Diet Quality and Contextual Factors Influencing Food Choice among Adolescents with Food Security and Food Insecurity in Baltimore City
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Recruitment and Data Collection
2.4. Measures Used in These Analyses
2.4.1. Dietary Measures
2.4.2. Non-Dietary Measures
2.5. Analysis
2.5.1. Preliminary Analyses
2.5.2. Diet Quality
2.5.3. Eating Behaviors
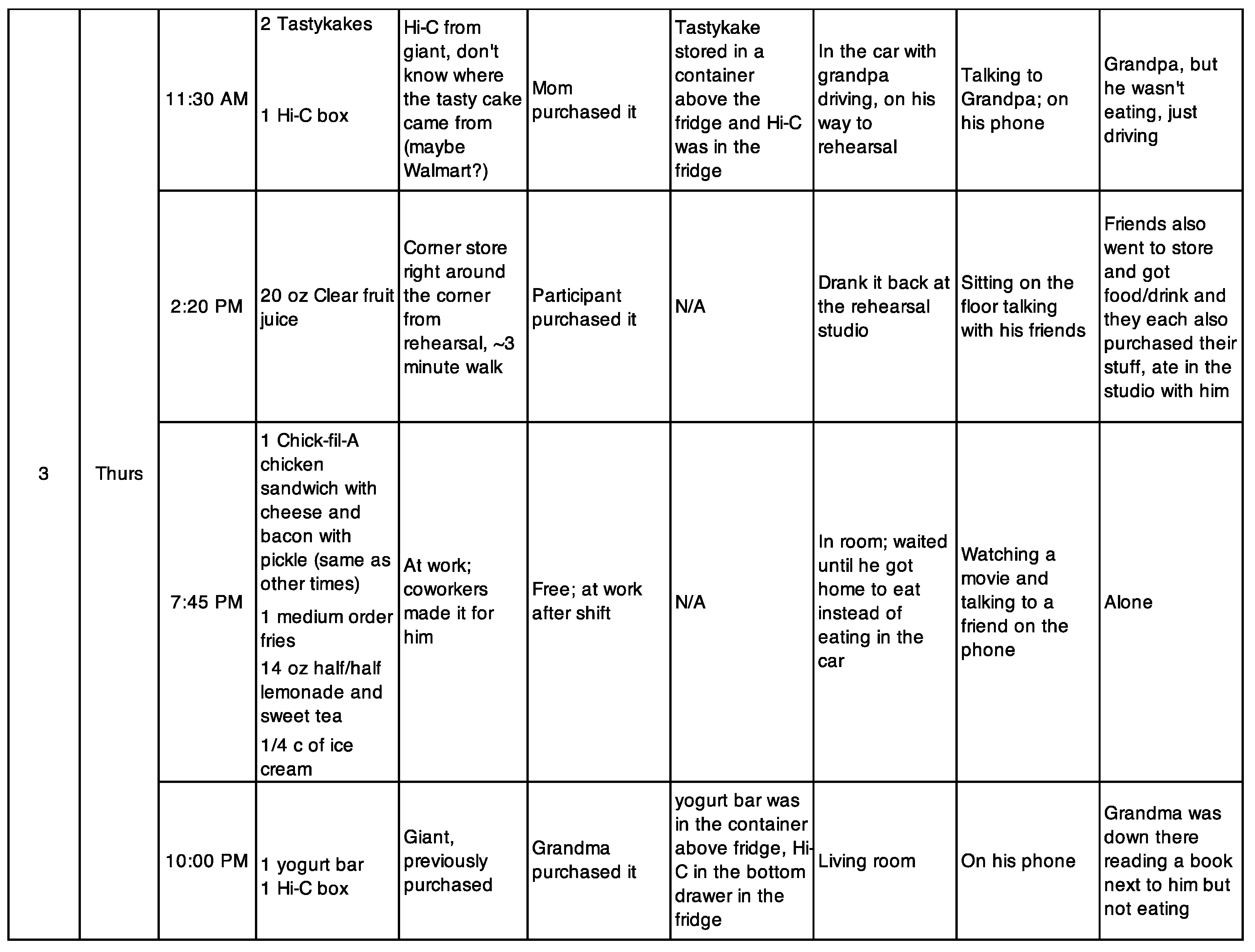
3. Results
3.1. Participant Characteristics
3.2. Differences in Diet Quality between Adolescents with Food Security and Food Insecurity
3.3. Factors Influencing Diet Quality
3.3.1. Availability and Accessibility of Seafood and Peanut Butter at Home
3.3.2. Parental Influence over Fruit and Vegetable Consumption
3.3.3. Convenient Access to Unhealthy Snacks and Breakfast Foods at Home
3.3.4. Food Environment at Adolescent Workplaces
