Sugar-Sweetened Beverages and Symptom Complaints among School-Aged Children: A National Longitudinal Study
Abstract
:1. Introduction
2. Methods
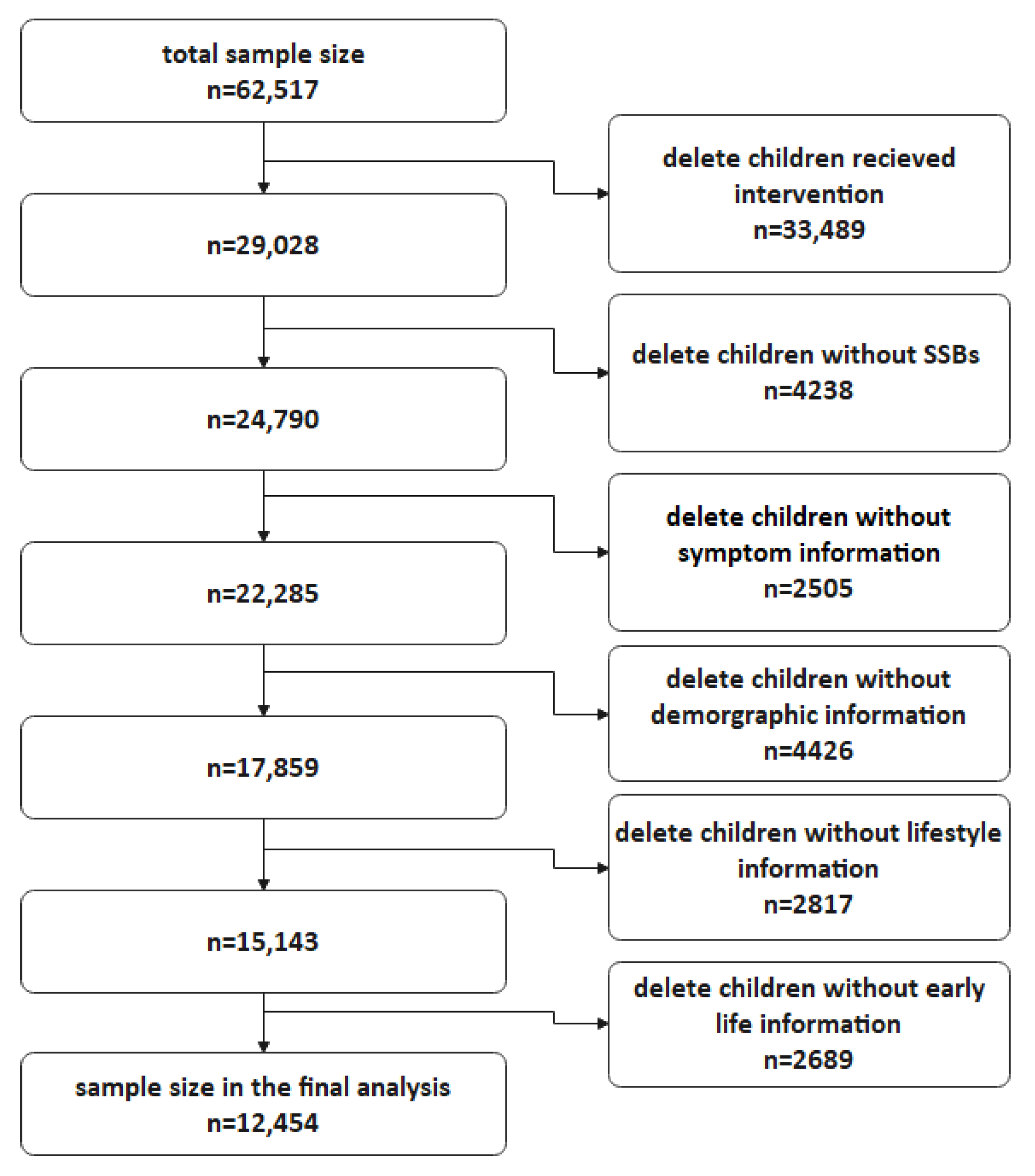
2.1. Participant Enrollment, Study Design, and Procedure
2.2. Questionnaire Survey
2.3. Exposure: Sugar-Sweetened Beverage Intake Amount and Frequency
2.4. Outcome: Symptoms
3. Covariates
3.1. Food Intake except for SSBs
3.2. Moderate Physical Activity, Sedentary Behavior, and Sleep Duration
3.3. Early Life History
3.4. Statistical Analysis
4. Results
| Characteristics | Overall (n = 12,454) | Symptom Presence | p-Value | ||
|---|---|---|---|---|---|
| Yes (n = 4345) | No (n = 8109) | ||||
| Age (year) | 10.32 (3.15) | 10.44 (3.18) | 10.26 (3.14) | 0.002 | |
| Child gender (%) | Boys | 6059 (48.7) | 1929 (31.8) | 4130 (68.2) | <0.001 |
| Girls | 6395 (51.3) | 2416 (37.8) | 3979 (62.2) | ||
| Ethnic background (%) | Han | 11,880 (95.4) | 4117 (34.7) | 7763 (65.3) | 0.013 |
| Minority | 574 (4.6) | 228 (39.7) | 346 (60.3) | ||
| Maternal education level (%) | 9 years or below | 6227 (50.0) | 2334 (37.5) | 3893 (62.5) | <0.001 |
| 9–12 years | 3219 (25.8) | 1061 (33.0) | 2158 (67.0) | ||
| 13–15 years | 1705 (13.7) | 532 (31.2) | 1173 (68.8) | ||
| 16 years or above | 1303 (10.5) | 418 (32.1) | 885 (67.9) | ||
| Residence (%) | Urban | 7525 (60.4) | 2449 (32.5) | 5076 (67.5) | <0.001 |
| Rural | 4929 (39.6) | 1896 (38.5) | 3033 (61.5) | ||
| Household income per month (%) | CNY 5000 or below | 4014 (32.2) | 1501 (37.4) | 2513 (62.6) | <0.001 |
| CNY 5001–12,000 | 3756 (30.2) | 1253 (33.4) | 2503 (66.6) | ||
| CNY 12,001 or above | 1246 (10.0) | 402 (32.3) | 844 (67.7) | ||
| Refused to answer | 3438 (27.6) | 1189 (34.6) | 2249 (65.4) | ||
| Research area (%) | Eastern and southern coast | 4289 (34.4) | 1267 (29.5) | 3022 (70.5) | <0.001 |
| Northern | 4530 (36.4) | 1694 (37.4) | 2836 (62.6) | ||
| Middle and western | 3635 (29.2) | 1384 (38.1) | 2251 (61.9) | ||
| Daily moderate physical activity time (%) | 0.75 h or less | 4320 (34.7) | 1523 (34.3) | 2797 (65.7) | 0.603 |
| 0.75–3 h | 4234 (34.0) | 1452 (34.3) | 2782 (65.7) | ||
| 3 h or more | 3900 (31.3) | 1370 (35.1) | 2530 (64.9) | ||
| Daily sedentary lifestyle time (%) | 2.5 h or less | 3340 (26.8) | 1186 (35.5) | 2154 (64.5) | 0.634 |
| 2.5–6.5 h | 3989 (32.0) | 1391 (34.9) | 2598 (65.1) | ||
| 6.5 h or more | 5125 (41.2) | 1768 (34.5) | 3357 (65.5) | ||
| Daily sleep time (%) | 7 h or less | 3423 (27.5) | 1178 (39.5) | 2245 (60.5) | <0.001 |
