Abstract
Few studies have analyzed the implementation of dietary management in Chinese adults with diabetes. Thus, we assessed and compared dietary intake and diet quality between diabetic patients with and without dietary management behaviors (DPDM vs. NDPDM), and evaluated the adherence to dietary guidelines in both groups of patients. The data were obtained from the 2002, 2010–2013, and 2015 China National Nutrition Survey. A total of 69,583, 67,177, and 96,631 subjects participated in the 2002, 2010–2013, and 2015 survey rounds, respectively. The dietary intake data were measured using 3-day 24 h dietary recalls and weighed records of household condiments. The China Healthy Diet Index (CHDI) was used to evaluate diet quality. The study included 6229 patients with diabetes, of which 78% had dietary management behaviors. The diabetic patients with dietary management behaviors showed higher percentages of energy from high-quality carbohydrates, animal protein, saturated fatty acids, and unsaturated fatty acids and lower percentages from low-quality carbohydrates and plant protein than NDPDM. The diabetic patients with dietary management behaviors also had lower intakes of cereals and tubers and higher intakes of vegetables than NDPDM. The total CHDI score of DPDM was higher than NDPDM (56.3 ± 12.7 vs. 54.1 ± 12.3). The proportion of DPDM meeting the recommended intake for different food items ranged from 3.3% to 42.8% and from 3.0% to 39.2% in NDPDM. The diabetic patients with dietary management behaviors showed better adherence to dietary guidelines and higher diet quality scores than NDPDM, while the overall adherence was poor in both groups of patients. Our findings suggested that measures are needed to promote and refine dietary management behaviors, which can help to improve disease management in diabetic patients.
1. Introduction
Diabetes is one of the most predominant chronic diseases nowadays. In 2021, an estimated 10.5% (537 million) of adults aged 20–79 years were living with diabetes globally, and the number is forecast to grow to 12.2% (783 million) by 2045 [1]. With the aging population and increasing obesity prevalence, diabetes has become an important public health issue in China with a prevalence of 12.8% in 2017 [2]. Dietary management is the cornerstone of diabetes management, which is essential to maintaining glycemic control and reducing the risk of diabetes-related complications [3,4]. Guidelines for diabetes management across different countries have emphasized the importance of conducting dietary management in all patients with diabetes [5,6]. However, adherence to dietary recommendations is a highly challenging task for patients with diabetes, as it usually requires long-term defiance of the patient’s own food cravings and preferences [7,8]. Therefore, it is important to evaluate dietary intake in diabetic patients based on current clinical practice to provide detailed guidance on dietary plans and improve patient management.
Several prior studies have analyzed the dietary intake in diabetic patients and their adherence to dietary guidelines where the dietary pattern and rate of adherence varied greatly in different study populations [9,10,11]. A few studies have analyzed the dietary adherence among diabetic populations in China, where most studies reported low adherence to dietary guidelines [12,13]. However, most of these studies had a small sample size and were not nationally representative. In addition, most previous studies focused on the whole diabetes population without considering whether they had conducted anti-diabetic dietary management behaviors, and these two groups of patients may benefit from different intervention strategies [14]. To the best of our knowledge, few studies have analyzed the implementation of dietary management in Chinese adults with diabetes.
In this study, we used three rounds of nationally representative data to assess and compare dietary intakes and diet quality between diabetic patients with and without dietary management behaviors (DPDM vs. NDPDM), and evaluated the adherence to dietary guidelines in both groups of patients. This study provided a theoretical basis for promoting and refining dietary management behaviors, which can help to improve disease management in diabetic patients.
2. Materials and Methods
2.1. Study Population and Sampling
We analyzed data from the 2002, 2010–2013 (2012), and 2015 China National Nutrition Survey (CNNS), which is one of the most representative national cross-sectional surveys in China. The specific study design has been described elsewhere [15]. Briefly, in the 2002, 2012, and 2015 CNNS, subjects were selected from the resident population of 31 provinces, autonomous regions, and municipalities (except Taiwan, Hong Kong, and Macao) in China. All these studies used multi-stage stratified cluster random sampling. A total of 69,583, 67,177, and 96,631 subjects participated in the dietary survey across the three rounds of CNNS, respectively. The inclusion criteria for this study included: (a) subjects who completed the dietary recall for at least 2 days; (b) aged 18 years or older; (c) those with doctor-diagnosed diabetes. The exclusion criteria were as follows: (a) subjects were pregnant or lactating women; (b) with daily energy intake of less than 800 kcal or greater than 5000 kcal; (c) with missing information on self-reported dietary management behavior. We identified 64,067, 62,960, and 83,538 adults with diabetes that completed at least 2 days of the dietary recall in 2002, 2012, and 2015, respectively, and a total of 6229 patients with diabetes were included in the final analysis (Figure 1).
