A Rapid Review of the Impact of Family-Based Digital Interventions for Obesity Prevention and Treatment on Obesity-Related Outcomes in Primary School-Aged Children
Highlights
- This review found digital approaches for childhood obesity prevention and treatment to be acceptable and highly engaging to families, with emerging evidence showing that the use of social media and gamification can enhance program delivery.
- Family-based digital interventions demonstrated modest improvements in child body mass index (BMI) scores and health behaviors. This review also reported on the delivery mediums (i.e., telehealth, apps, wearables) of digital interventions and process indicators (i.e., utilization and engagement rates) where available, in addition to health-related outcomes.
- Evidence around screen time and sleep remains scarce. More research is warranted to better understand how virtual delivery may impact screen time and sedentary behavior, the optimal dose and engagement for changing health-related behavior, and whether educational screen time and discretionary screen time contribute to health and behavior outcomes differently.
- Digital interventions for childhood obesity were accessible in online marketplaces to the wider public in Australia; however, the evidence base to support the quality and credibility of these readily accessible programs was unclear. There is a research–practice gap that limits the availability of evidence-based childhood obesity prevention and treatment programs in the public domain, and more support is needed to enhance the translation of effective interventions into health benefits for this population.
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.2.1. Study Design
2.2.2. Participants
2.2.3. Interventions
2.2.4. Outcomes
2.2.5. Settings
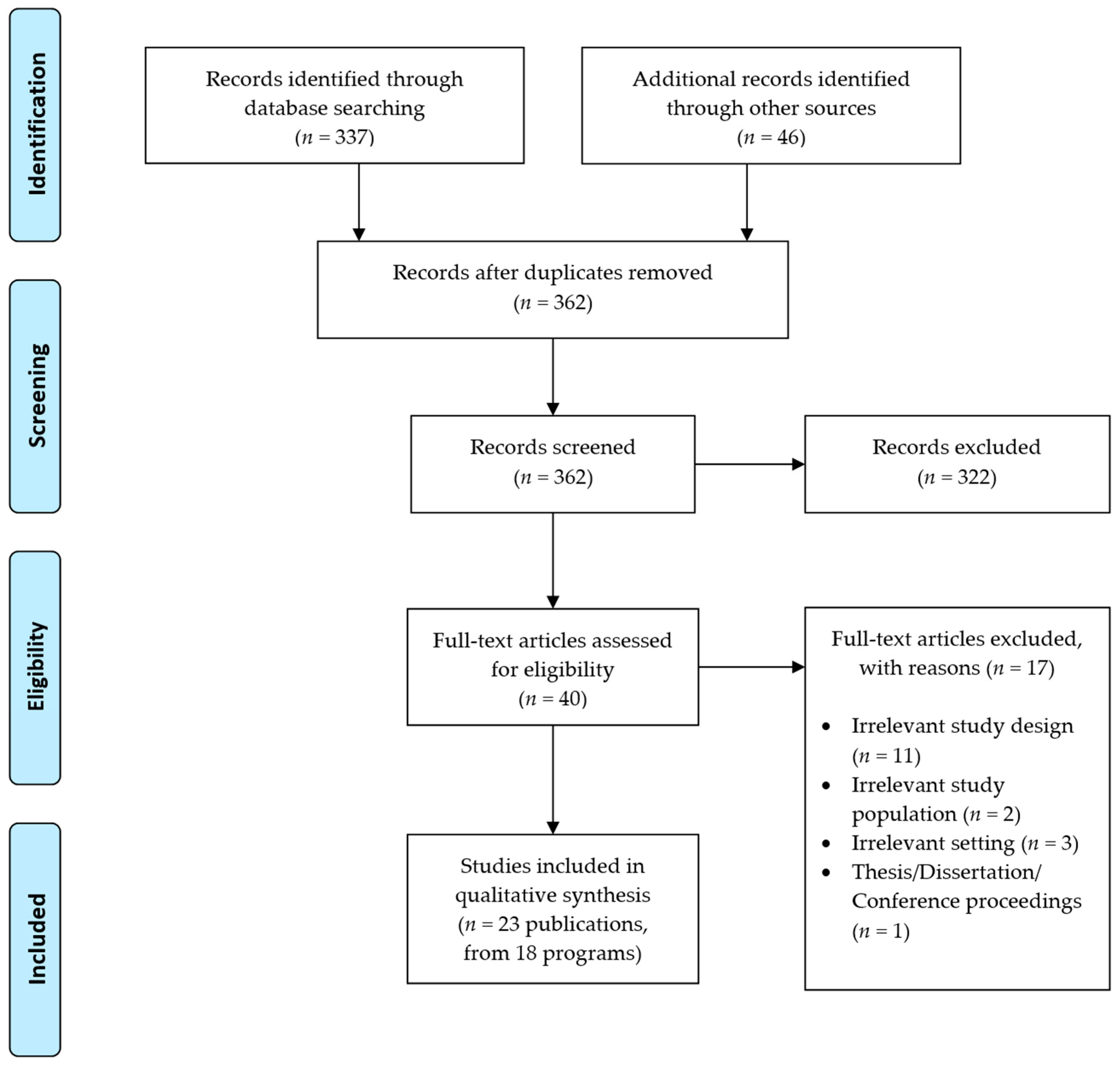
2.3. Study Selection
2.4. Data Extraction
2.5. Quality Appraisal
2.6. Data Synthesis
3. Results
3.1. Study Selection
3.2. Quality Appraisal
3.3. Study Characteristics
3.4. Theoretical Framework
3.5. Intervention Components and Usage
3.6. Intervention Effects
3.6.1. Anthropometry
3.6.2. Dietary Intakes
3.6.3. Physical Activity
3.6.4. Screen Time/Sedentary Behavior
3.6.5. Sleep
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Popkin, B.M.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, e13128. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.J.; Kompaniyets, L.; Freedman, D.S.; Kraus, E.M.; Porter, R.; Blanck, H.M.; Goodman, A.B. Longitudinal Trends in Body Mass Index Before and During the COVID-19 Pandemic Among Persons Aged 2–19 Years—United States, 2018–2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1278–1283. [Google Scholar] [CrossRef] [PubMed]