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
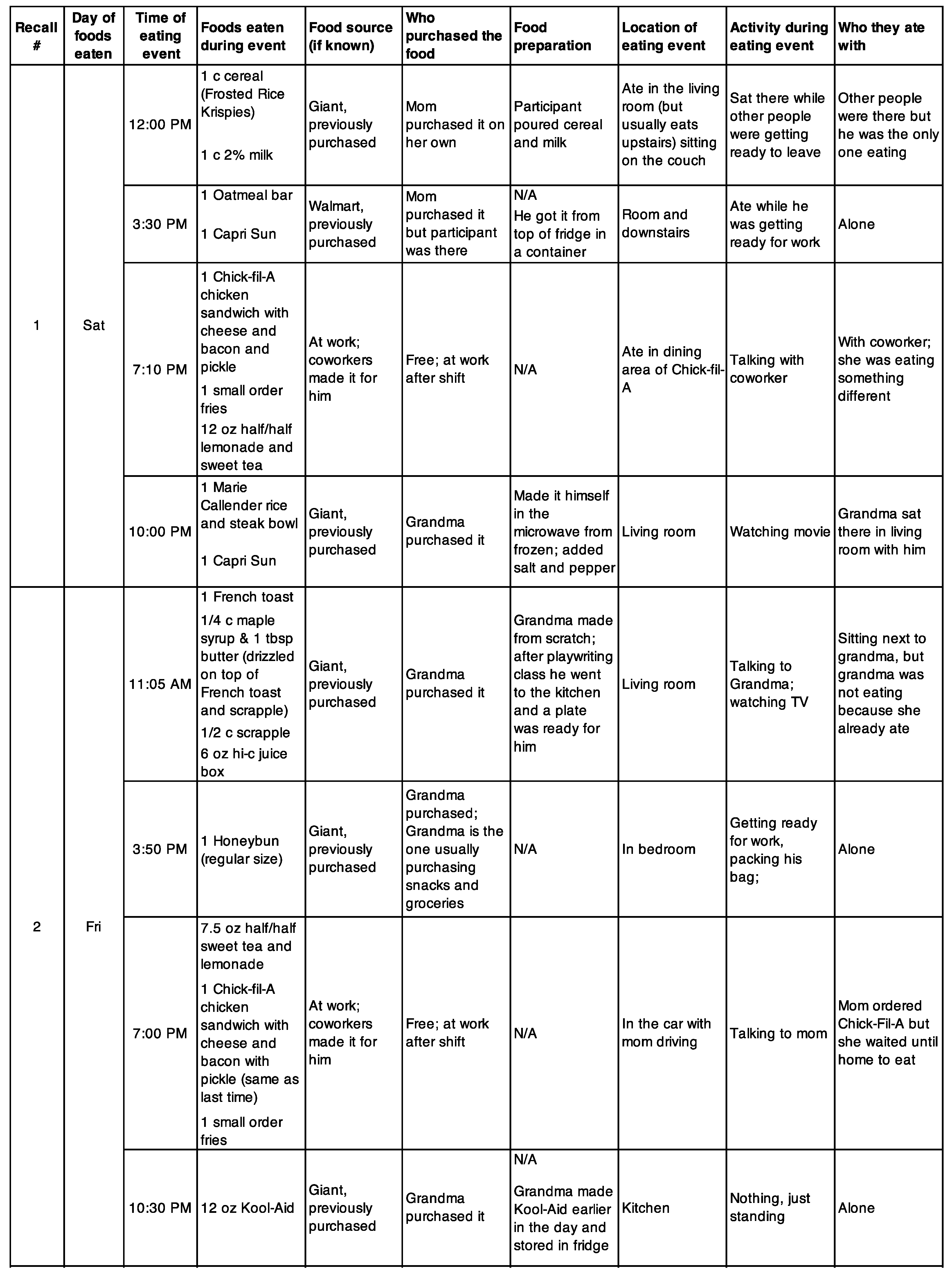
Appendix B. Structured Interview Guide for 24-h Dietary Recalls
- Introduction
- Hi [participant name]. Thanks again for agreeing to do this interview with me today. As a reminder, I’m interested in learning more about the kinds of foods you eat and more details about your experiences with food—so things like where you eat your meals, where you get your food from, and other things like that. So basically, I’m just going to ask you some questions about your day yesterday and also about your life in general, and every so often I’ll ask you some specific questions about what you ate, how much you ate, and things like that. There are no right or wrong answers to these questions; we’re just trying to understand your personal experiences. Any questions so far?
