Impact of Energy and Protein Delivery to Critically Ill Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocols and Registration
2.2. Search Strategies
2.3. Study Selection
2.4. Eligibility Criteria
2.5. Risk of Bias Assessment
2.6. Grading of Recommendations Assessment, Development and Evaluation Approach
2.7. Data Extraction
2.8. Data Summarization, Heterogeneity, and Synthesis
3. Results
3.1. Literature Search
3.2. Characteristics of Included Studies
3.3. Risk of Bias in Included Studies
3.4. Outcomes
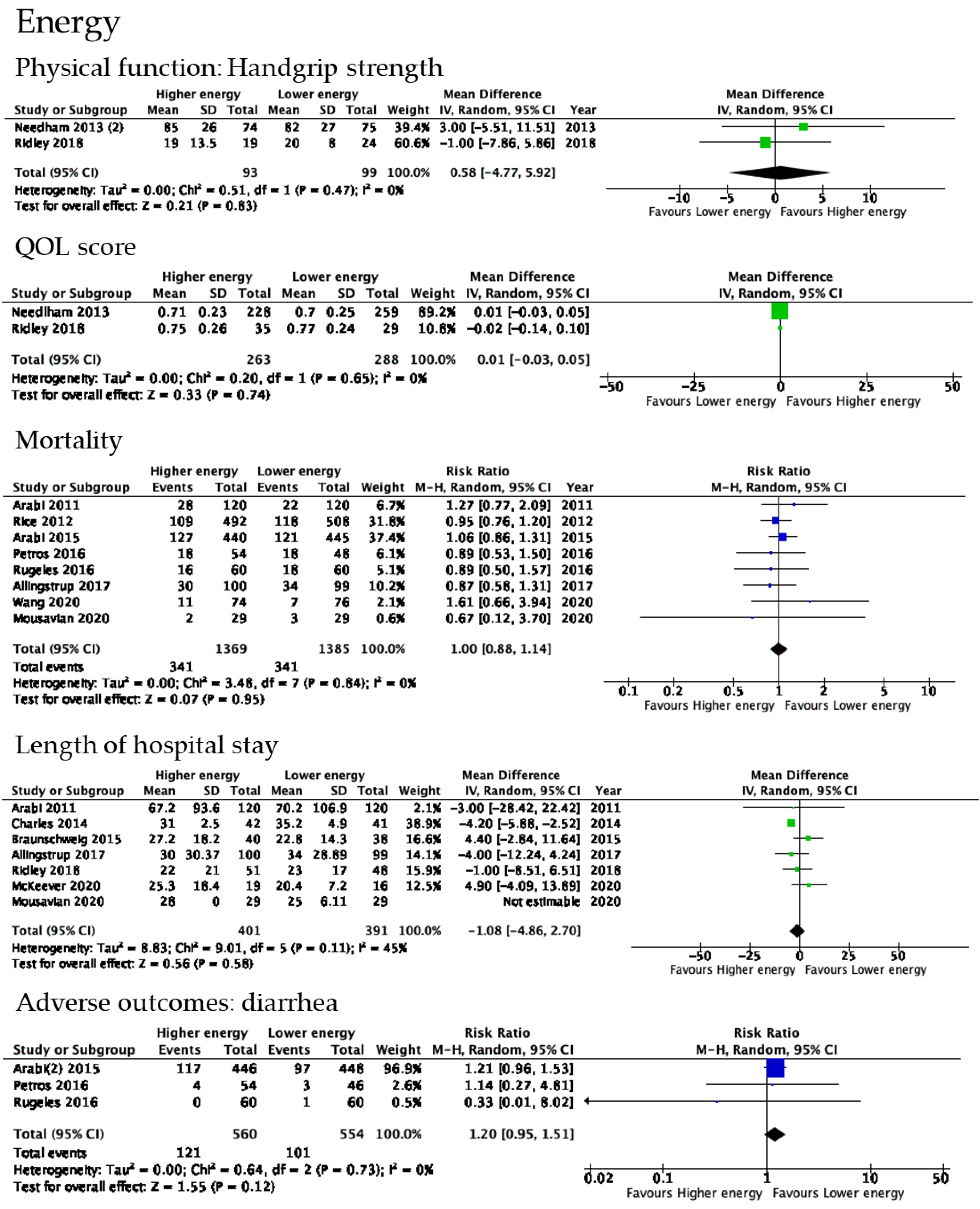
3.5. Primary and Secondary Outcomes of Energy Delivery
3.5.1. ADL
3.5.2. Physical Functions
3.5.3. Changes in Muscle Mass
3.5.4. QOL Scores
3.5.5. Mortality
3.5.6. Length of Hospital Stay
3.5.7. Adverse Events
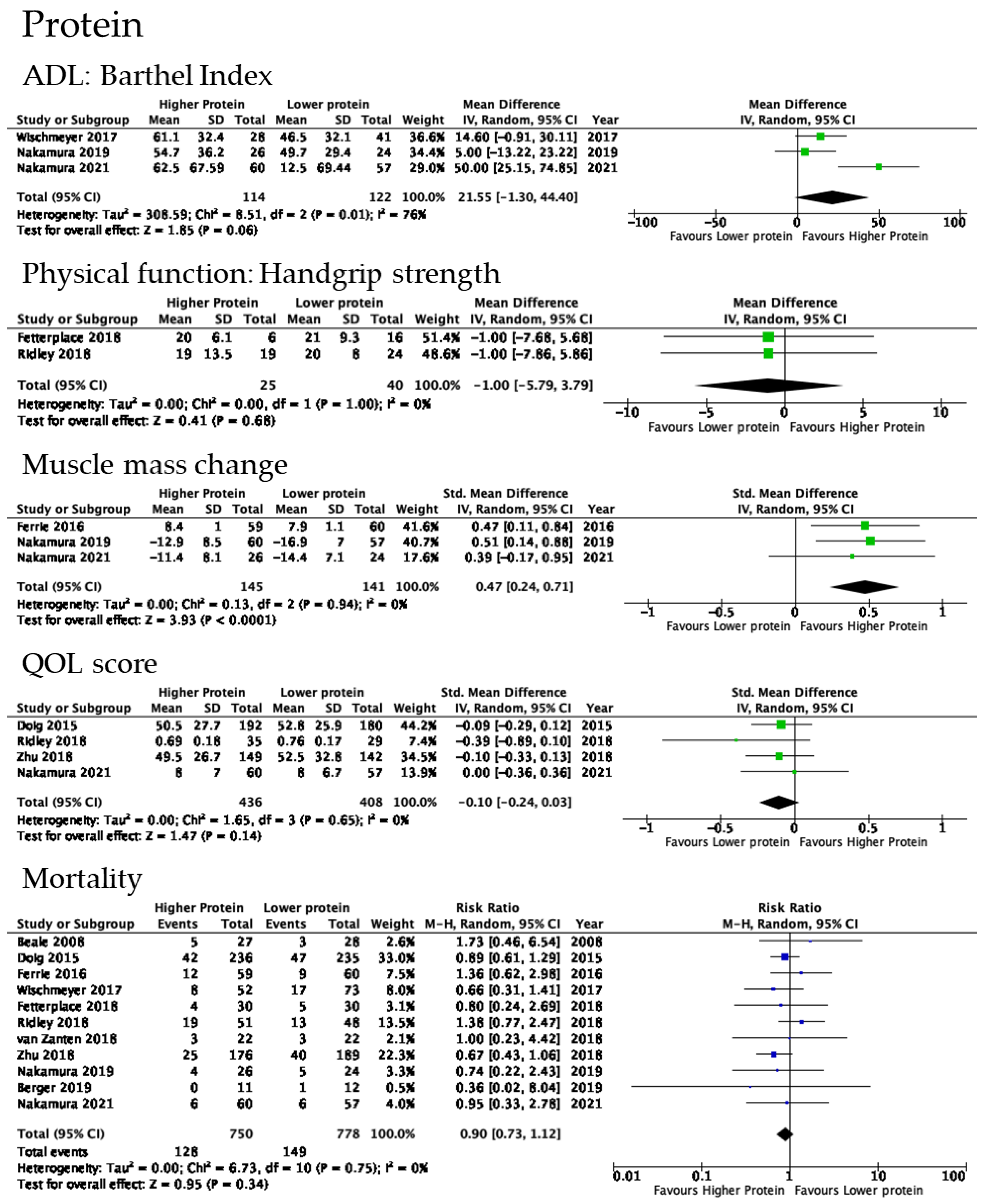
3.6. Primary and Secondary Outcomes of Protein Delivery
3.6.1. ADL
3.6.2. Physical Functions
3.6.3. Changes in Muscle Mass
3.6.4. QOL Scores
3.6.5. Mortality
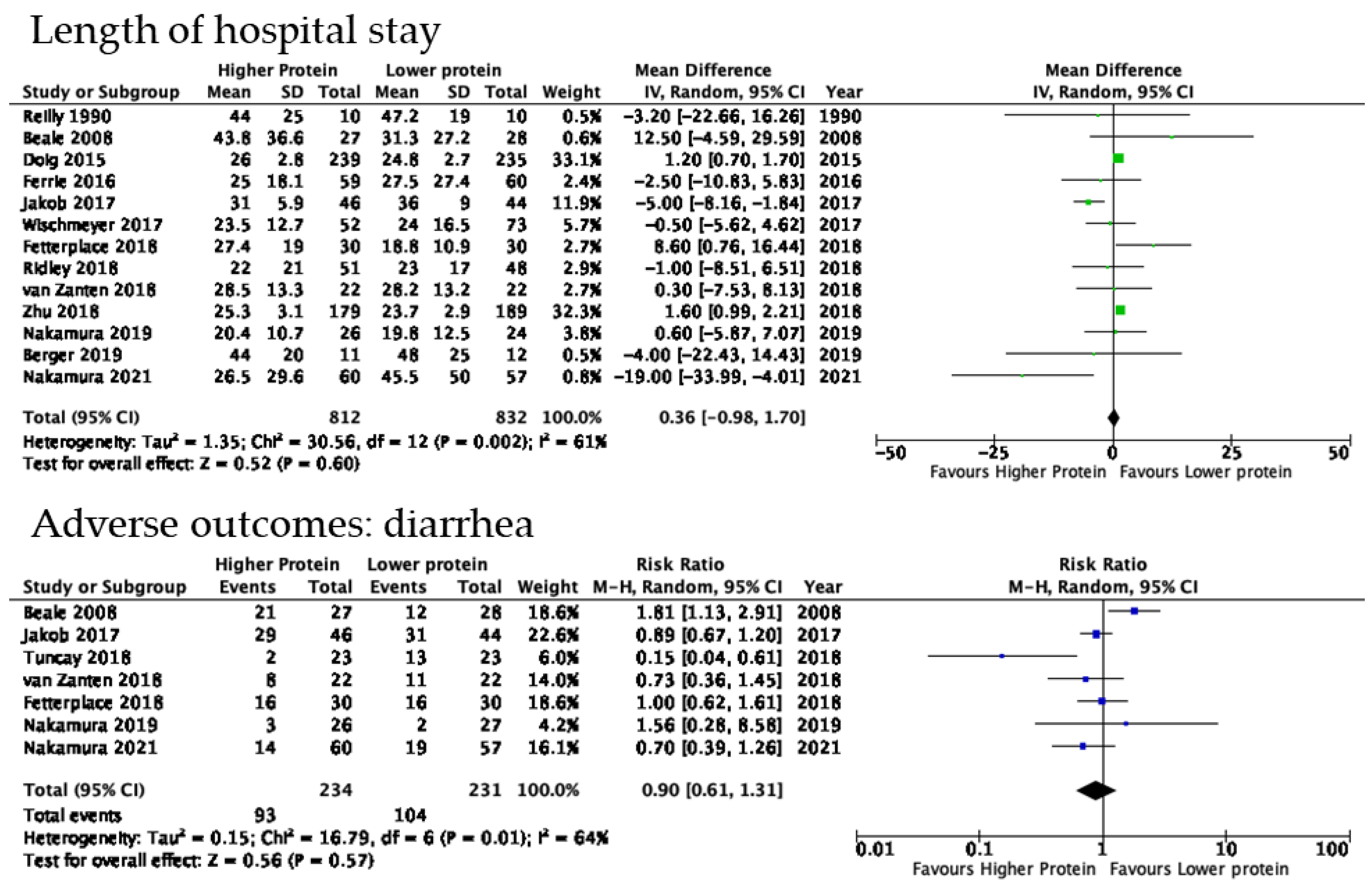
3.6.6. Length of Hospital Stay
3.6.7. Adverse Events
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nakanishi, N.; Oto, J.; Tsutsumi, R.; Iuchi, M.; Onodera, M.; Nishimura, M. Upper and lower limb muscle atrophy in critically ill patients: An observational ultrasonography study. Intensive Care Med. 2018, 44, 263–264. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, N.; Liu, K.; Kawakami, D.; Kawai, Y.; Morisawa, T.; Nishida, T.; Sumita, H.; Unoki, T.; Hifumi, T.; Iida, Y.; et al. Post-Intensive Care Syndrome and its new challenges in Coronavirus Disease 2019 (COVID-19) pandemic: A review of recent advances and perspectives. J. Clin. Med. 2021, 10, 3870. [Google Scholar] [CrossRef]
- Singer, P.; Blaser, A.R.; Berger, M.M.; Alhazzani, W.; Calder, P.C.; Casaer, M.P.; Hiesmayr, M.; Mayer, K.; Montejo, J.C.; Pichard, C.; et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 2019, 38, 48–79. [Google Scholar] [CrossRef] [PubMed]
- Compher, C.; Bingham, A.L.; McCall, M.; Patel, J.; Rice, T.W.; Braunschweig, C.; McKeever, L. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: The American Society for Parenteral and Enteral Nutrition. JPEN J. Parenter. Enter. Nutr. 2022, 46, 12–41. [Google Scholar] [CrossRef] [PubMed]
- Egi, M.; Ogura, H.; Yatabe, T.; Atagi, K.; Inoue, S.; Iba, T.; Kakihana, Y.; Kawasaki, T.; Kushimoto, S.; Kuroda, Y.; et al. The Japanese clinical practice guidelines for management of sepsis and septic shock 2020 (J-SSCG 2020). J. Intensive Care 2021, 9, 53. [Google Scholar] [CrossRef]
- Japanese Society of Intensive Care Medicine. Japanese guidelines for nutrition support therapy in the adult and pediatric critically ill patients. J. Jpn. Soc. Intensive Care Med. 2016, 23, 185–281. [Google Scholar] [CrossRef]
- Casaer, M.P.; Mesotten, D.; Hermans, G.; Wouters, P.J.; Schetz, M.; Meyfroidt, G.; Van Cromphaut, S.; Ingels, C.; Meersseman, P.; Muller, J.; et al. Early versus late parenteral nutrition in critically ill adults. N. Engl. J. Med. 2011, 365, 506–517. [Google Scholar] [CrossRef]
- Moher, D.; Booth, A.; Stewart, L. How to reduce unnecessary duplication: Use PROSPERO. Bjog 2014, 121, 784–786. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, W65-94. [Google Scholar] [CrossRef]
