Quality Specific Associations of Carbohydrate Consumption and Frailty Index
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Dietary Assessment and Carbohydrate Quality Indicators
2.3. Construction of Frailty Index (FI)
2.4. Assessment of Covariates
2.5. Statistical Analysis
3. Results
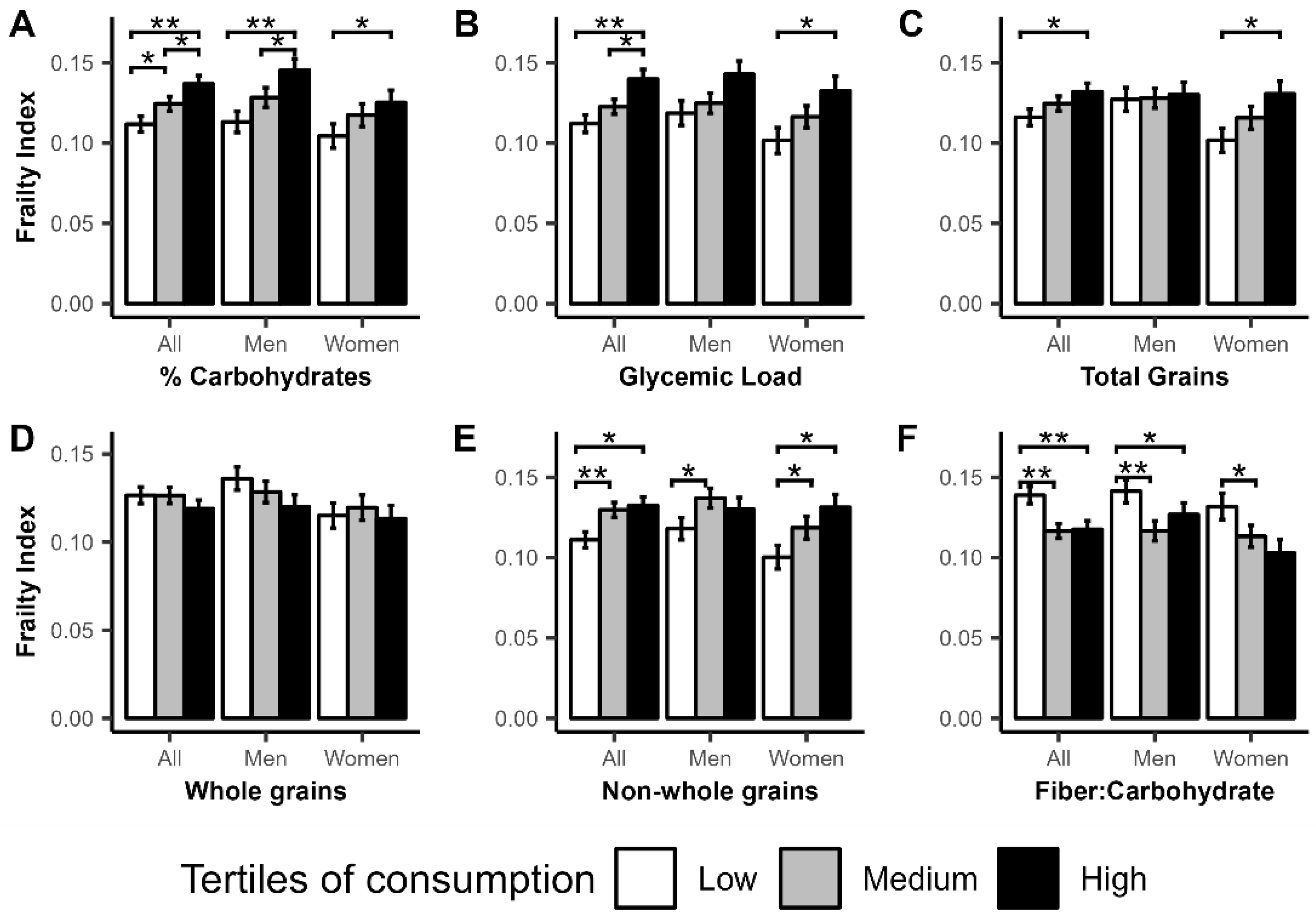
3.1. Cross-Sectional Associations of Carbohydrate Intake with Frailty Index
3.2. Longitudinal Association of Carbohydrate Intake with Frailty Index
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fedarko, N.S. The Biology of Aging and Frailty. Clin. Geriatr. Med. 2011, 27, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Thillainadesan, J.; A Scott, I.; Le Couteur, D.G. Frailty, a multisystem ageing syndrome. Age Ageing 2020, 49, 758–763. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Searle, S.D.; Mitnitski, A.; Gahbauer, E.A.; Gill, T.M.; Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr. 2008, 8, 24. [Google Scholar] [CrossRef]
- Yannakoulia, M.; Ntanasi, E.; Anastasiou, C.A.; Scarmeas, N. Frailty and nutrition: From epidemiological and clinical evidence to potential mechanisms. Metabolism 2017, 68, 64–76. [Google Scholar] [CrossRef] [PubMed]
- Coelho-Junior, H.J.; Marzetti, E.; Picca, A.; Cesari, M.; Uchida, M.C.; Calvani, R. Protein Intake and Frailty: A Matter of Quantity, Quality, and Timing. Nutrients 2020, 12, 2915. [Google Scholar] [CrossRef] [PubMed]
- Hu, N.; Yu, J.T.; Tan, L.; Wang, Y.L.; Sun, L.; Tan, L. Nutrition and the risk of Alzheimer’s disease. Biomed Res Int. 2013, 2013, 524820. [Google Scholar] [CrossRef]