- Before we start, I want to remind you that everything you say to me in this conversation is confidential and your name and other personal info won’t be linked back to you. We won’t share your information with other people or even with your parents.
- [Ask if they are okay with recording the interview]
- Part 1: General questions—building rapport (<10 min)
- [First recall]
- 1. Okay, first off I just want to know a little bit more about you. Tell me some things about yourself, like how old you are, where you go to school, and things like that.
- 2. How has online school been for you?
- a. Probe on whatever they say—make casual conversation
- 3. You said you lived in [name of part of city]. Who lives in the house with you?
- a. Do you spend part of your time anywhere else, like with grandparents or other friends or relatives?
- b. Probe on whatever they say
- [Subsequent recalls]
- 1. How have things been going? What have you been up to?
- 2. Probe on whatever they talked about in the previous interview.
- Part 2: Context
- Tell me a bit about your day yesterday. What did you do?
- a. When did you wake up?
- b. When did you start school?
- c. When did you get out of school?
- d. What did you do after school?
- e. Did you do anything at night?
- f. What time did you go to sleep? Do you normally [stay up late/go to bed at that time/go to bed early]?
- Part 3: 24-h dietary recall
- Okay, now I’m going to start asking you some questions that are more specific to food and drinks that you had yesterday. This also includes supplements like vitamins and protein shakes, by the way.
- Part 2A: descriptive details (open-ended, conversational)
- What’s something that you ate or drank yesterday?
- 1. What time did you eat it?
- 2. What were you doing when you ate it? OR if they already talked about their schedule: That must’ve been when you were… [just waking up, finishing school…]
- 3. Were you doing anything else while you ate the food, like using your phone, watching TV?
- 4. Did you have the [food/drink] by yourself or did you have it with other people?
- a. If other people, who? Were they having the same food/drink or something else?
- 5. Where did you get the food from? (i.e., home, the corner store, school)
- (A) Foods prepared at respondents’ home OR at a different house (e.g., grandmother, friend, neighbor)
- a. Did the food need to be prepared?
- a. If yes, who prepared it?
- b. [If applicable] How was it prepared? (e.g., microwave, cooked by oven, stove, etc.)
- b. Do you know where the food came from? (e.g., someone bought it at grocery store or corner store; someone brought it home from restaurant/carryout)
- (B) Foods prepared outside the home (e.g., carryout, restaurant, corner store)
- a. Who bought the food/drink?
- a. If youth bought it, did you buy foods/drinks for anyone else at the time?
- b. How did you get to the place where you bought the food from? (e.g., walked, drove, public transportation)
- a. How far was this place from where you live?
- Part 2B: dietary details (closed-ended)
- Now I’m going to ask some more detailed information about the [food] you told me about. Some of these questions are pretty specific, like asking about brand and stuff. That’s just because I want to make sure I’m understanding the whole picture about what you’re eating, and I’ll be able to compare things like, oh half the people eat frozen pepperoni pizza and the other half get veggie pizza from the store. Or stuff like that. [Feel free to include a different example.] Any questions?