| 7–9 h | 7406 (59.5) | 2525 (34.1) | 4881 (65.9) | ||
| 9 h or more | 1625 (13.0) | 642 (34.4) | 983 (65.6) | ||
| Consumption of vegetables (%) | 0–6 serves/week | 2511 (20.3) | 892 (35.5) | 1619 (64.5) | 0.211 |
| 7–14 serves/week | 7228 (58.4) | 2478 (34.3) | 4750 (65.7) | ||
| 15 or more serves/week | 2634 (21.3) | 949 (36.0) | 1685 (64.0) | ||
| Consumption of fruits (%) | 0–5 serves/week | 4012 (32.5) | 1400 (34.9) | 2612 (65.1) | 0.577 |
| 6–11 serves/week | 4913 (39.8) | 1735 (35.3) | 3178 (64.7) | ||
| 12 or more serves/week | 3418 (27.7) | 1169 (34.2) | 2249 (65.8) | ||
| Consumption of meats (%) | 0–4 serves/week | 4437 (36.0) | 1586 (35.7) | 1636 (34.2) | 0.314 |
| 5–7 serves/week | 4779 (38.8) | 1636 (34.2) | 3143 (65.8) | ||
| 8 or more serves/week | 3113 (25.2) | 1090 (35.0) | 2023 (65.0) | ||
| Sugar-sweetened beverage intake amount (SSBsM, %) | Never | 4385 (35.2) | 1425 (32.5) | 2960 (67.5) | <0.001 |
| Small amount (no more than 75 mL per day) | 4873 (39.1) | 1677 (34.4) | 3196 (65.6) | ||
| Large amount (75 mL or more per day) | 3196 (25.7) | 1243 (38.9) | 1953 (61.1) | ||
| Sugar-sweetened beverage intake frequency (SSBsF, %) | Never | 4385 (35.2) | 1425 (32.5) | 2960 (67.5) | <0.001 |
| Twice or less per week | 5594 (44.9) | 1976 (35.3) | 3618 (64.7) | ||
| Three times or more per week | 2475 (19.9) | 944 (38.1) | 1531 (61.9) | ||
| Birth weight (%) | Normal | 11,229 (90.2) | 3896 (34.7) | 7333 (65.3) | 0.196 |
| Low birthweight | 374 (3.0) | 128 (34.2) | 246 (65.8) | ||
| Macrosomia | 851 (6.8) | 321 (37.7) | 530 (62.3) | ||
| Breast feeding less than 6 months (%) | Yes | 4615 (37.1) | 1552 (33.6) | 3063 (66.4) | 0.024 |
| No | 7839 (62.9) | 3063 (35.6) | 5046 (64.4) | ||
| Characteristics | Never (n = 4385) | Small Amount (n = 4873) | Large Amount (n = 3196) | p-Value | |
|---|---|---|---|---|---|
| Age (year) | 9.91 (2.98) | 9.99 (3.03) | 11.40 (3.32) | <0.001 | |
| Child gender (%) | Boys | 1967 (44.9) | 2324 (47.7) | 1768 (55.3) | <0.001 |
| girls | 2418 (55.1) | 2549 (52.3) | 1428 (44.7) | ||
| Ethnic background (%) | Han | 4175 (95.2) | 4663 (95.7) | 3042 (95.2) | 0.441 |
| Minority | 210 (4.8) | 210 (4.3) | 154 (4.8) | ||
| Maternal education level (%) | 9 years or below | 2126 (48.5) | 2344 (48.1) | 1757 (55.0) | <0.001 |
| 9–12 years | 1070 (24.4) | 1320 (27.1) | 829 (25.9) | ||
| 13–15 years | 658 (15.0) | 695 (14.3) | 352 (11.0) | ||
| 16 years or above | 531 (12.1) | 514 (10.5) | 258 (8.1) | ||
