Abstract
Cognitive impairment and dementia can negatively impact the nutritional capacities of older people. Malnutrition is common in hospitalized frail elderly people with cognitive impairment and negatively affects prognosis. Malnutrition worsens the quality of life and increases morbidity and mortality. This scoping review aimed to identify factors affecting the risk of malnutrition and preventive strategies in hospitalized patients with cognitive impairment, focusing on nursing interventions. The authors researched population, context, and concept in international databases of nursing interest. Full texts that met the inclusion criteria were selected and reviewed. The extracted data were subject to thematic analysis. A five-stage approach, already reported in the scientific literature, was utilized in the following scoping review. Of 638 articles yielded, 9 were included. Two focus areas were identified as follows: (1) prevalence and risk factors of malnutrition in older patients with cognitive decline; (2) nursing strategies used to enhance clinical outcomes. Nursing health interventions aim to recognize and reduce malnutrition risk, positively impacting this phenomenon. A multidisciplinary team is essential to meet the nutritional needs of these patients.
1. Introduction
Due to the global increase in aging, the elderly population is constantly growing [1]. During the period 2015–2030, the elderly population is expected to grow from 901 million to 1.4 billion people (by 56%), and the 2015 population is expected to double by 2050 [2].
This increase in the elderly population is already placing substantial extra strain on healthcare and support services [3], increasing the costs due to health-related complications [4].
Among the main concerns linked to age, malnutrition is a common health problem in people older than 65 [5]; in fact, nutritional fragility is a frequent condition in vulnerable elderly people and is related to an increased incidence of mortality in this population [6]. Moreover, it is often associated with a reduced adaptive response to physiological and pathological conditions [7]; for instance, the elderly population experiences a physiological loss of taste, which impacts the frailty condition. Assessment of nutritional status through anthropometric measurements in these patients is essential to ensure healthy aging and adequate food intake [8].
Malnutrition has a negative impact on both people living independently and, overall, on those admitted to healthcare facilities, affecting up to 60% of hospitalized older adults [9]. In fact, according to estimates, up to 50% of patients are undernourished when they are admitted, increasing their malnutrition while being treated in a hospital [10]. This issue is linked to lengthier hospital stays, increased morbidity (pressure ulcers, infections, and falls), and mortality, especially in patients affected by chronic diseases [11,12].
In elderly people with cognitive impairment, the phenomenon is also more serious, since malnutrition irreversibly worsens other health conditions [13]. At the same time, mental status significantly affects nutritional status; people with lower cognitive levels tend to face a higher risk of malnutrition, especially during hospitalization [14,15]. The relationships between nutritional status, cognitive decline, and performance are complex and reciprocal: the presence or the risk of malnutrition may influence cognitive performance, and the presence of cognitive decline may affect the activities of daily living (ADL), also affecting food intake [16].
Unfortunately, malnutrition is also a frequently underdiagnosed entity, capable of subtly impacting patient outcomes, length of stay, hospital costs, and readmissions [9]. Recent studies suggest the crucial role of nurses in preventing, assessing, and treating malnutrition in this fragile population [2,7]. One of the possible key points could be implementing all known strategies to avoid worsening nutritional status, improving health status, and reducing mortality risk [17].
Therefore, this scoping review was targeted at evaluating the relationship between nursing activities and the identification, prevention, and management of malnutrition among hospitalized elderly individuals with cognitive impairment. In particular, our aims were collecting best practice and scientific evidence with regard to: (i) risk factors for developing low food intake in hospitalized older patients with cognitive impairment; (ii) prevalence of malnutrition in older patients with cognitive impairment; (iii) identify the nursing strategies to enhance clinical outcomes and care of patients with cognitive impairment in the hospital environments.
2. Materials and Methods
2.1. Literature Search
The five-step approach presented by Arksey and O’Malley [18], and advanced by Levac and collaborators [19] was utilized in the following scoping review. The foreseen steps were: 1. determining the study problem, 2. outlining relevant investigations, 3. studies selection, 4. data charting, 5. collating, summarization, and presenting the findings.
The choice of a scoping review was based on the need to identify the nature and extent of the research evidence in accordance with Grant et al. [20].
The study was conducted according to the Preferred Reporting Item for Systematic Review and Meta-analysis for Scoping Review (PRISMA-ScR) [21] (Supplementary Table S1).