- Collin, C.; Wade, D.T.; Davies, S.; Horne, V. The Barthel ADL Index: A reliability study. Int. Disabil. Stud. 1988, 10, 61–63. [Google Scholar] [CrossRef]
- Ottenbacher, K.J.; Hsu, Y.; Granger, C.V.; Fiedler, R.C. The reliability of the functional independence measure: A quantitative review. Arch Phys. Med. Rehabil. 1996, 77, 1226–1232. [Google Scholar] [CrossRef]
- Hermans, G.; Clerckx, B.; Vanhullebusch, T.; Segers, J.; Vanpee, G.; Robbeets, C.; Casaer, M.P.; Wouters, P.; Gosselink, R.; Van Den Berghe, G. Interobserver agreement of Medical Research Council sum-score and handgrip strength in the intensive care unit. Muscle Nerve 2012, 45, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Pavasini, R.; Guralnik, J.; Brown, J.C.; di Bari, M.; Cesari, M.; Landi, F.; Vaes, B.; Legrand, D.; Verghese, J.; Wang, C.; et al. Short Physical Performance Battery and all-cause mortality: Systematic review and meta-analysis. BMC Med. 2016, 14, 215. [Google Scholar] [CrossRef]
- Cataneo, D.C.; Kobayasi, S.; Carvalho, L.R.; Paccanaro, R.C.; Cataneo, A.J. Accuracy of six minute walk test, stair test and spirometry using maximal oxygen uptake as gold standard. Acta Cir. Bras. 2010, 25, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, L.; Geisler, C.; Pourhassan, M.; Braun, W.; Glüer, C.C.; Bosy-Westphal, A.; Müller, M.J. What is the best reference site for a single MRI slice to assess whole-body skeletal muscle and adipose tissue volumes in healthy adults? Am. J. Clin. Nutr. 2015, 102, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Katayama, S.; Okura, K.; Okamura, M.; Nawata, K.; Nakanishi, N.; Shinohara, A. Skeletal muscle mass assessment in critically ill patients: Method and application. Ann. Cancer Res. Ther. 2022, 30, 93–99. [Google Scholar] [CrossRef]
- Sonoo, T.; Hiromu, N.; Kibata, A.; Fukushima, K.; Daidoji, H.; Hashimoto, H.; Nakamura, K. Muscle volume measurement for intensive care unit acquired weakness using computed tomography: A pilot study. J. Med. Diagn. Methods 2018, 7, 3. [Google Scholar] [CrossRef]
- Lins, L.; Carvalho, F.M. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4, 2050312116671725. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Hays, R.D.; Morales, L.S. The RAND-36 measure of health-related quality of life. Ann. Med. 2001, 33, 350–357. [Google Scholar] [CrossRef]
- Golicki, D.; Młyńczak, K. Measurement properties of the EQ-5D-Y: A systematic review. Value Health 2022, 25, 1910–1921. [Google Scholar] [CrossRef] [PubMed]
- The EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G. Chapter 8: Assessing Risk of Bias in Included Studies. 2011. Available online: https://handbook-5-1.cochrane.org/ (accessed on 24 October 2022).
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490. [Google Scholar] [CrossRef]
- GRADEpro, G. GRADEpro GDT: GRADEpro Guideline Development Tool [Software]; Developed by Evidence Prime, Inc.; McMaster University: Hamilton, ON, Canada, 2015. [Google Scholar]
- Needham, D.M.; Dinglas, V.D.; Bienvenu, O.J.; Colantuoni, E.; Wozniak, A.W.; Rice, T.W.; Hopkins, R.O. One year outcomes in patients with acute lung injury randomised to initial trophic or full enteral feeding: Prospective follow-up of EDEN randomised trial. BMJ 2013, 346, f1532. [Google Scholar] [CrossRef]