| Residence (%) | Urban | 2666 (60.8) | 3042 (62.1) | 1835 (57.4) | <0.001 |
| Rural | 1719 (39.2) | 1849 (37.9) | 1361 (42.6) | ||
| Household income per month (%) | CNY 5000 or below CNY 5001–12,000 | 1445 (33.0) | 1502 (30.8) | 1067 (33.4) | 0.082 |
| 1275 (29.1) | 1523 (31.3) | 958 (30.0) | |||
| CNY 12,001 or above Refused to answer | 435 (9.9) | 509 (10.4) | 302 (9.4) | ||
| 1230 (28.1) | 1339 (27.5) | 869 (7.0) | |||
| Research area (%) | Easter and southern coast | 1620 (36.9) | 1678 (34.4) | 991 (31.0) | <0.001 |
| Northern | 1530 (34.9) | 1790 (36.7) | 1210 (37.9) | ||
| Middle and western | 1235 (28.2) | 1405 (28.8) | 995 (31.1) | ||
| Daily physical activity time (%) | 0.75 h or less | 1700 (38.8) | 1585 (32.5) | 1035 (32.4) | <0.001 |
| 0.75–3 h | 1391 (31.7) | 1769 (36.3) | 1074 (33.6) | ||
| 3 h or more | 1294 (29.5) | 1519 (31.2) | 1087 (34.0) | ||
| Daily sedentary lifestyle time (%) | 2.5 h or less | 1185 (27.0) | 1354 (27.8) | 801 (25.1) | <0.001 |
| 2.5–6.5 h | 1447 (33.0) | 1612 (33.1) | 930 (29.1) | ||
| 6.5 h or more | 1753 (40.0) | 1907 (39.1) | 1465 (45.8) | ||
| Daily sleep time (%) | 9 h or more | 1349 (30.8) | 1429 (29.3) | 645 (20.2) | <0.001 |
| 7–9 h | 2579 (58.8) | 2902 (59.6) | 1925 (60.2) | ||
| 7 h or less | 457 (10.4) | 542 (11.1) | 626 (19.6) | ||
| Consumption of vegetables (%) | 0–6 serves/week | 700 (16.1) | 1032 (21.3) | 779 (24.5) | <0.001 |
| 7–14 serves/week | 2631 (60.5) | 2884 (59.5) | 1713 (53.9) | ||
| 15 or more serves/week | 1016 (23.4) | 932 (19.2) | 686 (21.6) | ||
| Consumption of fruits (%) | 0–5 serves/week | 1341 (30.8) | 1642 (34.0) | 1029 (32.5) | 0.001 |
| 6–11 serves/week | 1797 (41.3) | 1908 (39.6) | 1208 (38.1) | ||
| 12 or more serves/week | 1211 (27.8) | 1274 (26.4) | 933 (29.4) | ||
| Consumption of meats (%) | 0–4 serves/week | 1664 (38.4) | 1855 (38.4) | 918 (29.0) | <0.001 |
| 5–7 serves/week | 1708 (39.4) | 1906 (39.5) | 1165 (36.8) | ||
| 8 or more serves/week | 964 (22.2) | 1067 (22.1) | 1082 (34.2) | ||
| Sugar-sweetened beverage intake frequency (SSBsF, %) | Never | 4385 (100) | 0 (0) | 0 (0) | <0.001 |
| Twice or less per week | 0 (0) | 4776 (98.0) | 818 (25.6) | ||
| Three times or more per week | 0 (0) | 97 (2.0) | 2378 (74.4) | ||
| Birth weight (%) | Normal | 3980 (90.8) | 4408 (90.5) | 2841 (88.9) | <0.001 |
| Low birthweight | 148 (3.4) | 141 (2.9) | 85 (2.7) | ||
| Macrosomia | 257 (5.9) | 324 (6.6) | 270 (8.4) | ||
