Acceptability of the FIGO Nutrition Checklist in Preconception and Early Pregnancy to Assess Nutritional Status and Prevent Excess Gestational Weight Gain: A Study of Women and Healthcare Practitioners in the UK
Abstract
:1. Introduction
1.1. Impact of Nutrition on Pregnancy and Offspring Health across the Life Course
1.2. The FIGO Nutrition Checklist
1.3. Aim
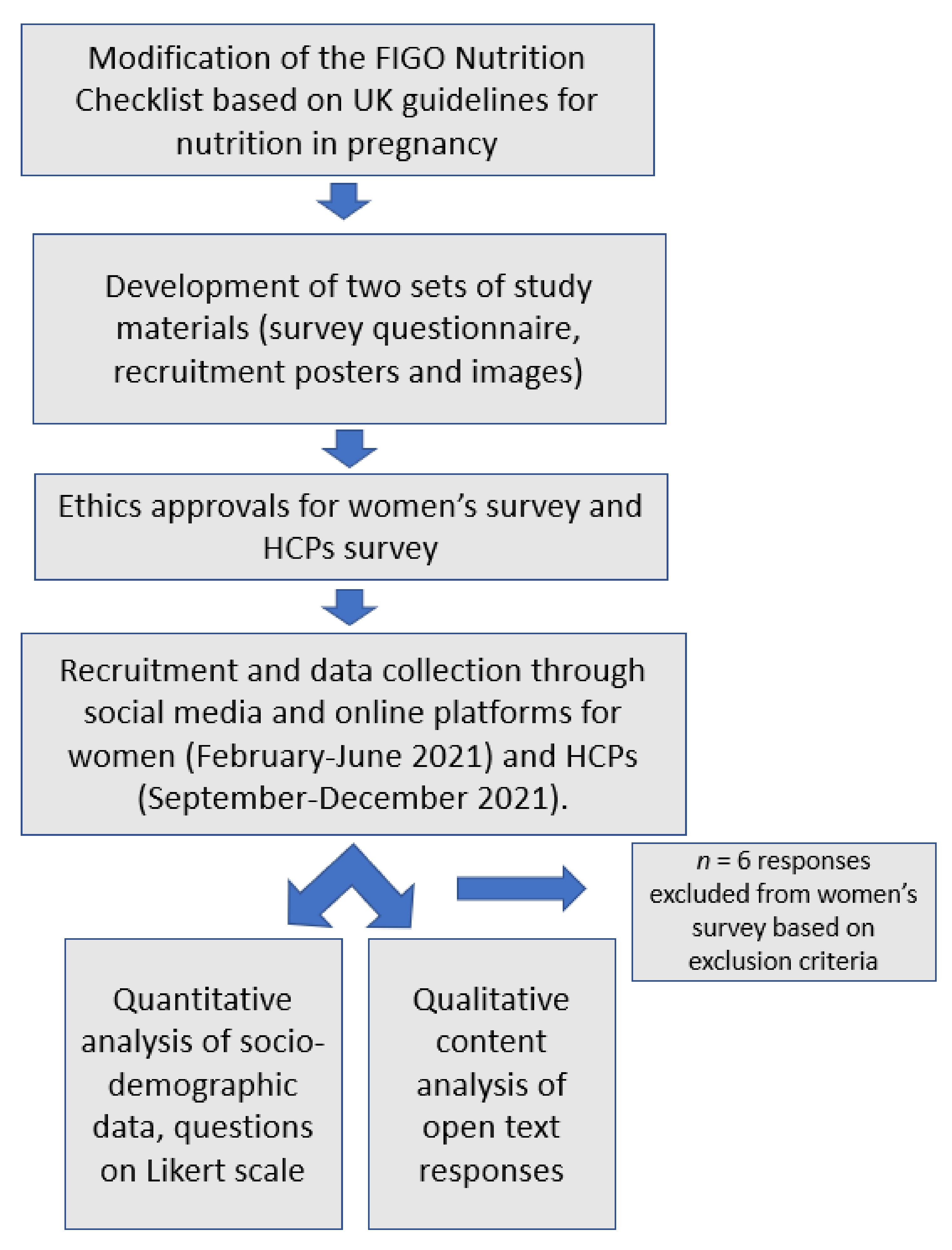
2. Materials and Methods
2.1. Participants and Sampling
2.2. Study Materials
2.3. Data Collection
2.4. Analysis
2.4.1. Quantitative Analysis
2.4.2. Qualitative Content Analysis
3. Results
3.1. Participant Characteristics
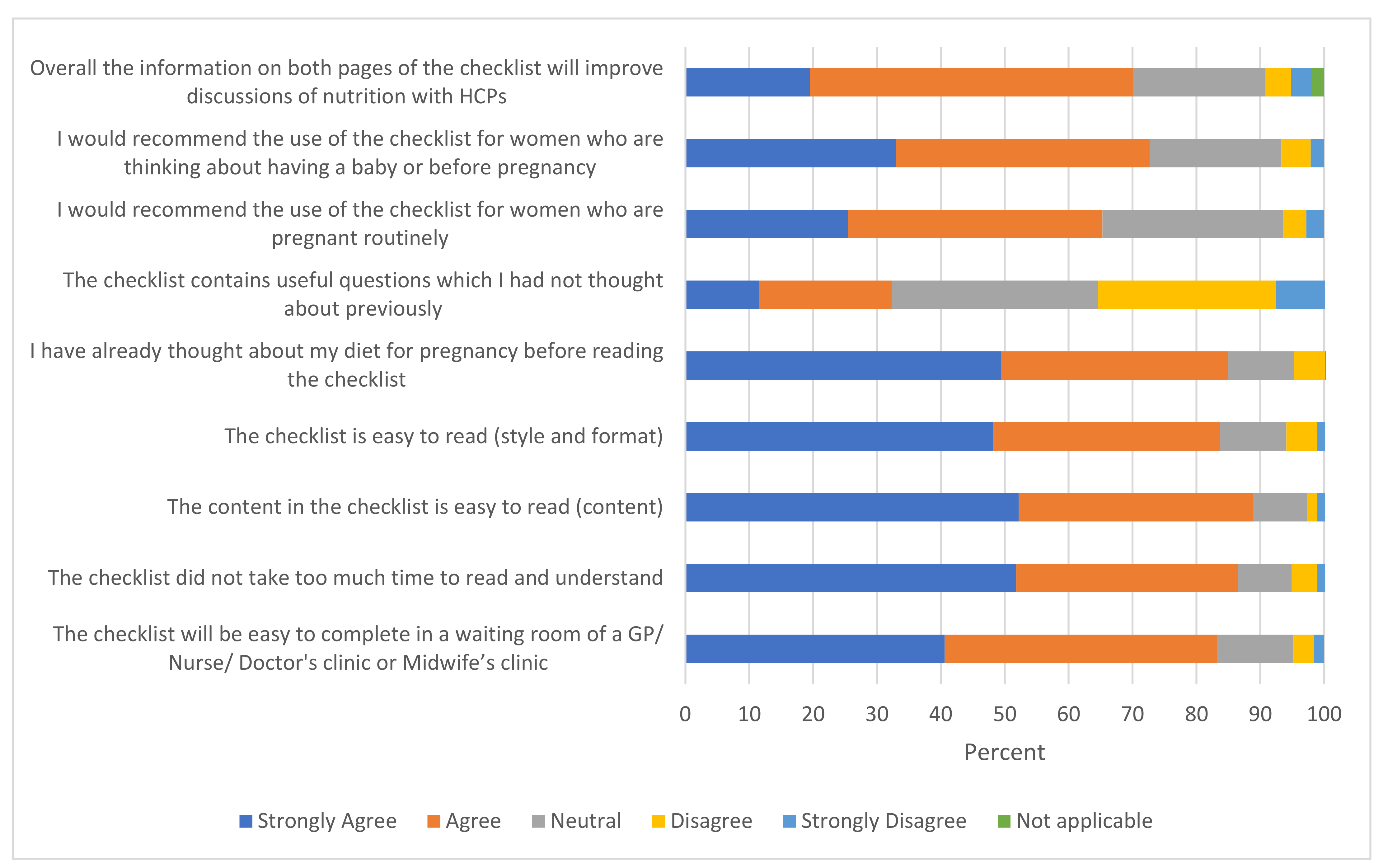
3.2. Acceptability of the Checklist
3.2.1. Findings from Regression Analysis
3.2.2. Suggestions for Modification and Implementation of the Checklist
“During my first pregnancy, the midwife couldn’t advise on whether I could continue the exercise regime I was doing because she didn’t know… you are advised of everything you can’t do … but not what you can actually do”(ID 1050)
“I believe more supportive tools to take away from the meeting along with the communications provided at the meetings.”(ID 1044)
“It might be better to concentrate on one aspect of the checklist that is a priority for the patient, would also be more patient-centred. e.g., physical activity—could talk about options…”(GP, 101)
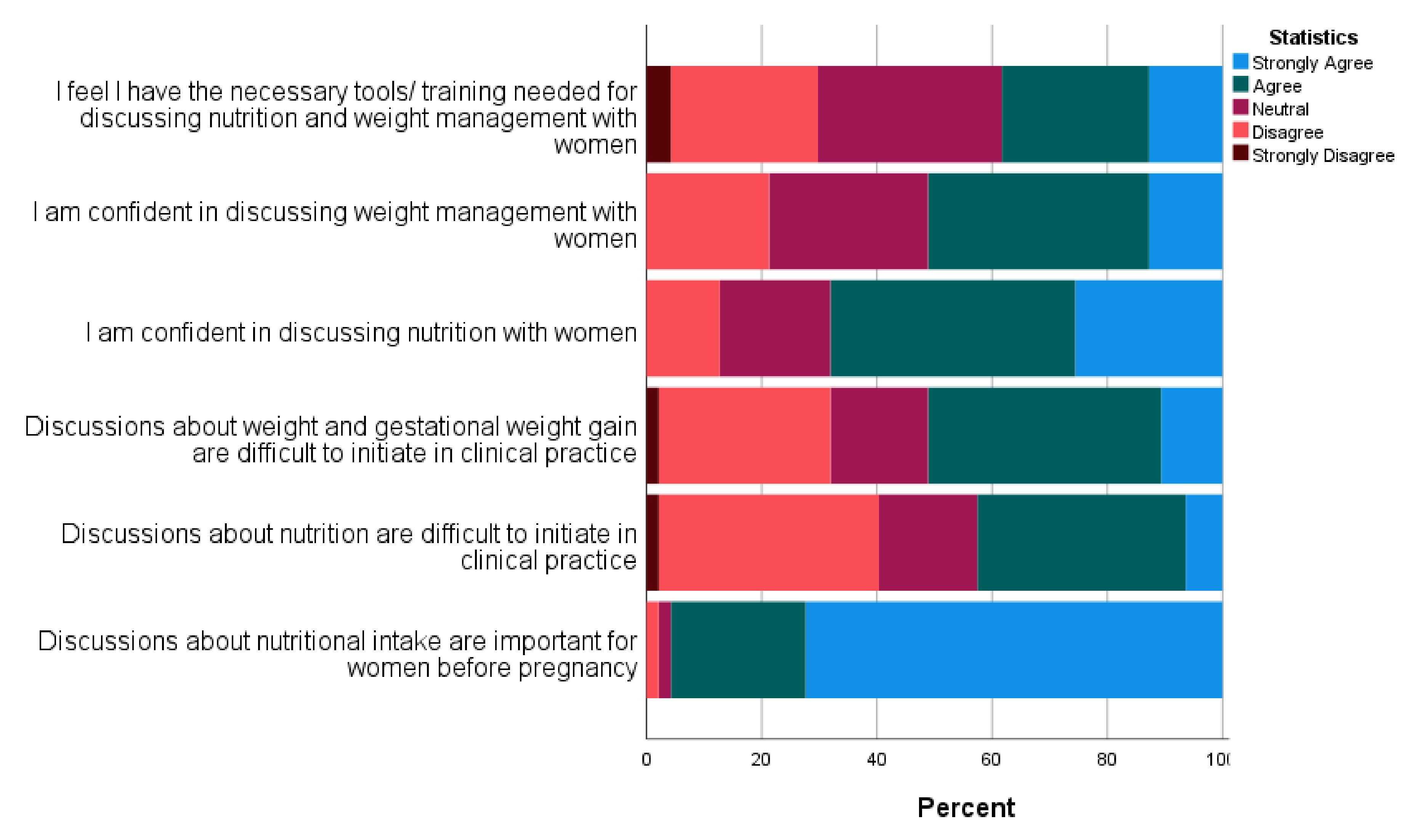
3.3. Response to Questions on Current Practice
3.4. Discussing Nutrition, Weight, and Obesity-Related Topics in Clinical Care Routinely
4. Discussion
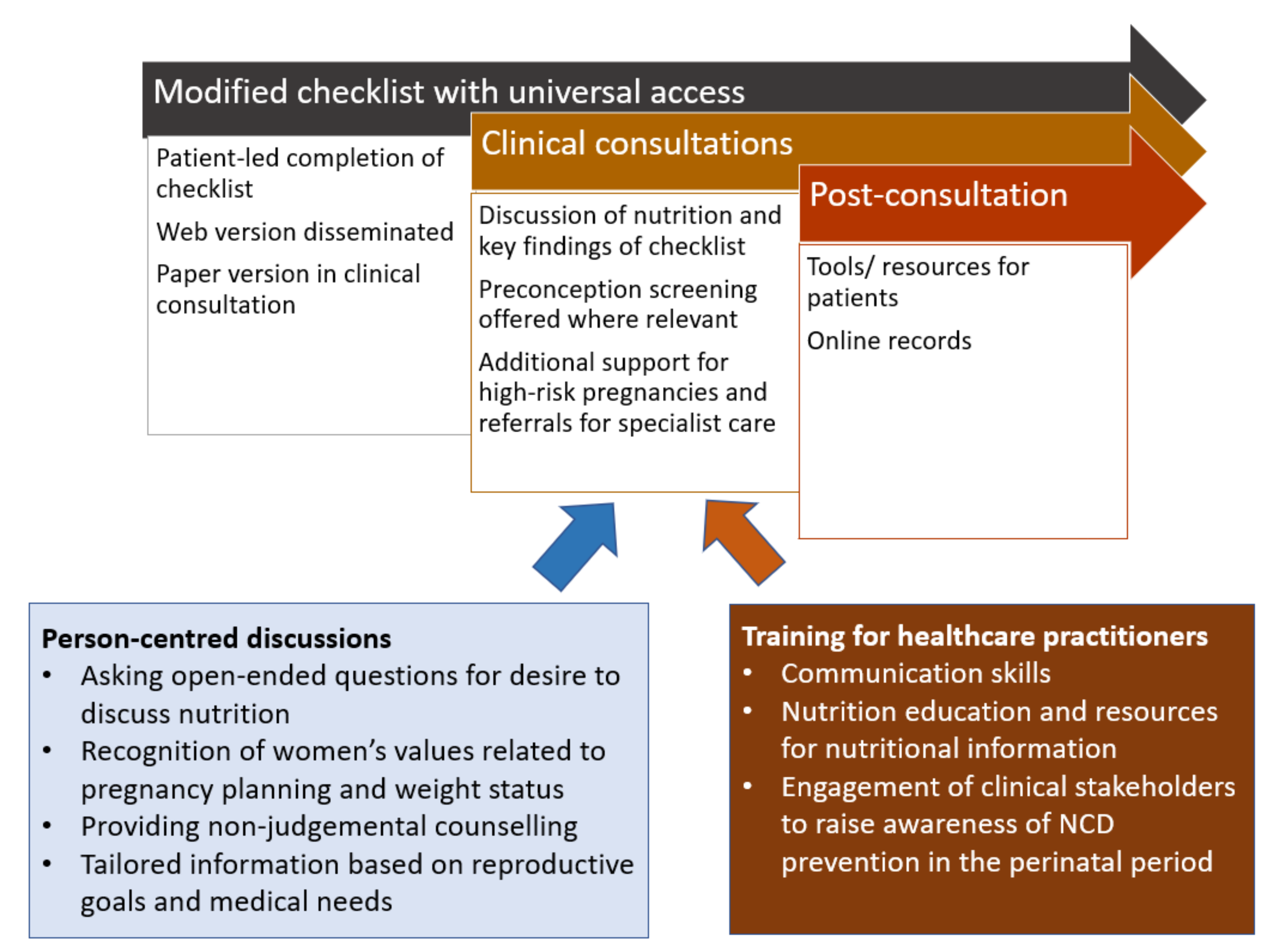
