Nutritional Assessment of Hospital Meals by Food-Recording Applications
Abstract
:1. Introduction
2. Materials and Methods
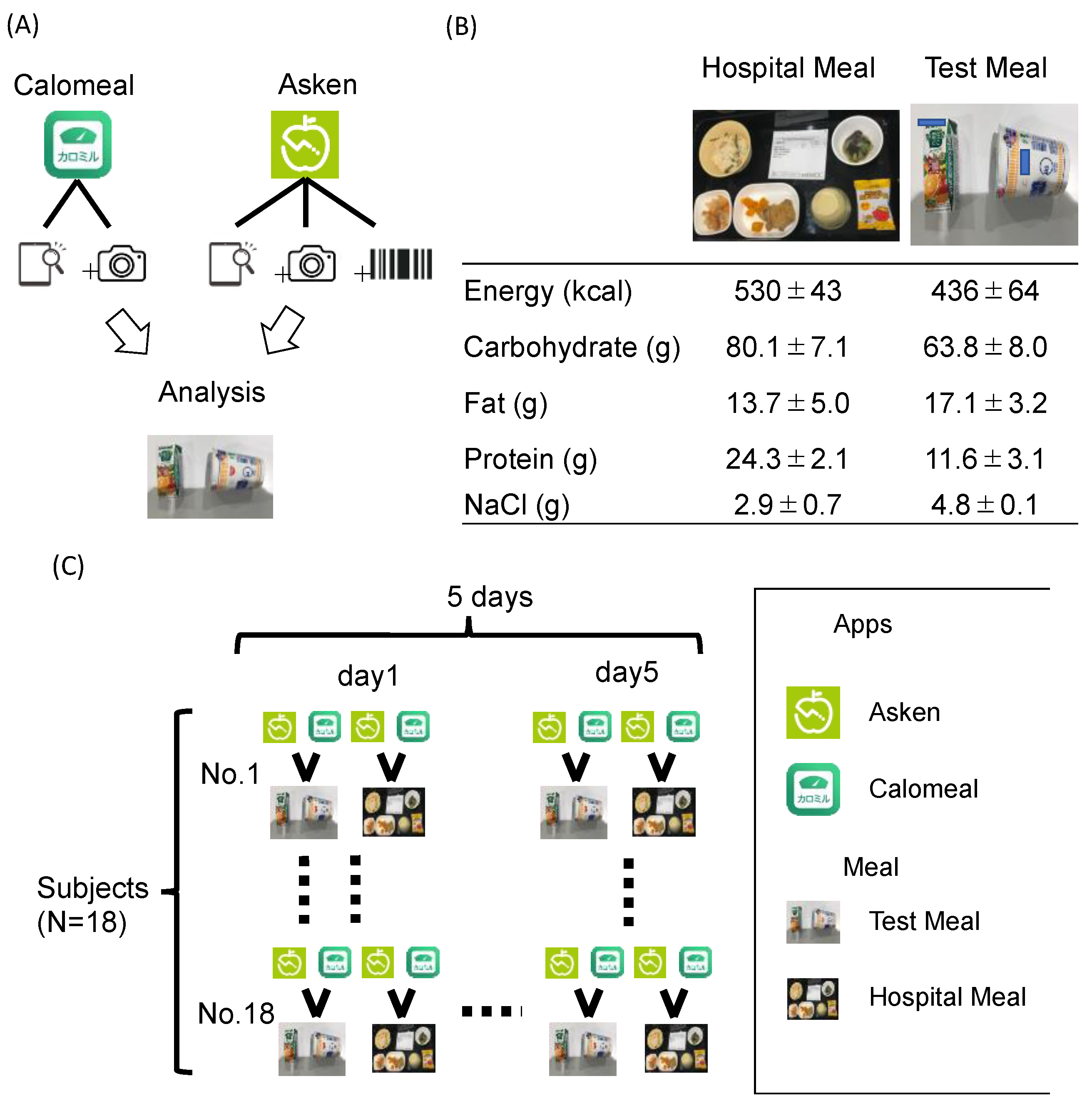
2.1. Mobile Food-Recording Application
2.2. Foods
2.3. Subjects
2.4. Statistics
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ralph, J.L.; Von Ah, D.; Scheett, A.J.; Hoverson, B.S.; Anderson, C.M. Diet assessment methods: A guide for oncology nurses. Clin. J. Oncol. Nurs. 2011, 15, E114–E121. [Google Scholar] [CrossRef]
- Zhang, L.; Misir, A.; Boshuizen, H.; Ocké, M. A Systematic Review and Meta-Analysis of Validation Studies Performed on Die-tary Record Apps. Adv. Nutr. 2021, 12, 2321–2332. [Google Scholar] [CrossRef] [PubMed]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed food intake and risk of cardiovascular disease: Prospective cohort study (NutriNet-Santé). BMJ 2019, 365, l1451. [Google Scholar] [CrossRef] [PubMed]
- Latasa, P.; da Coasta Louzada, M.L.; Steele, E.M.; Monteiro, C.A. Added sugars and ultra-processed foods in Spanish households (1990–2010). Eur. J. Clin. Nutr. 2018, 72, 1404–1412. [Google Scholar] [CrossRef] [PubMed]
- Bowen, K.J.; Sullivan, V.K.; Kris-Etherton, P.M.; Petersen, K.S. Nutrition and Cardiovascular Disease—An Update. Curr. Atheroscler. Rep. 2018, 20, 8. [Google Scholar] [CrossRef] [PubMed]
- Trang, S.; Fraser, J.; Wilkinson, L.; Steckham, K.; Oliphant, H.; Fletcher, H.; Tzianetas, R.; Arcand, J. A Multi-Center Assessment of Nutrient Levels and Foods Provided by Hospital Patient Menus. Nutrients 2015, 7, 9256–9264. [Google Scholar] [CrossRef] [PubMed]
- McClelland, A.; Williams, P. Trend to better nutrition on Australian hospital menus 1986–2001 and the impact of cook-chill food service systems. J. Hum. Nutr. Diet. 2003, 16, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Plourde, H.; Bouzo, V.; Kilgour, R.D.; Cohen, T.R. Validity and Usability of a Smartphone Image-Based Dietary Assessment App Compared to 3-Day Food Diaries in Assessing Dietary Intake Among Canadian Adults: Randomized Controlled Trial. JMIR mHealth uHealth 2020, 8, e16953. [Google Scholar] [CrossRef] [PubMed]
- Shinozaki, N.; Murakami, K. Evaluation of the Ability of Diet-Tracking Mobile Applications to Estimate Energy and Nutrient Intake in Japan. Nutrients 2020, 12, 3327. [Google Scholar] [CrossRef] [PubMed]
