ACE-Vitamin Index and Risk of Glaucoma: The SUN Project
Abstract
1. Introduction
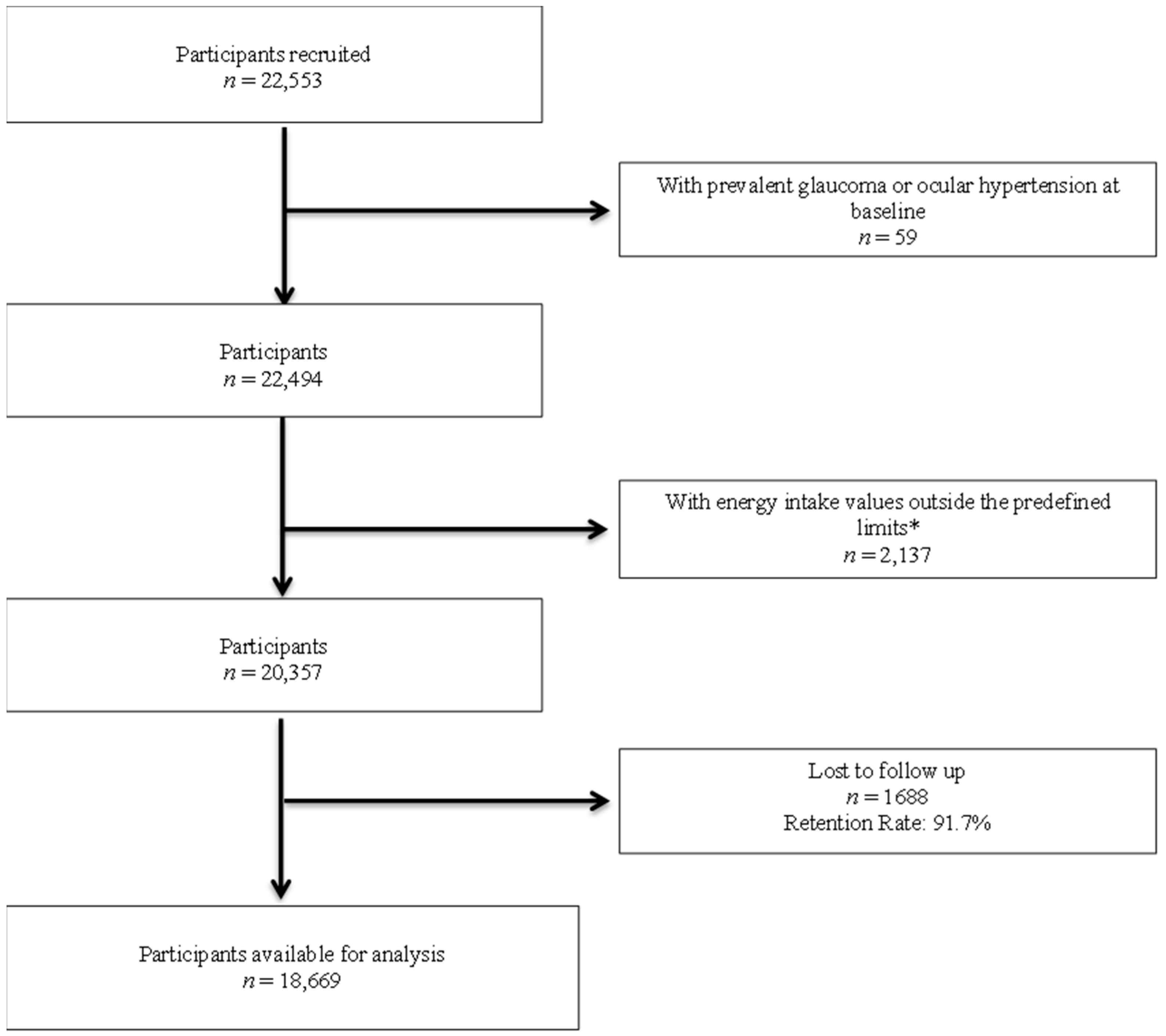
2. Materials and Methods
2.1. Study Population
2.2. Assessment of ACE-Vitamin Index
2.3. Outcome Assessment: Glaucoma Incidence
2.4. Assessment of Other Covariates
2.5. Statistical Analysis
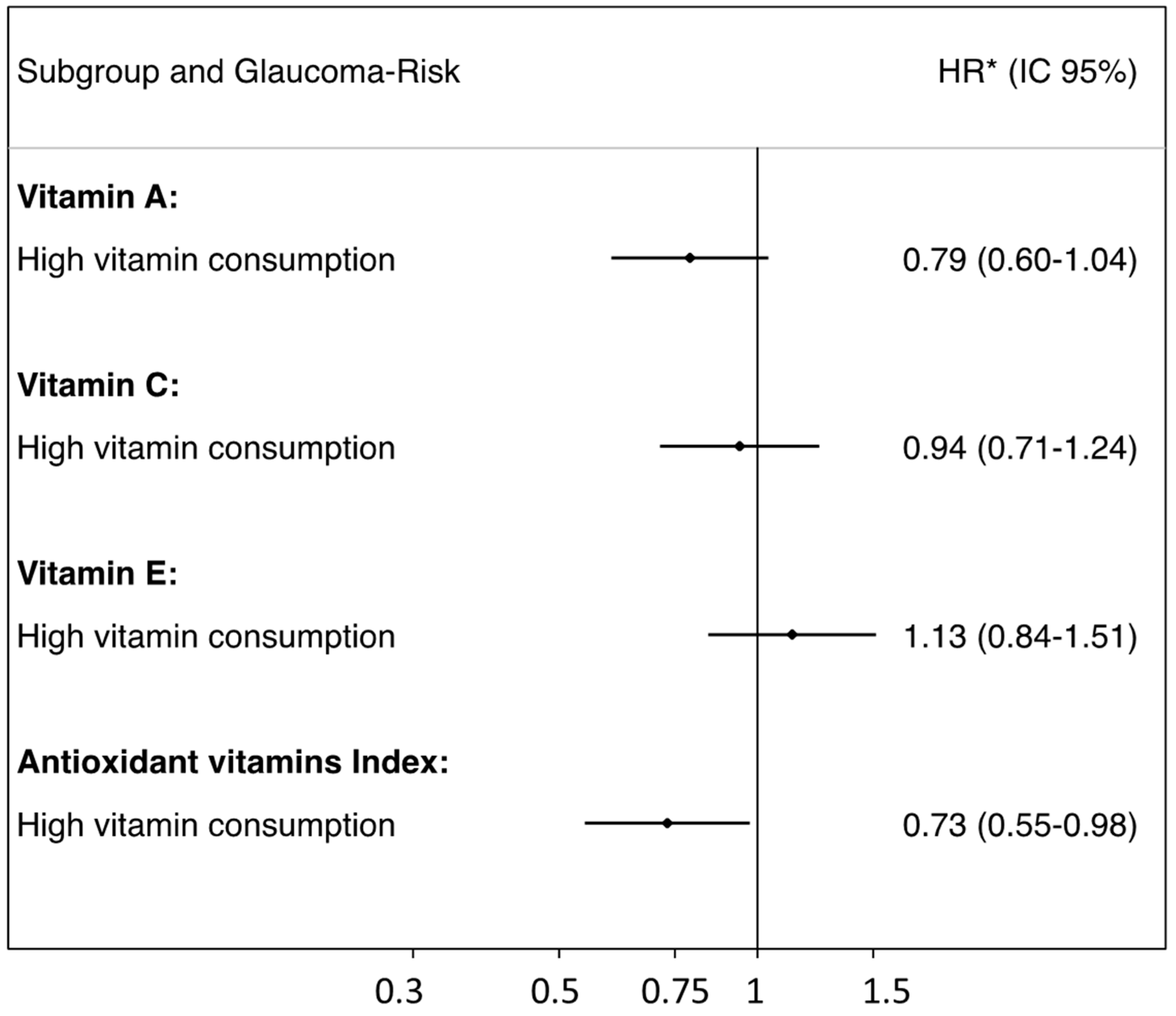
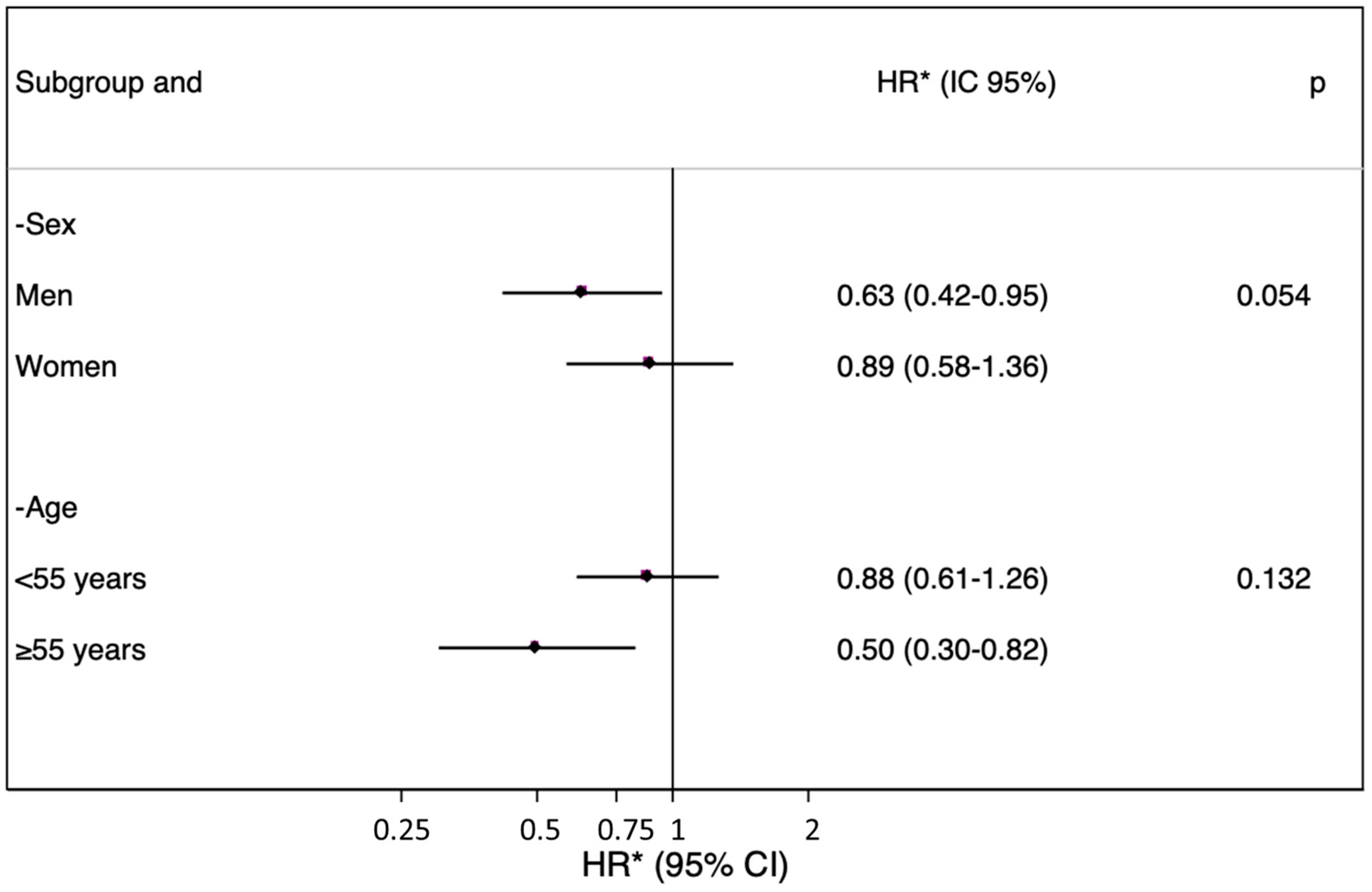
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McMonnies, C.W. Glaucoma history and risk factors. J. Optom. 2017, 10, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Tham, Y.-C.; Li, X.; Wong, T.Y.; Quigley, H.A.; Aung, T.; Cheng, C.-Y. Global Prevalence of Glaucoma and Projections of Glaucoma Burden through 2040 A Systematic Review and Meta-Analysis. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef] [PubMed]
- Allison, K.; Patel, D.; Alabi, O. Epidemiology of Glaucoma: The Past, Present, and Predictions for the Future. Cureus 2020, 12, e11686. [Google Scholar] [CrossRef] [PubMed]
- Izzotti, A.; Saccà, S.C.; Cartiglia, C.; De Flora, S. Oxidative deoxyribonucleic acid damage in the eyes of glaucoma patients. Am. J. Med. 2003, 114, 638–646. [Google Scholar] [CrossRef]
