Does Abdominal Obesity Increase All-Cause, Cardiovascular Disease, and Cancer Mortality Risks in Older Adults? A 10-Year Follow-Up Analysis
Abstract
1. Introduction
2. Material & Methods
2.1. Study Population
2.2. Study Variables
2.3. Abdominal Obesity (AO)
2.4. Mortality Ascertainment
2.5. Statistical Analysis
2.6. Ethical Aspects
3. Results
3.1. Baseline Characteristics
3.2. All-Cause Mortality
3.3. CVD Mortality
3.4. Cancer Mortality
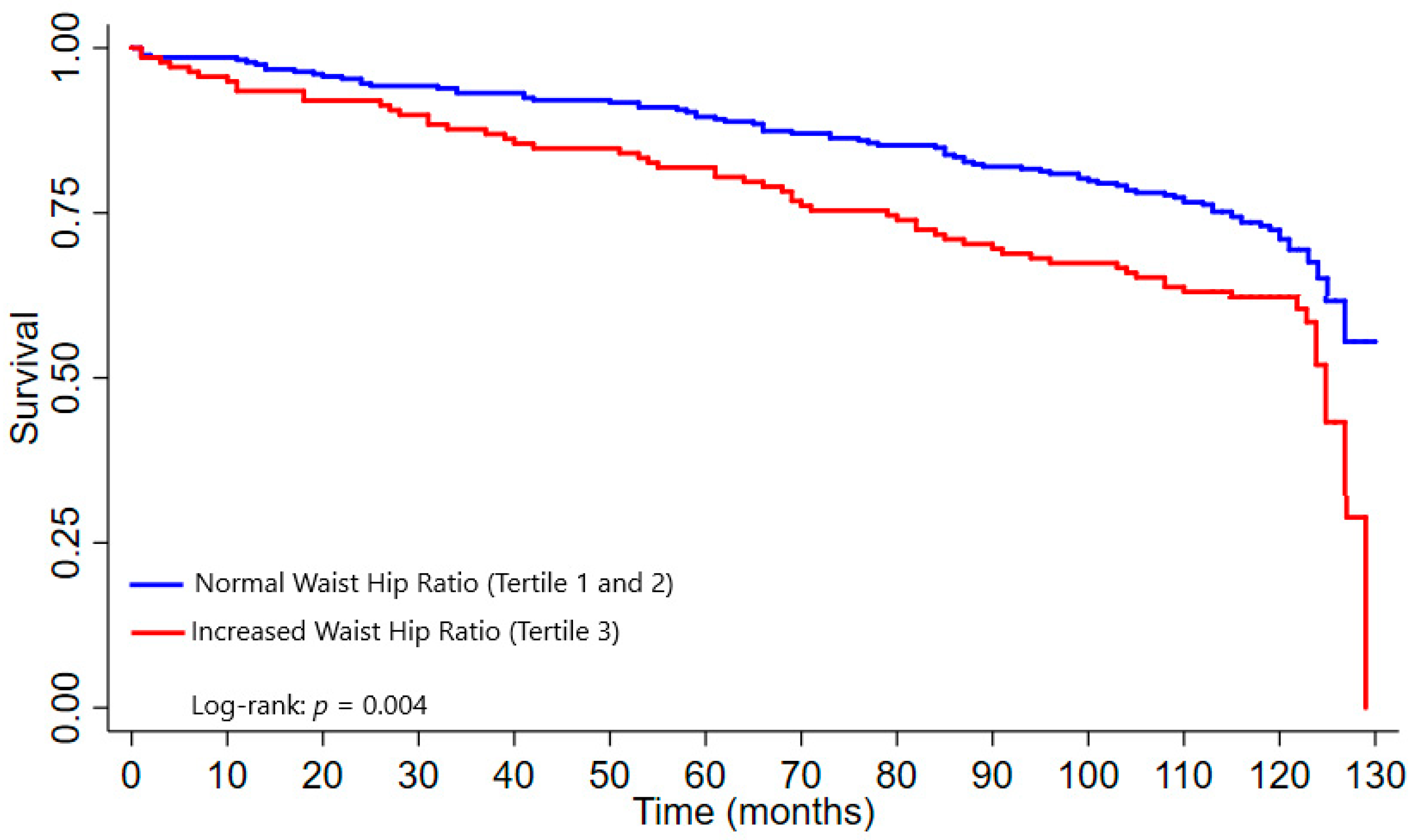
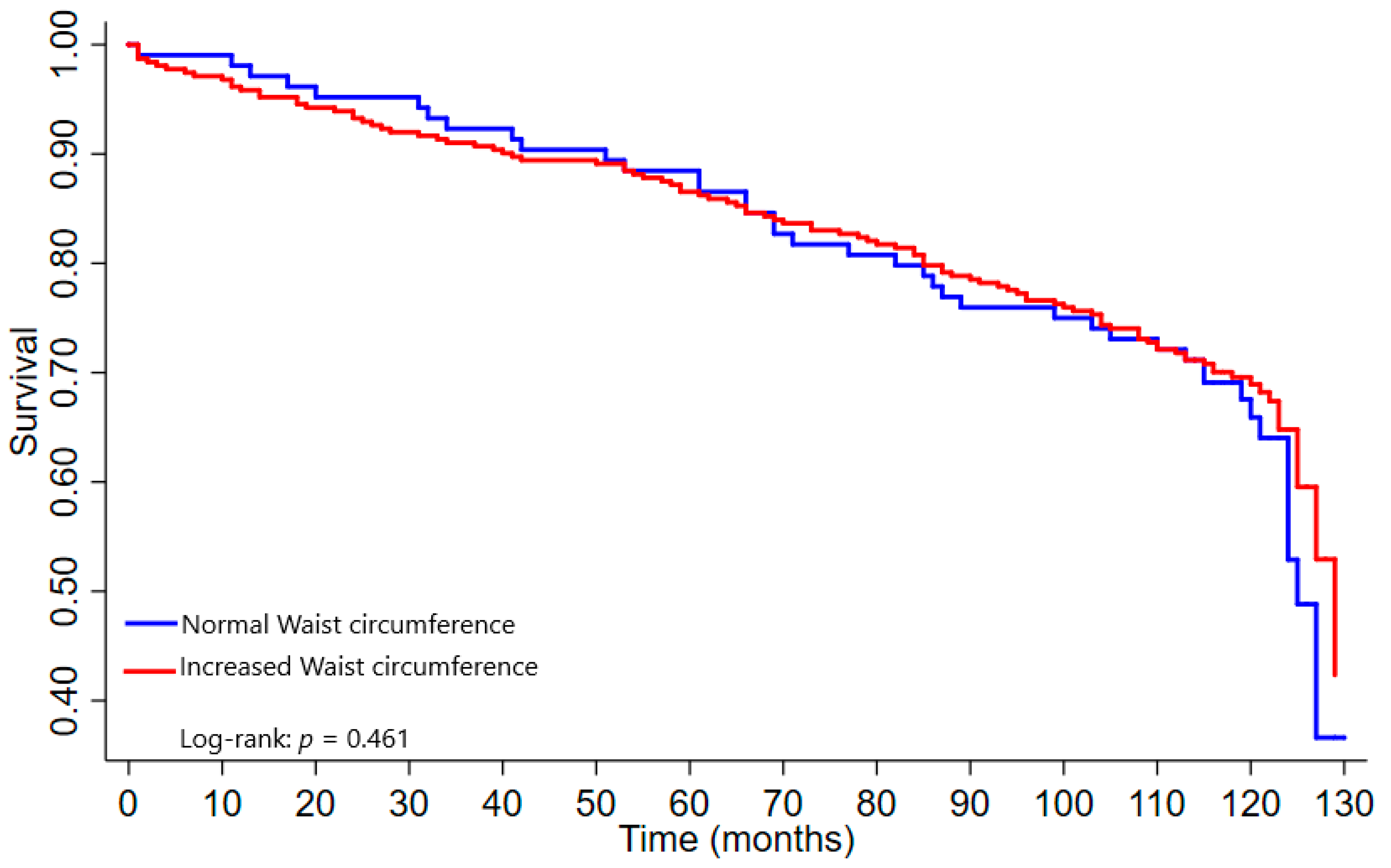
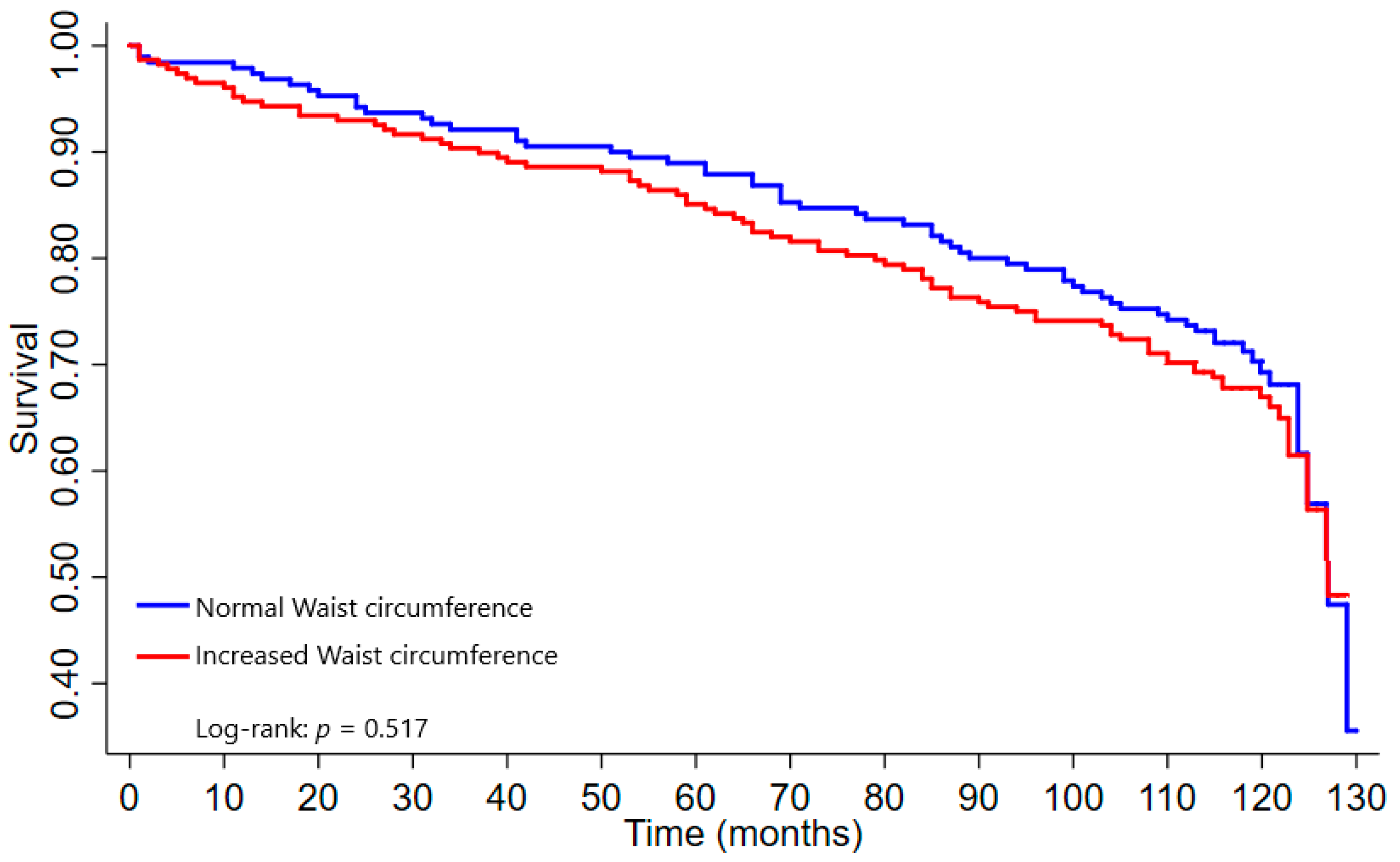
3.5. Survival Curves
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bennett, J.E.; Stevens, G.A.; Mathers, C.D.; Bonita, R.; Rehm, J.; Kruk, M.E.; Riley, L.M.; Dain, K.; Kengne, A.P.; Chalkidou, K.; et al. NCD Countdown 2030: Worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 2018, 392, 1072–1088. [Google Scholar] [CrossRef]
- GBD 2019 Ageing Collaborators. Global, regional, and national burden of diseases and injuries for adults 70 years and older: Systematic analysis for the Global Burden of Disease 2019 Study. BMJ 2022, 376, e068208. [Google Scholar] [CrossRef]
- Silveira, E.A.; Kliemann, N.; Noll, M.; Sarrafzadegan, N.; de Oliveira, C. Visceral obesity and incident cancer and cardiovascular disease: An integrative review ofthe epidemiological evidence. Obes. Rev. 2021, 22, e13088. [Google Scholar] [CrossRef] [PubMed]
- Silveira, E.A.; Vaseghi, G.; de Carvalho, A.S.S.; Kliemann, N.; Masoudkabir, F.; Noll, M.; Mohammadifard, N.; Sarrafzadegan, N.; de Oliveira, C. Visceral Obesity and Its Shared Role in Cancer and Cardiovascular Disease: A Scoping Review of the Pathophysiology and Pharmacological Treatments. Int. J. Mol. Sci. 2020, 21, 9042. [Google Scholar] [CrossRef]
- Jura, M.; Kozak, L.P. Obesity and related consequences to ageing. AGE 2016, 38, 23. [Google Scholar] [CrossRef]
- dos Santos Costa, C.; Schneider, B.C.; Cesar, J.A. General and abdominal obesity among the elderly from Southern Brazil: Results of the HOW ARE YOU DOING? (COMO VAI?) study. Ciênc. Saúde Colet. 2016, 21, 3585–3596. [Google Scholar] [CrossRef]