- [Repeat parts 2A and 2B for all foods]
- Okay, thanks for telling me all those details. So what’s something else you ate yesterday?
- [End: Ask about usual intake]
- Is this a normal day of eating for you, or did you eat more or less than usual?
Appendix C
| Item Order | Question * |
|---|---|
| 1 | Did you worry that food at home would run out before your family got money to buy more? |
| 2 | Did the food that your family bought run out and you didn’t have money to get more? |
| 3 | How often were you not able to eat a balanced meal because your family didn’t have enough money? |
| 4 | Did your meals only include a few kinds of cheap foods because your family was running out of money to buy food? |
| 5 | Has the size of your meals been cut because your family didn’t have enough money for food? |
| 6 | Did you have to eat less because your family didn’t have enough money to buy food? |
| 7 | Did you have to skip a meal because your family didn’t have enough money for food? |
| 8 | Were you hungry but didn’t eat because your family didn’t have enough food? |
| 9 | Did you not eat for a whole day because your family didn’t have enough money for food? |
References
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2020; United States Department of Agriculture Economic Research Service: Washington, DC, USA, 2021; p. 55.
- Committee on Examination of the Adequacy of Food Resources and SNAP Allotments; Food and Nutrition Board; Committee on National Statistics; Institute of Medicine; National Research Council; Caswell, J.A.; Yaktine, A.L. Questions on the Core Food Security Module; National Academies Press (US): Washington, DC, USA, 2013. [Google Scholar]
- Hanson, K.L.; Connor, L.M. Food Insecurity and Dietary Quality in US Adults and Children: A Systematic Review. Am. J. Clin. Nutr. 2014, 100, 684–692. [Google Scholar] [CrossRef]
- Larson, N.; Laska, M.N.; Neumark-Sztainer, D. Food Insecurity, Diet Quality, Home Food Availability, and Health Risk Behaviors among Emerging Adults: Findings from the EAT 2010–2018 Study. Am. J. Public Health 2020, 110, 1422–1428. [Google Scholar] [CrossRef]
- Lee, J.; Kubik, M.Y.; Fulkerson, J.A. Diet Quality and Fruit, Vegetable, and Sugar-Sweetened Beverage Consumption by Household Food Insecurity among 8- to 12-Year-Old Children during Summer Months. J. Acad. Nutr. Diet. 2019, 119, 1695–1702. [Google Scholar] [CrossRef]
- Leung, C.W.; Epel, E.S.; Ritchie, L.D.; Crawford, P.B.; Laraia, B.A. Food Insecurity Is Inversely Associated with Diet Quality of Lower-Income Adults. J. Acad. Nutr. Diet. 2014, 114, 1943–1953.e2. [Google Scholar] [CrossRef]
- Leung, C.W.; Tester, J.M. The Association between Food Insecurity and Diet Quality Varies by Race/Ethnicity: An Analysis of National Health and Nutrition Examination Survey 2011–2014 Results. J. Acad. Nutr. Diet. 2019, 119, 1676–1686. [Google Scholar] [CrossRef]
- Leung, C.W.; Wolfson, J.A. Food Insecurity among Older Adults: 10-Year National Trends and Associations with Diet Quality. J. Am. Geriatr. Soc. 2021, 69, 964–971. [Google Scholar] [CrossRef]
- Robaina, K.A.; Martin, K.S. Food Insecurity, Poor Diet Quality, and Obesity among Food Pantry Participants in Hartford, CT. J. Nutr. Educ. Behav. 2013, 45, 159–164. [Google Scholar] [CrossRef]
- Kral, T.V.E.; Chittams, J.; Moore, R.H. Relationship between Food Insecurity, Child Weight Status, and Parent-Reported Child Eating and Snacking Behaviors. J. Spec. Pediatr. Nurs. 2017, 22, e12177. [Google Scholar] [CrossRef]
- Darmon, N.; Drewnowski, A. Contribution of Food Prices and Diet Cost to Socioeconomic Disparities in Diet Quality and Health: A Systematic Review and Analysis. Nutr. Rev. 2015, 73, 643–660. [Google Scholar] [CrossRef]
- Ralston, K.; Treen, K.; Coleman-Jensen, A.; Guthrie, J. Children’s Food Security and USDA Child Nutrition Programs; USDA, ERS: Washington, DC, USA, 2017; p. 33.