- Saccà, S.C.; Pascotto, A.; Camicione, P.; Capris, P.; Izzotti, A. Oxidative DNA damage in the human trabecular meshwork: Clinical correlation in patients with primary open-angle glaucoma. Arch. Ophthalmol. 2005, 123, 458–463. [Google Scholar] [CrossRef]
- Nucci, C.; Russo, R.; Martucci, A.; Giannini, C.; Garaci, F.; Floris, R.; Bagetta, G.; Morrone, L.A. New strategies for neuroprotection in glaucoma, a disease that affects the central nervous system. Eur. J. Pharmacol. 2016, 787, 119–126. [Google Scholar] [CrossRef]
- Tanito, M.; Kaidzu, S.; Takai, Y.; Ohira, A. Association between systemic oxidative stress and visual field damage in open-angle glaucoma. Sci. Rep. 2016, 6, 25792. [Google Scholar] [CrossRef]
- Maneesh Kumar, D.; Agarwal, N. Oxidative stress in glaucoma: A burden of evidence. J. Glaucoma 2007, 16, 334–343. [Google Scholar] [CrossRef]
- Blaner, W.S.; Shmarakov, I.O.; Traber, M.G. Vitamin A and Vitamin E: Will the Real Antioxidant Please Stand Up? Annu. Rev. Nutr. 2021, 41, 105–131. [Google Scholar] [CrossRef]
