinger, P.; Nguyen, M.; Dietz, W.H. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the third National Health and Nutrition Examination Survey, 1988–1994. Arch. Pediatr. Adolesc. Med. 2003, 157, 821–827. [Google Scholar] [CrossRef]
- Zhu, Q.; Dai, Y.; Zhang, J.; Xie, W.; Zuo, H.; Zhang, J.; Zhou, Y. Association between serum zinc concentrations and metabolic risk factors among Chinese children and adolescents. Br. J. Nutr. 2021, 126, 1529–1536. [Google Scholar] [CrossRef]
- Song, P.; Li, X.; Gasevic, D.; Flores, A.B.; Yu, Z. BMI, Waist Circumference Reference Values for Chinese School-Aged Children and Adolescents. Int. J. Environ. Res. Public Health 2016, 13, 598. [Google Scholar] [CrossRef]
- Dong, Y.; Ma, J.; Song, Y.; Dong, B.; Wang, Z.; Yang, Z.; Wang, X.; Prochaska, J.J. National Blood Pressure Reference for Chinese Han Children and Adolescents Aged 7 to 17 Years. Hypertension 2017, 70, 897–906. [Google Scholar] [CrossRef]
- Lee, J.M.; Okumura, M.J.; Davis, M.M.; Herman, W.H.; Gurney, J.G. Prevalence and determinants of insulin resistance among U.S. adolescents: A population-based study. Diabetes Care 2006, 29, 2427–2432. [Google Scholar] [CrossRef]
- Ford, E.S.; Li, C.; Cook, S.; Choi, H.K. Serum concentrations of uric acid and the metabolic syndrome among US children and adolescents. Circulation 2007, 115, 2526–2532. [Google Scholar] [CrossRef] [PubMed]
- Damanhoury, S.; Newton, A.S.; Rashid, M.; Hartling, L.; Byrne, J.; Ball, G. Defining metabolically healthy obesity in children: A scoping review. Obes. Rev. 2018, 19, 1476–1491. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, H.; Wang, Z.; Du, W.; Su, C.; Zhang, J.; Jiang, H.; Jia, X.; Huang, F.; Ouyang, Y.; et al. Prevalence and stabilizing trends in overweight and obesity among children and adolescents in China, 2011–2015. BMC Public Health 2018, 18, 571. [Google Scholar] [CrossRef] [PubMed]
- Song, P.; Yu, J.; Chang, X.; Wang, M.; An, L. Prevalence and Correlates of Metabolic Syndrome in Chinese Children: The China Health and Nutrition Survey. Nutrients 2017, 9, 79. [Google Scholar] [CrossRef] [PubMed]
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef]
- Yang, C.; Chen, J.; Liu, Z.; Yun, C.; Li, Y.; Piao, J.; Yang, X. Association of Vitamin A Status with Overnutrition in Children and Adolescents. Int. J. Environ. Res. Public Health 2015, 12, 15531–15539. [Google Scholar] [CrossRef]
- García, O.P.; Ronquillo, D.; del Carmen Caamaño, M.; Martínez, G.; Camacho, M.; López, V.; Rosado, J.L. Zinc, iron and vitamins A, C and e are associated with obesity, inflammation, lipid profile and insulin resistance in Mexican school-aged children. Nutrients 2013, 5, 5012–5030. [Google Scholar] [CrossRef]
