The Risk of Cardiovascular Disease According to Chewing Status Could Be Modulated by Healthy Diet in Middle-Aged Koreans
Abstract
:1. Introduction
2. Subjects and Methods
2.1. Data Resources and Subjects Selects
2.2. Measurements
2.2.1. Chewing Status
2.2.2. Sociodemographic Characteristics
2.2.3. Korean Health Eating Index
2.2.4. Factors of Cardiovascular Disease Risk (CVD) and Definitions of 10-Year Estimated CVD Risk
2.3. Statistical Analyses
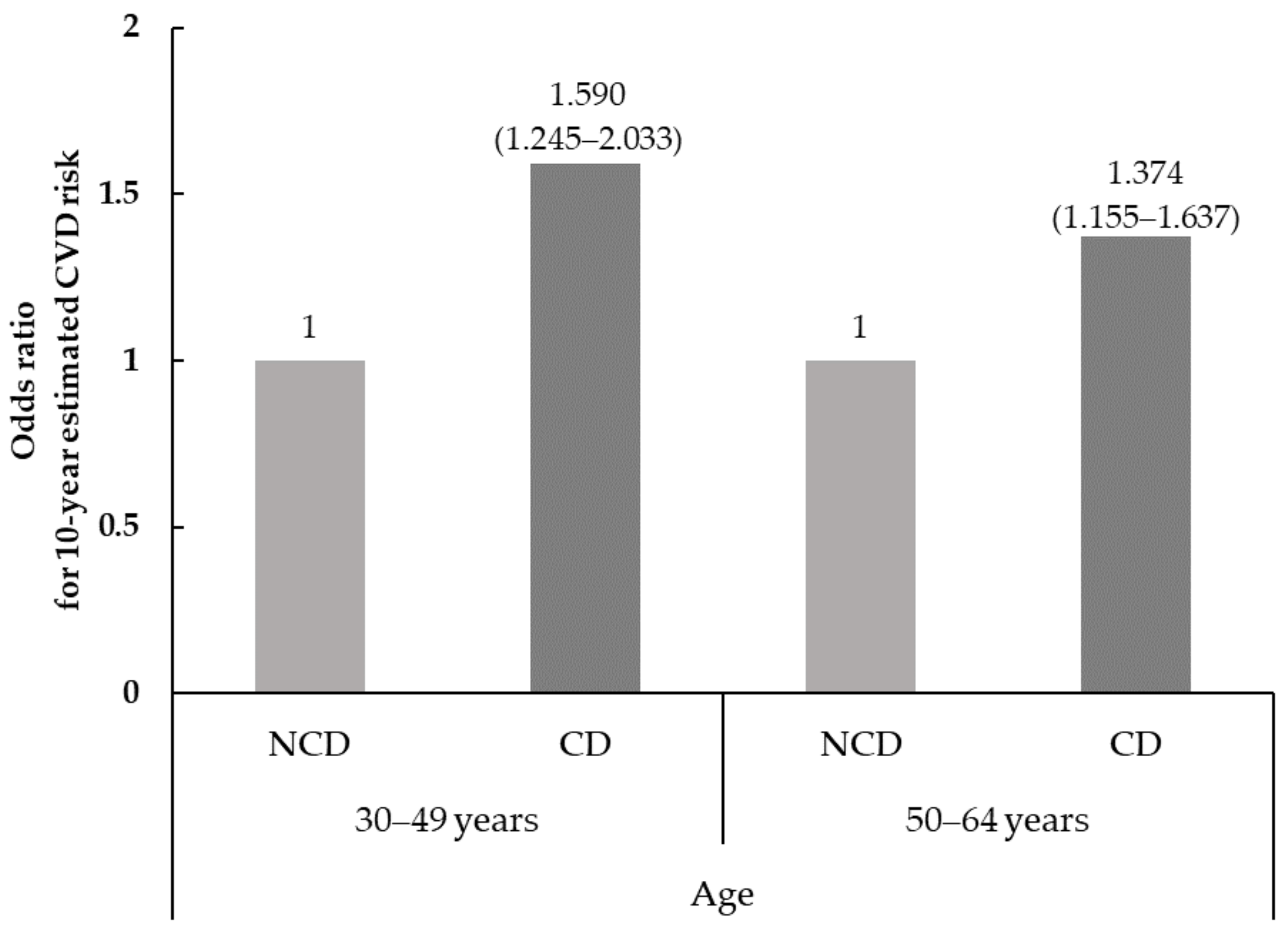
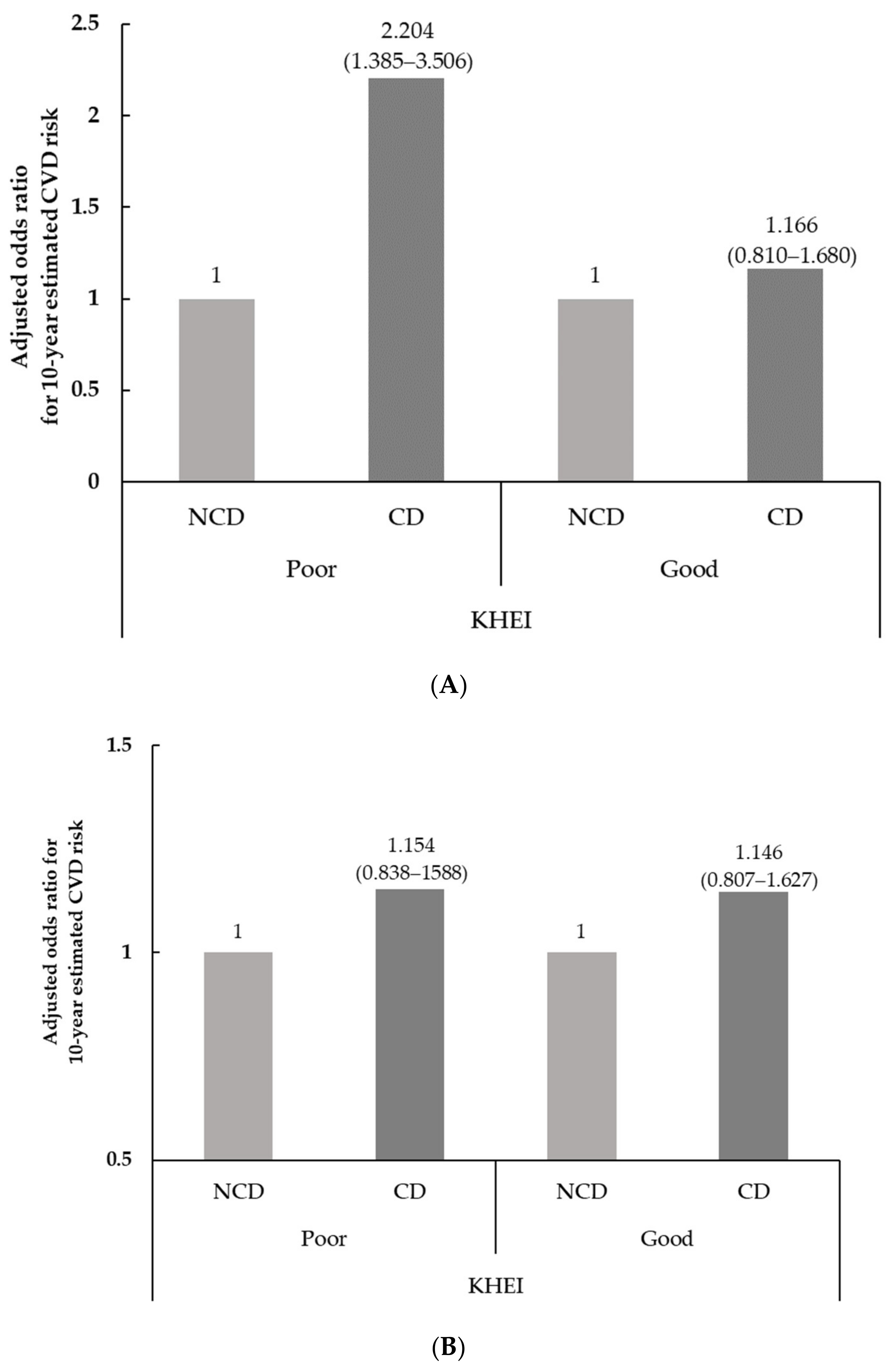
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Available online: https://www.who.int/ (accessed on 10 August 2022).
