Dietary Plant Protein Intake Can Reduce Maternal Insulin Resistance during Pregnancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Estimation of Dietary Intakes
2.3. Assessment of Glucose Homeostasis Indicators
2.4. Adjustment of Covariates
2.5. Animal Experiment
2.6. Laboratory Testing of Animal Experiment
2.7. Statistical Methods
3. Results
3.1. Characteristics of the Study Population
3.2. Results of the Population Study
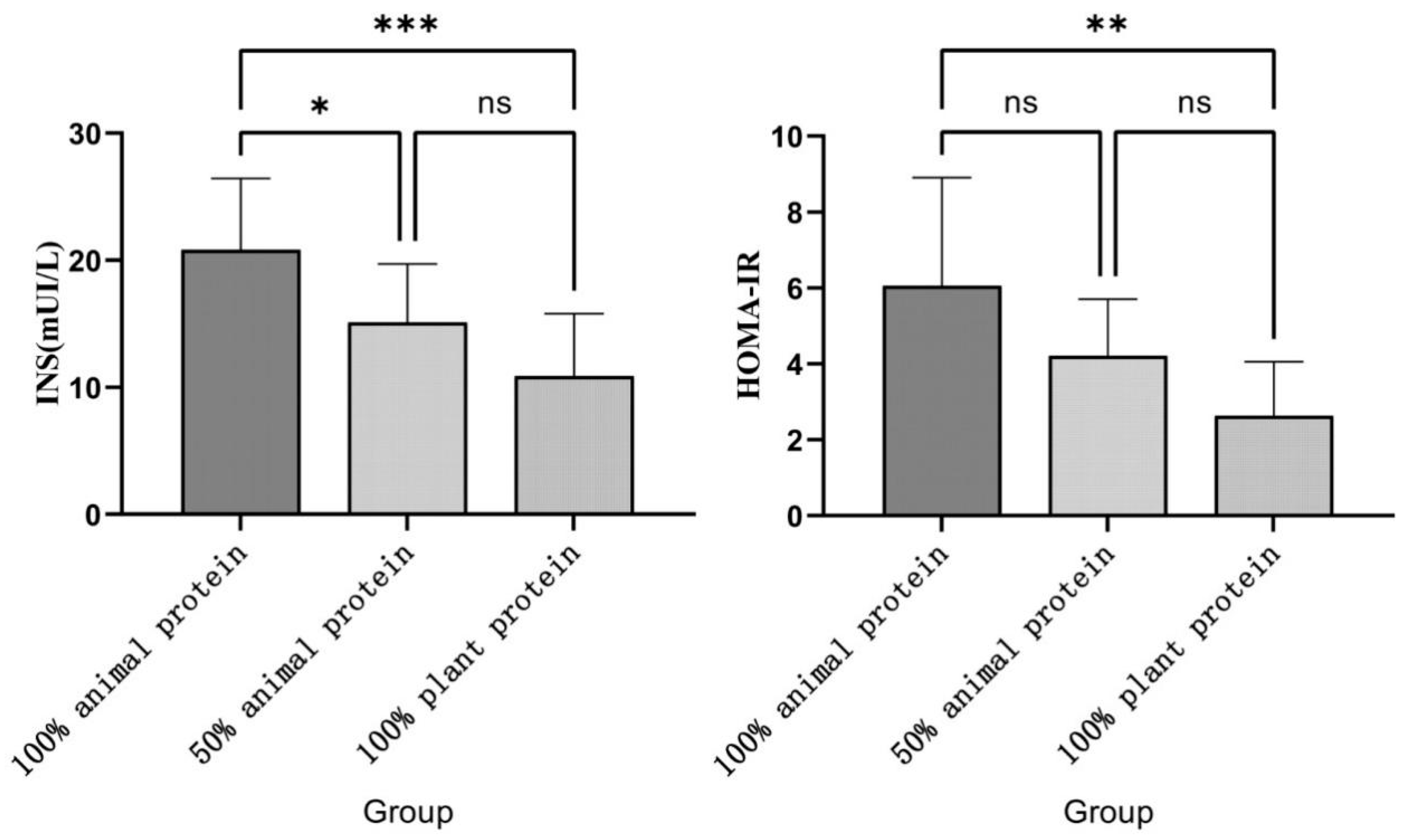
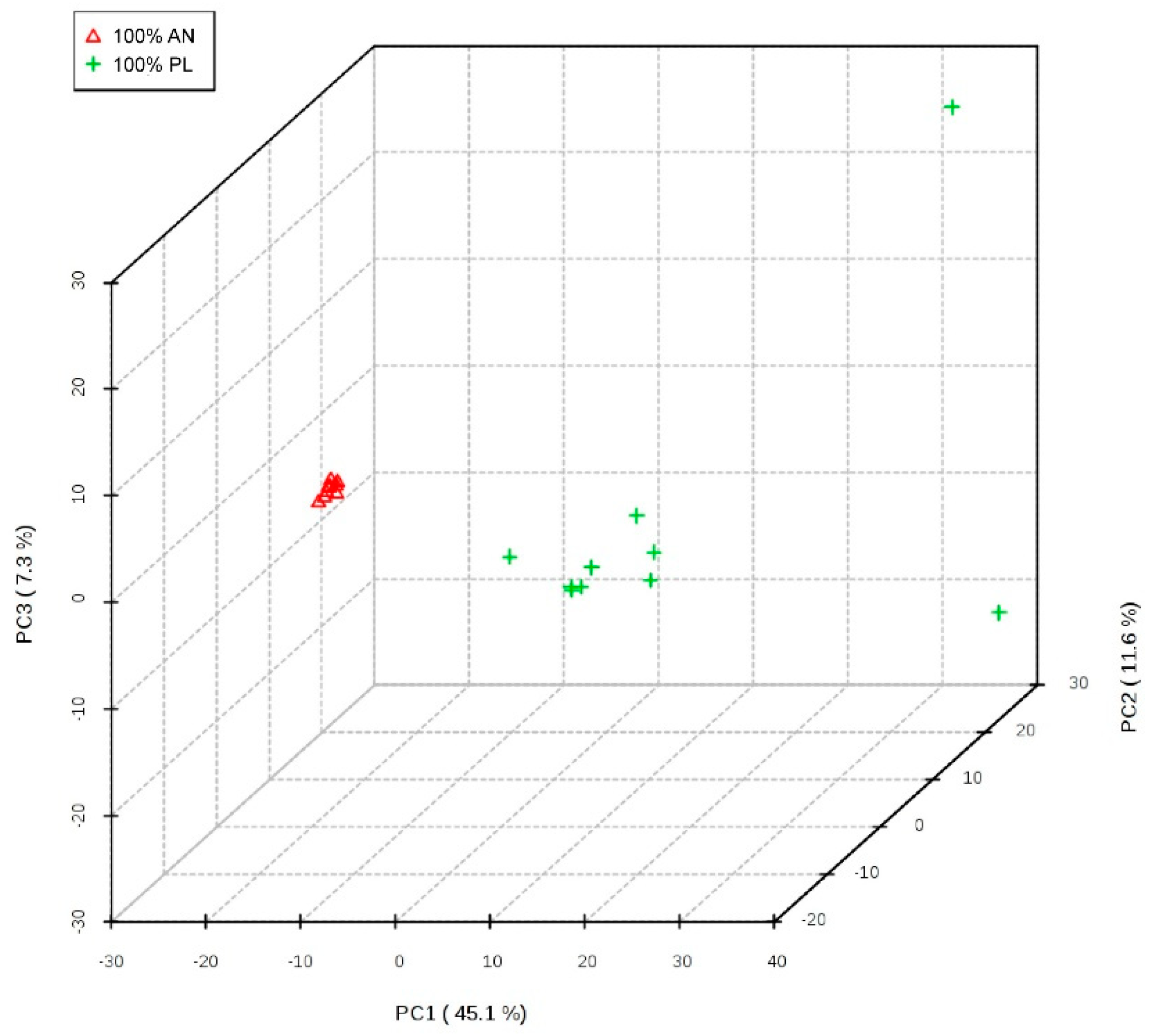
3.3. Results of the Animal Experiment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hill, M.A.; Yang, Y.; Zhang, L.; Sun, Z.; Jia, G.; Parrish, A.R.; Sowers, J.R. Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism 2021, 119, 154766. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-H.; Park, S.-Y.; Choi, C.S. Insulin Resistance: From Mechanisms to Therapeutic Strategies. Diabetes Metab. J. 2022, 46, 15–37. [Google Scholar] [CrossRef]
- Roberts, C.K.; Hevener, A.L.; Barnard, R.J. Metabolic Syndrome and Insulin Resistance: Underlying Causes and Modification by Exercise Training. Compr. Physiol. 2013, 3, 158. [Google Scholar] [CrossRef]
- Mazaki-Tovi, S.; Kanety, H.; Pariente, C.; Hemi, R.; Yissachar, E.; Schiff, E.; Cohen, O.; Sivan, E. Insulin sensitivity in late gestation and early postpartum period: The role of circulating maternal adipokines. Gynecol. Endocrinol. 2011, 27, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Newbern, D.; Freemark, M. Placental hormones and the control of maternal metabolism and fetal growth. Curr. Opin. Endocrinol. Diabetes 2011, 18, 409–416. [Google Scholar] [CrossRef] [PubMed]
- King, J.C. Physiology of pregnancy and nutrient metabolism. Am. J. Clin. Nutr. 2000, 71 (Suppl. S5), 1218S–1225S. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Jin, H.; Chen, L. Associations between insulin resistance and adverse pregnancy outcomes in women with gestational diabetes mellitus: A retrospective study. BMC Pregnancy Childbirth 2021, 21, 526. [Google Scholar] [CrossRef] [PubMed]
- Mastrogiannis, D.S.; Spiliopoulos, M.; Mulla, W.; Homko, C.J. Insulin resistance: The possible link between gestational diabetes mellitus and hypertensive disorders of pregnancy. Curr. Diabetes Rep. 2009, 9, 296–302. [Google Scholar] [CrossRef]
- Briana, D.D.; Malamitsi-Puchner, A. Adipocytokines in Normal and Complicated Pregnancies. Reprod. Sci. 2009, 16, 921–937. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.-Y.; Juan, J.; Xu, Q.; Su, R.; Hirst, J.E.; Yang, H.-X.; Qian-Qian, X.; Ri-Na, S. Increasing insulin resistance predicts adverse pregnancy outcomes in women with gestational diabetes mellitus. J. Diabetes 2020, 12, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Latini, G.; Marcovecchio, M.L.; Del Vecchio, A.; Gallo, F.; Bertino, E.; Chiarelli, F. Influence of environment on insulin sensitivity. Environ. Int. 2009, 35, 987–993. [Google Scholar] [CrossRef]