| Breast feeding less than 6 months (%) | Yes | 1633 (37.2) | 1834 (37.6) | 1148 (35.9) | 0.281 |
| No | 2752 (62.8) | 3039 (62.4) | 2048 (64.1) | ||
| Symptom reported (%) | Yes | 1425 (32.5) | 1677 (34.4) | 1243 (38.9) | <0.001 |
| No | 2960 (67.5) | 3196 (65.6) | 1953 (61.1) | ||
5. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Malik, V.S.; Hu, F.B. Sugar-sweetened beverages and cardiometabolic health: An update of the evidence. Nutrients 2019, 11, 1840. [Google Scholar] [CrossRef] [Green Version]
- Seferidi, P.; Millett, C.; Laverty, A.A. Sweetened beverage intake in association to energy and sugar consumption and cardiometabolic markers in children. Pediatr. Obes. 2018, 13, 195–203. [Google Scholar] [CrossRef]
- Li, S.; Cao, M.; Yang, C.; Zheng, H.; Zhu, Y. Association of sugar-sweetened beverage intake with risk of metabolic syndrome among children and adolescents in urban China. Public Health Nutr. 2020, 23, 2770–2780. [Google Scholar] [CrossRef]
- Nieswand, V.; Richter, M.; Berner, R.; Von Der Hagen, M.; Klimova, A.; Roeder, I.; Koch, T.; Sabatowski, R.; Gossrau, G. The prevalence of headache in German pupils of different ages and school types. Cephalalgia 2019, 39, 1030–1040. [Google Scholar] [CrossRef]
- Groenewald, C.B.; Giles, M.; Palermo, T.M. School absence associated with childhood pain in the United States. Clin. J. Pain 2019, 35, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Klausen, S.H.; Rønde, G.; Tornøe, B.; Bjerregaard, L. Nonpharmacological interventions addressing pain, sleep, and quality of life in children and adolescents with primary headache: A systematic review. J. Pain Res. 2019, 12, 3437–3459. [Google Scholar] [CrossRef] [Green Version]
- Steenbruggen, T.G.; Hoekstra, S.J.; Van Der Gaag, E.J. Could a change in diet revitalize children who suffer from unresolved fatigue? Nutrients 2015, 7, 1965–1977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferreira, A.V.M.; Mario, G.; Porto, L.C.J.; Andrade, S.P.; Botion, L.M. High-carbohydrate diet selectively induces tumor necrosis factor-α production in mice liver. Inflammation 2011, 34, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Shearrer, G.; Daniels, M.; Toledo-Corral, C.; Weigensberg, M.; Spruijt-Metz, D.; Davis, J. Associations among sugar sweetened beverage intake, visceral fat, and cortisol awakening response in minority youth. Physiol. Behav. 2016, 167, 188–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, D.; Jin, W.; Wu, R.; Li, J.; Park, S.-A.; Tu, E.; Zanvit, P.; Xu, J.; Liu, O.; Cain, A.; et al. High glucose intake exacerbates autoimmunity through reactive-oxygen-species-mediated TGF-β cytokine activation. Immunity 2019, 51, 671–681. [Google Scholar] [CrossRef]