- Korean Statistical Information Service. Available online: http://kostat.go.kr (accessed on 10 August 2022).
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.M.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef]
- D'Agostino, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- Goff, D.C.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129, S49–S73. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, A.H.; Appel, L.J.; Vadiveloo, M.; Hu, F.B.; Kris-Etherton, P.M.; Rebholz, C.M.; Sacks, F.M.; Thorndike, A.N.; Van Horn, L.; Wylie-Rosett, J.; et al. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement from the American Heart Association. Circulation 2021, 144, e472–e487. [Google Scholar] [CrossRef] [PubMed]
- Chareonrungrueangchai, K.; Wongkawinwoot, K.; Anothaisintawee, T.; Reutrakul, S. Dietary Factors and Risks of Cardiovascular Diseases: An Umbrella Review. Nutrients 2020, 12, 1088. [Google Scholar] [CrossRef] [PubMed]
- Alexander, R.M. Engineering approaches to chewing and digestion. Sci. Prog. 1999, 82, 171–184. [Google Scholar] [CrossRef]
- Aoyama, N.; Fujii, T.; Kida, S.; Nozawa, I.; Taniguchi, K.; Fujiwara, M.; Iwane, T.; Tamaki, K.; Minabe, M. Association of Periodontal Status, Number of Teeth, and Obesity: A Cross-Sectional Study in Japan. J. Clin. Med. 2021, 10, 208. [Google Scholar] [CrossRef]
- Maruyama, K.; Nishioka, S.; Miyoshi, N.; Higuchi, K.; Mori, H.; Tanno, S.; Tomooka, K.; Eguchi, E.; Furukawa, S.; Saito, I.; et al. The impact of masticatory ability as evaluated by salivary flow rates on obesity in Japanese: The Toon health study. Obesity 2015, 23, 1296–1302. [Google Scholar] [CrossRef]
- Iwasaki, T.; Fukuda, H.; Kitamura, M.; Kawashita, Y.; Hayashida, H.; Furugen, R.; Koyama, Z.; Ando, Y.; Saito, T. Association between number of pairs of opposing posterior teeth, metabolic syndrome, and obesity. Odontology 2018, 107, 111–117. [Google Scholar] [CrossRef]
- Nakamura, T.; Zou, K.; Shibuya, Y.; Michikawa, M. Oral dysfunctions and cognitive impairment/dementia. J. Neurosci. Res. 2020, 99, 518–528. [Google Scholar] [CrossRef]
- Kim, E.-K.; Lee, S.K.; Choi, Y.-H.; Tanaka, M.; Hirotsu, K.; Kim, H.C.; Lee, H.-K.; Jung, Y.-S.; Amano, A. Relationship between chewing ability and cognitive impairment in the rural elderly. Arch. Gerontol. Geriatr. 2017, 70, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Rangé, H.; Perier, M.-C.; Boillot, A.; Offredo, L.; Lisan, Q.; Guibout, C.; Thomas, F.; Danchin, N.; Boutouyrie, P.; Jouven, X.; et al. Chewing capacity and ideal cardiovascular health in adulthood: A cross-sectional analysis of a population-based cohort study. Clin. Nutr. 2019, 39, 1440–1446. [Google Scholar] [CrossRef] [PubMed]
- Schwahn, C.; Polzer, I.; Haring, R.; Dörr, M.; Wallaschofski, H.; Kocher, T.; Mundt, T.; Holtfreter, B.; Samietz, S.; Völzke, H.; et al. Missing, unreplaced teeth and risk of all-cause and cardiovascular mortality. Int. J. Cardiol. 2012, 167, 1430–1437. [Google Scholar] [CrossRef] [PubMed]
- Motokawa, K.; Mikami, Y.; Shirobe, M.; Edahiro, A.; Ohara, Y.; Iwasaki, M.; Watanabe, Y.; Kawai, H.; Kera, T.; Obuchi, S.; et al. Relationship between Chewing Ability and Nutritional Status in Japanese Older Adults: A Cross-Sectional Study. Int. J. Environ. Res. Public Heal. 2021, 18, 1216. [Google Scholar] [CrossRef]
- Cupples, L.A.; D’Agostino, R.B. Section 34: Some risk factors related to the annual incidence of cardiovascular disease and death in pooled repeated biennial measurements. In Framingham Heart Study: 30 Year Follow-Up; Kannel, W.B., Wolf, P.A., Garrison, R.J., Eds.; US Department of Health and Human Services: Bethesda, MD, USA, 1987. [Google Scholar]
- Yun, S.; Park, S.; Yook, S.M.; Kim, K.; Shim, J.E.; Hwang, J.Y.; Oh, K. Development of the Korean Healthy Eating Index for adults, based on the Korea National Health and Nutrition Examination Survey. Nutr. Res. Pract. 2022, 16, 233–247. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare. The Korean National Health and Nutrition Examination Survey (KNHANES). Available online: http://knhanes.cdc.go.kr (accessed on 10 June 2022).