- Silveira, E.A.; Vieira, L.L.; de Souza, J.D. High prevalence of abdominal obesity in elderly and association with diabetes, hypertension and respiratory diseases. Ciênc. Saúde Colet. 2018, 23, 903–912. [Google Scholar] [CrossRef]
- Løvsletten, O.; Jacobsen, B.K.; Grimsgaard, S.; Njølstad, I.; Wilsgaard, T.; Løchen, M.L.; Eggen, A.E.; Hopstock, L.A. Prevalence of general and abdominal obesity in 2015–2016 and 8-year longitudinal weight and waist circumference changes in adults and elderly: The Tromsø Study. BMJ Open 2020, 10, e038465. [Google Scholar] [CrossRef] [PubMed]
- Orces, C.H.; Montalvan, M.; Tettamanti, D. Prevalence of abdominal obesity and its association with cardio metabolic risk factors among older adults in Ecuador. Diabetes Metab. Syndr. 2017, 11, S727–S733. [Google Scholar] [CrossRef] [PubMed]
- Shaharuddin, A.B.; Aziz, N.S.A.; Ahmad, M.H.; Singh, J.S.M.; Chan, Y.Y.; Palaniveloo, L.; Kee, C.C.; Zulkafly, N.; Wong, N.I.; Salleh, R.; et al. Abdominal obesity and its associated factors among older adults in Malaysia. Geriatr. Gerontol. Int. 2020, 20, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Nam, G.E.; Kim, Y.-H.; Han, K.; Jung, J.-H.; Rhee, E.-J.; Lee, S.-S.; Kim, D.J.; Lee, K.-W.; Lee, W.-Y. Obesity fact sheet in Korea, 2019: Prevalence of obesity and abdominal obesity from 2009 to 2018 and social factors. J. Obes. Metab. Syndr. 2020, 29, 124. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chen, Y.; Boucher, N.L.; Rothberg, A.E. Prevalence and change of central obesity among US Asian adults: NHANES 2011–2014. BMC Public Health 2017, 17, 678. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, D.; Sharma, S. Abdominal Obesity, Adipokines and Non-communicable Diseases. J. Steroid Biochem. Mol. Biol. 2020, 203, 105737. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Berg, E.; Cheng, X.; Shen, W. How to best assess abdominal obesity. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Milagres, L.C.; Martinho, K.O.; Milagres, D.C.; Franco, F.S.; Ribeiro, A.Q.; de Novaes, J.F. Waist-to-height ratio and the conicity index are associated to cardiometabolic risk factors in the elderly population. Ciênc. Saúde Colet. 2019, 24, 1451–1461. [Google Scholar] [CrossRef] [PubMed]