- Ramdas, W.D.; Schouten, J.S.A.G.; Webers, C.A.B. The effect of vitamins on glaucoma: A systematic review and meta-analysis. Nutrients 2018, 10, 359. [Google Scholar] [CrossRef]
- Moreno-Montañés, J.; Gándara, E.; Gutierrez-Ruiz, I.; Moreno-Galarraga, L.; Ruiz-Canela, M.; Bes-Rastrollo, M.; Martínez-González, M.Á.; Fernandez-Montero, A. Healthy Lifestyle Score and Incidence of Glaucoma: The Sun Project. Nutrients 2022, 14, 779. [Google Scholar] [CrossRef] [PubMed]
- Carlos, S.; De La Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Razquin, C.; Rico-Campà, A.; Martínez-González, M.; Ruiz-Canela, M. Mediterranean Diet and Health Outcomes in the SUN Cohort. Nutrients 2018, 10, 439. [Google Scholar] [CrossRef] [PubMed]
- Willet, W. Nutritional Epidemiology. In Nutritional Epidemiology; Willett, W., Ed.; Oxford University Press: London, UK, 2012; pp. 74–100. ISBN 978-0-19-975403-8. [Google Scholar]
- Moreiras, O.; Carbajal, A.; Cabrera, L.; Cuadrado, C. Food Composition Tables; Ediciones Pirámides: Madrid, Spain, 2008; ISBN 978-84-368-2182-6. [Google Scholar]