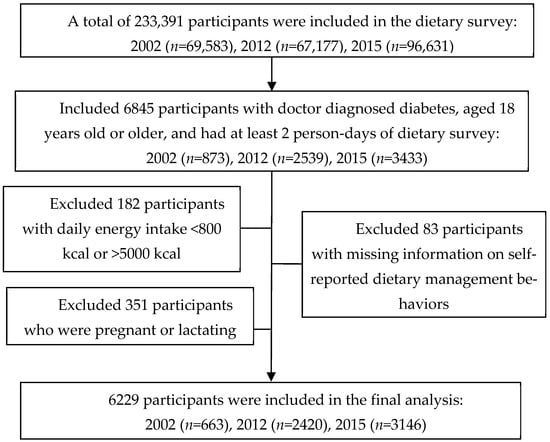
Figure 1.
Flow of inclusion into the study.
The series of CNNS was approved by the ethics committee of the National Institute for Nutrition and Health at the Chinese Center for Disease Control and Prevention (201519-A and 201614). All the subjects signed informed consent before the investigation.
2.2. Data Collection and Measurements
Sociodemographic characteristics were collected using questionnaires, including age, gender, marital status, education, occupation, and annual income. The questionnaire also collected data on the diagnosis of diabetes by doctors and whether the subject conducted dietary management behaviors for glycemic control. Height and weight were measured in the morning before breakfast. Fasting plasma glucose and HbA1c were measured by the hexokinase G-6-PDH method and HPLC method, respectively. All measurements were conducted with the Hitachi 7600 automated bio3chemical analyzer and all reagents were produced by Wako Pure Chemical, Ltd. (Richmond, VA, USA).
2.3. Definitions of Diabetic Patients and Dietary Management
In the three CNNS rounds, participants were asked whether they had ever been diagnosed with diabetes, and if they answered yes, they were followed up with questions about what measures they had taken over the past year to control blood sugar. The diabetic patients were defined as participants once diagnosed as having diabetes mellitus. The categorization for dietary management in patients with diabetes was based on the history of dietary management reported in the questionnaire.
2.4. Dietary Assessment
Dietary intake was assessed using 24 h dietary recall for three consecutive days (including two weekdays and one weekend) in addition to weighing household cooking oil and condiments. Food intake during the past 24 h was reported by participants for each dietary recall day, and the household cooking oil and condiments were weighed by investigators at the beginning and end of each 24 h. The recall was assisted by an interviewer to ensure accurate information was collected. Nutrient intakes were calculated based on the China Food Composition Tables, which are updated every few years to capture commonly consumed foods and changes in nutrient composition [16,17]. The percentage of participants meeting the recommendations for nutrient intake was evaluated according to the Guidelines for the Prevention and Treatment of Type 2 Diabetes Milieus in China (2020 Edition), which recommends 50–65% of total energy intake comes from carbohydrates, 15–20% from proteins, and 20–30% from fat, and daily fiber consumption should be greater than 14 g/1000 kcal [6]. We further subdivided carbohydrates into high-quality carbohydrates and low-quality carbohydrates, proteins into animal proteins and plant proteins, and fats into saturated fatty acids, monounsaturated fatty acids, and polyunsaturated fatty acids, as described in detail in previous articles [18]. Foods were classified into ten major categories according to the 2016 Dietary Guidelines for Chinese Residents, and the percentage of participants meeting the dietary guidelines was evaluated based on the following recommended levels: 250–400 g of cereals and tubers per day; 25–35 g of soybeans and nuts per day; 300–500 g of vegetables per day; 200–350 g of fruits per day; 40–75 g of livestock and poultry meats per day; greater than 300 g of dairy products per day; 40–50 g of eggs per day; 40–75 g of aquatic products per day; 25–30 g of oil per day; and less than 6 g of salt per day [19].
We used the China Healthy Diet Index (CHDI) [20] to evaluate the diet quality of the patients. The CHDI was established based on the 2016 Dietary Guidelines for Chinese Residents [19,20]. The standards for scoring are presented in Table S1. In this study, we included 13 items, including food variety, refined cereals and tubers, whole grains, dry beans and tubers, total vegetables, dark green and orange vegetables, fruit, dairy, soybeans, meat and egg, fish, shellfish and mollusk, sodium, calories from saturated fatty acids (SFAs), and empty calories. The total score ranged from 0 to 100, with higher scores representing better diet quality.
2.5. Statistical Analysis
We obtained and applied post-stratified population sampling weights derived from the sampling probabilities of the Chinese population aged 18 years or older in 2010 (based on census data) [21]. Means and 95% confidence intervals (CIs) were calculated for weight-adjusted dietary intake. Data were log-transformed before analysis if they were non-normal distribution. The CHDI score was calculated for DPDM and NDPDM in the total population and the stratified population by survey round, age, gender, and area of residence. We compared total energy, the percentages of macronutrients contributing to energy, absolute intake of food groups, and diet quality between DPDM and NDPDM using the Chi-square test for categorical variables, and t-test or ANOVA was used for continuous variables. We calculated the adjusted p-value using a general linear model to adjust for gender and area and annual income per capita. Two-sided p < 0.05 was statistically significant. Statistical analyses were conducted using SPSS 25.0 software (IBM SPSS, Inc., Chicago, IL, USA).