- da Silva, A.T.; Scholes, S.; Ferreira, S.J.L.; de Oliveira, D.Y.A.; de Oliveira, C. Dynapenic Abdominal Obesity Increases Mortality Risk Among English and Brazilian Older Adults: A 10-Year Follow-Up of the ELSA and SABE Studies. J. Nutr. Health Aging 2018, 22, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Pujilestari, C.U.; Nyström, L.; Norberg, M.; Ng, N. Waist Circumference and All-Cause Mortality among Older Adults in Rural Indonesia. Int. J. Environ. Res. Public Health 2019, 16, 116. [Google Scholar] [CrossRef] [PubMed]
- Puzianowska-Kuznicka, M.; Kuryłowicz, A.; Walkiewicz, D.; Borkowska, J.; Owczarz, M.; Olszanecka-Glinianowicz, M.; Wieczorowska-Tobis, K.; Skalska, A.; Szybalska, A.; Mossakowska, M. Obesity Paradox in Caucasian Seniors: Results of the PolSenior Study. J. Nutr. Health Aging 2019, 23, 796–804. [Google Scholar] [CrossRef]
- Sharma, S.; Batsis, J.A.; Coutinho, T.; Somers, V.K.; Hodge, D.O.; Carter, R.E.; Sochor, O.; Kragelund, C.; Kanaya, A.M.; Zeller, M.; et al. Normal-Weight Central Obesity and Mortality Risk in Older Adults with Coronary Artery Disease. Mayo. Clin. Proc. Innov. Qual. Outcomes 2016, 91, 343–351. [Google Scholar] [CrossRef]
- Streng, K.W.; Voors, A.A.; Hillege, H.L.; Anker, S.D.; Cleland, J.G.; Dickstein, K.; Filippatos, G.; Metra, M.; Ng, L.L.; Ponikowski, P.; et al. Waist-to-hip ratio and mortality in heart failure. Eur. J. Heart Fail. 2018, 20, 1269–1277. [Google Scholar] [CrossRef]
- Bowman, K.; Atkins, J.L.; Delgado, J.; Kos, K.; Kuchel, G.A.; Ble, A.; Ferrucci, L.; Melze, D. Central adiposity and the overweight risk paradox in aging: Follow-up of 130,473 UK Biobank participants. Am. J. Clin. Nutr. 2017, 106, 130–135. [Google Scholar] [CrossRef]