- Vuralli, D.; Tumer, L.; Hasanoglu, A.; Biberoglu, G.; Pasaoglu, H. Vitamin A status and factors associated in healthy school-age children. Clin. Nutr. 2014, 33, 509–512. [Google Scholar] [CrossRef]
- Gunanti, I.R.; Marks, G.C.; Al-Mamun, A.; Long, K.Z. Low serum concentrations of carotenoids and vitamin E are associated with high adiposity in Mexican-American children. J. Nutr. 2014, 144, 489–495. [Google Scholar] [CrossRef]
- Aeberli, I.; Hurrell, R.F.; Zimmermann, M.B. Overweight children have higher circulating hepcidin concentrations and lower iron status but have dietary iron intakes and bioavailability comparable with normal weight children. Int. J. Obes. 2009, 33, 1111–1117. [Google Scholar] [CrossRef]
- Kim, T.; Kang, J. Association between Serum Retinol and α-Tocopherol Levels and Metabolic Syndrome in Korean General Population: Analysis of Population-based Nationally Representative Data. Nutrients 2020, 12, 1689. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Chen, X.; Jha, K.; Beydoun, H.A.; Zonderman, A.B.; Canas, J.A. Carotenoids, vitamin A, and their association with the metabolic syndrome: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 32–45. [Google Scholar] [CrossRef] [PubMed]
- Chatelaine, H.; Dey, P.; Mo, X.; Mah, E.; Bruno, R.S.; Kopec, R.E. Vitamin A and D Absorption in Adults with Metabolic Syndrome versus Healthy Controls: A Pilot Study Utilizing Targeted and Untargeted LC-MS Lipidomics. Mol. Nutr. Food Res. 2021, 65, e2000413. [Google Scholar] [CrossRef] [PubMed]
- Majerczyk, M.; Kocełak, P.; Choręza, P.; Arabzada, H.; Owczarek, A.J.; Bożentowicz-Wikarek, M.; Brzozowska, A.; Szybalska, A.; Puzianowska-Kuźnicka, M.; Grodzicki, T.; et al. Components of metabolic syndrome in relation to plasma levels of retinol binding protein 4 (RBP4) in a cohort of people aged 65 years and older. J. Endocrinol. Investig. 2018, 41, 1211–1219. [Google Scholar] [CrossRef] [PubMed]
- Wessel, H.; Saeed, A.; Heegsma, J.; Connelly, M.A.; Faber, K.N.; Dullaart, R. Plasma Levels of Retinol Binding Protein 4 Relate to Large VLDL and Small LDL Particles in Subjects with and without Type 2 Diabetes. J. Clin. Med. 2019, 8, 1792. [Google Scholar] [CrossRef]
- De Pee, S.; Dary, O. Biochemical indicators of vitamin A deficiency: Serum retinol and serum retinol binding protein. J. Nutr. 2002, 132, 2895S–2901S. [Google Scholar] [CrossRef]
- Wakil, S.J.; Abu-Elheiga, L.A. Fatty acid metabolism: Target for metabolic syndrome. J. Lipid Res. 2009, 50, S138–S143. [Google Scholar] [CrossRef]
- Amengual, J.; Petrov, P.; Bonet, M.L.; Ribot, J.; Palou, A. Induction of carnitine palmitoyl transferase 1 and fatty acid oxidation by retinoic acid in HepG2 cells. Int. J. Biochem. Cell Biol. 2012, 44, 2019–2027. [Google Scholar] [CrossRef]