- Ridley, E.J.; Davies, A.R.; Parke, R.; Bailey, M.; McArthur, C.; Gillanders, L.; Cooper, D.J.; McGuinness, S. Supplemental parenteral nutrition versus usual care in critically ill adults: A pilot randomized controlled study. Crit. Care 2018, 22, 12. [Google Scholar] [CrossRef]
- Charles, E.J.; Petroze, R.T.; Metzger, R.; Hranjec, T.; Rosenberger, L.H.; Riccio, L.M.; McLeod, M.D.; Guidry, C.A.; Stukenborg, G.J.; Swenson, B.R.; et al. Hypocaloric compared with eucaloric nutritional support and its effect on infection rates in a surgical intensive care unit: A randomized controlled trial. Am. J. Clin. Nutr. 2014, 100, 1337–1343. [Google Scholar] [CrossRef]
- Rugeles, S.; Villarraga-Angulo, L.G.; Ariza-Gutiérrez, A.; Chaverra-Kornerup, S.; Lasalvia, P.; Rosselli, D. High-protein hypocaloric vs normocaloric enteral nutrition in critically ill patients: A randomized clinical trial. J. Crit. Care 2016, 35, 110–114. [Google Scholar] [CrossRef]
- Rice, T.W.; Mogan, S.; Hays, M.A.; Bernard, G.R.; Jensen, G.L.; Wheeler, A.P. Randomized trial of initial trophic versus full-energy enteral nutrition in mechanically ventilated patients with acute respiratory failure. Crit. Care Med. 2011, 39, 967–974. [Google Scholar] [CrossRef]
- Braunschweig, C.A.; Sheean, P.M.; Peterson, S.J.; Gomez Perez, S.; Freels, S.; Lateef, O.; Gurka, D.; Fantuzzi, G. Intensive nutrition in acute lung injury: A clinical trial (INTACT). JPEN J. Parenter. Enter. Nutr. 2015, 39, 13–20. [Google Scholar] [CrossRef]
- Petros, S.; Horbach, M.; Seidel, F.; Weidhase, L. Hypocaloric vs normocaloric nutrition in critically ill patients: A prospective randomized pilot trial. JPEN J. Parenter. Enter. Nutr. 2016, 40, 242–249. [Google Scholar] [CrossRef]
- Needham, D.M.; Dinglas, V.D.; Morris, P.E.; Jackson, J.C.; Hough, C.L.; Mendez-Tellez, P.A.; Wozniak, A.W.; Colantuoni, E.; Ely, E.W.; Rice, T.W.; et al. Physical and cognitive performance of patients with acute lung injury 1 year after initial trophic versus full enteral feeding. EDEN trial follow-up. Am. J. Respir. Crit. Care Med. 2013, 188, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Arabi, Y.M.; Tamim, H.M.; Dhar, G.S.; Al-Dawood, A.; Al-Sultan, M.; Sakkijha, M.H.; Kahoul, S.H.; Brits, R. Permissive underfeeding and intensive insulin therapy in critically ill patients: A randomized controlled trial. Am. J. Clin. Nutr. 2011, 93, 569–577. [Google Scholar] [CrossRef]
- Wang, C.Y.; Fu, P.K.; Chao, W.C.; Wang, W.N.; Chen, C.H.; Huang, Y.C. Full versus trophic feeds in critically ill adults with high and low nutritional risk scores: A randomized controlled trial. Nutrients 2020, 12, 3518. [Google Scholar] [CrossRef]
- McKeever, L.; Peterson, S.J.; Cienfuegos, S.; Rizzie, J.; Lateef, O.; Freels, S.; Braunschweig, C.A. Real-Time energy exposure Is associated with increased oxidative stress among feeding-tolerant critically ill patients: Results from the FEDOX trial. JPEN J. Parenter. Enter. Nutr. 2020, 44, 1484–1491. [Google Scholar] [CrossRef] [PubMed]
- Arabi, Y.M.; Aldawood, A.S.; Haddad, S.H.; Al-Dorzi, H.M.; Tamim, H.M.; Jones, G.; Mehta, S.; McIntyre, L.; Solaiman, O.; Sakkijha, M.H.; et al. Permissive underfeeding or standard enteral feeding in critically ill adults. N. Engl. J. Med. 2015, 372, 2398–2408. [Google Scholar] [CrossRef] [PubMed]