3. Results
3.1. Participant Characteristics
A flow diagram of the diabetic patients in the study is presented in Figure 1. A total of 6229 adults with diabetes were included in this study, including 663, 2420, and 3146 patients from the 2002, 2012, and 2015 survey rounds, respectively. The average age was 61.6 years old (range 18.0 to 96.0 years old), and 48.7% of patients were male. The average HbA1c of the included patients was 6.8 ± 1.8% (Table 1). The demographic characteristics were similar across the patients from the three survey rounds (Table S2). In this study, 78.0% of the patients reported having dietary management behaviors. The diabetic patients with dietary management behaviors were more likely to be females, urban residents, and had higher income levels. Body mass index and levels of HbA1c and blood plasma glucose were similar between DPDM and NDPDM.

Table 1.
Characteristics of adults with diabetes in the three rounds of China National Nutrition Surveys.
3.2. Dietary Intake
A comparison of dietary intake between DPDM and NDPDM is shown in Table 2. The total energy was 1756.0 and 1821.1 kcal/day for DPDM and NDPDM, respectively, and no significant difference was observed after adjustment for gender, area, and annual income per capita. After adjustment, compared to NDPDM, DPDM showed a lower estimated percentage of energy from carbohydrates (52.0 vs. 53.5%, p = 0.001), specifically a higher estimated percentage of energy from high-quality carbohydrates (5.3 vs. 4.6%, p = 0.026) and a lower estimated percentage of energy from low-quality carbohydrates (46.7 vs. 48.8%, p < 0.001). Although there was no statistical difference in the estimated percentage of energy from protein between the two groups, DPDM had a higher estimated percentage of energy from animal protein (4.8 vs. 4.3%, p = 0.015) and a lower estimated percentage of energy from plant protein (7.4 vs. 7.5%, p = 0.030) than NDPDM. The diabetic patients with dietary management behaviors showed a higher estimated percentage of energy from fat (35.4 vs. 33.8%, p < 0.001), specifically a higher estimated percentage of energy from saturated fatty acids (8.7 vs. 8.3%, p = 0.006), estimated percentage of energy from monounsaturated fatty acids (14.2 vs. 13.5%, p = 0.002), and estimated percentage of energy from polyunsaturated fatty acids (11.2 vs. 10.3%, p = 0.002) compared to NDPDM. Moreover, DPDM had a lower intake of cereals and tubers (330.2 vs. 363.1 g/day, p < 0.001), and a higher intake of vegetables (281.2 vs. 256.4 g/day, p < 0.001) and oil (31.9 vs.31.1 g/day, p = 0.046) than NDPDM.

Table 2.
Mean intake of dietary-related items among Chinese adults with diabetes in the three rounds of China National Nutrition Surveys.
We observed that the majority of patients, both DPDM and NDPDM, did not meet the dietary recommendations (Figure 2). A higher percentage of patients met the dietary recommendations for total carbohydrates (carbohydrates%: 42.6 vs. 41.7%, p = 0.005) and fat (fat%: 24.4 vs. 26.9%, p = 0.004), while the percentage of patients who met the recommendation for the percentage of energy from protein was around 22% for both groups. Only 18.0% and 15.8% of subjects, respectively, fulfilled the recommendation of fiber intake in DPDM and NDPDM. For the intake of specific food groups, the proportion of DPDM meeting the recommended intake ranged from 3.3% to 42.8% and from 3.0% to 39.2% in NDPDM, DPDM showing an improvement in the intake of vegetables (28.0 vs. 24.7%, p = 0.028), cereals and tubers (42.8 vs. 39.2%, p < 0.001), and fruits (5.8 vs. 3.7%, p = 0.050). In addition, the salt consumption for more than 60% of the subjects was higher than the recommended level in both groups.
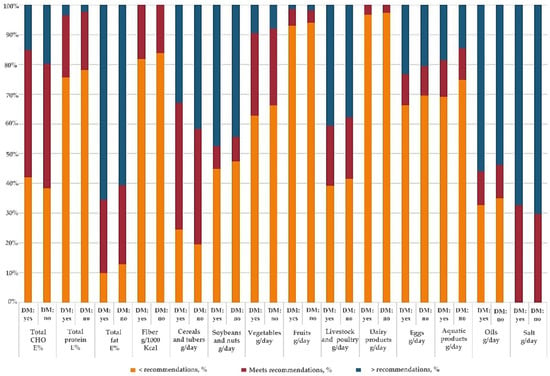
Figure 2.