- Kahleova, H.; Rembert, E.; Alwarith, J.; Yonas, W.N.; Tura, A.; Holubkov, R.; Agnello, M.; Chutkan, R.; Barnard, N.D. Effects of a Low-Fat Vegan Diet on Gut Microbiota in Overweight Individuals and Relationships with Body Weight, Body Composition, and Insulin Sensitivity. A Randomized Clinical Trial. Nutrients 2020, 12, 2917. [Google Scholar] [CrossRef] [PubMed]
- Napoleão, A.; Fernandes, L.; Miranda, C.; Marum, A. Effects of Calorie Restriction on Health Span and Insulin Resistance: Classic Calorie Restriction Diet vs. Ketosis-Inducing Diet. Nutrients 2021, 13, 1302. [Google Scholar] [CrossRef] [PubMed]
- Ryan, B.J.; Schleh, M.W.; Ahn, C.; Ludzki, A.C.; Gillen, J.B.; Varshney, P.; Van Pelt, D.W.; Pitchford, L.M.; Chenevert, T.L.; Gioscia-Ryan, R.A.; et al. Moderate-Intensity Exercise and High-Intensity Interval Training Affect Insulin Sensitivity Similarly in Obese Adults. J. Clin. Endocrinol. Metab. 2020, 105, e2941–e2959. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G.; Lampousi, A.-M.; Knüppel, S.; Iqbal, K.; Schwedhelm, C.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food groups and risk of type 2 diabetes mellitus: A systematic review and meta-analysis of prospective studies. Eur. J. Epidemiology 2017, 32, 363–375. [Google Scholar] [CrossRef]
- Janiszewska, J.; Ostrowska, J.; Szostak-Węgierek, D. Milk and Dairy Products and Their Impact on Carbohydrate Metabolism and Fertility—A Potential Role in the Diet of Women with Polycystic Ovary Syndrome. Nutrients 2020, 12, 3491. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Drouin-Chartier, J.-P.; Li, Y.; Baden, M.Y.; Manson, J.E.; Willett, W.C.; Voortman, T.; Hu, F.B.; Bhupathiraju, S.N. Changes in Plant-Based Diet Indices and Subsequent Risk of Type 2 Diabetes in Women and Men: Three U.S. Prospective Cohorts. Diabetes Care 2021, 44, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zuurmond, M.G.; van der Schaft, N.; Nano, J.; Wijnhoven, H.A.H.; Ikram, M.A.; Franco, O.H.; Voortman, T. Plant versus animal based diets and insulin resistance, prediabetes and type 2 diabetes: The Rotterdam Study. Eur. J. Epidemiology 2018, 33, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.; Poulsen, C.W.; Kampmann, U.; Smedegaard, S.B.; Ovesen, P.G.; Fuglsang, J. Diet and Healthy Lifestyle in the Management of Gestational Diabetes Mellitus. Nutrients 2020, 12, 3050. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Huang, L.; Lin, L.; Chen, X.; Zhong, C.; Li, Q.; Li, N.; Gao, D.; Zhou, X.; Chen, R.; et al. The overall plant-based diet index during pregnancy and risk of gestational diabetes mellitus: A prospective cohort study in China. Br. J. Nutr. 2021, 126, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Riccardi, G.; Giacco, R.; Rivellese, A. Dietary fat, insulin sensitivity and the metabolic syndrome. Clin. Nutr. 2004, 23, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Morenga, L.T.; Docherty, P.; Williams, S.; Mann, J. The Effect of a Diet Moderately High in Protein and Fiber on Insulin Sensitivity Measured Using the Dynamic Insulin Sensitivity and Secretion Test (DISST). Nutrients 2017, 9, 1291. [Google Scholar] [CrossRef]