- Yanagitani, A.; Yamada, S.; Yasui, S.; Shimomura, T.; Murai, R.; Murawaki, Y.; Hashiguchi, K.; Kanbe, T.; Saeki, T.; Ichiba, M.; et al. Retinoic acid receptor alpha dominant negative form causes steatohepatitis and liver tumors in transgenic mice. Hepatology 2004, 40, 366–375. [Google Scholar] [CrossRef]
- Albuquerque, M.N.; Diniz Ada, S.; Arruda, I.K. Elevated Serum Retinol and Low Beta-Carotene but not Alpha-Tocopherol Concentrations Are Associated with Dyslipidemia in Brazilian Adolescents. J. Nutr. Sci. Vitaminol. 2016, 62, 73–80. [Google Scholar] [CrossRef][Green Version]
- Gajewska, J.; Ambroszkiewicz, J.; Weker, H.; Chełchowska, M. Relations between oxidized low-density lipoproteins and fat-soluble vitamin concentrations in obese children—Preliminary study. Dev. Period. Med. 2017, 21, 266–271. [Google Scholar] [PubMed]
- Wang, N.; Ru, Y.; Yang, Z.; Sun, C.; Li, S.; Min, Y.; Zhao, X.; Lu, Y.; Hsing, A.W.; Zhu, S. Metabolomic Profiles of Plasma Retinol-Associated Dyslipidemia in Men and Women. Front. Nutr. 2021, 8, 740435. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Choi, H.K. Associations between concentrations of uric acid with concentrations of vitamin A and beta-carotene among adults in the United States. Nutr. Res. 2013, 33, 995–1002. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kim, Y.; Choi, J.H.; Kang, J.; Kim, G.T.; Lee, S.G. Associations of Serum Retinol and α-Tocopherol Levels with Uric Acid Concentrations: Analysis of a Population-Based, Nationally Representative Sample. Nutrients 2020, 12, 1797. [Google Scholar] [CrossRef] [PubMed]
- Taibi, G.; Nicotra, C.M. Xanthine oxidase catalyzes the oxidation of retinol. J. Enzyme Inhib. Med. Chem. 2007, 22, 471–476. [Google Scholar] [CrossRef] [PubMed]
| Variables | Serum Vitamin A Levels | p-Value | p for Trend | |||
|---|---|---|---|---|---|---|
| Q1 (n = 756) | Q2 (n = 757) | Q3 (n = 762) | Q4 (n = 750) | |||
| Age, years | 10.2 ± 2.7 | 10.8 ± 2.8 | 11.8 ± 3.0 | 12.8 ± 2.7 | <0.001 | <0.001 |
| Residence | <0.001 | <0.001 | ||||
| Urban | 596 (78.8) | 638 (84.3) | 655 (86.0) | 642 (85.6) | ||
| Rural | 160 (21.2) | 119 (15.7) | 107 (14.0) | 108 (14.4) | ||
| Physical activity | 0.114 | 0.151 | ||||
| Low | 460 (60.8) | 482 (63.7) | 442 (58.0) | 442 (58.9) | ||
| High | 296 (39.2) | 275 (36.3) | 320 (42.0) | 308 (41.1) | ||
| Screen time | 0.708 | 0.700 | ||||
| Low | 657 (86.9) | 672 (88.8) | 673 (88.3) | 658 (87.7) | ||
| High | 99 (13.1) | 85 (11.2) | 89 (11.7) | 92 (12.3) | ||
| Anthropometrics | ||||||
| Height (cm) | 141.8 (132.3, 155.2) | 146.6 (135.1, 160.2) | 155.6 (141.9, 164.4) | 160.0 (150.9, 168.0) | <0.001 | <0.001 |
| Weight (kg) | 34.5 (27.4, 46.0) | 39.1 (29.8, 50.6) | 47.2 (34.5, 57.2) | 52.6 (42.2, 63.1) | <0.001 | <0.001 |