4.1. Recommendations for Implementation of the FIGO Nutrition Checklist
4.2. Recommendations to Support Discussion on Diet and Nutrition in the Perinatal Period in the UK
4.3. Strengths and Limitations of This Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ma, R.C.W.; Schmidt, M.I.; Tam, W.H.; McIntyre, H.D.; Catalano, P.M. Clinical management of pregnancy in the obese mother: Before conception, during pregnancy, and post partum. Lancet Diabetes Endocrinol. 2016, 4, 1037–1049. [Google Scholar] [CrossRef]
- Daly, M.; Kipping, R.R.; Tinner, L.E.; Sanders, J.; White, J.W. Preconception exposures and adverse pregnancy, birth and postpartum outcomes: Umbrella review of systematic reviews. Paediatr. Perinat. Epidemiol. 2022, 36, 288–299. [Google Scholar] [CrossRef]
- Fleming, T.P.; Watkins, A.J.; Velazquez, M.A.; Mathers, J.C.; Prentice, A.M.; Stephenson, J.; Barker, M.; Saffery, R.; Yajnik, C.S.; Eckert, J.J. Origins of lifetime health around the time of conception: Causes and consequences. Lancet 2018, 391, 1842–1852. [Google Scholar] [CrossRef]
- Stephenson, J.; Heslehurst, N.; Hall, J.; Schoenaker, D.A.; Hutchinson, J.; Cade, J.E.; Poston, L.; Barrett, G.; Crozier, S.R.; Barker, M.; et al. Before the beginning: Nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018, 391, 1830–1841. [Google Scholar] [CrossRef]
- Hanson, M.A.; Bardsley, A.; De-Regil, L.M.; Moore, S.E.; Oken, E.; Poston, L.; Ma, R.C.; McAuliffe, F.M.; Maleta, K.; Purandare, C.N. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition: “Think Nutrition First”. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2015, 131, S213. [Google Scholar] [CrossRef]