- Chun, H.; Doo, M. Factors Related to Depression Associated with Chewing Problems in the Korean Elderly Population. Int. J. Environ. Res. Public Health 2021, 18, 6158. [Google Scholar] [CrossRef]
- Anderson, T.J.; Grégoire, J.; Pearson, G.J.; Barry, A.R.; Couture, P.; Dawes, M.; Francis, G.A.; Genest, J.; Grover, S.; Gupta, M.; et al. 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can. J. Cardiol. 2016, 32, 1263–1282. [Google Scholar] [CrossRef]
- Locker, D. Changes in chewing ability with ageing: A 7-year study of older adults. J. Oral Rehabil. 2002, 29, 1021–1029. [Google Scholar] [CrossRef]
- Woo, J.; Tong, C.; Yu, R. Chewing Difficulty Should be Included as a Geriatric Syndrome. Nutrients 2018, 10, 1997. [Google Scholar] [CrossRef]
- Laudisio, A.; Milaneschi, Y.; Bandinelli, S.; Gemma, A.; Ferrucci, L.; Incalzi, R.A. Chewing problems are associated with depression in the elderly: Results from the InCHIANTI study. Int. J. Geriatr. Psychiatry 2013, 29, 236–244. [Google Scholar] [CrossRef]
- Darnaud, C.; Thomas, F.; Pannier, B.; Danchin, N.; Bouchard, P. Oral Health and Blood Pressure: The IPC Cohort. Am. J. Hypertens. 2015, 28, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.H.; Moon, M.K.; Oh, S.; Koo, B.K.; Cho, N.H.; Lee, M.-K. Validation of Risk Prediction Models for Atherosclerotic Cardiovascular Disease in a Prospective Korean Community-Based Cohort. Diabetes Metab. J. 2020, 44, 458–469. [Google Scholar] [CrossRef] [PubMed]
| Risk Factors | β | P Value | HR | 95% CI |
|---|---|---|---|---|
| Men | ||||
| Log of Age | 3.06117 | <0.001 | 21.35 | (14.03–32.48) |
| Log of total cholesterol | 1.12370 | <0.001 | 3.08 | (2.05–4.62) |
| Log of HDL cholesterol | −0.93263 | <0.001 | 0.39 | (0.30–0.52) |
| Log of SBP if not treated | 1.93303 | <0.001 | 6.91 | (3.91–12.20) |
| Log of SBP if treated | 1.99881 | <0.001 | 7.38 | (4.22–12.92) |
| Smoking status | 0.65451 | <0.001 | 1.92 | (1.65–2.24) |
| Diabetes mellitus | 0.57367 | <0.001 | 1.78 | (1.43–2.20) |
| Women | ||||
| Log of Age | 2.32888 | <0.001 | 10.27 | (5.65–18.64) |
| Log of total cholesterol | 1.20904 | <0.001 | 3.35 | (2.00–5.62) |
| Log of HDL cholesterol | −0.70833 | <0.001 | 0.49 | (0.35–0.69) |
| Log of SBP if not treated | 2.76157 | <0.001 | 15.82 | (7.86–31.87) |
| Log of SBP if treated | 2.82263 | <0.001 | 16.82 | (8.46–33.46) |
| Smoking status | 0.52873 | <0.001 | 1.70 | (1.40–2.06) |
| Diabetes mellitus | 0.69154 | <0.001 | 2.00 | (1.49–2.67) |
| 30~49 Years (n = 5159) | 50~64 Years (n = 4252) | |||||