- Antwi, F.A.; Fazylova, N.; Garcon, M.-C.; Lopez, L.; Rubiano, R.; Slyer, J.T. Effectiveness of web-based programs on the reduction of childhood obesity in school-aged children: A systematic review. JBI Evid. Synth. 2013, 11, 1–44. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guideline Recommendations on Digital Interventions for Health System Strengthening; World Health Organization: Geneva, Switzerland, 2019. Available online: https://www.ncbi.nlm.nih.gov/books/NBK541905/ (accessed on 1 November 2022).
- Tozzi, F.; Nicolaidou, I.; Galani, A.; Antoniades, A. E-health interventions for anxiety management targeting young children and adolescents: An exploratory review. JMIR Pediatr. Parent. 2018, 1, e7248. [Google Scholar] [CrossRef] [PubMed]
- Armoiry, X.; Sturt, J.; Phelps, E.E.; Walker, C.L.; Court, R.; Taggart, F.; Sutcliffe, P.; Griffiths, F.; Atherton, H. Digital Clinical Communication for Families and Caregivers of Children or Young People With Short- or Long-Term Conditions: Rapid Review. J. Med. Internet Res. 2018, 20, e7999. [Google Scholar] [CrossRef]
- Baumüller, H. The Little We Know: An Exploratory Literature Review on the Utility of Mobile Phone-Enabled Services for Smallholder Farmers. J. Int. Dev. 2018, 30, 134–154. [Google Scholar] [CrossRef]
- Tsertsvadze, A.; Chen, Y.F.; Moher, D.; Sutcliffe, P.; McCarthy, N. How to conduct systematic reviews more expeditiously? Syst. Rev. 2015, 4, 160. [Google Scholar] [CrossRef]
- Tricco, A.C.; Antony, J.; Zarin, W.; Strifler, L.; Ghassemi, M.; Ivory, J.; Perrier, L.; Hutton, B.; Moher, D.; Straus, S.E. A scoping review of rapid review methods. BMC Med. 2015, 13, 224. [Google Scholar] [CrossRef]
- Chai, L.K.; Collins, C.; May, C.; Brain, K.; Wong See, D.; Burrows, T. Effectiveness of family-based weight management interventions for children with overweight and obesity: An umbrella review. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 1341–1427. [Google Scholar] [CrossRef]
- Yoong, S.L.; Chai, L.K.; Williams, C.M.; Wiggers, J.; Finch, M.; Wolfenden, L. Systematic review and meta-analysis of interventions targeting sleep and their impact on child body mass index, diet, and physical activity. Obesity 2016, 24, 1140–1147. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022). Available online: www.training.cochrane.org/handbook (accessed on 3 May 2022).