- Stephenson, J.; Vogel, C.; Hall, J.; Hutchinson, J.; Mann, S.; Duncan, H.; Woods-Townsend, K.; de Lusignan, S.; Poston, L.; Cade, J. Preconception health in England: A proposal for annual reporting with core metrics. Lancet 2019, 393, 2262–2271. [Google Scholar] [CrossRef]
- Stephenson, J.; Schoenaker, D.A.; Hinton, W.; Poston, L.; Barker, M.; Alwan, N.A.; Godfrey, K.; Hanson, M.; de Lusignan, S. A wake-up call for preconception health: A clinical review. Br. J. Gen. Pract. 2021, 71, 233–236. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M.; Godfrey, K.; Poston, L.; Bustreo, F.; Stephenson, J. Pre-conception health. In Annual Report of the Chief Medical Officer—The Health of the 51% Women; Department of Health: London, UK, 2015. [Google Scholar]
- Black, M.M.; Walker, S.P.; Fernald, L.C.H.; Andersen, C.T.; DiGirolamo, A.M.; Lu, C.; McCoy, D.C.; Fink, G.; Shawar, Y.R.; Shiffman, J.; et al. Early childhood development coming of age: Science through the life course. Lancet 2017, 389, 77–90. [Google Scholar] [CrossRef]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Chopra, M.; Kaur, N.; Singh, K.D.; Maria Jacob, C.; Divakar, H.; Babu, G.R.; Hong Nguyen, P.; Bhanot, A.; Sabharwal, M.; Deb, S. Population estimates, consequences, and risk factors of obesity among pregnant and postpartum women in India: Results from a national survey and policy recommendations. Int. J. Gynecol. Obstet. 2020, 151, 57–67. [Google Scholar] [CrossRef]
- Poston, L.; Bell, R.; Croker, H.; Flynn, A.C.; Godfrey, K.M.; Goff, L.; Hayes, L.; Khazaezadeh, N.; Nelson, S.M.; Oteng-Ntim, E. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): A multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2015, 3, 767–777. [Google Scholar] [CrossRef]