- De La Fuente-Arrillaga, C.; Vázquez Ruiz, Z.; Bes-Rastrollo, M.; Sampson, L.; Martinez-González, M.A. Reproducibility of an FFQ validated in Spain. Public Health Nutr. 2010, 13, 1364–1372. [Google Scholar] [CrossRef]
- Moreno-Montañés, J.; Gutierrez-Ruiz, I.; Gándara, E.; Moreno-Galarraga, L.; Santiago, S.; Ruiz-Canela, M.; Martínez-González, J.; Martínez-González, M.Á.; Fernandez-Montero, A. Carbohydrate intake and risk of glaucoma in the sun cohort. Eur. J. Ophthalmol. 2022, 32, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Pérez de Arcelus, M.; Toledo, E.; Martínez-González, M.A.; Sayón-Orea, C.; Gea, A.; Moreno-Montañés, J. Omega 3:6 ratio intake and incidence of glaucoma: The SUN cohort. Clin. Nutr. 2014, 33, 1041–1045. [Google Scholar]
- Sajovic, J.; Meglič, A.; Glavač, D.; Markelj, Š.; Hawlina, M.; Fakin, A. The Role of Vitamin A in Retinal Diseases. Int. J. Mol. Sci. 2022, 23, 1014. [Google Scholar] [CrossRef]
- National Institutes of Health. Nutrient Recommendations: Dietary Reference Intakes. Available online: https://ods.od.nih.gov/HealthInformation/nutrientrecommendations.aspx#dri (accessed on 30 November 2022).