2.2. Step 1: Determining the Study Problem
The objectives of the review were to provide answers to the following questions:
- What is the prevalence of malnutrition in older patients with cognitive impairment?
- What are the risk factors for developing low food intake in hospitalized older patients with cognitive impairment?
- Which nursing strategies are used to enhance clinical outcomes and patients with cognitive impairment care in the hospital environments?
The PCCT (population, concept, context, and type of study) methodology was utilized to identify search questions according to Peters et al. [22]. Specifically, the population included hospitalized elderly patients (aged > 65 years) with cognitive impairment and malnutrition. The concept was prevalence of phenomenon, nursing health interventions aimed at recognizing, reducing the risk of malnutrition, and positively affecting this phenomenon. The context was health care services admitting older people with cognitive impairment. With regards to type of study, all observational, experimental, and quasi-experimental studies with available full text in English, Spanish, and Italian were included.
2.3. Step 2: Outlining Relevant Investigations
A systematic search was conducted on the following scientific databases: PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Psychological Abstracts Information Services (PsycINFO), Scopus, and National Library of Medicine (MEDLINE) via EBSCO and Cochrane Library. Observational, experimental, and quasi-experimental studies on malnourished elderly inpatients (>65 years) with cognitive impairment (including dementia and Alzheimer’s disease) in English, Spanish, and Italian were included. Studies involving people living at home and the adult and pediatric population (<65 years old) were excluded. No limits for country of origin or geographical context were applied. No time limits were applied.
2.4. Step 3: Study Selection
Citations were imported into Zotero® Reference Manager, and the duplicates were eliminated. Two independent researchers conducted the initial screening, from March 2022 to May 2022, by reading the titles and abstracts of the publications. Unrelated studies were removed. If the publication’s relevance was undefined based on the title or abstract reading, the reviewers read the paper in full text to determine its eligibility.
The same investigators retrieved and assessed the whole text of articles deemed eligible for inclusion criteria. Any disagreement was resolved by discussion and final consensus. When the latter was not reached, arbitration was sought from a third researcher who supervised the study.
2.5. Step 4: Data Charting
The selected articles were summarized in Table 1 [23,24,25,26,27,28,29,30,31], including authors and year, aim, method, and main results.

Table 1.
Summary of findings.
2.6. Step 5: Collating, Summarization, and Presenting the Findings
Lastly, the results were collated and summarized according to Arksey and O’Malley’s framework [18], respecting the proposed search strategy.
3. Results
The search strategy yielded 638 articles; 142 duplicates were excluded. A further 421 records were excluded after applying the title and abstract eligibility criteria. The full texts of 75 articles were reviewed. Of these, nine articles met the inclusion criteria and were included in this scoping review [23,24,25,26,27,28,29,30,31]. Figure 1 shows the search and selection process according to the PRISMA statement [21]. (Figure 1).
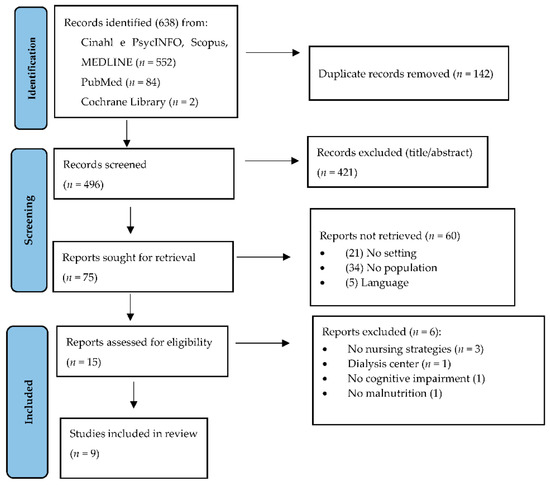
Figure 1.
Flow diagram of the search and selection process, based on PRISMA flowchart.
The relationship between older people’s nutritional status, hospitalization, and cognitive impairment as a result of the included studies is shown in Table 1 and in the Supplementary Material Table S1.
According to the scoping review framework, the main themes were divided into two results sections.