- Sawani, A.; Farhangi, M.; Maul, T.M.; Parthasarathy, S.; Smallwood, J.; Wei, J.L. Limiting dietary sugar improves pediatric sinonasal symptoms and reduces inflammation. J. Med. Food 2018, 21, 527–534. [Google Scholar] [CrossRef]
- Hu, D.; Cheng, L.; Jiang, W. Sugar-sweetened beverages consumption and the risk of depression: A meta-analysis of observational studies. J. Affect. Disord. 2019, 245, 348–355. [Google Scholar] [CrossRef]
- Edgcomb, J.B.; Tseng, C.-H.; Kerner, B. Medically unexplained somatic symptoms and bipolar spectrum disorders: A systematic review and meta-analysis. J. Affect. Disord. 2016, 204, 205–213. [Google Scholar] [CrossRef]
- Giacobo, R.S.; Jané, M.C.; Bonillo, A.; Ballespí, S.; Díaz-Regañon, N. Somatic symptoms, severe mood dysregulation, and aggressiveness in preschool children. Eur. J. Pediatr. 2012, 171, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Bagayogo, I.P.; Interian, A.; Escobar, J.I. Transcultural aspects of somatic symptoms in the context of depressive disorders. Cult. Psychiatry 2013, 33, 64–74. [Google Scholar] [CrossRef]
- Chen, Y.; Ma, L.; Ma, Y.; Wang, H.; Luo, J.; Zhang, X.; Luo, C.; Wang, H.; Zhao, H.; Pan, D.; et al. A national school-based health lifestyles interventions among Chinese children and adolescents against obesity: Rationale, design and methodology of a randomized controlled trial in China. BMC Public Health 2015, 15, 210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- FFisher, J.D.; Amico, K.R.; Fisher, W.A.; Harman, J.J. The information-motivation-behavioral skills model of antiretroviral adherence and its applications. Curr. HIV AIDS Rep. 2008, 5, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Cao, M.; Zhu, Y.; Li, X.; Chen, Y.; Ma, J.; Jing, J. Gender-dependent association between sleep duration and overweight incidence in CHINESE school children: A national follow-up study. BMC Public Health 2018, 18, 615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chinese Nutrition Society. Dietary Guidelines for Chinese School-Age Children-2016, 3rd ed.; People’s Medical Publishing House: Beijing, China, 2016. [Google Scholar]
- Tucker, R.M.; Tan, S.-Y. Do non-nutritive sweeteners influence acute glucose homeostasis in humans? A systematic review. Physiol. Behav. 2017, 182, 17–26. [Google Scholar] [CrossRef]