- Taheri, S.; Asadi, S.; Nilashi, M.; Ali Abumalloh, R.; Ghabban, N.M.A.; Mohd Yusuf, S.Y.; Supriyanto, E.; Samad, S. A literature review on beneficial role of vitamins and trace elements: Evidence from published clinical studies. J. Trace Elem. Med. Biol. 2021, 67, 126789. [Google Scholar] [CrossRef]
- Sinopoli, A.; Caminada, S.; Isonne, C.; Santoro, M.M.; Baccolini, V. What Are the Effects of Vitamin A Oral Supplementation in the Prevention and Management of Viral Infections? A Systematic Review of Randomized Clinical Trials. Nutrients 2022, 14, 4081. [Google Scholar] [CrossRef]
- Wang, S.Y.; Singh, K.; Lin, S.C. Glaucoma and vitamins A, C, and e supplement intake and serum levels in a population-based sample of the United States. Eye 2013, 27, 487–494. [Google Scholar] [CrossRef]
- Giaconi, J.A.; Yu, F.; Stone, K.L.; Pedula, K.L.; Ensrud, K.E.; Cauley, J.A.; Hochberg, M.C.; Coleman, A.L. The association of consumption of fruits/vegetables with decreased risk of glaucoma among older African-American women in the study of osteoporotic fractures. Am. J. Ophthalmol. 2012, 154, 635–644. [Google Scholar] [CrossRef] [PubMed]
- Ramdas, W.D.; Wolfs, R.C.W.; Kiefte-De Jong, J.C.; Hofman, A.; De Jong, P.T.V.M.; Vingerling, J.R.; Jansonius, N.M. Nutrient intake and risk of open-Angle glaucoma: The Rotterdam Study. Eur. J. Epidemiol. 2012, 27, 385–393. [Google Scholar] [CrossRef]
- Kang, J.H.; Pasquale, L.R.; Willett, W.; Rosner, B.; Egan, K.M.; Faberowski, N.; Hankinson, S.E. Antioxidant intake and primary open-angle glaucoma: A prospective study. Am. J. Epidemiol. 2003, 158, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Juneja, D.; Gupta, A.; Kataria, S.; Singh, O. Role of high dose vitamin C in management of hospitalised COVID-19 patients: A minireview. World J. Virol. 2022, 11, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Granger, M.; Eck, P. Dietary Vitamin C in Human Health. Adv. Food Nutr Res. 2018, 83, 281–310. [Google Scholar] [PubMed]
- Iqbal, Z.; Midgley, J.M.; Watson, D.G.; Karditsas, S.D.; Dutton, G.N.; Wilson, W.S. Effect of oral administration of vitamin C on human aqueous humor ascorbate concentration. Acta Pharmacol. Sin. 1999, 20, 879–883. [Google Scholar]
- Yuki, K.; Murat, D.; Kimura, I.; Ohtake, Y.; Tsubota, K. Reduced-serum vitamin C and increased uric acid levels in normal-tension glaucoma. Graefe’s Arch. Clin. Exp. Ophthalmol. 2010, 248, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Willett, W.C.; Rosner, B.A.; Buys, E.; Wiggs, J.L.; Pasquale, L.R. Association of dietary nitrate intake with primary open-angle glaucoma: A prospective analysis from the nurses’ health study and health professionals follow-up study. JAMA Ophthalmol. 2016, 134, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Moïse, M.M.; Benjamin, L.M.; Doris, T.M.; Dalida, K.N.; Augustin, N.O. Role of Mediterranean diet, tropical vegetables rich in antioxidants, and sunlight exposure in blindness, cataract and glaucoma among African type 2 diabetics. Int. J. Ophthalmol. 2012, 5, 231–237. [Google Scholar] [CrossRef]
- Liao, S.; Omage, S.O.; Börmel, L.; Kluge, S.; Schubert, M.; Wallert, M.; Lorkowski, S. Vitamin E and Metabolic Health: Relevance of Interactions with Other Micronutrients. Antioxidants 2022, 11, 1785. [Google Scholar] [CrossRef]
- Tanito, M. Reported evidence of vitamin E protection against cataract and glaucoma. Free Radic. Biol. Med. 2021, 177, 100–119. [Google Scholar] [CrossRef]