- McAuliffe, F.M.; Killeen, S.L.; Jacob, C.M.; Hanson, M.A.; Hadar, E.; McIntyre, H.D.; Kapur, A.; Kihara, A.B.; Ma, R.C.; Divakar, H. Management of prepregnancy, pregnancy, and postpartum obesity from the FIGO Pregnancy and Non-Communicable Diseases Committee: A FIGO (International Federation of Gynecology and Obstetrics) guideline. Int. J. Gynaecol. Obstet. 2020, 151, 16–36. [Google Scholar] [CrossRef]
- Mazza, D.; Chapman, A.; Michie, S. Barriers to the implementation of preconception care guidelines as perceived by general practitioners: A qualitative study. BMC Health Serv. Res. 2013, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- International Federation of Gynaecology and Obstetrics. The FIGO Nutrition Checklist; FIGO: London, UK, 2020. [Google Scholar]
- Killeen, S.; Callaghan, S.; Jacob, C.; Hanson, M.; McAuliffe, F.M. Examining the use of the FIGO Nutrition Checklist in routine antenatal practice: Multi-stakeholder feedback to implementation. Int. J. Gynecol. Obstet. 2020, 151, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Tsoi, K.Y.; Chan, R.; Li, L.; McAuliffe, F.; Hanson, M.; Tam, W.; Ma, R. Evaluation of dietary pattern in early pregnancy using the FIGO Nutritional Checklist compared to a Food Frequency Questionnaire (FFQ). Int. J. Gynaecol. Obstet. 2020, 151, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Killeen, S.L.; Callaghan, S.L.; Jacob, C.M.; Hanson, M.A.; McAuliffe, F.M. “It only takes two minutes to ask”—A qualitative study with women on using the FIGO Nutrition Checklist in pregnancy. Int. J. Gynecol. Obstet. 2020, 151, 45–50. [Google Scholar] [CrossRef]