- Fram, M.S.; Frongillo, E.A.; Jones, S.J.; Williams, R.C.; Burke, M.P.; DeLoach, K.P.; Blake, C.E. Children Are Aware of Food Insecurity and Take Responsibility for Managing Food Resources. J. Nutr. 2011, 141, 1114–1119. [Google Scholar] [CrossRef]
- Miller, D.P. Accessibility of Summer Meals and the Food Insecurity of Low-Income Households with Children. Public Health Nutr. 2016, 19, 2079–2089. [Google Scholar] [CrossRef]
- Food Research & Action Center. Hunger Doesn’t Take a Vacation: Summer Nutrition Status Report: 2018; Food Research Action Center: Washington, DC, USA, 2019. [Google Scholar]
- Feeding America; Urban Institute. Bringing Teens to the Table: A Focus on Food Insecurity in America; Feeding America: Chicago, IL, USA; Urban Institute: Washington, DC, USA, 2016. [Google Scholar]
- Eicher-Miller, H.A.; Mason, A.C.; Weaver, C.M.; McCabe, G.P.; Boushey, C.J. Food Insecurity Is Associated with Diet and Bone Mass Disparities in Early Adolescent Males but Not Females in the United States. J. Nutr. 2011, 141, 1738–1745. [Google Scholar] [CrossRef]
- Eicher-Miller, H.A.; Mason, A.C.; Weaver, C.M.; McCabe, G.P.; Boushey, C.J. Food Insecurity Is Associated with Iron Deficiency Anemia in US Adolescents. Am. J. Clin. Nutr. 2009, 90, 1358–1371. [Google Scholar] [CrossRef]
- Nord, M.; Hanson, K. Adult Caregiver Reports of Adolescents’ Food Security Do Not Agree Well with Adolescents’ Own Reports. J. Hunger. Environ. Nutr. 2012, 7, 363–380. [Google Scholar] [CrossRef]
- Duke, N.N. Adolescent-Reported Food Insecurity: Correlates of Dietary Intake and School Lunch Behavior. Int. J. Environ. Res. Public Health 2021, 18, 6647. [Google Scholar] [CrossRef]
- Widome, R.; Neumark-Sztainer, D.; Hannan, P.J.; Haines, J.; Story, M. Eating When There Is Not Enough to Eat: Eating Behaviors and Perceptions of Food among Food-Insecure Youth. Am. J. Public Health 2009, 99, 822–828. [Google Scholar] [CrossRef]
- Story, M.; Neumark-sztainer, D.; French, S. Individual and Environmental Influences on Adolescent Eating Behaviors. J. Am. Diet. Assoc. 2002, 102, S40–S51. [Google Scholar] [CrossRef]
- Maxwell, K.A. Friends: The Role of Peer Influence across Adolescent Risk Behaviors. J. Youth Adolesc. 2002, 31, 267–277. [Google Scholar] [CrossRef]
- Contento, I.R.; Williams, S.S.; Michela, J.L.; Franklin, A.B. Understanding the Food Choice Process of Adolescents in the Context of Family and Friends. J. Adolesc. Health 2006, 38, 575–582. [Google Scholar] [CrossRef]
- Ziegler, A.M.; Kasprzak, C.M.; Mansouri, T.H.; Gregory, A.M.; Barich, R.A.; Hatzinger, L.A.; Leone, L.A.; Temple, J.L. An Ecological Perspective of Food Choice and Eating Autonomy Among Adolescents. Front. Psychol. 2021, 12, 654139. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S.J.; Gorely, T. Family Correlates of Fruit and Vegetable Consumption in Children and Adolescents: A Systematic Review. Public Health Nutr. 2009, 12, 267–283. [Google Scholar] [CrossRef]
- van der Horst, K.; Oenema, A.; Ferreira, I.; Wendel-Vos, W.; Giskes, K.; van Lenthe, F.; Brug, J. A Systematic Review of Environmental Correlates of Obesity-Related Dietary Behaviors in Youth. Health Educ. Res. 2007, 22, 203–226. [Google Scholar] [CrossRef]