- de Almeida, R.M.; de Fátima, N.M.M.; Quintiliano, S.D.D.A.; de Oliveira, C.; Santos, J.L.F.; de Oliveira, D.Y.A. Body Composition Changes and 10-Year Mortality Risk in Older Brazilian Adults: Analysis of Prospective Data from the SABE Study. J. Nutr. Health Aging 2019, 23, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Kazempour-Ardebili, S.; Ramezankhani, A.; Eslami, A.; Akbarpour, S.; Azizi, F.; Hadaegh, F. Metabolic mediators of the impact of general and central adiposity measures on cardiovascular disease and mortality risks in older adults: Tehran Lipid and Glucose Study. Geriatr. Gerontol. Int. 2017, 17, 2017–2024. [Google Scholar] [CrossRef] [PubMed]
- Folsom, A.R.; Kushi, L.H.; Anderson, K.E.; Mink, P.J.; Olson, J.E.; Hong, C.-P.; Sellers, T.A.; Lazovich, D.; Prineas, R.J. Associations of General and Abdominal Obesity with Multiple Health Outcomes in Older Women. Arch. Intern. Med. 2000, 160, 2117. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Liu, B.; Linda, G.S.; Robert, B.W.; Bette, J.C.; Thomas, E.R.; Marian, L.N.; Aladdin, H.S.; Rowan, T.C.; . Manson, J.E.; et al. Association of Normal-Weight Central Obesity with All-Cause and Cause-Specific Mortality Among Postmenopausal Women. JAMA Netw. Open 2019, 2, e197337. [Google Scholar] [CrossRef] [PubMed]
- Pagotto, V.; Nakatani, A.Y.K.; Silveira, E.A. Factors associated with poor self-rated health in elderly users of the Brazilian Unified National Health System. Cad. Saude Publica 2011, 27, 1593–1602. [Google Scholar] [CrossRef] [PubMed][Green Version]
- de Araújo, N.C.; Silveira, E.A.; Mota, B.G.; Mota, J.P.N.; de Camargo Silva, A.E.B.; Guimarães, R.A.; Pagotto, V. Potentially inappropriate medications for the elderly: Incidence and impact on mortality in a cohort ten-year follow-up. PLoS ONE 2020, 15, e0240104. [Google Scholar] [CrossRef] [PubMed]
- Silveira, E.A.; Pagotto, V.; Barbosa, L.S.; Oliveira, C.; das Graças Pena, G.; Velasquez-Melendez, G. Accuracy of cutoff points for BMI and WC in predicting excess body fat in the older adults. Cien. Saude Colet. 2020, 25, 1073–1082. [Google Scholar] [CrossRef] [PubMed]
- Pagotto, V.; Silveira, E.A.; Velasco, W.D. The profile of hospitalizations and associated factors among elderly users of the Brazilian Unified Health System (SUS). Cien. Saude Colet. 2013, 18, 3061–3070. [Google Scholar] [CrossRef][Green Version]