- Parisi, F.; Savasi, V.M.; di Bartolo, I.; Mandia, L.; Cetin, I. Associations between First Trimester Maternal Nutritional Score, early markers of placental function, and pregnancy outcome. Nutrients 2020, 12, 1799. [Google Scholar] [CrossRef] [PubMed]
- Sekhon, M.; Cartwright, M.; Francis, J.J. Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv. Res. 2017, 17, 88. [Google Scholar] [CrossRef] [PubMed]
- Wilding, S.; Ziauddeen, N.; Smith, D.; Roderick, P.; Alwan, N.A. Maternal and early-life area-level characteristics and childhood adiposity: A systematic review. Obes. Rev. 2019, 20, 1093–1105. [Google Scholar] [CrossRef]
- Ministry of Housing, Communities & Local Government. National Statistics. English Indices of Deprivation 2019; Ministry of Housing, Communities & Local Government: London, UK, 2019.
- Hill, B.; Hall, J.; Skouteris, H.; Currie, S. Defining preconception: Exploring the concept of a preconception population. BMC Pregnancy Childbirth 2020, 20, 280. [Google Scholar] [CrossRef]
- Edwards, M.L.; Smith, B.C. The effects of the neutral response option on the extremeness of participant responses. J. Undergrad. Scholarsh. 2014, 6, 30. [Google Scholar]
- Nowlis, S.M.; Kahn, B.E.; Dhar, R. Coping with ambivalence: The effect of removing a neutral option on consumer attitude and preference judgments. J. Consum. Res. 2002, 29, 319–334. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Robson, C. Real World Research: A Resource for Social Scientists and Practitioner-Researchers; Wiley-Blackwell: Hoboken, NJ, USA, 2002. [Google Scholar]