- Lee, A.H.; Dixit, V.D. Dietary regulation of immunity. Immunity 2020, 53, 510–523. [Google Scholar] [CrossRef]
- Rogero, M.M.; Calder, P.C. Obesity, inflammation, toll-like receptor 4 and fatty acids. Nutrients 2018, 10, 432. [Google Scholar] [CrossRef] [Green Version]
- Thaiss, C.A.; Levy, M.; Grosheva, I.; Zheng, D.; Soffer, E.; Blacher, E.; Braverman, S.; Tengeler, A.C.; Barak, O.; Elazar, M.; et al. Hyperglycemia drives intestinal barrier dysfunction and risk for enteric infection. Science 2018, 359, 1376–1383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Feltz-Cornelis, C.M.; Bakker, M.; Kaul, A.; Kuijpers, T.W.; von Känel, R.; Sluijs, J.F.V.E.V.D. IL-6 and hsCRP in Somatic Symptom Disorders and related disorders. Brain Behav. Immun. Health 2020, 9, 100176. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Creed, F.H.; Ma, Y.-L.; MC Leung, C. Somatic symptom burden and health anxiety in the population and their correlates. J. Psychosom. Res. 2015, 78, 71–76. [Google Scholar] [CrossRef]
- Jacques, A.; Chaaya, N.; Beecher, K.; Ali, S.A.; Belmer, A.; Bartlett, S. The impact of sugar consumption on stress driven, emotional and addictive behaviors. Neurosci. Biobehav. Rev. 2019, 103, 178–199. [Google Scholar] [CrossRef] [PubMed]
- Falbe, J.; Thompson, H.R.; Patel, A.; Madsen, K.A. Potentially addictive properties of sugar-sweetened beverages among adolescents. Appetite 2018, 133, 130–137. [Google Scholar] [CrossRef]
- Wang, G.-J.; Freeman, C.R.; Zehra, A.; Ramirez, V.; E Wiers, C.; Volkow, N.D. Impact of sugar on the body brain and behavior. Front. Biosci. 2018, 23, 2255–2266. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.-J.; Du, J.-C.; Chiou, H.-C.; Feng, C.-C.; Chung, M.-Y.; Yang, W.; Chen, Y.-S.; Chien, L.-C.; Hwang, B.; Chen, M.-L. Sugar-sweetened beverage consumption is adversely associated with childhood attention deficit/hyperactivity disorder. Int. J. Environ. Res. Public Health 2016, 13, 678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Z.M.; Parker, L.; Dummer, T.J.B. Associations of coffee, diet drinks, and non-nutritive sweetener use with depression among populations in Eastern Canada. Sci. Rep. 2017, 7, 6255. [Google Scholar] [CrossRef]
- Trasande, L.; Shaffer, R.M.; Sathyanarayana, S. Food additives and child health. Pediatrics 2018, 142, e20181408. [Google Scholar] [CrossRef] [Green Version]