- Zhao, L.-G.; Zhang, Q.-L.; Liu, X.-L.; Wu, H.; Zheng, J.-L.; Xiang, Y.-B. Dietary protein intake and risk of type 2 diabetes: A dose–response meta-analysis of prospective studies. Eur. J. Nutr. 2019, 58, 1351–1367. [Google Scholar] [CrossRef]
- Azemati, B.; Rajaram, S.; Jaceldo-Siegl, K.; Sabate, J.; Shavlik, D.; Fraser, G.E.; Haddad, E.H. Animal-Protein Intake Is Associated with Insulin Resistance in Adventist Health Study 2 (AHS-2) Calibration Substudy Participants: A Cross-Sectional Analysis. Curr. Dev. Nutr. 2017, 1, e000299. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Xu, Q.; Jiang, R.; Han, T.; Sun, C.; Na, L. Dietary Protein Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Meta-Analysis of Cohort Studies. Nutrients 2017, 9, 982. [Google Scholar] [CrossRef] [PubMed]
- Viguiliouk, E.; Stewart, S.E.; Jayalath, V.H.; Ng, A.P.; Mirrahimi, A.; De Souza, R.J.; Hanley, A.J.; Bazinet, R.P.; Mejia, S.B.; Leiter, L.A.; et al. Effect of Replacing Animal Protein with Plant Protein on Glycemic Control in Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2015, 7, 9804–9824. [Google Scholar] [CrossRef]
- Elango, R.; Ball, R.O. Protein and Amino Acid Requirements during Pregnancy. Adv. Nutr. Int. Rev. J. 2016, 7, 839S–844S. [Google Scholar] [CrossRef] [PubMed]
- Stephens, T.V.; Payne, M.; Ball, R.O.; Pencharz, P.B.; Elango, R. Protein Requirements of Healthy Pregnant Women during Early and Late Gestation Are Higher than Current Recommendations. J. Nutr. 2015, 145, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Heng, J.; Tian, M.; Song, H.; Chen, F.; Guan, W.; Zhang, S. Amino acid transportation, sensing and signal transduction in the mammary gland: Key molecular signalling pathways in the regulation of milk synthesis. Nutr. Res. Rev. 2020, 33, 287–297. [Google Scholar] [CrossRef]
- White, P.J.; McGarrah, R.W.; Herman, M.A.; Bain, J.R.; Shah, S.H.; Newgard, C.B. Insulin action, type 2 diabetes, and branched-chain amino acids: A two-way street. Mol. Metab. 2021, 52, 101261. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Shao, J.; Wu, C.-Y.; Shu, L.; Dong, W.; Liu, Y.; Chen, M.; Wynn, R.M.; Wang, J.; Wang, J.; et al. Targeting BCAA Catabolism to Treat Obesity-Associated Insulin Resistance. Diabetes 2019, 68, 1730–1746. [Google Scholar] [CrossRef] [PubMed]
- Nie, C.; He, T.; Zhang, W.; Zhang, G.; Ma, X. Branched Chain Amino Acids: Beyond Nutrition Metabolism. Int. J. Mol. Sci. 2018, 19, 954. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Lin, X.; Li, X.; Hu, Z.; Hou, Q.; Wang, Y.; Wang, Z. Integration of transcriptomics and metabolomics provides metabolic and functional insights into reduced insulin secretion in MIN6 β-cells exposed to deficient and excessive arginine. FASEB J. 2022, 36, e22206. [Google Scholar] [CrossRef] [PubMed]