- Tricco, A.; Langlois, E.; Straus, S. (Eds.) Rapid Reviews to Strengthen Health Policy and Systems: A Practical Guide; World Health Organization: Geneva, Switzerland, 2017; Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- Tufanaru, C.M.Z.; Aromataris, E.; Campbell, J.; Hopp, L. Chapter 3: Systematic reviews of effectiveness. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E.M.Z.E., Ed.; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Cueto, V.; Wang, C.J.; Sanders, L.M. Impact of a Mobile App–Based Health Coaching and Behavior Change Program on Participant Engagement and Weight Status of Overweight and Obese Children: Retrospective Cohort Study. JMIR Mhealth Uhealth 2019, 7, e14458. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Shariff, Z.M.; Mukhtar, F.; Lye, M.S. Family-based intervention using face-to-face sessions and social media to improve Malay primary school children’s adiposity: A randomized controlled field trial of the Malaysian REDUCE programme. Nutr. J. 2018, 17, 74. [Google Scholar] [CrossRef] [PubMed]
- Bakırcı-Taylor, A.L.; Reed, D.B.; McCool, B.; Dawson, J.A. mHealth Improved Fruit and Vegetable Accessibility and Intake in Young Children. J. Nutr. Educ. Behav. 2019, 51, 556–566. [Google Scholar] [CrossRef]
- Baranowski, T.; Baranowski, J.C.; Cullen, K.W.; Thompson, D.I.; Nicklas, T.; Zakeri, I.E.; Rochon, J. The Fun, Food, and Fitness Project (FFFP): The Baylor GEMS pilot study. Ethn. Dis. 2003, 13, S30–S39. [Google Scholar]
- Chai, L.K.; Collins, C.E.; May, C.; Ashman, A.; Holder, C.; Brown, L.J.; Burrows, T.L. Feasibility and efficacy of a web-based family telehealth nutrition intervention to improve child weight status and dietary intake: A pilot randomised controlled trial. J. Telemed. Telecare 2021, 27, 146–158. [Google Scholar] [CrossRef]
- Cullen, K.W.; Thompson, D.; Chen, T.-A. Outcome Evaluation of Family Eats: An Eight-Session Web-Based Program Promoting Healthy Home Food Environments and Dietary Behaviors for African American Families. Health Educ. Behav. 2017, 44, 32–40. [Google Scholar] [CrossRef]
- De Lepeleere, S.; De Bourdeaudhuij, I.; Cardon, G.; Verloigne, M. The effect of an online video intervention ‘Movie Models’ on specific parenting practices and parental self-efficacy related to children’s physical activity, screen-time and healthy diet: A quasi experimental study. BMC Public Health 2017, 17, 366. [Google Scholar] [CrossRef]
- Jake-Schoffman, D.E.; Turner-McGrievy, G.; Wilcox, S.; Moore, J.B.; Hussey, J.; Kaczynski, A. The mFIT (Motivating Families with Interactive Technology) Study: A Randomized Pilot to Promote Physical Activity and Healthy Eating Through Mobile Technology. J. Technol. Behav. Sci. 2018, 3, 179–189. [Google Scholar] [CrossRef]
- Johansson, L.; Hagman, E.; Danielsson, P. A novel interactive mobile health support system for pediatric obesity treatment: A randomized controlled feasibility trial. BMC Pediatr. 2020, 20, 447. [Google Scholar] [CrossRef]
- Knowlden, A.P.; Sharma, M.; Cottrell, R.R.; Wilson, B.R.; Johnson, M.L. Impact evaluation of Enabling Mothers to Prevent Pediatric Obesity through Web-Based Education and Reciprocal Determinism (EMPOWER) Randomized Control Trial. Health Educ. Behav. 2015, 42, 171–184. [Google Scholar] [CrossRef] [PubMed]
- Maddison, R.; Marsh, S.; Foley, L.; Epstein, L.H.; Olds, T.; Dewes, O.; Heke, I.; Carter, K.; Jiang, Y.; Mhurchu, C.N. Screen-Time Weight-loss Intervention Targeting Children at Home (SWITCH): A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 111. [Google Scholar] [CrossRef] [PubMed]
- Morgan, P.J.; Young, M.D.; Barnes, A.T.; Eather, N.; Pollock, E.R.; Lubans, D.R. Engaging Fathers to Increase Physical Activity in Girls: The “Dads And Daughters Exercising and Empowered” (DADEE) Randomized Controlled Trial. Ann. Behav. Med. 2019, 53, 39–52. [Google Scholar] [CrossRef] [PubMed]