Percentage of adults with diabetes complying with the dietary recommendations in the three rounds of China National Nutrition Surveys. Dietary recommendations in the Dietary Guidelines for Chinese Residents (2016): 250–400 g/day cereals and tubers; 25–35 g/day soybeans and nuts; 300–500 g/day vegetables; 200–350 g/day fruits; 40–75 g/day livestock and poultry meats; 40–50 g/day eggs; 40–75 g/day aquatic products; 25–30 g/day oil; >300 g/day dairy products; <6 g/day salt. Dietary recommendations in the Guidelines for the Prevention and Treatment of Type 2 Diabetes Milieus in China (2020 Edition): 50–65 E% CHO, 15–20 E% protein, and 20–30 E% fat; >14 g/1000 kcal fiber. Abbreviations: CHO, carbohydrate; E%, percentage of energy; DM: yes, dietary management: yes; DM: no, dietary management: no.
3.3. Diet Quality Score
The comparison of diet quality scores between DPDM and NDPDM is displayed in Table 3. The total score of DPDM was higher than NDPDM (56.3 ± 12.7 vs. 54.1 ± 12.3, p = 0.016). The diabetic patients with dietary management behaviors scored higher than NDPDM on food variety (6.0 ± 2.9 vs. 5.5 ± 3.0, p = 0.002) and specific food groups including total vegetables (3.6 ± 1.4 vs. 3.3 ± 1.4, p < 0.001), dark green and orange vegetables (2.4 ± 1.9 vs. 2.0 ± 1.8 p < 0.001), and meat and egg (3.9 ± 1.6 vs. 3.6 ± 1.8, p < 0.001) but scored lower on refined grains (4.6 ± 0.9 vs. 4.7 ± 0.8, p = 0.047) and calories from SFAs (8.5 ± 2.9 vs. 8.7 ± 2.7, p = 0.022). The difference in total scores between DPDM and NDPDM was observed when stratified by survey year, gender, age, and area of residence, while no differences were observed in the 2015 survey round and the subjects aged below 40 years old subgroups (Table S3). In addition, we noted that subjects who lived in urban areas had higher diet quality scores than those who lived in rural areas, and patients aged ≥65 years had higher scores than patients in other age groups.

Table 3.
CHDI components and criteria for scoring and the score of adults with diabetes in the three rounds of China National Nutrition Surveys.
4. Discussion
The present study provided a sketch of the implementation of dietary management in patients with diabetes using a series of nationally representative data in China. On the one hand, the overall self-reported rate of having dietary management behaviors was 78%, suggesting that most patients were aware of the need to restrict their dietary intake. Moreover, DPDM showed slight improvements in adherence to dietary guidelines and dietary quality scores compared to NDPDM. On the other hand, we observed large room for improvement in the implementation of dietary management in both groups of diabetic patients where less than half of patients meet the recommended intake level of most food groups, and more scientific guidance on dietary management is required for diabetic patients.
In this study, we found that the majority of patients with diabetes reported having anti-diabetic dietary management behaviors. Previous research showed that the self-reported rate of dietary management behaviors varied across different studies [10,11,22]. For instance, a study in Switzerland found that 51% of diabetic patients reported having an anti-diabetic diet [10], and another study in Italy showed that 56% of patients had self-reported adherence to the anti-diabetic dietary plan [22]. Our findings were consistent with most previous studies in China, where more than half of patients with diabetes reported having dietary management behaviors [23,24]. For instance, a multi-center survey in 2013 showed that 83.8% of diabetic patients reported adherence to dietary management plans [23]. The high rate of self-reported dietary management behaviors was consistent with the treatment guidelines for diabetes where all diabetic patients were recommended to actively engage in dietary management [6]. However, consistent with previous studies [25,26], we observed a relatively low prevalence of the adoption of dietary management among rural patients and patients at lower income levels. Additionally, it is important to note that 69.3% of patients who did not take an anti-diabetic diet were overweight or obese in this study, and these patients were at increased risk for diabetes-related complications [27]. It is therefore still necessary to promote the adoption of self-dietary management in patients with diabetes, especially in rural areas, and with low-income or overweight and obese patients. First, education on self-management for diabetic patients should be enhanced. Such self-management education should be customized and meet the needs of patients, and needs to consider their personal characteristics, health literacy, economic status, and literacy level [28,29]. Second, improving the quality of communication between diabetic patients and healthcare providers, increasing patients’ self-efficacy, and promoting family support are also key to promoting the self-management of diabetic patients [30]. Finally, the Expert Consensus on Diabetes Self-Management Education and Support for Adults with Type 2 Diabetes Mellitus in Primary Healthcare Institutions should be implemented [31], in order to further promote and standardize the development of diabetes self-management education and support (DSMES) in primary care, improve the management and education of patients with type 2 diabetes and their health status, and reduce diabetes-related medical costs.