- Halperin, F.; Mezza, T.; Li, P.; Shirakawa, J.; Kulkarni, R.N.; Goldfine, A.B. Insulin regulates arginine-stimulated insulin secretion in humans. Metabolism 2022, 128, 155117. [Google Scholar] [CrossRef] [PubMed]
- Hertzler, S.R.; Lieblein-Boff, J.C.; Weiler, M.; Allgeier, C. Plant Proteins: Assessing Their Nutritional Quality and Effects on Health and Physical Function. Nutrients 2020, 12, 3704. [Google Scholar] [CrossRef] [PubMed]
- Reddy, P.; Elkins, A.; Panozzo, J.; Rochfort, S.J. High-Throughput Analysis of Amino Acids for Protein Quantification in Plant and Animal-Derived Samples Using High Resolution Mass Spectrometry. Molecules 2021, 26, 7578. [Google Scholar] [CrossRef] [PubMed]
- Bao, W.; Bowers, K.; Tobias, D.K.; Hu, F.B.; Zhang, C. Prepregnancy Dietary Protein Intake, Major Dietary Protein Sources, and the Risk of Gestational Diabetes Mellitus. Diabetes Care 2013, 36, 2001–2008. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, M.; Asemi, Z. The Effect of Soy Intake on Metabolic Profiles of Women with Gestational Diabetes Mellitus. J. Clin. Endocrinol. Metab. 2015, 100, 4654–4661. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.; Scott, D.; Hodge, A.M.; English, D.R.; Giles, G.G.; Ebeling, P.R.; Sanders, K.M. Dietary protein intake and risk of type 2 diabetes: Results from the Melbourne Collaborative Cohort Study and a meta-analysis of prospective studies. Am. J. Clin. Nutr. 2016, 104, 1352–1365. [Google Scholar] [CrossRef] [PubMed]
- Sluijs, I.; Beulens, J.W.; Van Der A, D.L.; Spijkerman, A.M.; Grobbee, D.E.; van der Schouw, Y.T. Dietary Intake of Total, Animal, and Vegetable Protein and Risk of Type 2 Diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)-NL Study. Diabetes Care 2010, 33, 43–48. [Google Scholar] [CrossRef]
- Allman, B.R.; Fuentes, E.D.; Williams, D.K.; Turner, D.E.; Andres, A.; Børsheim, E. Obesity Status Affects the Relationship Between Protein Intake and Insulin Sensitivity in Late Pregnancy. Nutrients 2019, 11, 2190. [Google Scholar] [CrossRef] [PubMed]
- Kirigiti, M.A.; Frazee, T.; Bennett, B.; Arik, A.; Blundell, P.; Bader, L.; Bagley, J.; Frias, A.E.; Sullivan, E.L.; Roberts, C.T., Jr.; et al. Effects of pre- and postnatal protein restriction on maternal and offspring metabolism in the nonhuman primate. Am. J. Physiol. Integr. Comp. Physiol. 2020, 318, R929–R939. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.; Chashnidel, Y.; Abdollahi, A.; Yansari, A.T.; Khazari, B.; Mansouryar, M. Moderate over-feeding of different sources of metabolizable energy and protein improved gestational insulin resistance markers and maternal metabolic status of sheep around lambing. Theriogenology 2021, 161, 332–342. [Google Scholar] [CrossRef] [PubMed]
- Yue, S.-J.; Liu, J.; Wang, A.-T.; Meng, X.-T.; Yang, Z.-R.; Peng, C.; Guan, H.-S.; Wang, C.-Y.; Yan, D. Berberine alleviates insulin resistance by reducing peripheral branched-chain amino acids. Am. J. Physiol. Metab. 2019, 316, E73–E85. [Google Scholar] [CrossRef]