- Perdew, M.; Liu, S.; Rhodes, R.; Ball, G.D.C.; Mâsse, L.C.; Hartrick, T.; Strange, K.; Naylor, P.J. The Effectiveness of a Blended In-Person and Online Family-Based Childhood Obesity Management Program. Child. Obes. 2021, 17, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Rangelov, N.; Della Bella, S.; Marques-Vidal, P.; Suggs, L.S. Does additional support provided through e-mail or SMS in a Web-based Social Marketing program improve children’s food consumption? A Randomized Controlled Trial. Nutr. J. 2018, 17, 24. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.; Bhatt, R.; Vazquez, I.; Cullen, K.W.; Baranowski, J.; Baranowski, T.; Liu, Y. Creating action plans in a serious video game increases and maintains child fruit-vegetable intake: A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 39. [Google Scholar] [CrossRef]
- Trost, S.G.; Brookes, D.S.K. Effectiveness of a novel digital application to promote fundamental movement skills in 3- to 6-year-old children: A randomized controlled trial. J. Sports Sci. 2021, 39, 453–459. [Google Scholar] [CrossRef]
- Trost, S.G.; Sundal, D.; Foster, G.D.; Lent, M.R.; Vojta, D. Effects of a pediatric weight management program with and without active video games a randomized trial. JAMA Pediatr. 2014, 168, 407–413. [Google Scholar] [CrossRef]
- Wald, E.R.; Ewing, L.J.; Moyer, S.C.L.; Eickhoff, J.C. An Interactive Web-Based Intervention to Achieve Healthy Weight in Young Children. Clin. Pediatr. 2018, 57, 547–557. [Google Scholar] [CrossRef]
- Williamson, D.A.; Martin, P.D.; White, M.A.; Newton, R.; Walden, H.; York-Crowe, E.; Alfonso, A.; Gordon, S.; Ryan, D. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eat. Weight. Disord. 2005, 10, 193–203. [Google Scholar] [CrossRef]
- Yau, K.W.; Tang, T.S.; Görges, M.; Pinkney, S.; Kim, A.D.; Kalia, A.; Amed, S. Effectiveness of Mobile Apps in Promoting Healthy Behavior Changes and Preventing Obesity in Children: Systematic Review. JMIR Pediatr. Parent 2022, 5, e34967. [Google Scholar] [CrossRef] [PubMed]
- Kracht, C.L.; Hutchesson, M.; Ahmed, M.; Müller, A.M.; Ashton, L.M.; Brown, H.M.; DeSmet, A.; Maher, C.A.; Mauch, C.E.; Vandelanotte, C.; et al. E-&mHealth interventions targeting nutrition, physical activity, sedentary behavior, and/or obesity among children: A scoping review of systematic reviews and meta-analyses. Obes. Rev. 2021, 22, e13331. [Google Scholar] [CrossRef]
- Oudeyer, P.-Y.; Kaplan, F. What is intrinsic motivation? A typology of computational approaches. Front. Neurorobot. 2009, 1, 6. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.; Deterding, S.; Kuhn, K.-A.; Staneva, A.; Stoyanov, S.; Hides, L. Gamification for health and wellbeing: A systematic review of the literature. Internet Interv. 2016, 6, 89–106. [Google Scholar] [CrossRef]
- Suleiman-Martos, N.; García-Lara, R.A.; Martos-Cabrera, M.B.; Albendín-García, L.; Romero-Béjar, J.L.; Cañadas-De la Fuente, G.A.; Gómez-Urquiza, J.L. Gamification for the Improvement of Diet, Nutritional Habits, and Body Composition in Children and Adolescents: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 2478. [Google Scholar] [CrossRef] [PubMed]
- Petkovic, J.; Duench, S.; Trawin, J.; Dewidar, O.; Pardo Pardo, J.; Simeon, R.; DesMeules, M.; Gagnon, D.; Hatcher Roberts, J.; Hossain, A.; et al. Behavioural interventions delivered through interactive social media for health behaviour change, health outcomes, and health equity in the adult population. Cochrane Database Syst. Rev. 2021, 5, Cd012932. [Google Scholar] [CrossRef]
- Maher, C.A.; Lewis, L.K.; Ferrar, K.; Marshall, S.; De Bourdeaudhuij, I.; Vandelanotte, C. Are Health Behavior Change Interventions That Use Online Social Networks Effective? A Systematic Review. J. Med. Internet Res. 2014, 16, e2952. [Google Scholar] [CrossRef]
| Author (Year) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ahmad (2018) [17] | Y | Y | Y | Y | NA | Y | Y | Y | Y | Y | Y | Y | Y |
| Bakirci-Taylor (2019) [18] | Y | Y | Y | N | Y | U | Y | Y | N | Y | Y | Y | Y |
| Baranowski (2003) [19] | Y | Y | N | U | NA | U | N | U | U | Y | Y | Y | Y |
| Chai (2021) [20] | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Cullen (2017) [21] | Y | U | Y | U | NA | U | Y | Y | N | Y | Y | Y | Y |