- Rasmussen, M.; Krølner, R.; Klepp, K.-I.; Lytle, L.; Brug, J.; Bere, E.; Due, P. Determinants of Fruit and Vegetable Consumption among Children and Adolescents: A Review of the Literature. Part I: Quantitative Studies. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 22. [Google Scholar] [CrossRef]
- Özcan, B.A.; Yeşilkaya, B.; Yaldiz, N.; Pehlivan, M. Factors Affecting Diet Quality in Adolescents: The Effect of Sociodemographic Characteristics and Meal Consumption: Factors Affecting Diet Quality in Adolescents. Progr. Nutr. 2020, 22, e2020094. [Google Scholar] [CrossRef]
- Tabbakh, T.; Freeland-Graves, J.H. The Home Environment: A Mediator of Nutrition Knowledge and Diet Quality in Adolescents. Appetite 2016, 105, 46–52. [Google Scholar] [CrossRef]
- Holsten, J.E.; Deatrick, J.A.; Kumanyika, S.; Pinto-Martin, J.; Compher, C.W. Children’s Food Choice Process in the Home Environment. A Qualitative Descriptive Study. Appetite 2012, 58, 64–73. [Google Scholar] [CrossRef]
- Creswell, J.W.; Plano Clark, V.L. Designing and Conducting Mixed Methods Research; SAGE: Los Angeles, CA, USA, 2007; ISBN 978-1-4129-2792-5. [Google Scholar]
- Ivankova, N.V.; Creswell, J.W.; Stick, S.L. Using Mixed-Methods Sequential Explanatory Design: From Theory to Practice. Field Methods 2006, 18, 3–20. [Google Scholar] [CrossRef]
- Connell, C.L.; Nord, M.; Lofton, K.L.; Yadrick, K. Food Security of Older Children Can Be Assessed Using a Standardized Survey Instrument. J. Nutr. 2004, 134, 2566–2572. [Google Scholar] [CrossRef]
- HHS Office of Disease Prevention and Health Promotion. USDA Center for Nutrition Policy and Promotion Current Dietary Guidelines. Available online: https://www.dietaryguidelines.gov/current-dietary-guidelines (accessed on 15 May 2022).
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- National Cancer Institute SAS Code: Healthy Eating Index. Available online: https://epi.grants.cancer.gov/hei/sas-code.html (accessed on 31 January 2022).
- Klassen, A.C.; Smith, K.C.; Black, M.M.; Caulfield, L.E. Mixed Methods Approaches to Understanding Cancer-Related Dietary Risk Reduction among Public Housing Residents. J. Urban Health 2009, 86, 624–640. [Google Scholar] [CrossRef]
- Boeije, H. A Purposeful Approach to the Constant Comparative Method in the Analysis of Qualitative Interviews. Qual. Quant. 2002, 36, 391–409. [Google Scholar] [CrossRef]
- United States Department of Agriculture Food and Nutrition Services HEI Scores for Americans. Available online: https://www.fns.usda.gov/hei-scores-americans (accessed on 21 February 2022).
- Liu, J.; Rehm, C.D.; Onopa, J.; Mozaffarian, D. Trends in Diet Quality among Youth in the United States, 1999–2016. JAMA 2020, 323, 1161–1174. [Google Scholar] [CrossRef]
- United States Department of Agriculture Food and Nutrition Security. Available online: https://www.usda.gov/nutrition-security (accessed on 20 October 2022).
- Gretchen Swanson Center for Nutrition Nutrition Security. Available online: https://www.centerfornutrition.org/food-insecurity-measures/nutrition-security (accessed on 20 October 2022).