- Zhao, X.; Han, Q.; Liu, Y.; Sun, C.; Gang, X.; Wang, G. The Relationship between Branched-Chain Amino Acid Related Metabolomic Signature and Insulin Resistance: A Systematic Review. J. Diabetes Res. 2016, 2016, 2794591. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Fleeman, R.; Hlozkova, A.; Holubkov, R.; Barnard, N.D. A plant-based diet in overweight individuals in a 16-week randomized clinical trial: Metabolic benefits of plant protein. Nutr. Diabetes 2018, 8, 58. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Orozco, J.M.; Saxton, R.A.; Condon, K.J.; Liu, G.Y.; Krawczyk, P.A.; Scaria, S.M.; Harper, J.W.; Gygi, S.P.; Sabatini, D.M. SAMTOR is an S -adenosylmethionine sensor for the mTORC1 pathway. Science 2017, 358, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Inoki, K.; Kim, J.; Guan, K.-L. AMPK and mTOR in Cellular Energy Homeostasis and Drug Targets. Annu. Rev. Pharmacol. Toxicol. 2012, 52, 381–400. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Goraksha-Hicks, P.; Li, L.; Neufeld, T.P.; Guan, K.-L. Regulation of TORC1 by Rag GTPases in nutrient response. Nat. Cell Biol. 2008, 10, 935–945. [Google Scholar] [CrossRef] [PubMed]
- Sancak, Y.; Peterson, T.R.; Shaul, Y.D.; Lindquist, R.A.; Thoreen, C.C.; Bar-Peled, L.; Sabatini, D.M. The Rag GTPases Bind Raptor and Mediate Amino Acid Signaling to mTORC1. Science 2008, 320, 1496–1501. [Google Scholar] [CrossRef] [PubMed]
- Jewell, J.L.; Kim, Y.C.; Russell, R.C.; Yu, F.-X.; Park, H.W.; Plouffe, S.W.; Tagliabracci, V.S.; Guan, K.-L. Differential regulation of mTORC1 by leucine and glutamine. Science 2015, 347, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Meng, D.; Yang, Q.; Wang, H.; Melick, C.H.; Navlani, R.; Frank, A.R.; Jewell, J.L. Glutamine and asparagine activate mTORC1 independently of Rag GTPases. J. Biol. Chem. 2020, 295, 2890–2899. [Google Scholar] [CrossRef]
- Lee, S.; Dong, H.H. FoxO integration of insulin signaling with glucose and lipid metabolism. J. Endocrinol. 2017, 233, R67–R79. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.E.; Kanyicska, B.; Lerant, A.; Nagy, G. Prolactin: Structure, Function, and Regulation of Secretion. Physiol. Rev. 2000, 80, 1523–1631. [Google Scholar] [CrossRef] [PubMed]
- Ahnen, R.T.; Jonnalagadda, S.S.; Slavin, J.L. Role of plant protein in nutrition, wellness, and health. Nutr. Rev. 2019, 77, 735–747. [Google Scholar] [CrossRef] [PubMed]

| Component (g/kg) a | 100% Animal Protein | 50% Animal Protein | 100% Plant Protein |
|---|---|---|---|
| Total energy (kcal/kg) a | 3832.48 | 3832.48 | 3832.48 |
| Protein | 200.00 | 200.00 | 200.00 |
| Fat | 70.00 | 70.00 | 70.00 |
| Carbohydrates | 600.62 | 600.62 | 600.62 |
| Dietary fiber | 50.00 | 50.00 | 50.00 |
| Milk protein concentrate | 241.08 | 120.54 | - |
| Soy protein isolate | - | 110.07 | 220.14 |