- Rugeles, S.J.; Rueda, J.D.; Díaz, C.E.; Rosselli, D. Hyperproteic hypocaloric enteral nutrition in the critically ill patient: A randomized controlled clinical trial. Indian J. Crit. Care Med. 2013, 17, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Mousavian, S.Z.; Pasdar, Y.; Ranjbar, G.; Jandari, S.; Akhlaghi, S.; Almasi, A.; Safarian, M. Randomized controlled trial of comparative hypocaloric vs full-energy enteral feeding during the first week of hospitalization in neurosurgical patients at the Intensive Care Unit. JPEN J. Parenter. Enter. Nutr. 2020, 44, 1475–1483. [Google Scholar] [CrossRef]
- Allingstrup, M.J.; Kondrup, J.; Wiis, J.; Claudius, C.; Pedersen, U.G.; Hein-Rasmussen, R.; Bjerregaard, M.R.; Steensen, M.; Jensen, T.H.; Lange, T.; et al. Early goal-directed nutrition versus standard of care in adult intensive care patients: The single-centre, randomised, outcome assessor-blinded EAT-ICU trial. Intensive Care Med. 2017, 43, 1637–1647. [Google Scholar] [CrossRef]
- Bastarache, J.A.; Ware, L.B.; Girard, T.D.; Wheeler, A.P.; Rice, T.W. Markers of inflammation and coagulation may be modulated by enteral feeding strategy. JPEN J. Parenter. Enter. Nutr. 2012, 36, 732–740. [Google Scholar] [CrossRef]
- McKeever, L.; Peterson, S.J.; Lateef, O.; Freels, S.; Fonseca, T.L.; Bocco, B.; Fernandes, G.W.; Roehl, K.; Nowak, K.; Mozer, M.; et al. Higher caloric exposure in critically ill patients transiently accelerates thyroid hormone activation. J. Clin. Endocrinol. Metab. 2020, 105, 523–533. [Google Scholar] [CrossRef]
- Rice, T.W.; Wheeler, A.P.; Thompson, B.T.; Steingrub, J.; Hite, R.D.; Moss, M.; Morris, A.; Dong, N.; Rock, P. Initial trophic vs full enteral feeding in patients with acute lung injury: The EDEN randomized trial. JAMA 2012, 307, 795–803. [Google Scholar] [CrossRef] [PubMed]
- van Zanten, A.R.H.; Petit, L.; De Waele, J.; Kieft, H.; de Wilde, J.; van Horssen, P.; Klebach, M.; Hofman, Z. Very high intact-protein formula successfully provides protein intake according to nutritional recommendations in overweight critically ill patients: A double-blind randomized trial. Crit. Care 2018, 22, 156. [Google Scholar] [CrossRef] [PubMed]
- Ferrie, S.; Allman-Farinelli, M.; Daley, M.; Smith, K. Protein requirements in the critically ill: A randomized controlled trial using parenteral nutrition. JPEN J. Parenter. Enter. Nutr. 2016, 40, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.M.; Pantet, O.; Jacquelin-Ravel, N.; Charrière, M.; Schmidt, S.; Becce, F.; Audran, R.; Spertini, F.; Tappy, L.; Pichard, C. Supplemental parenteral nutrition improves immunity with unchanged carbohydrate and protein metabolism in critically ill patients: The SPN2 randomized tracer study. Clin. Nutr. 2019, 38, 2408–2416. [Google Scholar] [CrossRef] [PubMed]
- Jakob, S.M.; Bütikofer, L.; Berger, D.; Coslovsky, M.; Takala, J. A randomized controlled pilot study to evaluate the effect of an enteral formulation designed to improve gastrointestinal tolerance in the critically ill patient-the SPIRIT trial. Crit. Care 2017, 21, 140. [Google Scholar] [CrossRef]