- Dehbalaei, M.G.; Ashtary-Larky, D.; Amarpoor Mesrkanlou, H.; Talebi, S.; Asbaghi, O. The effects of magnesium and vitamin E co-supplementation on some cardiovascular risk factors: A meta-analysis. Clin. Nutr. ESPEN 2021, 41, 110–117. [Google Scholar] [CrossRef]
- Goyal, A.; Srivastava, A.; Sihota, R.; Kaur, J. Evaluation of oxidative stress markers in aqueous humor of primary open angle glaucoma and primary angle closure glaucoma patients. Curr. Eye Res. 2014, 39, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Izzotti, A.; Bagnis, A.; Saccà, S.C. The role of oxidative stress in glaucoma. Mutat. Res.-Rev. Mutat. Res. 2006, 612, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Zanon-Moreno, V.; Marco-Ventura, P.; Lleo-Perez, A.; Pons-Vazquez, S.; Garcia-Medina, J.J.; Vinuesa-Silva, I.; Moreno-Nadal, M.A.; Pinazo-Duran, M. Oxidative stress in primary open-angle glaucoma. J Glaucoma. 2008, 17, 263–268. [Google Scholar] [CrossRef]
- Cheung, W.; Cordeiro, F. Neuroprotection in Glaucoma: Drug-bases approaches. Optom. Vis. Sci. 2008, 85, 406–416. [Google Scholar] [CrossRef] [PubMed]
- Age-Related Eye Disease Study Research Group. A Randomized, Placebo-Controlled, Clinical Trial of High-Dose Supplementation With Vitamins C and E, Beta Carotene, and Zinc for Age-Related Macular Degeneration and Vision Loss. AREDS Report No. 8. Arch. Ophthalmol. 2001, 119, 1417–1436. [Google Scholar] [CrossRef]
- Chew, E.Y.; Clemons, T.E.; SanGiovanni, J.P.; Danis, R.; Ferris, F.L.; Elman, M.; Antoszyk, A.; Ruby, A.; Orth, D.; Bressler, S.; et al. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: The Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA 2013, 309, 2005–2015. [Google Scholar] [CrossRef]
- Gartner, C.; Stahl, W.; Sies, H. Lycopene is more bioavailable from tomato paste than fresh tomatoes. Am. J. Clin. Nutr. 1997, 66, 116–122. [Google Scholar] [CrossRef]
- Van Hof, K.H.; West, C.E.; Weststrate, J.A.; Hautvast, J.G.A.J. Recent Advances in Nutritional Sciences Dietary Factors That Affect the Bioavailability of Carotenoids. Recent Adv. Nutr. Sci. 2000, 130, 503–506. [Google Scholar]
| Vitamins | Included Foods |
|---|---|
| Vitamin A | Whole milk, condensed milk, cream, milkshakes, yogurt, petit suisse, curds, portioned or cream cheese, cured or semi-cured cheese, fresh cheese, custard, eggs, liver, pate, white fish, blue fish, cod, salted and/or smoked fish, mussels, oysters, prawns, shrimps, squids, octopus, chard, cabbage, lettuce, tomato, carrot, beans, eggplant, orange, banana, apple, strawberries, peach, cherries, figs, watermelon, melon, fruits in syrup, dried fruits, dried fruits, olives, avocado, kiwi, lentils, chickpeas, peas, pizza, butter, margarine, donuts, industrial pastries, homemade pastries, cakes, pastries, natural juices, bottled juices, croquettes, mayonnaise, tomato sauce and jam. |
| Vitamin C | Whole milk, semi-skimmed or skimmed milk, custard, milkshakes, yogurt, chicken with skin or without skin, liver, viscera, chard, cabbage, lettuce, tomato, carrot, beans, eggplant, peppers, asparagus, green vegetables, French fries, baked potatoes, orange, banana, apple, strawberries, peaches, cherries, figs, watermelon, melon, grapes, fruits in syrup, fruits in juice, avocado, mango, kiwi, lentils, chickpeas, peas, cereals, pizza, donuts, natural orange juice, other natural juices, croquettes, tomato sauce and jam. |