- Timon, C.M.; Astell, A.J.; Hwang, F.; Adlam, T.D.; Smith, T.; Maclean, L.; Spurr, D.; Forster, S.E.; Williams, E.A. The validation of a computer-based food record for older adults: The Novel Assessment of Nutrition and Ageing (NANA) method. Br. J Nutr. 2015, 113, 654–664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, L.K.; Czeisler, C.A.; Lockley, S.W.; Rahman, S.A. Time-of-day and Meal Size Effects on Clinical Lipid Markers. J. Clin. Endocrinol. Metab. 2021, 106, e1373–e1379. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, A.J.; Willis, N.D.; Wilson, T.; Zubair, H.; Xie, L.; Chambers, E.; Garcia-Perez, I.; Tailliart, K.; Beckmann, M.; Mathers, J.C.; et al. Developing a Food Exposure and Urine Sampling Strategy for Dietary Exposure Biomarker Validation in Free-Living Individuals. Mol. Nutr. Food Res. 2019, 63, e1900062. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Yin, P.; Shao, Y.; Wang, Z.; Wang, B.; Lehmann, R.; Xu, G. Which is the urine sample material of choice for metabolomics-driven biomarker studies? Anal. Chim. Acta 2020, 1105, 120–127. [Google Scholar] [CrossRef] [PubMed]


| Asken | Calomeal | |||||||
|---|---|---|---|---|---|---|---|---|
| Energy | ||||||||
| Estimate | 2.50% | 97.50% | Pr(>|t|) | Estimate | 2.50% | 97.50% | Pr(>|t|) | |
| Meal | −0.249 | −0.382 | −0.115 | 0 | −0.431 | −0.599 | −0.264 | 0 |
| Time | 0.113 | 0.052 | 0.174 | 0 | 0.079 | 0.005 | 0.152 | 0.039 |
| Age (<or ≧45years) | −0.041 | −0.106 | 0.025 | 0.222 | −0.024 | −0.106 | 0.059 | 0.558 |
| MEAL*Time | −0.064 | −0.101 | −0.026 | 0.001 | −0.044 | −0.089 | 0.002 | 0.064 |
| Carbohydrate | ||||||||
| Estimate | 2.50% | 97.50% | Pr(>|t|) | Estimate | 2.50% | 97.50% | Pr(>|t|) | |
| Meal | −0.172 | −0.306 | −0.037 | 0.014 | −0.303 | −0.485 | −0.121 | 0.001 |
| Time | 0.071 | 0.009 | 0.133 | 0.027 | −0.029 | −0.113 | 0.056 | 0.509 |
| Age (<or ≧45 years) | −0.051 | −0.114 | 0.013 | 0.126 | −0.025 | −0.109 | 0.060 | 0.567 |
| MEAL*Time | −0.043 | −0.082 | −0.004 | 0.034 | 0.011 | −0.042 | 0.064 | 0.687 |
| Fat | ||||||||
| Estimate | 2.50% | 97.50% | Pr(>|t|) | Estimate | 2.50% | 97.50% | Pr(>|t|) | |