| De Lepeleere (2017) [22] | N | N | Y | NA | NA | Y | Y | Y | N | Y | Y | Y | N |
| Jake-Schoffman (2018) [23] | U | Y | U | U | U | Y | Y | N | U | Y | Y | Y | Y |
| Johansson (2020) [24] | Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Knowlden (2015) [25] | Y | U | Y | Y | U | Y | Y | Y | N | Y | Y | Y | Y |
| Maddison (2014) [26] | Y | Y | Y | NA | NA | U | Y | U | Y | Y | Y | Y | Y |
| Morgan (2019) [27] | Y | Y | U | NA | NA | N | Y | Y | Y | Y | Y | Y | Y |
| Perdew (2021) [28] | N | N | Y | NA | NA | N | Y | U | Y | Y | Y | Y | N |
| Rangelov (2018) [29] | Y | U | Y | U | Y | U | Y | Y | U | Y | Y | Y | Y |
| Thompson (2015) [30] | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | Y |
| Trost (2021) [31] | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Trost (2014) [32] | Y | U | Y | U | N | N | Y | Y | Y | Y | Y | Y | Y |
| Wald (2018) [33] | U | Y | Y | U | NA | U | U | Y | Y | Y | U | Y | Y |
| Williamson (2005) [34] | U | U | Y | Y | NA | N | Y | Y | Y | Y | Y | Y | Y |
| Author (Year) Country | Prevention/Treatment a | Study Design | Participant Characteristics | Intervention Duration and Intensity | Digital Components | Overall Findings b |
|---|---|---|---|---|---|---|
| Ahmad (2018) Malaysia [17] | Treatment | RCT | 134 parent-child dyads. Children aged 7–10 years. All participants were Malay females. | 4 weeks of weekly training for parents to change child behavior and 3 months of weekly booster which consisted of weekly one-hour sessions using a WhatsApp group. |
| BMI z-scores were significantly reduced in the intervention group compared to the wait-list group for all the children at 6-month post-training. For waist circumference percentile and body fat percentage, the intervention group experienced a significant reduction compared to the wait-list group, within the obese subgroup, and within the overweight subgroup. |
| Bakirci-Taylor (2019) USA [18] | Prevention | RCT | 30 parent-child dyads. Children were aged 3–8 years. All parents were female, married, and predominantly Caucasian. Over 70% had at least a bachelor’s degree and 40% reported incomes of ≥$75,000. | 10 weeks of the mobile Jump2Health intervention which included 3 components: a mobile website (Jump2Health), social media (Facebook page), and short message service or text messages. The Facebook page provided information that was unavailable on the mobile Jump2Health website, but it also Mentioned and reinforced information and text found on the website and promoted linked resources on the website. |
| Skin carotenoids of both children and parents showed significant Week x Treatment interactions in the INT group compared with CON (p < 0.001) indicating increased veg intake. |
| Baranowski (2003) USA [19] | Prevention | RCT | 35 parent-child dyads. Children aged 8 years with a BMI in the 50th percentile for age and gender specific BMI. All participants were female African Americans. Majority had a household income of > $40,000, college graduate, or higher education. | 4-week summer day camp, followed by an 8-week home Internet intervention for the girls and their parents which included weekly behavioral/environmental foci. The treatment camp blended usual camp activities with activities specially designed for GEMS-FFFP. |
| There were no significant changes in BMI, waist circumference, dietary intake, and physical activity level. |
| Chai (2021) Australia [20] | Treatment | RCT | 46 parent-child dyads. Children (mean age 9 years) were predominantly male, overweight/obese and resided with both biological parents. Most parents (mean age 41 years) were female, of middle SES, living in major cities, overweight/obese, and attained certificate/diploma or postgraduate degree. | Both INT 1 and 2 groups received two telehealth consultations delivered by a dietitian, 12 weeks access to a nutrition website and a private Facebook group. INT 2 group received additional text messages. |