- Beale, R.J.; Sherry, T.; Lei, K.; Campbell-Stephen, L.; McCook, J.; Smith, J.; Venetz, W.; Alteheld, B.; Stehle, P.; Schneider, H. Early enteral supplementation with key pharmaconutrients improves Sequential Organ Failure Assessment score in critically ill patients with sepsis: Outcome of a randomized, controlled, double-blind trial. Crit. Care Med. 2008, 36, 131–144. [Google Scholar] [CrossRef]
- Fetterplace, K.; Deane, A.M.; Tierney, A.; Beach, L.J.; Knight, L.D.; Presneill, J.; Rechnitzer, T.; Forsyth, A.; Gill, B.M.T.; Mourtzakis, M.; et al. Targeted Full Energy and Protein Delivery in Critically Ill Patients: A Pilot Randomized Controlled Trial (FEED Trial). JPEN J. Parenter. Enter. Nutr. 2018, 42, 1252–1262. [Google Scholar] [CrossRef]
- Tuncay, P.; Arpaci, F.; Doganay, M.; Erdem, D.; Sahna, A.; Ergun, H.; Atabey, D. Use of standard enteral formula versus enteric formula with prebiotic content in nutrition therapy: A randomized controlled study among neuro-critical care patients. Clin. Nutr. ESPEN 2018, 25, 26–36. [Google Scholar] [CrossRef]
- Reilly, J.; Mehta, R.; Teperman, L.; Cemaj, S.; Tzakis, A.; Yanaga, K.; Ritter, P.; Rezak, A.; Makowka, L. Nutritional support after liver transplantation: A randomized prospective study. JPEN J. Parenter. Enter. Nutr. 1990, 14, 386–391. [Google Scholar] [CrossRef]
- Wischmeyer, P.E.; Hasselmann, M.; Kummerlen, C.; Kozar, R.; Kutsogiannis, D.J.; Karvellas, C.J.; Besecker, B.; Evans, D.K.; Preiser, J.C.; Gramlich, L.; et al. A randomized trial of supplemental parenteral nutrition in underweight and overweight critically ill patients: The TOP-UP pilot trial. Crit. Care 2017, 21, 142. [Google Scholar] [CrossRef]
- Nakamura, K.; Nakano, H.; Naraba, H.; Mochizuki, M.; Takahashi, Y.; Sonoo, T.; Hashimoto, H.; Morimura, N. High protein versus medium protein delivery under equal total energy delivery in critical care: A randomized controlled trial. Clin. Nutr. 2021, 40, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Doig, G.S.; Simpson, F.; Bellomo, R.; Heighes, P.T.; Sweetman, E.A.; Chesher, D.; Pollock, C.; Davies, A.; Botha, J.; Harrigan, P.; et al. Intravenous amino acid therapy for kidney function in critically ill patients: A randomized controlled trial. Intensive Care Med. 2015, 41, 1197–1208. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Kihata, A.; Naraba, H.; Kanda, N.; Takahashi, Y.; Sonoo, T.; Hashimoto, H.; Morimura, N. β-Hydroxy-β-methylbutyrate, arginine, and glutamine complex on muscle volume loss in critically ill patients: A randomized control trial. JPEN J. Parenter. Enter. Nutr. 2020, 44, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Zhu, R.; Allingstrup, M.J.; Perner, A.; Doig, G.S. The effect of iv amino acid supplementation on mortality in ICU patients may be dependent on kidney function: Post hoc subgroup analyses of a multicenter randomized trial. Crit. Care Med. 2018, 46, 1293–1301. [Google Scholar] [CrossRef]
- Lee, Z.-Y.; Yap, C.S.L.; Hasan, M.S.; Engkasan, J.P.; Barakatun-Nisak, M.Y.; Day, A.G.; Patel, J.J.; Heyland, D.K. The effect of higher versus lower protein delivery in critically ill patients: A systematic review and meta-analysis of randomized controlled trials. Crit. Care 2021, 25, 260. [Google Scholar] [CrossRef]
- Casaer, M.P.; Wilmer, A.; Hermans, G.; Wouters, P.J.; Mesotten, D.; Van den Berghe, G. Role of disease and macronutrient dose in the randomized controlled EPaNIC trial: A post hoc analysis. Am. J. Respir. Crit. Care Med. 2013, 187, 247–255. [Google Scholar] [CrossRef]