| Meal | −0.171 | −1.133 | 0.792 | 0.731 | −0.335 | −1.109 | 0.44 | 0.402 |
| Time | 0.810 | 0.360 | 1.260 | 0.001 | 0.857 | 0.502 | 1.211 | 0 |
| Age (<or ≧45 years) | −0.171 | −0.632 | 0.295 | 0.463 | −0.126 | −0.512 | 0.246 | 0.528 |
| MEAL*Time | −0.409 | −0.677 | −0.141 | 0.003 | −0.451 | −0.673 | −0.229 | 0 |
| Protein | ||||||||
| Estimate | 2.50% | 97.50% | Pr(>|t|) | Estimate | 2.50% | 97.50% | Pr(>|t|) | |
| Meal | −0.147 | −0.335 | 0.040 | 0.128 | −0.588 | −0.874 | −0.302 | 0 |
| Time | 0.094 | 0.01 | 0.178 | 0.031 | 0.037 | −0.094 | 0.169 | 0.58 |
| Age (<or ≧45 years) | −0.017 | −0.113 | 0.080 | 0.718 | −0.012 | −0.153 | 0.129 | 0.865 |
| MEAL*Time | −0.033 | −0.086 | 0.020 | 0.222 | −0.022 | −0.103 | 0.059 | 0.600 |
| NaCl | ||||||||
| Estimate | 2.50% | 97.50% | Pr(>|t|) | Estimate | 2.50% | 97.50% | Pr(>|t|) | |
| Meal | −0.31 | −0.581 | −0.038 | 0.028 | −0.706 | −0.986 | −0.426 | 0 |
| Time | 0.232 | 0.106 | 0.358 | 0 | −0.02 | −0.149 | 0.109 | 0.765 |
| Age (<or ≧45 years) | −0.049 | −0.18 | 0.082 | 0.439 | −0.041 | −0.192 | 0.111 | 0.576 |
| MEAL*Time | −0.116 | −0.195 | −0.037 | 0.005 | 0.005 | −0.074 | 0.084 | 0.899 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iizuka, K.; Ishihara, T.; Watanabe, M.; Ito, A.; Sarai, M.; Miyahara, R.; Suzuki, A.; Saitoh, E.; Sasaki, H. Nutritional Assessment of Hospital Meals by Food-Recording Applications. Nutrients 2022, 14, 3754. https://doi.org/10.3390/nu14183754
Iizuka K, Ishihara T, Watanabe M, Ito A, Sarai M, Miyahara R, Suzuki A, Saitoh E, Sasaki H. Nutritional Assessment of Hospital Meals by Food-Recording Applications. Nutrients. 2022; 14(18):3754. https://doi.org/10.3390/nu14183754
Chicago/Turabian StyleIizuka, Katsumi, Takuma Ishihara, Mayuka Watanabe, Akemi Ito, Masayoshi Sarai, Ryoji Miyahara, Atsushi Suzuki, Eiichi Saitoh, and Hitomi Sasaki. 2022. "Nutritional Assessment of Hospital Meals by Food-Recording Applications" Nutrients 14, no. 18: 3754. https://doi.org/10.3390/nu14183754
APA StyleIizuka, K., Ishihara, T., Watanabe, M., Ito, A., Sarai, M., Miyahara, R., Suzuki, A., Saitoh, E., & Sasaki, H. (2022). Nutritional Assessment of Hospital Meals by Food-Recording Applications. Nutrients, 14(18), 3754. https://doi.org/10.3390/nu14183754