- Larson, N.; MacLehose, R.; Fulkerson, J.A.; Berge, J.M.; Story, M.; Neumark-Sztainer, D. Eating Breakfast and Dinner Together as a Family: Associations with Sociodemographic Characteristics and Implications for Diet Quality and Weight Status. J. Acad. Nutr. Diet. 2013, 113, 1601–1609. [Google Scholar] [CrossRef]
- Fink, S.K.; Racine, E.F.; Mueffelmann, R.E.; Dean, M.N.; Herman-Smith, R. Family Meals and Diet Quality among Children and Adolescents in North Carolina. J. Nutr. Educ. Behav. 2014, 46, 418–422. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Hannan, P.J.; Story, M.; Croll, J.; Perry, C. Family Meal Patterns: Associations with Sociodemographic Characteristics and Improved Dietary Intake among Adolescents. J. Am. Diet. Assoc. 2003, 103, 317–322. [Google Scholar] [CrossRef]
- Videon, T.M.; Manning, C.K. Influences on Adolescent Eating Patterns: The Importance of Family Meals. J. Adolesc. Health 2003, 32, 365–373. [Google Scholar] [CrossRef]
- Clohessy, S.; Walasek, L.; Meyer, C. Factors Influencing Employees’ Eating Behaviours in the Office-Based Workplace: A Systematic Review. Obes. Rev. 2019, 20, 1771–1780. [Google Scholar] [CrossRef]
- The Annie, E. Casey Foundation Unemployed Teens Age 16 to 19. Available online: https://datacenter.kidscount.org/data/tables/5051-unemployed-teens-age-16-to-19?loc=1&loct=1 (accessed on 17 March 2022).
- Logan, C.; Connor, P.; Harvill, E.L.; Harkness, J.; Nisar, H.; Checkoway, A.; Peck, L.R.; Shivji, A.; Bein, E.; Levin, M.; et al. Community Eligibility Provision Evaluation; Abt Associates for the U.S. Department of Agriculture, Food and Nutrition Service: Washington, DC, USA, 2014.
- 116th US Congress. Families First Coronavirus Response Act; US Government Publishing Office: Washington, DC, USA, 2020; Volume H.R.6201.
- Gregory, C.A.; Mancino, L.; Coleman, A. Food Security and Food Purchase Quality among Low-Income Households: Findings from the National Household Food Acquisition and Purchase Survey (FoodAPS); USDA Economic Research Service: Washington, DC, USA, 2019; p. 42.
- United States Department of Agriculture Food and Nutrition Services. Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): Food Package Policy and Guidance; United States Department of Agriculture Food and Nutrition Service: Washington, DC, USA, 2018; p. 44.
- Poverty in Baltimore City. Available online: https://www.welfareinfo.org/poverty-rate/maryland/baltimore (accessed on 13 January 2022).
| Variable | Overall (n = 61) | Food-Secure (n = 31) | Food Insecure (n = 30) |
|---|---|---|---|
| n (%) or Median (IQR) | |||
| Age | 16 (2.5) | 16 (2.5) | 16 (2.3) |
| Gender | |||
| Boy | 30 (49.2%) | 15 (48.3%) | 15 (50.0%) |
| Girl | 31 (50.8%) | 16 (51.7%) | 15 (50.0%) |
| Race | |||
| Black | 59 (96.7%) | 30 (96.8%) | 29 (96.7%) |
| Biracial (Black/White) | 2 (3.3%) | 1 (3.2%) | 1 (3.3%) |
| Youth employment | |||
| No job | 40 (65.6%) | 20 (64.5%) | 20 (66.7%) |
| Part-time | 19 (31.2%) | 10 (32.3%) | 9 (30.0%) |
| Full-time | 2 (3.4%) | 1 (3.2%) | 1 (3.3%) |