- Silveira, E.A.; Dalastra, L.; Pagotto, V. Polypharmacy, chronic diseases and nutritional markers in community-dwelling older. Rev. Bras. Epidemiol. 2014, 17, 818–829. [Google Scholar] [CrossRef]
- ABEP-Associação Brasileira de Empresas de Pesquisa. 2008. Available online: https://www.abep.org/ (accessed on 15 January 2022).
- Pardini, R.; Matsudo, S.; Araújo, T.; Matsudo, V.; Andrade, E.; Braggion, G.; Andrade, D.; Oliveira, L.; Figueira Jr., A.; Raso, V. Validation of the International Physical Activity Questionaire (IPAQ version 6): Pilot study in Brazilian young adults. Rev. Bras. Ciên E Mov. 2001, 9, 45–51. [Google Scholar]
- Ministério Da Saúde. Instituto Nacional de Câncer. Abordagem e Tratamento do Fumante–Consenso. Available online: https://www.inca.gov.br/publicacoes/livros/abordagem-e-tratamento-do-fumante-consenso (accessed on 20 January 2022).
- Drozda, J.; Messer, J.V.; Spertus, J.; Abramowitz, B.; Alexander, K.; Beam, C.T.; Robert, O.B.; Jill, S.B.; Crouch, M.; David, C.G.; et al. ACCF/AHA/AMA–PCPI 2011 Performance Measures for Adults with Coronary Artery Disease and Hypertension. Circulation 2011, 124, 248–270. [Google Scholar] [CrossRef] [PubMed]
- National Cholesterol Education Program; National Heart, lung and blood institute National Institutes of Health. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002, 106, 3143. [Google Scholar] [CrossRef]
- American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018, 41, S13–S27. [Google Scholar] [CrossRef] [PubMed]
- Lohman, T.G.; Roche, A.F.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics Books: Champaign, IL, USA, 1988. [Google Scholar]
- World Health Organization (WHO). Physical Status: The Use and Interpretation of Anthropometry; WHO: Geneva, Switzerland, 1995; p. 452. [Google Scholar]
- Hosmer, D.W.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons, Incorporated: New York, NY, USA, 2013. [Google Scholar]