- Kokura, Y.; Momosaki, R. Prevalence of malnutrition assessed by the GLIM criteria and association with activities of daily living in older residents in an integrated facility for medical and long-term care. Nutrients 2022, 14, 3656. [Google Scholar] [CrossRef]
- Nishioka, S.; Takayama, M.; Watanabe, M.; Urusihara, M.; Kiriya, Y.; Hijioka, S. Prevalence of malnutrition in convalescent rehabilitation wards in Japan and correlation of malnutrition with ADL and discharge outcome in elderly stroke patients. J. Jpn. Soc. Parenter. Enter. Nutr. 2015, 30, 1145–1151. [Google Scholar] [CrossRef]
- Mart, M.F.; Girard, T.D.; Thompson, J.L.; Whitten-Vile, H.; Raman, R.; Pandharipande, P.P.; Heyland, D.K.; Ely, E.W.; Brummel, N.E. Nutritional risk at intensive care unit admission and outcomes in survivors of critical illness. Clin. Nutr. 2021, 40, 3868–3874. [Google Scholar] [CrossRef]
- Schweickert, W.D.; Pohlman, M.C.; Pohlman, A.S.; Nigos, C.; Pawlik, A.J.; Esbrook, C.L.; Spears, L.; Miller, M.; Franczyk, M.; Deprizio, D.; et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet 2009, 373, 1874–1882. [Google Scholar] [CrossRef]
- Teixeira, C.; Kern, M.; Rosa, R.G. What outcomes should be evaluated in critically ill patients? Rev. Bras. Ter. Intensiv. 2021, 33, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Arai, Y.; Nakanishi, N.; Ono, Y.; Inoue, S.; Kotani, J.; Harada, M.; Oto, J. Ultrasound assessment of muscle mass has potential to identify patients with low muscularity at intensive care unit admission: A retrospective study. Clin. Nutr. ESPEN 2021, 45, 177–183. [Google Scholar] [CrossRef] [PubMed]

| Source | Population | No. of Patients | Age (Years) | Intervention | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | High | Low | High | Low | Route | Period | High | Low | ||
| Needham 2013 (1) [26] | ALI < 48 h, MV < 72 h, BMI ≥ 25, EN ≤ 48 h > 5 d | 487 | 228 | 259 | 52 ± 15 | 52 ± 16 | EN | Assignment up to 6 d | 80% of the caloric goal | 25% of caloric goal |
| Ridley 2018 [27] | ICU ≤ 48–72 h, MV, Organ system failure ≥ 1 | 99 | 51 | 48 | 59 ± 17 | 60 ± 17 | PN | Assignment up to 7 d | 100% of estimated energy requirement | Usual clinical practice |
| Charles 2014 [28] | Surgical ICU, Expected ICU stay > 48 h | 83 | 42 | 41 | 53.4 ± 2.7 | 50.4 ± 2.8 | EN+PN | During the ICU stay (10–13 d) | 25–30 kcal/kg/day | 50% of 25–30 kcal/kg/day |
| Rugeles 2016 [29] | Expected EN > 96 h | 120 | 60 | 60 | 51.8 ± 20.3 | 53.8 ± 19.0 | EN | Assignment up to 7 d | 25 kcal/kg/day | 15 kcal/kg/day |
| Rice 2011 [30] | MV ≥ 72 h | 200 | 102 | 98 | 54 ± 17 | 53 ± 19 | EN | Initial 6 d of MV | 25–30 kcal/kg/day (1418 ± 686 kcal/day in results) | 10 mL/h (300 ± 149 kcal/day in results) |
| Braunschweig 2015 [31] | Mixed ICU, ALI | 78 | 40 | 38 | 52.5 ± 17.1 | 58.6 ± 16.2 | EN | Within 24 h of ALI diagnosis to hospital discharge | Indirect calorimetry or 30 kcal/kg | Usual clinical practice |
| Petros 2016 [32] | Nutritional support ≥ 3 d | 100 | 54 | 46 | 64.3 ± 11.5 | 67.6 ± 11.5 | EN+PN | Within 24 h of ICU admission up to 7 d | 100% of daily energy expenditure (19.7 ± 5.7 kcal/kg/day in results) | 50% of daily energy expenditure (11.3 ± 3.1 kcal/kg/day in results) |