- Laclaustra, M.; Rodríguez-Artalejo, F.; Guallar-Castillón, P.; Banegas, J.R.; Graciani, A.; García-Esquinas, E.; Ordovás, J.; López-García, E. Prospective association between added sugars and frailty in older adults. Am. J. Clin. Nutr. 2018, 107, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Struijk, E.A.; Rodríguez-Artalejo, F.; Fung, T.T.; Willett, W.C.; Hu, F.B.; Lopez-Garcia, E. Sweetened beverages and risk of frailty among older women in the Nurses’ Health Study: A cohort study. PLOS Med. 2020, 17, e1003453. [Google Scholar] [CrossRef]
- Long, T.; Zhang, K.; Chen, Y.; Wu, C. Trends in Diet Quality Among Older US Adults From 2001 to 2018. JAMA Netw. Open 2022, 5, e221880. [Google Scholar] [CrossRef] [PubMed]
- Chuy, V.; Gentreau, M.; Artero, S.; Berticat, C.; Rigalleau, V.; Pérès, K.; Helmer, C.; Samieri, C.; Féart, C. Simple Carbohydrate Intake and Higher Risk for Physical Frailty Over 15 Years in Community-Dwelling Older Adults. Journals Gerontol. Ser. A 2022, 77, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Cesari, M.; Gambassi, G.; van Kan, G.A.; Vellas, B. The frailty phenotype and the frailty index: Different instruments for different purposes. Age Ageing 2014, 43, 10–12. [Google Scholar] [CrossRef]
- Kuo, P.; Schrack, J.A.; Shardell, M.D.; Levine, M.; Moore, A.Z.; An, Y.; Elango, P.; Karikkineth, A.; Tanaka, T.; de Cabo, R.; et al. A roadmap to build a phenotypic metric of ageing: Insights from the Baltimore Longitudinal Study of Aging. J. Intern. Med. 2020, 287, 373–394. [Google Scholar] [CrossRef] [PubMed]
- Shock, N.W.; Greulick, R.C.; Andres, R.; Arenberg, D.; Costa, P.; Lakatta., E.; Tobin, J.D. Normal Human Aging: The Baltimore Study of Aging; NIH publication no.84-2450; U.S. Government Printing Office: Washington, DC, USA, 1984.