|---|---|---|---|---|---|---|
| CD (n = 541) | NCD (n = 4618) | p Value * | CD (n = 1129) | NCD (n = 3123) | p Value * | |
| Gender, men | 55.5 (2.3) | 50.0 (0.7) | 0.044 | 53.0 (1.6) | 47.7 (1.0) | 0.008 |
| Education level, ≥high school | 9.9 (0.5) | 90.1 (0.5) | <0.001 | 20.5 (0.9) | 79.5 (0.9) | <0.001 |
| Household income, high | 58.0 (2.5) | 72.2 (1.0) | <0.001 | 57.2 (1.9) | 70.8 (1.2) | <0.001 |
| Regular drinker, yes | 67.5 (2.5) | 66.6 (0.8) | 0.737 | 56.9 (1.7) | 53.7 (1.0) | 0.106 |
| Aerobic physical activity, yes | 44.9 (2.6) | 49.5 (0.9) | 0.102 | 37.5 (1.8) | 44.4 (1.1) | 0.001 |
| Perceived stress, low | 60.7 (2.3) | 70.3 (0.8) | <0.001 | 67.8 (1.7) | 79.5 (0.9) | <0.001 |
| 30~49 Years (n = 5159) | 50~64 Year (n = 4252) | |||||
|---|---|---|---|---|---|---|
| CD | NCD | p Value * | CD | NCD | p Value * | |
| (n = 541) | (n = 4618) | (n = 1129) | (n = 3123) | |||
| Age, year | 41.54 (40.99–42.10) | 39.84 (39.61–40.07) | <0.001 | 56.99 (56.70–57.29) | 56.19 (56.00–56.37) | <0.001 |
| TC, mg/dL | 193.00 (189.81–196.19) | 196.83 (195.60–198.05) | 0.026 | 198.53 (195.75–201.30) | 199.60 (197.89–201.30) | 0.504 |
| HDL-C, mg/dL | 50.22 (49.05–51.40) | 51.85 (51.41–52.29) | 0.013 | 50.37 (49.44–51.29) | 50.69 (50.12–51.26) | 0.562 |
| SBP, mmHg | 114.04 (112.60–115.47) | 113.24 (112.71–113.76) | 0.279 | 122.52 (121.29–123.76) | 120.55 (119.84–121.26) | 0.006 |
| BP treatment, % | 5.3 (1.1) | 4.6 (0.4) | 0.517 | 25.3 (1.6) | 24.1 (0.8) | 0.503 |
| Smoking status, % | 36.4 (2.5) | 23.0 (0.8) | <0.001 | 29.2 (1.8) | 17.3 (0.9) | <0.001 |
| DM diagnosis, % | 2.3 (0.7) | 2.0 (0.2) | 0.690 | 12.1 (1.2) | 9.9 (0.6) | 0.093 |
| 10-year estimated CVD risk, % | 8.71 (7.54–9.87) | 6.84 (6.46–7.22) | 0.003 | 30.38 (28.12–32.65) | 26.42 (25.31–27.54) | 0.003 |
| Intermediate/high for CVD risk ** | 23.1 (2.1) | 15.9 (0.6) | <0.001 | 65.4 (1.7) | 57.9 (1.0) | 0.002 |
| Scoring | 30~49 Years (n = 5159) | 50~64 Years (n = 4252) | |||||
|---|---|---|---|---|---|---|---|
| CD (n = 541) | NCD (n = 4618) | p Value * | CD (n = 1129) | NCD (n = 3123) | p Value * | ||
| Have breakfast | 0–10 | 5.98 (5.55–6.41) | 6.26 (6.10–6.42) | 0.217 | 8.07 (7.83–8.31) | 8.40 (8.25–8.55) | 0.019 |
| Mixed grains intake | 0–5 | 1.56 (1.37–1.74) | 1.65 (1.58–1.73) | 0.318 | 2.15 (2.00–2.30) | 2.29 (2.19–2.38) | 0.105 |
| Total fruits intake | 0–5 | 1.55 (1.34–1.76) | 1.96 (1.88–2.04) | <0.001 | 2.33 (2.17–2.49) | 2.75 (2.65–2.85) | <0.001 |