| Needham 2013 (2) [33] | ALI < 48 h, MV < 72 h | 149 | 74 | 75 | 47 ± 14 | 48 ± 14 | EN | Assignment until discharge from the ICU | 1300 kcal/day | 400 kcal/day |
| Arabi 2011 [34] | Mixed ICU, Expected ICU stay > 48 h, Glucose > 110 mg/dL | 240 | 120 | 120 | 51.9 ± 22.1 | 50.3 ± 21.3 | EN | Within 48 h of ICU admission until discharge from the ICU | 90–100% of the Harris-Benedict equation | 60–70% of the Harris-Benedict equation |
| Wang 2020 [35] | Medical ICU, MV, Expected ICU stay > 72 h | 150 | 74 | 76 | 57.1–72.3 | 58.8 ± 70.2 | EN+PN | Assignment up to 6 d | 25 kcal/kg/day | 600 kcal/day |
| Arabi 2015 [37] | EN < 48 h after ICU admission, Expected ICU stay > 72 h | 894 | 446 | 448 | 50.9 ± 19.4 | 50.2 ± 19.5 | EN | Assignment up to 14 d | 70–100% of calculated caloric requirements | 40–60% of calculated caloric requirements |
| Mousavian 2020 [39] | Expected ICU stay > 96 h, GCS ≥ 4, ≤10, BMI > 18.5 kg/m2 | 58 | 29 | 29 | 40 ± 16 | 42 ± 14 | EN | Assignment up to 14 d | 75% of estimated energy requirement | 30% of estimated energy requirement |
| Allingstrup 2017 [40] | ICU ≤ 24 h, Expected ICU stay > 3 d, BMI > 17 kg/m2 | 199 | 100 | 99 | 63 (51–72) | 68 (52–75) | EN+PN | Within 24 h of ICU admission to the ICU discharge | 100% of caloric requirements | 25 kcal/kg/day |
| McKeever 2020 [42] | Mixed ICU, Expected MV > 72 h, SIRS | 35 | 19 | 16 | 55.6 ± 15.1 | 57.0 ± 16.6 | EN+PN | Assignment up to 7 d | 100% of estimated energy requirement (25–30 kcal/kg/day) | 40% of estimated energy requirement (10–12 kcal/kg/day) |
| Rice 2012 [43] | ALI < 48 h, MV ≥ 72 h | 1000 | 492 | 508 | 52 ± 16 | 52 ± 17 | EN | Initial 6 d of MV | 25–30 kcal/kg/day (1300 kcal/day in results) | 10–20 kcal/h (400 kcal/day in results) |
| Source | Population | No. of Patients | Age (Years) | Intervention | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | High | Low | High | Low | Route | Period | High | Low | ||
| van Zanten 2018 [44] | Mixed ICU, MV, BMI ≥ 25, EN ≤ 48 h > 5 d | 44 | 22 | 22 | 63.9 ± 13.3 | 60.8 ± 15.2 | EN | From day 1–2 of ICU admission to ICU discharge (up to 28 d) | 1.49 g/kg at day 5 in results | 0.76 g/kg on day 5 in results |
| Ferrie 2016 [45] | Mixed ICU, MV within 48 h ≥ 72 h | 119 | 59 | 60 | 67.0 (55.5–74.3) | 64.5 (49.3–70.0) | PN | From day 1–2 of ICU admission to 10 d | 1.2 g/kg (1.1 g/kg in results) | 0.8 g/kg (0.9 g/kg in results) |
| Ridley 2018 [27] | Mixed ICU, MV, BMI ≥ 25, EN ≤ 48 h > 5 d | 99 | 51 | 48 | 59 ± 17 | 60 ± 17 | PN | From day 2–3 of ICU admission to 7 d | Supplemental PN | Usual clinical practice |
| Berger 2019 [46] | MV, Expected ICU stay ≥ 5 d more | 23 | 11 | 12 | 63.0 (55.0–73.0) | 67.5 (62.3–75.0) | EN+PN | From day 3 of ICU admission | Indirect calorimetry 100% target (1.11 g/kg in results) | Usual clinical practice (0.69 g/kg in results) |
| Jakob 2017 [47] | Mixed ICU, expected ICU stay ≥ 7 d | 90 | 46 | 44 | 65.3 (52.6–75.3) | 61.6 (48.6–71.3) | EN | From day 1–3 of ICU admission to 10 d | Caloric target of 25 kcal/kg/day on the third day after enteral nutrition (1.13 g/kg/day) | Caloric target of 25 kcal/kg/day on the third day after enteral nutrition (0.80 g/kg/day) |