3.1. Prevalence and Risk Factors of Malnutrition in Older Patients with Cognitive Impairment
Orsitto et al. [23] described an extremely high prevalence of poor nutritional status in a sample of hospitalized older patients with different grades of cognitive impairment. Only 18% of the sample was well nourished, while 82% were at risk of malnutrition or malnourished. Findings showed a significantly greater malnutrition rate in hospitalized patients with severe cognitive impairment. This study showed the evidence of poor nutritional status even in patients with mild cognitive impairment who had not yet progressed to dementia [23]. Moreover, according to Salva et al. [28] patients with dementia showed a high risk of malnutrition with respect to other patients. According to Lin et al. [29], eating difficulty, no feeding assistance, moderate dependence, fewer family visits, and being female and older were six independent factors associated with low food intake after controlling for all other aspects [29].
Hospitalized frail patients develop a major risk of under-nutrition and weight loss [23,25]. However, according to the findings of another study [25] there are no differences in malnutrition among different groups of hospitalized patients concerning age, length of stay, gender, or baseline anthropometric scores.
3.2. Nursing Strategies Used to Enhance Clinical Outcomes
Simple, inexpensive, and easy-to-implement strategies, such as early dietary assessment; dietary “grazing” and staggered mealtimes, can improve nutrition in hospitalized elderly patients [25]. Nursing strategies that provide information on the clinical, functional, and cognitive aspects of the disease should be used in hospitalized patients, especially those with cognitive impairment [25]. The immediate evaluation of eating abilities, nutritional needs, and dietary preferences is a simple and inexpensive strategy that can lead to positive changes in nutritional intake in this population [25,31]. Indeed, assessing the patient’s nutritional needs early is critical to reducing hospitalization [24], as it improves the patient’s weight, but this does not affect cognitive impairment [25]. A positive element emerges from the study of Avelino-Silva et al.: hospitalization, by allowing more time to assess each patient, provides the opportunity for a detailed and structured nutritional clinical assessment through a CGA tool that has proven useful in reducing mortality in these patients [24]. Other tools have been used in order to evaluate nutritional status, for instance, Salva et al. used the mini nutritional assessment scale [28].
Some studies have also shown other strategies to enhance the nutritional outcome in patients with cognitive impairment. For example, the main objective of Lauque et al. [26] was to evaluate the effects of OS. Overall, 46 patients (intervention group) received 3-month OS, while the other 45 patients (control group) received standard care in geriatric wards and daycare centers in the Toulouse region. Protein and energy consumption considerably increased in the intervention group between baseline and 3 months, leading to a considerable gain in weight as well as fat-free mass. Nevertheless, no substantial changes in biological markers, cognitive function, or dependence were observed. Therefore, the authors conclude that the regular OS assumption can aid in preserving the gain in fat-free mass and enhance these individuals’ nutritional status. Additionally, a study conducted by Allen et al. [30] showed that supplement drinks may be beneficial in reducing the prevalence of malnutrition within the group, as more people meet their nutritional requirements. Moreover, another study by Allien et al. [27] showed that drinking nutritional beverages with a glass makes the patient more stimulated to drink rather than using a straw. Baumgartner et al. [31] found that individualized nutritional support improves functional outcomes and quality of life (QoL) over 30- and 180-day periods of nutritional support.
Finally, if nurses take the time to assess the nutritional status and needs, implement suitable care plans and provide food and drink in ways that ensure their safe consumption, this can positively affect both patients’ nutritional status and their general health condition, reducing the risk of mortality too [28,29,30,31].
4. Discussion
4.1. Nutritional Assessment and Screening
Malnutrition has a high prevalence in hospitalized elderly patients [25,26]. This review confirms that the potential associated factors are different: medical history, medicines intakes, diet, oral health, swallowing ability, physical and cognitive function, gastrointestinal, psychiatric, and neurological conditions, and also social aspects of a person’s life [24]. Therefore, every hospital should establish an interdisciplinary approach to nutrition care based on formal policies and procedures, ensuring the early identification of malnourished patients or malnutrition risk and implementing comprehensive nutrition care plans [24]. In fact, the review results suggest that patients should be screened for malnutrition within the first 24 h of admission and screened regularly during their hospital stay [23,24]. Moreover, it is critically important to establish individualized nutritional support to these patients, as this improves functional outcomes and QoL, as well as reducing mortality by 50% at 30 days in hospitalized elderly patients [31].
The MNA has become a tool allowed standardized, reproducible, and reliable determination of nutritional status [26,31]. However, some studies reported that the MNA-SF (mini nutritional assessment short-form) could overestimate malnutrition risk [28].
Avoiding and solving malnutrition in elderly individuals is a crucial element of geriatric care, since healthy people can also become malnourished during hospitalization. In this context, early dietary assessment and implementation of feeding strategies are crucial not only for vulnerable patients [25].