| Percentage energy from EDNP food was reduced and percentage energy from nutrient-rich core food was increased in Telehealth+SMS when compared to CON. |
| Cullen (2017) USA [21] | Prevention | RCT | 126 parent-child dyads. Children aged 8–12 years. All participants were African American. Majority of parents were female, aged < 40 years, college graduate or higher education, and have less than two children. | Approximately 8 weeks web-based program for African American families that was designed to promote healthy home food environments, positive parental behaviors related to improving dietary behaviors of family members, and goal setting. |
| Home availability of juice (p < 0.05), vegetables (p < 0.01), and low-fat/fat-free foods (p < 0.05) were significantly higher in INT at 2 months. Parent menu planning skills were significantly higher in INT at 6 months. Both INT and CON groups showed significant increases in home juice/fruit availability, parent modelling, food preparation practices, and menu planning, and a significant decrease in home sugar-sweetened beverage availability (all p < 0.05). |
| De Lepeleere (2017) Belgium [22] | Prevention | Quasi-experimental controlled trial | 135 parents of a primary school-aged child. Majority of parents were female and from a medium-high SES. | 4-week access to website (health promoting videos); content delivered weekly over four weeks; contact time ~2 min per video (22 videos) |
| Most significant intervention effects were found for more complex parenting practices (e.g., an increase in motivating the child to eat fruit). Subgroup analyses showed that the intervention had more effect on the actual parenting practices related to PA, screen-time, and healthy diet in parents of older children (10–12 years old), whereas intervention effects on parental self-efficacy related to those behaviors were stronger in parents of younger children (6–9 years). |
| Jake-Schoffman (2018) USA [23] | Prevention | RCT | 33 parent-child dyads. Majority of parents were female, Caucasian, college graduates, and have obesity. Majority of children were female, Caucasian, aged 11 years, and have a healthy weight. | Dyads were asked to self-monitor using a mobile responsive design website made for the intervention for 12 weeks. |
| There were no significant Group × Time × Parent or Group × Time effects on any of the intervention outcomes: minutes of MVPA (accelerometer), daily steps (pedometer), servings of fruit, vegetables, fast food, and SSBs. |
| Johansson (2020) Sweden [24] | Treatment | RCT | 28 children aged 5–12 years who have obesity according to the International Obesity Task Force (IOTF) with parents who speak Swedish. | 6 months daily self-monitoring of weight recorded via a mobile app used by parents, a website in which clinicians could track treatment progress, prespecified treatment goals for change in degree of obesity shown in the app and on the website, and text message interactions between clinicians and parents. In addition to the mHealth approach, the intervention group received standard care (clinical appointment). |
| At 6 months the intervention group had a greater reduction in standardized BMI than standard care. |
| Knowlden (2015) USA [25] | Prevention | RCT | 57 mothers with children aged 4–6 years. Mothers (mean age of 36 years) were predominantly Caucasian, married, unemployed/homemakers. Children (mean age of 5 years) were primarily Caucasian, male, with a mean age of 5 years. | 4 weekly audiovisual presentations (30 min per session) via website and 1 booster session. |
| The EMPOWER arm of the trial resulted in an overall increase of 1.680 daily cups of fruits and vegetables consumed by children, relative to the comparison group (p < 0.001, 95% confidence interval. Web-based maternal-facilitated interventions can induce sustained effects on child behaviors. |
| Maddison (2014) New Zealand [26] | Treatment | RCT | 251 parent-child dyads. Children (mean age of 11 years) were predominantly male and of Pacific origin | Delivered over 20 weeks, consisting of a face-to-face meeting with the parent/caregiver and the child to deliver intervention content; TV monitoring device; monthly newsletters. |