We found that DPDM tended to have better adherence to dietary guidelines than NDPDM, though they still require more scientific guidance on dietary management. On the bright side, DPDM had a slightly lower total energy intake compared to NDPDM. The estimated energy from carbohydrates was decreased and the estimated energy from protein and fat was increased in DPDM compared to NDPDM. More specifically, DPDM showed higher energy intake from high-quality carbohydrates, monounsaturated fatty acids, and polyunsaturated fatty acids, and lower energy intake from low-quality carbohydrates than NDPDM. In addition, DPDM had higher diet quality compared to NDPDM, and they scored higher than NDPDM on food variety and specific food groups including total vegetables, dark green and orange vegetables, and meat and eggs but scored lower on refined grains. These results were consistent with the dietary guidelines for diabetic patients, which recommended reducing overall carbohydrate intake and increasing the proportion of unsaturated fats and high-quality carbohydrate intake, as well as the intake of food high in fiber, such as nonstarchy vegetables and whole grains [5,6]. Similarly, a study conducted in Switzerland found that participants who reported an anti-diabetic diet had a higher consumption of vegetables compared to those not on a diet, while they did not observe significant differences in all other food groups and nutrients [10]. However, it is worth noting that the difference between DPDM and NDPDM in some perspectives did not follow the dietary guidelines. Despite various studies suggesting that a plant protein diet instead of an animal protein diet was beneficial to glycemic control [32], we observed that DPDM showed higher energy intake from animal protein and saturated fatty acids, and lower CHDI scores on calories from SFAs compared to NDPDM, which may be related to the higher intake of livestock and poultry meats in these subjects. These findings were consistent with several previous observational studies, which also reported a higher level of saturated fat intake than the recommendations in patients with diabetes [33,34,35]. In addition, we observed that the proportion of patients with lower than recommended carbohydrate intake was higher in DPDM compared to NDPDM. This finding suggested that some patients were too conscious on the quantity of carbohydrate intake, which may negatively influence dietary management [36]. These mismatches to dietary guidelines observed in this study suggested that more scientific guidance on dietary management was required for patients with diabetes, especially on detailed instructions for achieving a balanced diet.
Despite the general improvement in diet among DPDM, this study showed that the implementation of dietary management against diabetes was far below satisfactory in China. The majority of patients failed to meet the dietary recommendations for the intake of carbohydrates, protein, fat, and fiber, and even in DPDM only 3.3%, 5.8%, 27.9% and 32.4% of patients meet the recommended intake of dairy, fruits, vegetables, and salt, respectively. Low adherence to dietary recommendations has been reported by several studies, despite the variation of dietary guidelines between nations [10,11,37]. A systematic review in 2017 found that the majority of participants consumed less than the recommended servings of fruit, vegetables, grains, and dairy based on 11 cross-sectional studies in eight countries [38]. Moreover, our findings showed a significantly lower dietary quality than the recommended level in both patient groups, which was also true in Mexican adults with diabetes [39]. Moreover, studies in China also reported that the overall dietary quality remained poor in the population, where most people had an inadequate intake of milk and dairy products, nuts, fruits, other cereals and miscellaneous beans, and seafood compared with the recommended intake levels [40,41]. The implementation of dietary management in diabetic patients has long been considered a difficult task [37,42]. Previous studies reported that dietitian involvement or carbohydrate counting was not common in China, and patients usually paid more attention to medical treatments instead of lifestyle interventions [43,44]. The implementation of dietary management in China is challenging considering the large diabetic population, and a great proportion of patients live in rural areas or have low education levels [2]. Over the years, the ministry of health in China has tried to improve education on self-management for patients with chronic diseases through community healthcare centers [45], and we also found that the majority of participants in our study reported having dietary management behaviors. However, our findings also suggested that current education was not enough for patients to change their lifestyles, and many DPDM have an unbalanced intake of nutrients and foods. It is therefore important for the healthcare system to conduct education and management programs for patients with diabetes and truly help patients improve their dietary habits.
In this study, we used three rounds of nationally representative data to assess and compare the dietary intakes and diet quality between DPDM and NDPDM, and evaluated the adherence to dietary guidelines in both groups of patients. To the best of our knowledge, this is the first study in China that compared the composition of diets between DPDM and NDPDM using an unselected, population-based study. In the meantime, we acknowledge that this study had certain limitations. First, dietary intake was collected using a three-day dietary recall, while patients’ dietary habits may change over time along the disease process. Thus, it is necessary to conduct longitudinal studies in the future to capture the difference in dietary intake over time. Second, this was a cross-sectional study; thus, we were not able to make causal inferences regarding dietary behaviors and dietary intake in diabetic patients. Third, we were not able to distinguish between type 1 and type 2 diabetes in this study. However, as type 2 diabetes accounts for more than 90% of all diabetes cases in adults [46], most of the cases in this study were likely type 2 diabetes. Fourth, we cannot rule out some confounding factors that were not included in this analysis, such as antidiabetic medications.
In conclusion, according to our data, 78% of Chinese adults with diabetes adopted dietary management behaviors, but the prevalence was relatively lower in rural, low-income, obese and overweight patients. The diabetic patients with dietary management behaviors showed better adherence to dietary guidelines and higher diet quality scores than NDPDM, while there was large room for improvement in both groups. Our findings suggested that more effective strategies and measures are needed to purposefully promote and refine the implementation of dietary management in patients with diabetes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14235178/s1, Table S1: CHDI components and criteria for scoring; Table S2: Characteristics of adults with diabetes across the three rounds of China National Nutrition Surveys; Table S3: CHDI score of adults with diabetes in the three rounds of China National Nutrition Surveys. Reference [20] is cited in the supplementary materials.