| Fresh fruits intake | 0–5 | 1.66 (1.43–1.90) | 2.20 (2.11–2.29) | <0.001 | 2.62 (2.45–2.79) | 2.99 (2.88–3.09) | <0.001 |
| Total vegetables intake | 0–5 | 3.52 (3.38–3.66) | 3.50 (3.45–3.55) | 0.803 | 3.60 (3.49–3.72) | 3.80 (3.74–3.87) | 0.002 |
| Vegetables intake excluding Kimchi and pickled vegetables intake | 0–5 | 3.14 (2.98–3.31) | 3.22 (3.16–3.27) | 0.416 | 3.19 (3.07–3.32) | 3.44 (3.37–3.51) | <0.001 |
| Meat, fish, eggs and beans intake | 0–10 | 7.14 (6.84–7.45) | 7.59 (7.49–7.69) | 0.006 | 6.31 (6.08–6.54) | 7.02 (6.88–7.16) | <0.001 |
| Milk and milk products intake | 0–10 | 3.20 (2.75–3.64) | 3.34 (3.19–3.50) | 0.535 | 3.00 (2.68–3.31) | 3.37 (3.16–3.58) | 0.043 |
| Percentage of energy from saturated fatty acid | 0–10 | 6.79 (6.39–7.19) | 6.78 (6.64–6.93) | 0.957 | 8.37 (8.15–8.59) | 8.08 (7.92–8.23) | 0.029 |
| Sodium intake | 0–10 | 6.32 (6.00–6.64) | 6.31 (6.19–6.43) | 0.946 | 6.97 (6.71–7.22) | 6.68 (6.53–6.82) | 0.050 |
| Percentage of energy from Sweets and beverages | 0–10 | 9.08 (8.99–9.16) | 8.82 (8.54–9.10) | 0.079 | 9.29 (9.15–9.44) | 9.44 (9.37–9.52) | 0.066 |
| Percentage of energy from carbohydrate | 0–5 | 2.95 (2.75–3.16) | 2.91 (2.85–2.99) | 0.696 | 2.30 (2.15–2.45) | 2.46 (2.38–2.55) | 0.068 |
| Percentage of energy from fat | 0–5 | 3.70 (3.51–3.90) | 3.68 (3.61–3.75) | 0.851 | 3.26 (3.11–3.41) | 3.41 (3.32–3.50) | 0.093 |
| Energy Intake | 0–5 | 3.09 (2.89–3.29) | 3.16 (3.09–3.23) | 0.518 | 3.12 (2.96–3.27) | 3.16 (3.07–3.25) | 0.568 |
| Total score of KHEI | 59.42 (57.98–60.87) | 61.64 (61.13–62.14) | 0.004 | 64.56 (63.63–65.50) | 67.29 (66.71–67.87) | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chun, H.; Oh, J.; Doo, M. The Risk of Cardiovascular Disease According to Chewing Status Could Be Modulated by Healthy Diet in Middle-Aged Koreans. Nutrients 2022, 14, 3849. https://doi.org/10.3390/nu14183849
Chun H, Oh J, Doo M. The Risk of Cardiovascular Disease According to Chewing Status Could Be Modulated by Healthy Diet in Middle-Aged Koreans. Nutrients. 2022; 14(18):3849. https://doi.org/10.3390/nu14183849
Chicago/Turabian StyleChun, Hyejin, Jongchul Oh, and Miae Doo. 2022. "The Risk of Cardiovascular Disease According to Chewing Status Could Be Modulated by Healthy Diet in Middle-Aged Koreans" Nutrients 14, no. 18: 3849. https://doi.org/10.3390/nu14183849
APA StyleChun, H., Oh, J., & Doo, M. (2022). The Risk of Cardiovascular Disease According to Chewing Status Could Be Modulated by Healthy Diet in Middle-Aged Koreans. Nutrients, 14(18), 3849. https://doi.org/10.3390/nu14183849