| Beale 2008 [48] | Infection, APACHE II > 10, Expected ICU stay > 5 d, EN > 5 d | 55 | 27 | 28 | 57.4 ± 19.0 | 64.3 ± 16.8 | EN | Within 24 h after the enrollment to 10 d | 1.4 g/kg/day | 0.5 g/kg/day |
| Fetterplace 2018 [49] | Mixed ICU, MV within 48 h, expected > 72 h | 60 | 30 | 30 | 55 ± 13 | 57 ± 16 | EN | From day 1–2 of ICU admission to ICU discharge (up to15 d) | 1.2 g/kg/day over the study period | 0.75 g/kg/day over the study period |
| Tuncay 2018 [50] | Neurocritical ICU | 46 | 23 | 23 | 73.9 ± 15.3 | 71.8 ± 20.0 | EN | During ICU stay | 1.02 g/kg/day at 21 d in results | 0.85 g/kg/day at 21 d in results |
| Reilly 1990 [51] | Patients to undergo liver transplantation | 20 | 10 | 10 | 44–50 | 51 ± 9 | PN | Immediately after liver transplantation to 7 d | 1.5 g/kg/day | No nutritional support |
| Wischmeyer 2017 [52] | Mixed ICU, MV, Acute respiratory failure, EN ≤ 48 h, BMI < 25 kg/m2, >35 kg/m2 | 125 | 52 | 73 | 55.8 ± 19.8 | 55.1 ± 16.2 | PN | From day 1–2 of ICU admission to 7 d | PN solution (100% calorie goal) (106 g in results) | A standard polymeric solution (100 g in results) |
| Nakamura 2021 [53] | Mixed ICU, No lower limb injury, No expected death or discharge from the ICU | 117 | 60 | 57 | 68.3 ± 14.3 | 67.9 ± 14.9 | EN | From day 1–2 of ICU admission to 10 d | 1.8 g/kg/day | 0.9 g/kg/day |
| Doig 2015 [54] | Mixed ICU, Expected ICU stay ≥ 2 d | 474 | 239 | 235 | 63.3 ± 15.4 | 62.7 ± 16.6 | PN | From day 1–2 of ICU admission to ICU discharge | 100 g of amino acids or maximum 2.0 g/kg/day | Usual clinical practice |
| Nakamura 2019 [55] | Mixed ICU, No lower limb event, Early expected discharge from the ICU | 50 | 26 | 24 | 71.8 ± 12.4 | 76.6 ± 12.3 | EN | From day 1–2 of ICU admission to 10 d | HMB (1.06 g/kg/day at day 7 in results) | Usual clinical practice (0.87 g/kg/day on day 7 in results) |
| Zhu 2018 [56] | Mixed ICU, Expected ICU stay ≥ 2 d | 368 | 179 | 189 | 62.4 ± 15.8 | 62.3 ± 17.1 | PN | From day 1–2 of ICU admission to ICU discharge | 2.0 g/kg/day | Usual clinical practice |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakanishi, N.; Matsushima, S.; Tatsuno, J.; Liu, K.; Tamura, T.; Yonekura, H.; Yamamoto, N.; Unoki, T.; Kondo, Y.; Nakamura, K. Impact of Energy and Protein Delivery to Critically Ill Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2022, 14, 4849. https://doi.org/10.3390/nu14224849
Nakanishi N, Matsushima S, Tatsuno J, Liu K, Tamura T, Yonekura H, Yamamoto N, Unoki T, Kondo Y, Nakamura K. Impact of Energy and Protein Delivery to Critically Ill Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2022; 14(22):4849. https://doi.org/10.3390/nu14224849
Chicago/Turabian StyleNakanishi, Nobuto, Shinya Matsushima, Junko Tatsuno, Keibun Liu, Takahiko Tamura, Hiroshi Yonekura, Norimasa Yamamoto, Takeshi Unoki, Yutaka Kondo, and Kensuke Nakamura. 2022. "Impact of Energy and Protein Delivery to Critically Ill Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Nutrients 14, no. 22: 4849. https://doi.org/10.3390/nu14224849
APA StyleNakanishi, N., Matsushima, S., Tatsuno, J., Liu, K., Tamura, T., Yonekura, H., Yamamoto, N., Unoki, T., Kondo, Y., & Nakamura, K. (2022). Impact of Energy and Protein Delivery to Critically Ill Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients, 14(22), 4849. https://doi.org/10.3390/nu14224849