| L-cystine | 3.00 | 3.00 | 3.00 |
| Corn starch | 360.35 | 361.67 | 362.98 |
| Maltodextrin | 132.00 | 132.00 | 132.00 |
| Sucrose | 100.00 | 100.00 | 100.00 |
| Cellulose | 50.00 | 49.86 | 49.71 |
| Oil | 66.07 | 68.01 | 69.96 |
| Mineral mix | 35.00 | 35.00 | 35.00 |
| Vitamin mix | 10.00 | 10.00 | 10.00 |
| Choline bitartrate | 2.50 | 2.50 | 2.50 |
| BHT b | 0.01 | 0.01 | 0.01 |
| Distilled water | 0.00 | 7.35 | 14.70 |
| Characteristics | n (%) | GLU (mmol/L) | INS (pmol/L) | HOMA-IR |
|---|---|---|---|---|
| All subjects | 1034 (100) | 4.61 (4.31, 4.96) | 57.0 (38.6, 94.4) | 2.01 (1.31, 3.29) |
| pre-pregnancy BMI | ||||
| <18.5 | 22 (2.1) | 4.28 (3.98, 4.59) c | 29.7 (19.6, 44.8) c | 0.88 (0.60, 1.55) c |
| 18.5–23.9 | 193 (18.7) | 4.56 (4.29, 4.84) c | 46.9 (34.1, 74.2) c | 1.60 (1.14, 2.41) c |
| ≥24.0 | 252 (24.4) | 4.70 (4.37, 5.05) c | 69.4 (47.2, 107.6) c | 2.32 (1.65, 3.84) c |
| Gestation period | ||||
| First | 150 (14.5) | 4.76 (4.55, 5.05) c | 48.4 (37.0, 89.0) c | 1.77 (1.29, 3.18) c |
| Second | 305 (29.5) | 4.49 (4.22, 4.84) c | 53.5 (37.2, 84.4) c | 1.84 (1.19, 2.65) c |
| Third | 277 (26.8) | 4.47 (4.22, 4.79) c | 73.6 (53.6, 108.9) c | 2.40 (1.81, 3.76) c |
| Parity | ||||
| Primiparous | 42 (4.1) | 4.71 (4.54, 5.02) | 49.2 (39.1, 72.1) | 1.76 (1.26, 2.56) |
| Non-primiparous | 675 (65.3) | 4.61 (4.31, 4.95) | 55.2 (38.8, 87.0) | 1.91 (1.30, 2.91) |
| Age | ||||
| 20–24 | 320 (30.9) | 4.51 (4.22, 4.88) c | 62.1 (40.1, 100.7) c | 2.15 (1.37, 3.43) |
| 25–29 | 313 (30.3) | 4.59 (4.34, 4.86) c | 62.0 (39.8, 89.9) c | 2.03 (1.30, 3.28) |
| 30–34 | 257 (24.9) | 4.65 (4.31, 5.11) c | 61.0 (38.3, 98.2) c | 2.18 (1.35, 3.68) |
| 35–39 | 122 (11.8) | 4.78 (4.53, 5.11) c | 48.1 (33.2, 62.8) c | 1.80 (1.14, 2.33) |
| 40–44 | 22 (2.1) | 4.83 (4.59, 5.11) c | 37.4 (28.7, 50.5) c | 1.28 (1.02, 1.83) |
| Race | ||||
| Mexican | 250 (24.4) | 4.63 (4.27, 5.03) | 66.6 (45.5, 102.5) c | 2.22 (1.56, 3.63) c |
| Other Hispanic | 73 (7.1) | 4.69 (4.38, 5.00) | 70.4 (48.8, 100.7) c | 2.31 (1.81, 3.28) c |
| Non-Hispanic White | 445 (43.5) | 4.61 (4.33, 4.88) | 50.3 (33.3, 79.1) c | 1.77 (1.12, 2.69) c |
| Non-Hispanic Black | 165 (16.1) | 4.57 (4.23, 4.98) | 62.0 (40.1, 97.3) c | 2.10 (1.32, 3.47) c |
| Other race | 101 (9.9) | 4.66 (4.38, 5.11) | 58.8 (39.2, 88.1) c | 2.09 (1.25, 3.28) c |
| Education | ||||
| Less than 9th grade | 76 (7.4) | 4.61 (4.23, 4.94) | 53.5 (40.6, 90.8) | 1.90 (1.32, 3.28) |
| 9–11th grade | 176 (17.0) | 4.57 (4.28, 4.86) | 66.7 (46.9, 104.1) | 2.28 (1.69, 3.53) |
| High school graduate | 214 (20.7) | 4.62 (4.31, 5.00) | 62.1 (40.1, 104.5) | 2.19 (1.37, 3.76) |
| AA degree | 294 (28.4) | 4.63 (4.33, 4.91) | 55.6 (37.9, 91.3) | 1.96 (1.27, 3.13) |
| College graduate or above | 273 (26.4) | 4.61 (4.33, 5.00) | 53.2 (33.4, 80.6) | 1.83 (1.10, 2.76) |
| Family income b | ||||
| <1.00 | 244 (23.6) | 4.61 (4.31, 4.94) | 55.6 (39.2, 90.6) | 1.98 (1.32, 3.15) |