| Experiencing housing instability | 3 (4.9%) | 1 (3.2%) | 2 (6.7%) |
| HH size | |||
| 1–4 people | 27 (45.0%) | 15 (48.4%) | 12 (41.4%) |
| >4 people | 33 (55.0%) | 16 (51.6%) | 17 (58.6%) |
| Lives in single-parent household | 33 (52.4%) | 18 (58.1%) | 15 (50.0%) |
| Component (Max Score) | Overall (n = 61) | Food Secure (n = 31) | Food Insecure (n = 30) | Difference in Median (FS-FI) | p-Value * | |||
|---|---|---|---|---|---|---|---|---|
| Median | Q1, Q3 § | Median | Q1, Q3 † | Median | Q1, Q3 § | |||
| Total fruits (5) | 1.58 | 0.39, 4.29 | 1.36 | 0.16, 4.35 | 1.74 | 0.59, 3.87 | −0.38 | 0.90 |
| Whole fruits (5) | 0.11 | 0, 3.20 | 0.31 | 0, 2.53 | 0.10 | 0, 3.40 | +0.21 | 0.90 |
| Total vegetables (5) | 2.47 | 1.71, 3.33 | 2.73 | 1.65, 3.54 | 2.16 | 1.72, 2.94 | +0.57 | 0.46 |
| Beans and greens (5) | 0.55 | 0, 3.37 | 0.2 | 0, 4.23 | 0.56 | 0, 2.16 | −0.36 | 0.56 |
| Whole grains (10) | 0.1 | 0, 1.55 | 0 | 0, 1.84 | 0.59 | 0, 1.45 | −0.59 | 0.64 |
| Dairy (10) | 4.82 | 3.49, 6.76 | 5.61 | 3.69, 6.99 | 4.09 | 2.96, 6.40 | +1.52 | 0.17 |
| Total protein foods (5) | 5.0 | 4.51, 5.0 | 5 | 4.75, 5 | 5 | 4.43, 5.0 | 0 | 0.58 |
| Seafood & plant proteins (5) | 1.68 | 0.07, 4.93 | 0.52 | 0.02, 2.72 | 3.23 | 0.65, 5.0 | −2.71 | 0.02 |
| Fatty acids (10) | 3.82 | 2.35, 8.06 | 3.82 | 2.08, 7.88 | 4.45 | 2.62, 7.98 | −0.63 | 0.68 |
| Refined grains (10) † | 6.97 | 4.17, 9.15 | 6.97 | 5.47, 9.89 | 7.15 | 3.56, 8.15 | −0.18 | 0.25 |
| Sodium (10) † | 3.17 | 1.27, 5.10 | 3.08 | 0.16, 5.55 | 3.18 | 2.35, 4.65 | −0.10 | 0.80 |
| Added sugars (10) † | 7.16 | 5.08, 8.66 | 7.27 | 4.78, 8.35 | 6.65 | 5.20, 8.99 | +0.62 | 0.87 |
| Saturated fats (10) † | 4.42 | 2.04, 6.16 | 4.96 | 2.07, 6.03 | 4.10 | 2.07, 6.47 | +0.86 | 0.96 |
| Total HEI score (100) | 46.53 | 37.64, 53.23 | 46.82 | 39.28, 53.68 | 45.82 | 37.48, 53.09 | +1 | 0.77 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harper, K.; Caulfield, L.E.; Lu, S.V.; Mmari, K.; Gross, S.M. Diet Quality and Contextual Factors Influencing Food Choice among Adolescents with Food Security and Food Insecurity in Baltimore City. Nutrients 2022, 14, 4573. https://doi.org/10.3390/nu14214573
Harper K, Caulfield LE, Lu SV, Mmari K, Gross SM. Diet Quality and Contextual Factors Influencing Food Choice among Adolescents with Food Security and Food Insecurity in Baltimore City. Nutrients. 2022; 14(21):4573. https://doi.org/10.3390/nu14214573
Chicago/Turabian StyleHarper, Kaitlyn, Laura E. Caulfield, Stacy V. Lu, Kristin Mmari, and Susan M. Gross. 2022. "Diet Quality and Contextual Factors Influencing Food Choice among Adolescents with Food Security and Food Insecurity in Baltimore City" Nutrients 14, no. 21: 4573. https://doi.org/10.3390/nu14214573
APA StyleHarper, K., Caulfield, L. E., Lu, S. V., Mmari, K., & Gross, S. M. (2022). Diet Quality and Contextual Factors Influencing Food Choice among Adolescents with Food Security and Food Insecurity in Baltimore City. Nutrients, 14(21), 4573. https://doi.org/10.3390/nu14214573