- Wong, M.C.S.; Huang, J.; Wang, J.; Paul, S.; Chan, F.; Lok, V.; Chen, X.; Leung, C.; Wang, H.H.X.; Lao, X.Q.; et al. Global, regional and time-trend prevalence of central obesity: A systematic review and meta-analysis of 13.2 million subjects. Eur. J. Epidemiol. 2020, 35, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Tchernof, A.; Després, J.-P. Pathophysiology of Human Visceral Obesity: An Update. Physiol. Rev. 2013, 93, 359–404. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief 2020, 360, 1–8. [Google Scholar]
- Sahakyan, K.R.; Somers, V.K.; Juan, P.; Rodriguez-Escudero, D.O.H.; Carter, R.E.; Sochor, O.; Coutinho, T.; Jensen, M.D.; Roger, V.L.; Singh, P.; et al. Normal-Weight Central Obesity: Implications for Total and Cardiovascular Mortality. Ann. Intern. Med. 2015, 163, 827. [Google Scholar] [CrossRef] [PubMed]
- Srikanthan, P.; Seeman, T.E.; Karlamangla, A.S. Waist-Hip-Ratio as a Predictor of All-Cause Mortality in High-Functioning Older Adults. Ann. Epidemiol. 2009, 19, 724–731. [Google Scholar] [CrossRef]
- Yu, J.Y.; Choi, W.J.; Lee, H.S.; Lee, J.W. Relationship between inflammatory markers and visceral obesity in obese and overweight Korean adults: An observational study. Medicine 2019, 98, e14740. [Google Scholar] [CrossRef]
- de Hollander, E.L.; Bemelmans, W.J.; Boshuizen, H.C.; Friedrich, N.; Wallaschofski, H.; Guallar-Castillón, P.; Walter, S.; Zillikens, M.C.; Rosengren, A.; Lissner, L.; et al. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: A meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Int. J. Epidemiol. 2012, 41, 805–817. [Google Scholar] [CrossRef]
- Price, G.M.; Uauy, R.; Breeze, E.; Bulpitt, C.J.; Fletcher, A.E. Weight, shape, and mortality risk in older persons: Elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death1–3. Am. J. Clin. Nutr. 2006, 84, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Neeland, I.J.; Ross, R.; Després, J.P.; Matsuzawa, Y.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; et al. International Atherosclerosis Society; International Chair on Cardiometabolic Risk Working Group on Visceral Obesity. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: A position statement. Lancet Diabetes Endocrinol. 2019, 7, 715–725. [Google Scholar] [CrossRef]