Author Contributions
Conceptualization, M.L., L.Z., J.L. and Y.L.; data collection, D.Y., L.Z. and S.C.; formal analysis, Y.L., P.Y., S.C. and Z.Y.; writing—original draft preparation, Y.L., M.L. and D.Y.; writing—review and editing, Y.L., M.L., D.Y. and L.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Health Commission of the People’s Republic of China Medical Reform Major Program: China National Chronic Diseases and Nutrition Surveillance of Adults (2015–2017); and the Natural Science Foundation of Hunan Province (2022JJ40668).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Chinese Center for Disease Control and Prevention (Approval number: 201519-A and 201614).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are not allowed to be disclosed according to the National Institute for Nutrition and Health and the Chinese Center for Disease Control and Prevention.
Acknowledgments
We thank all the participants who took part in CNNS and the staff who conducted this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ogurtsova, K.; Guariguata, L.; Barengo, N.C.; Ruiz, P.L.; Sacre, J.W.; Karuranga, S.; Sun, H.; Boyko, E.J.; Magliano, D.J. IDF diabetes Atlas: Global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res. Clin. Pract. 2022, 183, 109118. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Teng, D.; Shi, X.; Qin, G.; Qin, Y.; Quan, H.; Shi, B.; Sun, H.; Ba, J.; Chen, B.; et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: National cross sectional study. BMJ 2020, 369, m997. [Google Scholar] [CrossRef] [PubMed]
- Ajala, O.; English, P.; Pinkney, J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am. J. Clin. Nutr. 2013, 97, 505–516. [Google Scholar] [CrossRef] [PubMed]
- Brand-Miller, J.; Hayne, S.; Petocz, P.; Colagiuri, S. Low-glycemic index diets in the management of diabetes: A meta-analysis of randomized controlled trials. Diabetes Care 2003, 26, 2261–2267. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 3. Prevention or Delay of Type 2 Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43, S32–S36. [Google Scholar] [CrossRef]
- Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China(2020 edition) (part 1). Chin. J. Pract. Intern. Med. 2021, 41, 668–695. [Google Scholar] [CrossRef]
- Akbar, H.; Anderson, D.; Gallegos, D. Predicting intentions and behaviours in populations with or at-risk of diabetes: A systematic review. Prev. Med. Rep. 2015, 2, 270–282. [Google Scholar] [CrossRef]
- Hawley, J.A.; Sassone-Corsi, P.; Zierath, J.R. Chrono-nutrition for the prevention and treatment of obesity and type 2 diabetes: From mice to men. Diabetologia 2020, 63, 2253–2259. [Google Scholar] [CrossRef]
- Katsaridis, S.; Grammatikopoulou, M.G.; Gkiouras, K.; Tzimos, C.; Papageorgiou, S.T.; Markaki, A.G.; Exiara, T.; Goulis, D.G.; Papamitsou, T. Low Reported Adherence to the 2019 American Diabetes Association Nutrition Recommendations among Patients with Type 2 Diabetes Mellitus, Indicating the Need for Improved Nutrition Education and Diet Care. Nutrients 2020, 12, 3516. [Google Scholar] [CrossRef]
- Marques-Vidal, P.; Vollenweider, P.; Grange, M.; Guessous, I.; Waeber, G. Dietary intake of subjects with diabetes is inadequate in Switzerland: The CoLaus study. Eur. J. Nutr. 2017, 56, 981–989. [Google Scholar] [CrossRef]
- Saleh, F.; Mumu, S.J.; Ara, F.; Hafez, M.A.; Ali, L. Non-adherence to self-care practices & medication and health related quality of life among patients with type 2 diabetes: A cross-sectional study. BMC Public Health 2014, 14, 431. [Google Scholar] [CrossRef]
- Mai, T.; Mo, C.; Cai, J.; He, H.; Lu, H.; Tang, X.; Chen, Q.; Xu, X.; Nong, C.; Liu, S.; et al. Adherence to dietary guide for elderly adults and health risks of older adults in ethnic minority areas in China: A cross-sectional study. BMC Public Health 2022, 22, 372. [Google Scholar] [CrossRef]
- Ping, Z.; Bao-zhu, Y.; Xin-xin, L. Compliance of diet therapy and its influence factors among patients with diabetes mellitus. Chin. J. Public Health 2010, 26, 1563–1564. [Google Scholar] [CrossRef]