| WC (cm) | 59.9 (54.3, 65.7) | 62.1 (56.4, 69.1) | 65.7 (59.0, 73.0) | 69.3 (62.9, 77.8) | <0.001 | <0.001 |
| BMI (kg/m2) | 16.8 (15.4, 19.2) | 17.8 (15.8, 20.4) | 19.1 (16.7, 22.0) | 20.5 (17.9, 23.3) | <0.001 | <0.001 |
| SBP (mmHg) | 111.7 (104.3, 119.3) | 114.0 (106.0, 122.3) | 115.7 (107.7, 123.7) | 117.3 (110.3, 125.7) | <0.001 | <0.001 |
| DBP (mmHg) | 66.7 (61.3, 73.0) | 67.0 (61.7, 73.3) | 67.3 (62.3, 72.3) | 69.0 (64.7, 74.0) | <0.001 | <0.001 |
| Biochemistry | ||||||
| FBG (mmol/L) | 5.2 (4.9, 5.5) | 5.2 (4.9, 5.5) | 5.3 (5.0, 5.6) | 5.3 (5.0, 5.6) | 0.010 | 0.036 |
| TG (mmol/L) | 0.7 (0.6, 0.9) | 0.8 (0.6, 1.0) | 0.8 (0.6, 1.1) | 1.0 (0.7, 1.3) | <0.001 | <0.001 |
| TC (mmol/L) | 3.9 (3.5, 4.3) | 4.1 (3.7, 4.6) | 4.0 (3.6, 4.5) | 4.1 (3.7, 4.7) | <0.001 | <0.001 |
| LDL (mmol/L) | 2.1 (1.8, 2.4) | 2.2 (1.9, 2.6) | 2.2 (1.8. 2.6) | 2.3 (1.9, 2.7) | <0.001 | <0.001 |
| HDL (mmol/L) | 1.6 (1.4, 1.9) | 1.6 (1.4, 1.9) | 1.6 (1.4, 1.9) | 1.5 (1.3, 1.8) | <0.001 | <0.001 |
| Serum Uric acid (μmol/L) | 270.0 (237.0, 314.8) | 296.0 (252.0) | 322.0 (278.0, 375.0) | 358.0 (300.8, 419.3) | <0.001 | <0.001 |
| Metabolic Condition | Serum Vitamin A Levels | p-Value | p for Trend | |||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |||
| Weight groups | <0.001 | <0.001 | ||||
| Others | 627 (82.9) | 587 (77.6) | 552 (72.4) | 474 (63.4) | ||
| Overweight | 71 (9.4) | 103 (13.6) | 114 (15.0) | 134 (17.9) | ||
| Obesity | 58 (7.7) | 66 (8.7) | 96 (12.6) | 140 (18.7) | ||
| Metabolic syndrome | <0.001 | <0.001 | ||||
| No | 740 (97.9) | 733 (96.8) | 726 (95.3) | 671 (89.5) | ||
| Yes | 16 (2.1) | 24 (3.2) | 36 (4.7) | 79 (10.5) | ||
| Obesity phenotype | <0.001 | <0.001 | ||||
| MHNO | 691 (91.4) | 679 (89.7) | 651 (85.4) | 586 (78.1) | ||
| MHO | 49 (6.5) | 54 (7.1) | 75 (9.8) | 85 (11.3) | ||
| MNHNO | 7 (0.9) | 12 (1.6) | 15 (2.0) | 24 (3.2) | ||
| MNHO | 9 (1.2) | 12 (1.6) | 21 (2.8) | 55 (7.3) | ||
| Metabolic Risk Factors | Vitamin A Quantiles | p for Trend | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Metabolic syndrome | |||||
| Model 1 | 1 (reference) | 1.514 (0.798–2.874) | 2.293 (1.261–4.169) | 5.445 (3.150–9.413) | <0.001 |
| Model 2 | 1 (reference) | 1.479 (0.777–2.813) | 2.244 (1.221–4.123) | 5.257 (2.968–9.310) | <0.001 |
| Central obesity | |||||
| Model 1 | 1 (reference) | 1.404 (1.037–1.899) | 1.961 (1.469–2.617) | 3.299 (2.503–4.349) | <0.001 |
| Model 2 | 1 (reference) | 1.444 (1.063–1.962) | 2.257 (1.674–3.042) | 4.135 (3.073–5.564) | <0.001 |
| Elevated blood pressure | |||||
| Model 1 | 1 (reference) | 1.065 (0.868–1.307) | 1.014 (0.826–1.245) | 1.059 (0.863–1.300) | 0.260 |
| Model 2 | 1 (reference) | 1.150 (0.934–1.416) | 1.224 (0.989–1.515) | 1.420 (1.114–1.770) | <0.001 |