- Deng, T.; Lyon, C.J.; Bergin, S.; Caligiuri, M.A.; Hsueh, W.A. Obesity, Inflammation, and Cancer. Annu. Rev. Pathol. 2016, 11, 421–449. [Google Scholar] [CrossRef]
- Cabrera, M.A.S.; Wajngarten, M.; Gebara, O.C.E.; Diament, J. Relação do índice de massa corporal, da relação cintura-quadril e da circunferência abdominal com a mortalidade em mulheres idosas: Seguimento de 5 anos. Cad. Saude Publica 2005, 21, 767–775. [Google Scholar] [CrossRef]
- Sandoval-Insausti, H.; Jiménez-Onsurbe, M.; Donat-Vargas, C.; Rey-García, J.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. Ultra-Processed Food Consumption Is Associated with Abdominal Obesity: A Prospective Cohort Study in Older Adults. Nutrients 2020, 12, 2368. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, S.K.; Papandreou, D.; Tassoulas, E.; Biskanaki, F.; Kalogiannis, S.; Hassapidou, M.N. Gender and Exercise in Relation to Obesity in Greek Elderly Population. Int. J. Environ. Res. Public Health 2020, 17, 6575. [Google Scholar] [CrossRef]
| Variables | “n” (%)/Mean ± SD |
|---|---|
| Gender | |
| Men | 142 (34.0) |
| Woman | 276 (66.0) |
| Age group (years) | |
| 60–69 | 203 (48.6) |
| 70–79 | 168 (40.2) |
| 80+ | 47 (11.2) |
| Waist circumference (WC) | 93.49 ± 12.86 |
| Increased WC (WHO, 1995) [38] | |
| No | 104 (25.0) |
| Yes | 312 (75.0) |
| Increased WC (Silveira et al., 2020) [28] | |
| No | 190 (45.5) |
| Yes | 228 (54.5) |
| Hip circumference | 99.59 ± 10.30 |
| Waist hip ratio (WHR) | 0.94 ± 0.09 |
| WHR | |
| 1st and 2nd tertiles | 278 (66.8) |
| 3rd tertile | 138 (33.2) |
| Mortality-all-cause | 147 (35.2) |
| Mortality-CVD | 49 (11.2) |
| Mortality-cancer | 22 (5.3) |
| Abdominal Obesity Indicators | Causes of Mortality | |||||
|---|---|---|---|---|---|---|
| All-Cause | CVD | Cancer | ||||
| HR (CI 95%) | p-Value | HR (CI 95%) | p-Value | HR (CI 95%) | p-Value | |
| WC (WHO, 1995) [38] | 0.83 (0.58–1.17) | 0.284 | 1.70 (0.83–3.52) | 0.149 | 0.85 (0.34–2.08) | 0.717 |
| WC (Silveira et al., 2020) [28] | 0.87 (0.61–1.25) | 0.463 | 2.01 (0.90–4.47) | 0.089 | 0.91 (0.35–2.32) | 0.839 |
| WHR | 1.62 (1.16–2.25) | 0.004 | 1.71 (0.96–3.05) | 0.067 | 1.57 (0.67–3.67) | 0.301 |