- Bukhsh, A.; Goh, B.H.; Zimbudzi, E.; Lo, C.; Zoungas, S.; Chan, K.G.; Khan, T.M. Type 2 Diabetes Patients’ Perspectives, Experiences, and Barriers Toward Diabetes-Related Self-Care: A Qualitative Study From Pakistan. Front. Endocrinol. 2020, 11, 534873. [Google Scholar] [CrossRef]
- He, Y.; Zhao, W.; Zhang, J.; Zhao, L.; Yang, Z.; Huo, J.; Yang, L.; Wang, J.; He, L.; Sun, J.; et al. Data Resource Profile: China National Nutrition Surveys. Int. J. Epidemiol. 2019, 48, 368–368f. [Google Scholar] [CrossRef]
- Yang, Y. China Food Composition Tables, 2nd ed.; Peking University Medical Press: Beijing, China, 2009. [Google Scholar]
- Yang, Y. China Food Composition Tables, 2002nd ed.; Peking University Medical Press: Beijing, China, 2002. [Google Scholar]
- Shan, Z.; Rehm, C.D.; Rogers, G.; Ruan, M.; Wang, D.D.; Hu, F.B.; Mozaffarian, D.; Zhang, F.F.; Bhupathiraju, S.N. Trends in Dietary Carbohydrate, Protein, and Fat Intake and Diet Quality Among US Adults, 1999–2016. JAMA 2019, 322, 1178–1187. [Google Scholar] [CrossRef]
- Wang, S.-s.; Lay, S.; Yu, H.-n.; Shen, S.-r. Dietary guidelines for Chinese residents (2016): Comments and comparisons. J. Zhejiang Univ. Sci. B 2016, 17, 649–656. [Google Scholar] [CrossRef]
- He, Y.; Fang, Y.; Yang, X. Establishment and application of China healthy diet index. Acta Nutr. Sin. 2017, 39, 436–441. [Google Scholar] [CrossRef]
- Zhu, Z.; Yang, X.; Fang, Y.; Zhang, J.; Yang, Z.; Wang, Z.; Liu, A.; He, L.; Sun, J.; Lian, Y.; et al. Trends and Disparities of Energy Intake and Macronutrient Composition in China: A Series of National Surveys, 1982–2012. Nutrients 2020, 12, 2168. [Google Scholar] [CrossRef]
- Ponzo, V.; Rosato, R.; Tarsia, E.; Goitre, I.; De Michieli, F.; Fadda, M.; Monge, T.; Pezzana, A.; Broglio, F.; Bo, S. Self-reported adherence to diet and preferences towards type of meal plan in patient with type 2 diabetes mellitus. A cross-sectional study. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 642–650. [Google Scholar] [CrossRef]
- Yang, X.; Yuan, L.; Guo, X. Current situation of diet self-management in patients with type 2 diabetes: A multi-centre survey in China. Chin. J. Diabetes Mellit. 2013, 5, 666–669. [Google Scholar] [CrossRef]
- Liu, K.; Zhao, X.; Chen, J. Study on the control rates of type 2 diabetes and its influencing factors in Chuansha community of Shanghai. Chin. J. Health Educ. 2016, 32, 544–546+550. [Google Scholar] [CrossRef]
- Wang, X.; Li, M.A.; Lili, L.I.; School, N. The Current Status and Influencing Factors of Self-management Level in Patients with Type 2 Diabetic in Community. J. Ningxia Med. Univ. 2017, 39, 436–442. [Google Scholar] [CrossRef]
- Alexandre, K.; Campbell, J.; Bugnon, M.; Henry, C.; Schaub, C.; Serex, M.; Elmers, J.; Desrichard, O.; Peytremann-Bridevaux, I. Factors influencing diabetes self-management in adults: An umbrella review of systematic reviews. JBI Evid. Synth. 2021, 19, 1003–1118. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.; Ramachandran, A.; Yancy, W.S., Jr.; Forouhi, N.G. Nutritional basis of type 2 diabetes remission. BMJ 2021, 374, n1449. [Google Scholar] [CrossRef] [PubMed]
- Bagnasco, A.; Di Giacomo, P.; Da Rin Della Mora, R.; Catania, G.; Turci, C.; Rocco, G.; Sasso, L. Factors influencing self-management in patients with type 2 diabetes: A quantitative systematic review protocol. J. Adv. Nurs. 2014, 70, 187–200. [Google Scholar] [CrossRef]
- Gopalan, A.; Kellom, K.; McDonough, K.; Schapira, M.M. Exploring how patients understand and assess their diabetes control. BMC Endocr. Disord. 2018, 18, 79. [Google Scholar] [CrossRef]
- Lambrinou, E.; Hansen, T.B.; Beulens, J.W. Lifestyle factors, self-management and patient empowerment in diabetes care. Eur. J. Prev. Cardiol. 2019, 26, 55–63. [Google Scholar] [CrossRef]
- Diabetes Professional Committee of Chinese Research Hospital Association, S.D.C. Expert Consensus on Diabetes Self-Management Education and Support for Adults with Type 2 Diabetes Mellitus in Primary Healthcare Institutions. Chin. J. Diabetes Mellit. 2022, 14, 307–315. [Google Scholar] [CrossRef]