| 1.00–2.99 | 213 (20.6) | 4.61 (4.28, 5.00) | 56.0 (39.1, 94.5) | 1.90 (1.31, 3.32) |
| 3.00–4.99 | 129 (12.5) | 4.59 (4.35, 4.93) | 62.2 (40.9, 91.5) | 2.09 (1.31, 3.37) |
| ≥5.00 | 177 (17.1) | 4.64 (4.35, 5.05) | 49.2 (33.3, 81.6) | 1.75 (1.10, 2.90) |
| Variables | GLU | INS | HOMA-IR | ||
|---|---|---|---|---|---|
| Total protein intake | Model 1 a | β (95%CI) | 0.01 (−0.06, 0.08) | 8.74 (−4.58, 22.07) | 0.46 (−0.19, 1.10) |
| p-value | 0.724 | 0.198 | 0.168 | ||
| Model 2 b | β (95%CI) | −0.01 (−0.08, 0.06) | 5.47 (−11.85, 22.78) | 0.28 (−0.56, 1.12) | |
| p-value | 0.704 | 0.535 | 0.513 |
| Variables | GLU (mmol/L) | INS (mIU/L) | HOMA-IR | ||
|---|---|---|---|---|---|
| animal protein intake | Model 1 a | β (95%CI) | −0.09 (−0.16, −0.02) | 7.31 (−6.02, 20.65) | 0.31 (−0.34, 0.96) |
| p-value | 0.015 | 0.282 | 0.351 | ||
| Model 2 b | β (95%CI) | −0.06 (−0.13, 0.01) | 3.49 (−14.12, 21.10) | 0.20 (−0.67, 1.05) | |
| p-value | 0.103 | 0.696 | 0.667 | ||
| plant protein intake | Model 1 a | β (95%CI) | −0.03 (−0.10, 0.04) | −18.73 (−31.97, −5.49) | −0.96 (−1.60, −0.32) |
| p-value | 0.398 | 0.006 | 0.004 | ||
| Model 2 b | β (95%CI) | 0.00 (−0.06, 0.07) | −20.60 (−37.91, −3.30) | −1.04 (−1.89, −0.20) | |
| p-value | 0.892 | 0.020 | 0.015 | ||
| AP ratio | Model 1 a | β (95%CI) | −0.03 (−0.10, 0.04) | 12.39 (−0.91, 25.69) | 0.63 (−0.02, 1.27) |
| p-value | 0.360 | 0.068 | 0.058 | ||
| Model 2 b | β (95%CI) | −0.05 (−0.12, 0.02) | 13.91 (−3.66, 31.48) | 0.73 (−0.13, 1.59) | |
| p-value | 0.175 | 0.120 | 0.096 |
| Variables | Gestation Period | INS (mIU/L) | HOMA-IR | |
|---|---|---|---|---|
| Plant protein intake | First trimester | β (95%CI) | −26.23 (−60.73, 8.27) | −1.25 (−2.88, 0.39) |
| p-value | 0.133 | 0.133 | ||
| Second trimester | β (95%CI) | −4.03 (−19.77, 11.71) | −0.19 (−0.81, 0.43) | |
| p-value | 0.614 | 0.541 | ||
| Third trimester | β (95%CI) | −38.47 (−76.99, 0.04) | −2.10 (−4.04, −0.15) | |
| p-value | 0.050 | 0.035 | ||
| AP ratio | First trimester | β (95%CI) | 18.69 (−15.97, 53.34) | 0.93 (−0.70, −2.57) |
| p-value | 0.285 | 0.258 | ||
| Second trimester | β (95%CI) | 3.96 (−11.53, −19.45) | 0.12 (−0.50, 0.73) | |
| p-value | 0.614 | 0.707 | ||
| Third trimester | β (95%CI) | 36.76 (−2.06, 75.57) | 1.96 (0.01, 3.91) | |
| p-value | 0.063 | 0.048 |
| Group | 100% Animal Protein Mean ± sd | 50% Animal Protein Mean ± sd | 100% Plant Protein Mean ± sd | p for ANOVA | p for Trend |
|---|---|---|---|---|---|
| GLU (mmol/L) | 6.40 ± 2.15 | 6.25 ± 1.11 | 5.61 ± 1.74 | 0.557 | 0.314 |
| INS (mIU/L) | 20.83 ± 5.62 | 15.09 ± 4.60 | 10.88 ± 4.91 | 0.001 | 0.000 |
| HOMA-IR | 6.06 ± 2.85 | 4.22 ± 1.49 | 2.63 ± 1.42 | 0.007 | 0.002 |
| Metabolites | log2FC a | p-Value | VIP |
|---|---|---|---|
| L-Tyrosine | −9.19 | <0.000 | 1.55 |
| L-Histidine | −5.37 | <0.000 | 1.55 |
| L-asparagine | −4.73 | <0.000 | 1.55 |
| 5-Aminolevulinic acid | −7.41 | <0.000 | 1.55 |
| Phenylalanine | −6.43 | <0.000 | 1.55 |