| Vitamin E | Whole milk, semi-skimmed milk, condensed milk, whipped custard, yogurt, curd, cheese in portions or cream cheese, cured or semi-cured cheese, fresh cheese, eggs, chicken with or without skin, veal, pork, lamb, rabbit, liver, other offal, cured ham, sausages, sausages, blood sausage, hamburger, bacon, blue fish, cod, salted or smoked fish, mussels, oysters, prawns, shrimps, squids, chard, beans, eggplants, peppers, French fries, baked potatoes, bananas, nuts, dried fruits, avocado, lentils, chickpeas, beans, peas, black bread, rice, pizza, butter, margarine, olive oil, sunflower oil, corn oil, cookies, muffins, donuts, churros, chocolate, chocolates, chocolates, nougat, marzipan, crop nuts, soups and creams, tomato sauce and mayonnaise. |
| Participants’ Baseline Characteristics | Low Vitamin Consumption | High Vitamin Consumption |
|---|---|---|
| ACE-Vitamin Index | 0–1 point | 2–3 points |
| n | 9343 | 9326 |
| Age, years | 38.1 (12.2) | 38.6 (12.4) |
| Sex. men, % | 46.79 | 33.14 |
| Educational level, % | ||
| College | 21.73 | 25.86 |
| Postgraduate | 50.30 | 46.96 |
| Master | 8.20 | 7.91 |
| Doctorate | 10.53 | 9.76 |
| Missing or no college | 9.24 | 9.51 |
| Body mass index, kg/m2 | 23.8 (3.6) | 23.3 (3.5) |
| Physical activity, METS-h/week | 19.4 (20.3) | 24.1 (25.0) |
| Total energy intake, Kcal/day | 2119.5 (582.5) | 2568.1 (568.4) |
| Omega 3:6 ratio | 0.2 (0.1) | 0.2 (0.1) |
| Hypertension, % | 11.07 | 10.46 |
| Cancer, % | 2.30 | 2.81 |
| Type 2 diabetes, % | 1.56 | 2.34 |
| Smoking, packages/year | 6.01(10.9) | 4.8 (9.1) |
| Alcohol intake, mg/day | 7.1 (11.2) | 6.2 (9.1) |
| Caffeine intake, mg/day | 42.5 (40.4) | 42.3 (39.0) |
| Special diet, % | 6.75 | 10.07 |
| Low Vitamin Consumption | High Vitamin Consumption | |
|---|---|---|
| ACE-Vitamin Index | 0–1 point | 2–3 points |
| Persons/year | 97,252 | 95,148 |
| New glaucoma cases, n | 120 | 146 |
| Crude hazard ratio HR (95% CI) | 1 (ref.) | 0.91 (0.71–1.18) |
| Sex- and age-adjusted HR (95% CI) | 1 (ref.) | 0.87 (0.67–0.76) |
| Multivariable-adjusted HR (95% CI) * | 1 (ref.) | 0.73 (0.55–0.98) |
| Multivariable-adjusted HR (95% CI) ** | 1 (ref.) | 0.72 (0.52–0.99) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Montañés, J.; Gándara, E.; Moreno-Galarraga, L.; Hershey, M.S.; López-Gil, J.F.; Kales, S.; Bes-Rastrollo, M.; Martínez-González, M.Á.; Fernandez-Montero, A. ACE-Vitamin Index and Risk of Glaucoma: The SUN Project. Nutrients 2022, 14, 5129. https://doi.org/10.3390/nu14235129
Moreno-Montañés J, Gándara E, Moreno-Galarraga L, Hershey MS, López-Gil JF, Kales S, Bes-Rastrollo M, Martínez-González MÁ, Fernandez-Montero A. ACE-Vitamin Index and Risk of Glaucoma: The SUN Project. Nutrients. 2022; 14(23):5129. https://doi.org/10.3390/nu14235129
Chicago/Turabian StyleMoreno-Montañés, Javier, Elsa Gándara, Laura Moreno-Galarraga, Maria S. Hershey, José Francisco López-Gil, Stefanos Kales, Maira Bes-Rastrollo, Miguel Ángel Martínez-González, and Alejandro Fernandez-Montero. 2022. "ACE-Vitamin Index and Risk of Glaucoma: The SUN Project" Nutrients 14, no. 23: 5129. https://doi.org/10.3390/nu14235129
APA StyleMoreno-Montañés, J., Gándara, E., Moreno-Galarraga, L., Hershey, M. S., López-Gil, J. F., Kales, S., Bes-Rastrollo, M., Martínez-González, M. Á., & Fernandez-Montero, A. (2022). ACE-Vitamin Index and Risk of Glaucoma: The SUN Project. Nutrients, 14(23), 5129. https://doi.org/10.3390/nu14235129