| There was no significant difference in change of BMI z-scores between the intervention and control groups, although a favorable trend was observed (−0.016; 95% CI: −0.084, 0.051; p = 0.64). There were also no significant differences in secondary outcomes, except for a trend towards increased children’s moderate intensity physical activity in the intervention group (24.3 min/d; 95% CI: −0.94, 49.51; p = 0.06). |
| Morgan (2019) Australia [27] | Prevention | RCT | 153 father-child dyads. Children were aged 4–12 years. Most fathers were employed, born in Australia, and were married or living with a partner (99%). Families were represented from most socio-economic areas. | 90-min group sessions weekly for 8 weeks that included educational and practical components. They were provided with a web-based app at the conclusion of the program for long-term maintenance. |
| ITT analyses revealed favorable group-by-time effects for physical activity in daughters (p = 0.02, d = 0.4) and fathers (p < 0.001, d = 0.7) at 9 months. At postintervention and follow-up, significant effects (p < 0.05) were also identified for daughters’ fundamental movement skills competence (objective: d = 1.1–1.2; perceived: d = 0.4–0.6), a range of fathers’ physical activity parenting practices (d = 0.3–0.8), and screen-time for daughters (d = 0.5–0.8) and fathers (d = 0.4–0.6, postintervention only). Program satisfaction and attendance were very high. |
| Perdew (2021) Canada [28] | Treatment | Quasi-experimental design | 71 parent-child dyads. Children were aged 8–12 years; at or above 85th percentile for BMI for age and sex. | 10 weekly face-to-face 90 min sessions, four community-based activities (i.e., family grocery store tour), and an interactive web-portal. |
| Children’s BMI z-scores were not significantly changed. The intervention group significantly improved their days of moderate-to-vigorous physical activity relative to control; however, child dietary behaviors were not significantly changed. Relative to control, intervention group showed significant improvements in physical activity. |
| Rangelov (2018) Switzerland [29] | Prevention | RCT | 608 parent-child dyads. Children (mean age of 8.5 years) were in the first two years of secondary school and about equal proportion of boys and girls. | 8 weeks access to website (parents) and a personalized and tailored letter by post (children). The emails (INT 1) and mobile text messages (INT 2) were used as weekly reminders to prompt parents to visit the Website. The email also provided a short summary of the weekly theme. |
| Overall, the intervention effects were not significantly different across groups. Children increased their daily consumption of fruit and decreased that of sweets regardless of the group they were assigned. |
| Thompson (2015) USA [30] | Prevention | RCT | 400 parent-child dyads. Children were in 4th or 5th grade (around 9–11 years). Almost evenly distributed by gender (female, 52.7%) and were of diverse ethnicity (White-36.8%, Hispanic 27.4%, African American 26.4%). Parents were mostly female (96.3%), White (40.3%), married (77.5%), and 40–59 years old (55.3%). Highest level of household education was predominately post-graduate study (36.7%), and average household income was >$61,000 (57.6%). | All INT groups played the 10-episode (1 h each) online videogame. The groups varied only in type of implementation intention created after setting a goal to eat FV, including the use of an action plan (specifying actions), or a coping plan (identifying barriers), or both action and coping plans. |
| A significant group-by-time interaction for FV intake (p < 0.001) was found in only the Action group, which had significant increases in FV intake at post 1 (p < 0.0001) and post 2 (p < 0.0001). No other significant interactions were observed. |