| Glutamine | −3.41 | <0.000 | 1.55 |
| Threonine | −2.71 | <0.000 | 1.54 |
| Succinic acid | −2.04 | <0.000 | 1.50 |
| N-Acetylaspartate | −6.99 | <0.000 | 1.50 |
| 2-hydroxy-6-methylisonicotinic acid | 3.97 | <0.000 | 1.50 |
| N, N-Dimethylarginine | 6.42 | <0.000 | 1.49 |
| Arginine | 6.14 | <0.000 | 1.49 |
| Gly | 3.85 | <0.000 | 1.46 |
| 1-Methylhistamine | −3.80 | <0.000 | 1.45 |
| Pantothenate | −7.00 | <0.000 | 1.45 |
| L-Leucine | −5.49 | <0.000 | 1.44 |
| L-Glutamic acid | −3.63 | <0.000 | 1.43 |
| L-Citrulline | 3.87 | <0.000 | 1.43 |
| D-Glucosamine-6-phosphate | 6.71 | <0.000 | 1.42 |
| N-Methyl-L-proline | 5.80 | <0.000 | 1.37 |
| Glutamic acid | 1.97 | <0.000 | 1.35 |
| Thiamine | 3.98 | <0.000 | 1.33 |
| Lysine | 6.59 | <0.000 | 1.33 |
| Riboflavin | 5.29 | <0.000 | 1.30 |
| N8-Acetylspermidine | 3.27 | <0.000 | 1.30 |
| Pathway Name | KEGG Pathway ID | Adjusted p-Value |
|---|---|---|
| Biosynthesis of amino acids | rno01230 | <0.000 |
| Alanine, aspartate, and glutamate metabolism | rno00250 | <0.000 |
| GABAergic synapse | rno04727 | <0.000 |
| Arginine biosynthesis | rno00220 | 0.000 |
| FoxO signaling pathway | rno04068 | 0.000 |
| Glutamatergic synapse | rno04724 | 0.002 |
| Glyoxylate and dicarboxylate metabolism | rno00630 | 0.003 |
| Prolactin signaling pathway | rno04917 | 0.004 |
| Histidine metabolism | rno00340 | 0.005 |
| D-Glutamine and D-glutamate metabolism | rno00471 | 0.006 |
| Glycine, serine, and threonine metabolism | rno00260 | 0.006 |
| mTOR signaling pathway | rno04150 | 0.007 |
| Tyrosine metabolism | rno00350 | 0.008 |
| Phenylalanine metabolism | rno00360 | 0.012 |
| Pyrimidine metabolism | rno00240 | 0.014 |
| Purine metabolism | rno00230 | 0.015 |
| Bile secretion | rno04976 | 0.016 |
| Taurine and hypotaurine metabolism | rno00430 | 0.016 |
| cAMP signaling pathway | rno04024 | 0.022 |
| Cholesterol metabolism | rno04979 | 0.028 |
| Phospholipase D signaling pathway | rno04072 | 0.032 |
| Thiamine metabolism | rno00730 | 0.033 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, Y.; Yang, C.; Zhong, J.; Hou, Y.; Xie, K.; Wang, L. Dietary Plant Protein Intake Can Reduce Maternal Insulin Resistance during Pregnancy. Nutrients 2022, 14, 5039. https://doi.org/10.3390/nu14235039
Hong Y, Yang C, Zhong J, Hou Y, Xie K, Wang L. Dietary Plant Protein Intake Can Reduce Maternal Insulin Resistance during Pregnancy. Nutrients. 2022; 14(23):5039. https://doi.org/10.3390/nu14235039
Chicago/Turabian StyleHong, Yuting, Chen Yang, Jinjing Zhong, Yanmei Hou, Kui Xie, and Linlin Wang. 2022. "Dietary Plant Protein Intake Can Reduce Maternal Insulin Resistance during Pregnancy" Nutrients 14, no. 23: 5039. https://doi.org/10.3390/nu14235039
APA StyleHong, Y., Yang, C., Zhong, J., Hou, Y., Xie, K., & Wang, L. (2022). Dietary Plant Protein Intake Can Reduce Maternal Insulin Resistance during Pregnancy. Nutrients, 14(23), 5039. https://doi.org/10.3390/nu14235039