4.2. Nutritional Strategies and Management
Breaking the vicious circle between malnutrition and cognitive impairment can help patients and reduce the impact of this degenerative condition [25,28].
The management of elderly adults who are malnourished or at malnutrition risk should be multimodal and multidisciplinary, as reported by Salva et al. in their nutritional intervention program, “The NutriAlz”, aimed at preventing weight loss patients affected by dementia [28].
A routine and impersonalized hospital nutrition in elderly patients carries an increased risk of mortality compared with individualized nutritional support [31]. Especially, patients with dementia and cognitive impairment hospitalized for acute diseases often require individualized strategies to maintain adequate caloric intake.
Moreover, eating difficulties is a factor associated with low food intake [29]. Therefore, attention must be paid to oral frailty, defined as a gradual age-related loss of oral function along with decline in cognitive and physical function [32]. In addition, altered eating behavior and dysphagia are factors to be managed in these frail hospitalized patients [26]. These patients have impaired oral motor skills, particularly chewing function, oral diadochokinesis, swallowing and salivary disorders, all associated with few teeth left in the oral cavity [29,32].
4.3. Environmental Changes to Improve Mealtime Habitat and Experience
Environmental elements such as food accessibility (for example a glass door refrigerator with snack food easily visible), companions and furniture, smell, ambient sounds, lighting and temperature, size of the portion, eating location, and presentation of food play a crucial role during mealtimes, improving the patients’ compliance to eat [25]. It is demonstrated that changes in mealtime habits and atmosphere, based on the personal needs of patients, could increase nutritional intake and reduce the malnutrition risk [25,29], especially among older people.
A great variety of environmental variables might have an influence on the nutritional intake of elderly inpatients as also reported in the review findings [25,30]. Wong, et al. have shown that appetite increased if those people needing more assistance were fed earlier than other patients; it is not the time of meal initiation that is important, but the longer duration [25]. To reduce the prevalence of malnutrition in these patients, it is useful to offer supplementary drinks, as they can improve oral intake and increase appetite [30]. Another environmental change to improve mealtime habitats is music. Wong et al. have shown that patients spent more time at the table when music was played, so it appears to be an effective strategy to lengthen mealtime and increase patients’ appetite [25].
Family style meals, eating meals with caregivers, relaxing music during mealtime, patient education, protected mealtimes, and additional food assistance (implemented alone or in combination) were among the most promising interventions to improve mealtime experiences [25,29,30]. It is crucial that these fragile patients receive support from nurses or family members at mealtimes [25]. This relational strategy helps the patient to increase food intake during meals [29]. Receiving good mealtime assistance and increasing time spent by nurses or volunteers on feeding or helping during meals may positively affect eating behavior with a positive effect on the nutritional intake in older inpatients [27,29].
The physical presence of a caregiver helps the patient to be more focused on his or her meal [25,29]. Caregiver education is crucial to ensure proper weight maintenance for the patient who may go through weight loss even if they have a positive energy balance [26].
4.4. Limits of the Study
This scoping review focused only on the relationship between nursing activities and identification, prevention, and management of cognitive impairment in elderly hospitalized individuals, and the main limitation is the reduced availability of studies in the hospital environment. The majority of published studies recruited patients in the home setting. Hospitalization is usually due to further acute illnesses; therefore, general conditions and eventually chronic diseases associated with acute events worsen. Moreover, in this study, we could not take into consideration the intensity of care, including some invasive treatments such as intravenous or enteral support. Finally, we could not stratify nursing activities considering the cause of cognitive impairment, its worsening, its stage, or the duration of the cognitive impairment.
5. Conclusions
The findings of this scoping review suggest that malnutrition may have high frequency in hospitalized elderly patients, especially those affected by cognitive impairment. The relationship between nutritional status and cognitive impairment is complex and reciprocal. Therefore, an appropriate nutritional status evaluation along the hospitalization, followed by both healthcare and environmental managing strategies is necessary to maintain or improve the patients’ nutritional status. A multidisciplinary team is essential to fulfilling the nutritional needs of these patients, and the role of nursing activities is crucial.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14194036/s1, Table S1: Summary of findings.