- Ballinger, C. Writing up rigour: Representing and evaluating good scholarship in qualitative research. Br. J. Occup. Ther. 2004, 67, 540–546. [Google Scholar] [CrossRef]
- Pawson, R.; Tilley, N. Realist Evaluation (Chapter Introduction); Sage Publications Ltd.: London, UK, 2004. [Google Scholar]
- Heslehurst, N.; Rankin, J.; Wilkinson, J.R.; Summerbell, C.D. A nationally representative study of maternal obesity in England, UK: Trends in incidence and demographic inequalities in 619,323 births, 1989–2007. Int. J. Obes. 2010, 34, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, S.E.; Parsons, J.; Naughton, F.; Fulton, E.A.; Tombor, I.; Brown, K.E. Are digital interventions for smoking cessation in pregnancy effective? A systematic review and meta-analysis. Health Psychol. Rev. 2018, 12, 333–356. [Google Scholar] [CrossRef]
- Van Dijk, M.R.; Huijgen, N.A.; Willemsen, S.P.; Laven, J.S.; Steegers, E.A.; Steegers-Theunissen, R.P. Impact of an mHealth platform for pregnancy on nutrition and lifestyle of the reproductive population: A survey. JMIR Mhealth Uhealth 2016, 4, e5197. [Google Scholar] [CrossRef]
- Guendelman, S.; Broderick, A.; Mlo, H.; Gemmill, A.; Lindeman, D. Listening to communities: Mixed-method study of the engagement of disadvantaged mothers and pregnant women with digital health technologies. J. Med. Internet Res. 2017, 19, e240. [Google Scholar] [CrossRef]
- FIGO. FIGO’s Nutrition Checklist Wins Semi-Final at the HSE-HIHI Spark Ignite Awards. Available online: https://www.figo.org/news/figos-nutrition-checklist-wins-semi-final-hse-hihi-spark-ignite-awards (accessed on 20 June 2022).