- Viguiliouk, E.; Stewart, S.E.; Jayalath, V.H.; Ng, A.P.; Mirrahimi, A.; de Souza, R.J.; Hanley, A.J.; Bazinet, R.P.; Blanco Mejia, S.; Leiter, L.A.; et al. Effect of Replacing Animal Protein with Plant Protein on Glycemic Control in Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2015, 7, 9804–9824. [Google Scholar] [CrossRef]
- Breen, C.; Ryan, M.; McNulty, B.; Gibney, M.J.; Canavan, R.; O’Shea, D. High saturated-fat and low-fibre intake: A comparative analysis of nutrient intake in individuals with and without type 2 diabetes. Nutr. Diabetes 2014, 4, e104. [Google Scholar] [CrossRef]
- Vitale, M.; Masulli, M.; Cocozza, S.; Anichini, R.; Babini, A.C.; Boemi, M.; Bonora, E.; Buzzetti, R.; Carpinteri, R.; Caselli, C.; et al. Sex differences in food choices, adherence to dietary recommendations and plasma lipid profile in type 2 diabetes—The TOSCA.IT study. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 879–885. [Google Scholar] [CrossRef]
- Ewers, B.; Trolle, E.; Jacobsen, S.S.; Vististen, D.; Almdal, T.P.; Vilsboll, T.; Bruun, J.M. Dietary habits and adherence to dietary recommendations in patients with type 1 and type 2 diabetes compared with the general population in Denmark. Nutrition 2019, 61, 49–55. [Google Scholar] [CrossRef]
- Mehta, S.N.; Haynie, D.L.; Higgins, L.A.; Bucey, N.N.; Rovner, A.J.; Volkening, L.K.; Nansel, T.R.; Laffel, L.M. Emphasis on carbohydrates may negatively influence dietary patterns in youth with type 1 diabetes. Diabetes Care 2009, 32, 2174–2176. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Hattori, M.; Wada, S.; Iwase, H.; Kadono, M.; Tatsumi, H.; Kuwahata, M.; Fukui, M.; Hasegawa, G.; Nakamura, N.; et al. Assessment of daily food and nutrient intake in Japanese type 2 diabetes mellitus patients using dietary reference intakes. Nutrients 2013, 5, 2276–2288. [Google Scholar] [CrossRef]
- Burch, E.; Ball, L.; Somerville, M.; Williams, L.T. Dietary intake by food group of individuals with type 2 diabetes mellitus: A systematic review. Diabetes Res. Clin. Pract. 2018, 137, 160–172. [Google Scholar] [CrossRef]
- Lopez-Olmedo, N.; Jonnalagadda, S.; Basto-Abreu, A.; Reyes-Garcia, A.; Alish, C.J.; Shamah-Levy, T.; Barrientos-Gutierrez, T. Adherence to Dietary Guidelines in Adults by Diabetes Status: Results From the 2012 Mexican National Health and Nutrition Survey. Nutrients 2020, 12, 3464. [Google Scholar] [CrossRef]
- Huang, F.; Wang, Z.; Wang, L.; Wang, H.; Zhang, J.; Du, W.; Su, C.; Jia, X.; Ouyang, Y.; Wang, Y.; et al. Evaluating adherence to recommended diets in adults 1991-2015: Revised China dietary guidelines index. Nutr. J. 2019, 18, 70. [Google Scholar] [CrossRef]
- He, Y.; Li, Y.; Yang, X.; Hemler, E.C.; Fang, Y.; Zhao, L.; Zhang, J.; Yang, Z.; Wang, Z.; He, L.; et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: A cross-sectional population-based study. Lancet Diabetes Endocrinol. 2019, 7, 540–548. [Google Scholar] [CrossRef]
- Thanopoulou, A.; Karamanos, B.; Angelico, F.; Assaad-Khalil, S.; Barbato, A.; Del Ben, M.; Djordjevic, P.; Dimitrijevic-Sreckovic, V.; Gallotti, C.; Katsilambros, N.; et al. Nutritional habits of subjects with Type 2 diabetes mellitus in the Mediterranean Basin: Comparison with the non-diabetic population and the dietary recommendations. Multi-Centre Study of the Mediterranean Group for the Study of Diabetes (MGSD). Diabetologia 2004, 47, 367–376. [Google Scholar] [CrossRef]
- Jaacks, L.M.; Liu, W.; Ji, L.; Mendez, M.A.; Du, S.; Crandell, J.; Rosamond, W.; Mayer-Davis, E.J. Diabetes nutrition therapy and dietary intake among individuals with Type 1 diabetes in China. Diabet. Med. 2015, 32, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Vijan, S.; Stuart, N.S.; Fitzgerald, J.T.; Ronis, D.L.; Hayward, R.A.; Slater, S.; Hofer, T.P. Barriers to following dietary recommendations in Type 2 diabetes. Diabet. Med. 2005, 22, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liu, Y.; Li, L. Diabetes Management in China: Types and Reflections. Chin. Gen. Pract. 2021, 24, 3019–3025. [Google Scholar] [CrossRef]
- Kaur, R.; Kaur, M.; Singh, J. Endothelial dysfunction and platelet hyperactivity in type 2 diabetes mellitus: Molecular insights and therapeutic strategies. Cardiovasc. Diabetol. 2018, 17, 121. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).