| Mortality Causes | WC a (Who, 1995 [38]) | WC b (Silveira et al., 2020 [28]) | WHR c | |||
|---|---|---|---|---|---|---|
| HR (CI 95%) | p-Value | HR (CI 95%) | p-Value | HR (CI 95%) | p-Value | |
| All-cause | ||||||
| Model 1 | 0.91 (0.65–1.27) | 0.567 | 0.92 (0.65–1.29) | 0.626 | 1.46 (1.00–2.11) | 0.044 |
| Model 2 | 0.59 (0.35–1.02) | 0.058 | 0.59 (0.65–1.01) | 0.055 | 1.31 (0.77–2.23) | 0.319 |
| CVD | ||||||
| Model 1 | 2.61 (1.15–5.91) | 0.022 | 2.71 (1.14–6.44) | 0.023 | 1.61 (0.92–2.84) | 0.101 |
| Model 2 | 2.45 (1.03–5.84) | 0.043 | 2.88 (1.15–7.23) | 0.024 | 1.34 (0.57–3.13) | 0.506 |
| Cancer | ||||||
| Model 1 | 1.03 (0.37–2.42) | 0.948 | 1.08 (0.38–3.09) | 0.878 | 1.41 (0.56–3.55) | 0.467 |
| Model 2 | 1.14 (0.35–3.74) | 0.830 | 0.90 (0.23–3.56) | 0.882 | 2.05 (0.63–6.32) | 0.230 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moura, L.d.A.N.e.; Pagotto, V.; Camargo Pereira, C.; de Oliveira, C.; Silveira, E.A. Does Abdominal Obesity Increase All-Cause, Cardiovascular Disease, and Cancer Mortality Risks in Older Adults? A 10-Year Follow-Up Analysis. Nutrients 2022, 14, 4315. https://doi.org/10.3390/nu14204315
Moura LdANe, Pagotto V, Camargo Pereira C, de Oliveira C, Silveira EA. Does Abdominal Obesity Increase All-Cause, Cardiovascular Disease, and Cancer Mortality Risks in Older Adults? A 10-Year Follow-Up Analysis. Nutrients. 2022; 14(20):4315. https://doi.org/10.3390/nu14204315
Chicago/Turabian StyleMoura, Letícia de Almeida Nogueira e, Valéria Pagotto, Cristina Camargo Pereira, Cesar de Oliveira, and Erika Aparecida Silveira. 2022. "Does Abdominal Obesity Increase All-Cause, Cardiovascular Disease, and Cancer Mortality Risks in Older Adults? A 10-Year Follow-Up Analysis" Nutrients 14, no. 20: 4315. https://doi.org/10.3390/nu14204315
APA StyleMoura, L. d. A. N. e., Pagotto, V., Camargo Pereira, C., de Oliveira, C., & Silveira, E. A. (2022). Does Abdominal Obesity Increase All-Cause, Cardiovascular Disease, and Cancer Mortality Risks in Older Adults? A 10-Year Follow-Up Analysis. Nutrients, 14(20), 4315. https://doi.org/10.3390/nu14204315