- Picó, C.; Serra, F.; Rodríguez, A.M.; Keijer, J.; Palou, A. Biomarkers of Nutrition and Health: New Tools for New Approaches. Nutrients 2019, 11, 1092. [Google Scholar] [CrossRef]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Irwin, M.; Artin, K.H.; Oxman, M.N. Screening for Depression in the Older Adult: Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch. Intern. Med. 1999, 159, 1701–1704. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State”. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Kim, S.; Haines, P.S.; Siega-Riz, A.M.; Popkin, B.M. The Diet Quality Index-International (DQI-I) Provides an Effective Tool for Cross-National Comparison of Diet Quality as Illustrated by China and the United States. J. Nutr. 2003, 133, 3476–3484. [Google Scholar] [CrossRef]
- Wang, Y.; Hao, Q.; Su, L.; Liu, Y.; Liu, S.; Dong, B. Adherence to the Mediterranean Diet and the Risk of Frailty in Old People: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2018, 22, 613–618. [Google Scholar] [CrossRef]
- Rashidi Pour Fard, N.; Amirabdollahian, F.; Haghighatdoost, F. Dietary patterns and frailty: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 498–513. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.H.; Martins, B.A.; Okada, K.; Matsushita, E.; Uno, C.; Satake, S.; Kuzuya, M. A 3-year prospective cohort study of dietary patterns and frailty risk among community-dwelling older adults. Clin. Nutr. 2021, 40, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Verspoor, E.; Voortman, T.; van Rooij, F.J.A.; Rivadeneira, F.; Franco, O.H.; Jong, J.C.K.-D.; Schoufour, J.D. Macronutrient intake and frailty: The Rotterdam Study. Eur. J. Nutr. 2020, 59, 2919–2928. [Google Scholar] [CrossRef]
- Cleasby, M.E.; Jamieson, P.M.; Atherton, P.J. Insulin resistance and sarcopenia: Mechanistic links between common co-morbidities. J. Endocrinol. 2016, 229, R67–R81. [Google Scholar] [CrossRef]
- Tumasian, R.A., 3rd; Harish, A.; Kundu, G.; Yang, J.H.; Ubaida-Mohien, C.; Gonzalez-Freire, M.; Kaileh, M.; Zukley, L.M.; Chia, C.W.; Lyashkov, A.; et al. Skeletal muscle transcriptome in healthy aging. Nat. Commun. 2021, 12, 1–16. [Google Scholar] [CrossRef]
- Augustin, L.S.A.; Kendall, C.W.C.; Jenkins, D.J.A.; Willett, W.C.; Astrup, A.; Barclay, A.W.; Björck, I.; Brand-Miller, J.C.; Brighenti, F.; Buyken, A.E.; et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr. Metab. Cardiovasc. Dis. 2015, 25, 795–815. [Google Scholar] [CrossRef] [PubMed]

| Combined | Women | Men | p | ||||
|---|---|---|---|---|---|---|---|
| n | 1024 | 523 | 501 | ||||
| Frailty Index | 0.11 | (0.08) | 0.11 | (0.08) | 0.11 | (0.08) | 0.653 |
| Age (years) | 74 | (7.86) | 73.3 | (8.03) | 74.72 | (7.62) | 0.004 |
| Sex (%men) | 501 | (48.90) | 0 | (0.00) | 501 | (100.00) | |
| Diabetes | 134 | (13.10) | 48 | (9.20) | 86 | (17.20) | <0.001 * |
| Fasting glucose (mg/dL) | 92.03 | (18.30) | 89.48 | (15.11) | 94.69 | (20.81) | <0.001 * |
| HBA1C (%) | 5.85 | (0.59) | 5.87 | (0.56) | 5.83 | (0.63) | 0.378 * |
| BMI (kg/m2) | 26.93 | (4.59) | 26.63 | (4.94) | 27.23 | (4.18) | 0.005 * |
| Total energy (kcal/day) | 1953.6 | (672.69) | 1805.94 | (606.92) | 2107.76 | (703.33) | <0.001 * |