Author Contributions
Conceptualization, M.D.M., G.B.O. and C.N.; methodology, S.D., E.D.S., V.D., and N.G.; data collection: F.R., V.D., G.L., F.F. and A.D.L.; original draft preparation, G.L., C.N. and R.M.A.; writing—review and editing, E.D.S., D.D.N., C.N. and N.G.; supervision, M.D.M., G.B.O. and C.N.; project administration, M.D.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Scotellaro, M.; Ruggeri, M.; D’inzeo, V.; Di Simone, E.; Di Muzio, M.; Dionisi, S.; Giannetta, N. Multidimensional assessment using a modified S.Va.M.A scale, a pilot study in patients aged 65 or older. J. Gerontol. Geriatr. 2021, 69, 171–176. [Google Scholar] [CrossRef]
- Di Muzio, M.; Rosa, F.; Moriconi, A. Nutrition in dementia: A challenge for nurses. Prog. Nutr. 2018, 20, 5–11. [Google Scholar] [CrossRef]
- Prince, M.J.; Wu, F.; Guo, Y.; Gutierrez Robledo, L.M.; O’Donnell, M.; Sullivan, R.; Yusuf, S. The burden of disease in older people and implications for health policy and practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef]
- Giraldi, G.; Montesano, M.; Napoli, C.; Frati, P.; La Russa, R.; Santurro, A.; Scopetti, M.; Orsi, G.B. Healthcare-Associated Infections Due to Multidrug-Resistant Organisms: A Surveillance Study on Extra Hospital Stay and Direct Costs. Curr. Pharm. Biotechnol. 2019, 20, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Park, J.E.; Baik, H.W. Aging and Nutrition. J. Korean Soc. Parenter. Enter. Nutr. 2013, 5, 42–49. [Google Scholar] [CrossRef]
- Zupo, R.; Castellana, F.; Guerra, V.; Donghia, R.; Bortone, I.; Griseta, C.; Lampignano, L.; Dibello, V.; Lozupone, M.; Coelho-Jùnior, H.J.; et al. Associations between nutritional frailty and 8-year all-cause mortality in older adults: The Salus in Apulia Study. J. Intern. Med. 2021, 290, 1071–1082. [Google Scholar] [CrossRef]
- Di Simone, E.; Giannetta, N.; Gazzelloni, A.; Torre, R.; Livadiotti, J.; Dionisi, S.; Di Muzio, F.; Montesano, M.; Moriconi, A.; Fabbian, F.; et al. Nutrition in patients with unilateral neglect. Prog. Nutr. 2020, 22, e2020001. [Google Scholar] [CrossRef]
- Zupo, R.; Castellana, F.; Bortone, I.; Griseta, C.; Sardone, R.; Lampignano, L.; Lozupone, M.; Solfrizzi, V.; Castellana, M.; Giannelli, G.; et al. Nutritional domains in frailty tools: Working towards an operational definition of nutritional frailty. Ageing Res. Rev. 2020, 64, 101148. [Google Scholar] [CrossRef]
- Agarwal, E.; Miller, M.; Yaxley, A.; Isenring, E. Malnutrition in the elderly: A narrative review. Maturitas 2013, 76, 296–302. [Google Scholar] [CrossRef]
- Kirkland, L.L.; Kashiwagi, D.T.; Brantley, S.; Scheurer, D.; Varkey, P. Nutrition in the hospitalised patient. J. Hosp. Med. 2013, 8, 52–58. [Google Scholar] [CrossRef]
- Correia, M.; Hegazi, R.; Higashiguchi, T.; Michel, J.; Reddy, B.; Tappenden, K.; Uyar, M.; Muscaritoli, M. Evidence-based recommendations for addressing malnutrition in health care: An updated strategy from feed ME. Glob. Study Group JAMDA 2014, 15, 544–550. [Google Scholar]
- Di Stefano, V.; Rispoli, M.G.; Pellegrino, N.; Graziosi, A.; Rotondo, E.; Napoli, C.; Pietrobon, D.; Brighina, F.; Parisi, P. Diagnostic and therapeutic aspects of hemiplegic migraine. J. Neurol. Neurosurg. Psychiatry 2020, 91, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Shlisky, J.; Bloom, D.E.; Beaudreault, A.R.; Tucker, K.L.; Keller, H.H.; Freund-Levi, Y.; Fielding, R.A.; Cheng, F.W.; Jensen, G.L.; Wu, D.; et al. Nutritional Considerations for Healthy Aging and Reduction in Age-Related Chronic Disease. Adv. Nutr. 2017, 8, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.N.; Cheng, Y.; Chen, L.K.; Tung, H.H.; Chu, K.H.; Liang, S.Y. Cognition and social-physiological factors associated with malnutrition in hospitalised older adults in Taiwan. J. Nurs. Res. 2015, 23, 1–5. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mudge, A.M.; Ross, L.J.; Young, A.M.; Isenring, E.A.; Banks, M.D. Helping understand nutritional gaps in the elderly (HUNGER): A prospective study of patient factors associated with inadequate nutritional intake in older medical inpatients. Clin. Nutr. 2011, 30, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Del Parigi, A.; Panza, F.; Capurso, C.; Solfrizzi, V. Nutritional factors, cognitive decline, and dementia. Brain Res. Bull. 2006, 69, 1–19. [Google Scholar] [CrossRef]
- De Giorgi, A.; Di Simone, E.; Cappadona, R.; Boari, B.; Savriè, C.; López-Soto, P.J.; Rodríguez-Borrego, M.A.; Gallerani, M.; Manfredini, R.; Fabbian, F. Validation and Comparison of a Modified Elixhauser Index for Predicting In-Hospital Mortality in Italian Internal Medicine Wards. Risk Manag. Healthc. Policy 2020, 13, 443–451. [Google Scholar] [CrossRef]
- Arksey, H.; & O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 24 September 2022). [CrossRef]
- Orsitto, G.; Fulvio, F.; Tria, D.; Turi, V.; Venezia, A.; Manca, C. Nutritional status in hospitalised elderly patients with mild cognitive impairment. Clin. Nutr. 2009, 28, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Avelino-Silva, T.J.; Farfel, J.M.; Curiati, J.A.; Amaral, J.R.; Campora, F.; Jacob-Filho, W. Comprehensive geriatric assessment predicts mortality and adverse outcomes in hospitalised older adults. BMC Geriatr. 2014, 14, 129. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.; Burford, S.; Wyles, C.L.; Mundy, H.; Sainsbury, R. Evaluation of strategies to improve nutrition in people with dementia in an assessment unit. J. Nutr. Health Aging 2008, 12, 309–312. [Google Scholar] [CrossRef]
- Lauque, S.; Arnaud-Battandier, F.; Gillette, S.; Plaze, J.M.; Andrieu, S.; Cantet, C.; Vellas, B. Improvement of weight and fat-free mass with oral nutritional supplementation in patients with Alzheimer’s disease at risk of malnutrition: A prospective randomised study. J Am Geriatr. Soc. 2004, 52, 1702–1707. [Google Scholar] [CrossRef] [PubMed]
- Allen, V.J.; Methven, L.; Gosney, M. Impact of serving method on the consumption of nutritional supplement drinks: Randomised trial in older adults with cognitive impairment. J. Adv. Nurs. 2014, 70, 1323–1333. [Google Scholar] [CrossRef] [PubMed]
- Salva, A.; Andrieu, S.; Fernandez, E.; Schiffrin, E.J.; Moulin, J.; Decarli, B.; Guigoz, Y.; Vellas, B.; NutriAlz Group. Health and nutritional promotion program for patients with dementia (NutriAlz Study): Design and baseline data. J. Nutr. Health Aging 2009, 13, 529–537. [Google Scholar] [CrossRef]
- Lin, L.C.; Watson, R.; Wu, S.C. What is associated with low food intake in older people with dementia? J. Clin. Nurs. 2010, 19, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Allen, V.; Methven, L.; Gosney, M. The influence of nutritional supplement drinks on providing adequate calorie and protein intake in older adults with dementia. J. Nutr. Health Aging 2013, 17, 752–755. [Google Scholar] [CrossRef]
- Baumgartner, A.; Pachnis, D.; Parra, L.; Hersberger, L.; Bargetzi, A.; Bargetzi, L.; Kaegi-Braun, N.; Tribolet, P.; Gomes, F.; Hoess, C.; et al. The impact of nutritional support on malnourished inpatients with aging-related vulnerability. Nutrition 2021, 89, 111279. [Google Scholar] [CrossRef]
- Dibello, V.; Zupo, R.; Sardone, R.; Lozupone, M.; Castellana, F.; Dibello, A.; Daniele, A.; De Pergola, G.; Bortone, I.; Lampignano, L.; et al. Oral frailty and its determinants in older age: A systematic review. Lancet Healthy Longev. 2021, 2, e507–e520. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).