- Scharf, R.J.; DeBoer, M.D. Sugar-sweetened beverages and children’s health. Annu. Rev. Public Health 2016, 37, 273–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gan, Q.; Xu, P.; Yang, T.; Cao, W.; Xu, J.; Li, L.; Pan, H.; Zhao, W.; Zhang, Q. Sugar-sweetened beverage consumption status and its association with childhood obesity among chinese children aged 6–17 years. Nutrients 2021, 13, 2211. [Google Scholar] [CrossRef]
- Della Corte, K.; Fife, J.; Gardner, A.; Murphy, B.L.; Kleis, L.; Della Corte, D.; Schwingshackl, L.; LeCheminant, J.D.; Buyken, A.E. World trends in sugar-sweetened beverage and dietary sugar intakes in children and adolescents: A systematic review. Nutr. Rev. 2021, 79, 274–288. [Google Scholar] [CrossRef] [PubMed]
- Jia, P.; Liu, L.; Xie, X.; Yuan, C.; Chen, H.; Guo, B.; Zhou, J.; Yang, S. Changes in dietary patterns among youths in China during COVID-19 epidemic: The COVID-19 impact on lifestyle change survey (COINLICS). Appetite 2021, 158, 105015. [Google Scholar] [CrossRef] [PubMed]
| Crude Model a | Adjusted Model 1 b | Adjusted Model 2 c | ||
|---|---|---|---|---|
| Sugar-sweetened beverage intake amount | Never | Reference | Reference | Reference |
| Small amount | 1.09 (1.00–1.19) | 1.09 (1.00–1.19) * | 1.09 (1.00–1.19) * | |
| Large amount | 1.32 (1.20–1.45) * | 1.33 (1.20–1.47) * | 1.32 (1.20–1.46) * | |
| Sugar-sweetened beverage intake frequency | Never | Reference | Reference | Reference |
| Twice or less per week | 1.13 (1.04–1.23) * | 1.14 (1.04–1.24) * | 1.13 (1.04–1.23) * | |
| Three times or more per week | 1.28 (1.16–1.42) * | 1.29 (1.17–1.44) * | 1.28 (1.16–1.43) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, M.; Zhu, Y.; Chen, Y.; Jing, J. Sugar-Sweetened Beverages and Symptom Complaints among School-Aged Children: A National Longitudinal Study. Nutrients 2022, 14, 406. https://doi.org/10.3390/nu14030406
Cao M, Zhu Y, Chen Y, Jing J. Sugar-Sweetened Beverages and Symptom Complaints among School-Aged Children: A National Longitudinal Study. Nutrients. 2022; 14(3):406. https://doi.org/10.3390/nu14030406
Chicago/Turabian StyleCao, Muqing, Yanna Zhu, Yajun Chen, and Jin Jing. 2022. "Sugar-Sweetened Beverages and Symptom Complaints among School-Aged Children: A National Longitudinal Study" Nutrients 14, no. 3: 406. https://doi.org/10.3390/nu14030406
APA StyleCao, M., Zhu, Y., Chen, Y., & Jing, J. (2022). Sugar-Sweetened Beverages and Symptom Complaints among School-Aged Children: A National Longitudinal Study. Nutrients, 14(3), 406. https://doi.org/10.3390/nu14030406