| Glycemic load (g/day) ** | 107.54 | (42.78) | 99.32 | (39.29) | 116.12 | (44.59) | <0.001 * |
| Total grain (serv/day) | 6.01 | (2.65) | 5.41 | (2.28) | 6.64 | (2.86) | <0.001 * |
| Whole grains (serv/day) | 1.81 | (1.14) | 1.73 | (1.05) | 1.9 | (1.22) | 0.009 * |
| Non-whole grains (serv/day) | 4.2 | (2.18) | 3.69 | (1.74) | 4.73 | (2.44) | <0.001 * |
| Fiber: Carbohydrate | 0.1 | (0.02) | 0.1 | (0.03) | 0.09 | (0.02) | <0.001 * |
| Fiber (g/day) | 20.92 | (7.97) | 20.57 | (8.10) | 21.27 | (7.83) | 0.161 * |
| % energy Carbohydrate | 46.28 | (7.32) | 46.78 | (7.16) | 45.75 | (7.45) | 0.003 * |
| % energy PUFA | 7.91 | (1.73) | 8.12 | (1.67) | 7.7 | (1.77) | <0.001 * |
| % energy MUFA | 12.72 | (2.19) | 12.84 | (2.07) | 12.6 | (2.31) | 0.175 * |
| % energy SFA | 10.99 | (2.36) | 11 | (2.25) | 10.97 | (2.47) | 0.990 * |
| All | Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| β * | (SE) | p | β * | (SE) | p | β * | (SE) | p | |
| % Carbohydrate | |||||||||
| Med | 0.005 | (0.005) | 0.291 | 0.008 | (0.007) | 0.256 | 0.003 | (0.007) | 0.692 |
| High | 0.020 | (0.006) | 0.001 | 0.025 | (0.008) | 0.003 | 0.015 | (0.009) | 0.091 |
| Glycemic Load | |||||||||
| Med | 0.008 | (0.006) | 0.147 | −0.001 | (0.008) | 0.945 | 0.016 | (0.007) | 0.039 |
| High | 0.017 | (0.008) | 0.041 | 0.018 | (0.012) | 0.132 | 0.014 | (0.011) | 0.221 |
| Total Grains | |||||||||
| Med | 0.006 | (0.005) | 0.279 | −0.006 | (0.008) | 0.471 | 0.013 | (0.007) | 0.067 |
| High | 0.004 | (0.007) | 0.523 | −0.007 | (0.010) | 0.487 | 0.016 | (0.009) | 0.088 |
| Whole Grains | |||||||||
| Med | 0.006 | (0.005) | 0.261 | −0.001 | (0.007) | 0.923 | 0.010 | (0.007) | 0.168 |
| High | −0.007 | (0.006) | 0.191 | −0.017 | (0.008) | 0.037 | 0.003 | (0.008) | 0.679 |
| Non-whole grains | |||||||||
| Med | 0.011 | (0.005) | 0.031 | 0.004 | (0.007) | 0.554 | 0.017 | (0.007) | 0.015 |
| High | 0.012 | (0.007) | 0.059 | 0.001 | (0.009) | 0.947 | 0.025 | (0.009) | 0.007 |
| Fiber: Carbohydrate | |||||||||
| Med | −0.013 | (0.005) | 0.008 | −0.013 | (0.007) | 0.065 | −0.014 | (0.007) | 0.044 |
| High | −0.010 | (0.005) | 0.050 | −0.007 | (0.007) | 0.365 | −0.015 | (0.007) | 0.035 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, T.; Kafyra, M.; Jin, Y.; Chia, C.W.; Dedoussis, G.V.; Talegawkar, S.A.; Ferrucci, L. Quality Specific Associations of Carbohydrate Consumption and Frailty Index. Nutrients 2022, 14, 5072. https://doi.org/10.3390/nu14235072
Tanaka T, Kafyra M, Jin Y, Chia CW, Dedoussis GV, Talegawkar SA, Ferrucci L. Quality Specific Associations of Carbohydrate Consumption and Frailty Index. Nutrients. 2022; 14(23):5072. https://doi.org/10.3390/nu14235072
Chicago/Turabian StyleTanaka, Toshiko, Maria Kafyra, Yichen Jin, Chee W. Chia, George V. Dedoussis, Sameera A. Talegawkar, and Luigi Ferrucci. 2022. "Quality Specific Associations of Carbohydrate Consumption and Frailty Index" Nutrients 14, no. 23: 5072. https://doi.org/10.3390/nu14235072
APA StyleTanaka, T., Kafyra, M., Jin, Y., Chia, C. W., Dedoussis, G. V., Talegawkar, S. A., & Ferrucci, L. (2022). Quality Specific Associations of Carbohydrate Consumption and Frailty Index. Nutrients, 14(23), 5072. https://doi.org/10.3390/nu14235072