| Elevated FBG | |||||
| Model 1 | 1 (reference) | 0.916 (0.515–1.629) | 1.282 (0.752–2.184) | 1.092 (0.628–1.900) | 0.733 |
| Model 2 | 1 (reference) | 0.835 (0.467–1.491) | 1.075 (0.619–1.868) | 0.820 (0.456–1.475) | 0.386 |
| Low HDL | |||||
| Model 1 | 1 (reference) | 0.637 (0.384–1.054) | 0.632 (0.382–1.047) | 0.798 (0.496–1.284) | 0.516 |
| Model 2 | 1 (reference) | 0.607 (0.364–1.013) | 0.549 (0.325–0.927) | 0.611 (0.366–1.018) | 0.121 |
| High TG | |||||
| Model 1 | 1 (reference) | 1.469 (1.030–2.096) | 2.003 (1.428–2.811) | 4.706 (3.439–6.441) | <0.001 |
| Model 2 | 1 (reference) | 1.515 (1.060–2.166) | 2.072 (1.466–2.930) | 4.903 (3.524–6.820) | <0.001 |
| General Obesity | |||||
| Model 1 | 1 (reference) | 1.149 (0.795–1.661) | 1.735 (1.231–2.444) | 2.762 (1.996–3.822) | <0.001 |
| Model 2 | 1 (reference) | 1.227 (0.843–1.784) | 2.277 (1.592–3.256) | 4.101(2.877–5.845) | <0.001 |
| High LDL | |||||
| Model 1 | 1 (reference) | 1.837 (1.054–3.204) | 1.825(1.046–3.182) | 2.798 (1.656–4.729) | <0.001 |
| Model 2 | 1 (reference) | 1.940 (1.109–3.394) | 2.156(1.223–3.799) | 3.779 (2.177–6.559) | <0.001 |
| High TC | |||||
| Model 1 | 1 (reference) | 1.868 (1.190–2.933) | 1.963 (1.255–3.069) | 2.753 (1.794–4.226) | <0.001 |
| Model 2 | 1 (reference) | 1.910 (1.213–3.008) | 2.125 (1.347–3.355) | 3.318 (2.115–5.205) | <0.001 |
| Hyperuricemia | |||||
| Model 1 | 1 (reference) | 1.750 (1.330–2.304) | 3.338 (2.575–4.326) | 6.816 (5.280–8.797) | <0.001 |
| Model 2 | 1 (reference) | 1.565 (1.167–2.099) | 2.641 (1.988–3.507) | 4.709 (3.552–6.242) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tian, T.; Wang, Y.; Xie, W.; Zhang, J.; Ni, Y.; Peng, X.; Sun, G.; Dai, Y.; Zhou, Y. Associations between Serum Vitamin A and Metabolic Risk Factors among Eastern Chinese Children and Adolescents. Nutrients 2022, 14, 610. https://doi.org/10.3390/nu14030610
Tian T, Wang Y, Xie W, Zhang J, Ni Y, Peng X, Sun G, Dai Y, Zhou Y. Associations between Serum Vitamin A and Metabolic Risk Factors among Eastern Chinese Children and Adolescents. Nutrients. 2022; 14(3):610. https://doi.org/10.3390/nu14030610
Chicago/Turabian StyleTian, Ting, Yuanyuan Wang, Wei Xie, Jingxian Zhang, Yunlong Ni, Xianzhen Peng, Guiju Sun, Yue Dai, and Yonglin Zhou. 2022. "Associations between Serum Vitamin A and Metabolic Risk Factors among Eastern Chinese Children and Adolescents" Nutrients 14, no. 3: 610. https://doi.org/10.3390/nu14030610
APA StyleTian, T., Wang, Y., Xie, W., Zhang, J., Ni, Y., Peng, X., Sun, G., Dai, Y., & Zhou, Y. (2022). Associations between Serum Vitamin A and Metabolic Risk Factors among Eastern Chinese Children and Adolescents. Nutrients, 14(3), 610. https://doi.org/10.3390/nu14030610