| Trost (2021) Australia [31] | Prevention | RCT | 34 parent-child dyads. Children aged 3–6 years and predominantly were Caucasian. Parents were college graduate or higher education. | Families were free to use the app ad libitum but were asked to complete a minimum of three Moovosity™ activities per week, over 8 weeks. Parents were sent mobile text messages and emails every two weeks. |
| There were no significant intervention effects observed for child PA. |
| Trost (2014) USA [32] | Treatment | RCT | 75 parent-child dyads. Children aged 8–12 years, had a BMI greater than the 85th percentile for sex and age and predominantly were female and White. Parents were college graduates or postgraduates. | INT group received hardware consisting of a game console and motion capture device and 1 active game at their second treatment session and a second game in week 9 of the program. |
| Participants in the program and active gaming group exhibited significant increases in MVPA at week 16 (p < 0.05). In the program-only group, a decline or no change was observed in the moderate-to-vigorous and vigorous physical activity. Participants in both groups exhibited significant reductions in percentage overweight and BMI z scores at week 16. However, the program and active gaming group exhibited significantly greater reductions in percentage overweight. |
| Wald (2018) USA [33] | Treatment | RCT | 73 parent-child dyads. Children (mean age 5 years) were predominantly non-Hispanic and overweight/obese. Mothers were predominantly aged < 40 years, college graduate or higher education, and married. | The INT was composed of 6-in-person group sessions and a customized website over 12 months. |
| Among children with 12-month visits, BMI z-scores decreased from baseline to 12 months in both the control and intervention arms; however, the mean reductions were not significantly different between the control and intervention groups (p = 0.7492). The percent of children who reduced their screen time by ≥15% did not differ significantly between the intervention and control groups. |
| Williamson (2005) USA [34] | Treatment | RCT | 57 African American girls aged 11–15 years. | Interactive website and 4 face-to-face sessions of behavior modification over 12 weeks focused on goal setting, behavioral contracting, monitoring of progress, and problem-solving. Participant-initiated weekly emails with counsellor. |
| Participants in the intervention group lost significantly (p < 0.05) more body fat (−1.12 ± 0.47 SE) than the control group 0.43 ± 0.47 SE). There was a significant difference in BMI change between groups (intervention −0.19 ± 0.24 SE, < 0.05, control +0.65 ± 0.23 SE, p < 0.05). Participants in the intervention group significantly reduced fat intake compared with control group (FFQ) (−145.67 ± 37.67 SE, p < 0.05) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chai, L.K.; Farletti, R.; Fathi, L.; Littlewood, R. A Rapid Review of the Impact of Family-Based Digital Interventions for Obesity Prevention and Treatment on Obesity-Related Outcomes in Primary School-Aged Children. Nutrients 2022, 14, 4837. https://doi.org/10.3390/nu14224837
Chai LK, Farletti R, Fathi L, Littlewood R. A Rapid Review of the Impact of Family-Based Digital Interventions for Obesity Prevention and Treatment on Obesity-Related Outcomes in Primary School-Aged Children. Nutrients. 2022; 14(22):4837. https://doi.org/10.3390/nu14224837
Chicago/Turabian StyleChai, Li Kheng, Rebecca Farletti, Leila Fathi, and Robyn Littlewood. 2022. "A Rapid Review of the Impact of Family-Based Digital Interventions for Obesity Prevention and Treatment on Obesity-Related Outcomes in Primary School-Aged Children" Nutrients 14, no. 22: 4837. https://doi.org/10.3390/nu14224837
APA StyleChai, L. K., Farletti, R., Fathi, L., & Littlewood, R. (2022). A Rapid Review of the Impact of Family-Based Digital Interventions for Obesity Prevention and Treatment on Obesity-Related Outcomes in Primary School-Aged Children. Nutrients, 14(22), 4837. https://doi.org/10.3390/nu14224837