- Jacob, C.; Killeen, S.; McAuliffe, F.; Stephenson, J.; Hod, M.; Diaz Yamal, I.; Malhotra, J.; Mocanu, E.; McIntyre, H.; Kihara, A.; et al. Prevention of noncommunicable diseases by interventions in the preconception period: A FIGO position paper for action by healthcare practitioners. Int. J. Gynecol. Obstet. 2020, 151, 6–15. [Google Scholar] [CrossRef]
- Lawrence, W.; Vogel, C.; Strömmer, S.; Morris, T.; Treadgold, B.; Watson, D.; Hart, K.; McGill, K.; Hammond, J.; Harvey, N.C. How can we best use opportunities provided by routine maternity care to engage women in improving their diets and health? Matern. Child Nutr. 2020, 16, e12900. [Google Scholar] [CrossRef]
- Heslehurst, N.; Russell, S.; McCormack, S.; Sedgewick, G.; Bell, R.; Rankin, J. Midwives perspectives of their training and education requirements in maternal obesity: A qualitative study. Midwifery 2013, 29, 736–744. [Google Scholar] [CrossRef]
- Nyman, V.M.; Prebensen, Å.K.; Flensner, G.E. Obese women’s experiences of encounters with midwives and physicians during pregnancy and childbirth. Midwifery 2010, 26, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Abayomi, J.; Charnley, M.; Cassidy, L.; McCann, M.T.; Jones, J.; Wright, M.; Newson, L. A patient and public involvement investigation into healthy eating and weight management advice during pregnancy. Int. J. Qual. Health Care 2020, 32, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Olander, E.K.; Berg, M.; McCourt, C.; Carlström, E.; Dencker, A. Person-centred care in interventions to limit weight gain in pregnant women with obesity-a systematic review. BMC Pregnancy Childbirth 2015, 15, 50. [Google Scholar] [CrossRef] [PubMed]
- Ekman, I.; Swedberg, K.; Taft, C.; Lindseth, A.; Norberg, A.; Brink, E.; Carlsson, J.; Dahlin-Ivanoff, S.; Johansson, I.-L.; Kjellgren, K. Person-centered care—ready for prime time. Eur. J. Cardiovasc. Nurs. 2011, 10, 248–251. [Google Scholar] [PubMed]
- Morris, T.; Strömmer, S.; Vogel, C.; Harvey, N.; Cooper, C.; Inskip, H.; Woods-Townsend, K.; Baird, J.; Barker, M.; Lawrence, W. Improving pregnant women’s diet and physical activity behaviours: The emergent role of health identity. BMC Pregnancy Childbirth 2020, 20, 244. [Google Scholar] [CrossRef]
- Strachan, S.M.; Woodgate, J.; Brawley, L.R.; Tse, A. The relationship of self-efficacy and self-identity to long-term maintenance of vigorous physical activity 1. J. Appl. Biobehav. Res. 2005, 10, 98–112. [Google Scholar] [CrossRef]
- Sattler, K.M.; Deane, F.P.; Tapsell, L.; Kelly, P.J. Gender differences in the relationship of weight-based stigmatisation with motivation to exercise and physical activity in overweight individuals. Health Psychol. Open 2018, 5, 2055102918759691. [Google Scholar] [CrossRef]
- Rothbaum, J. How Does the Pandemic Affect Survey Response: Using Administrative Data to Evaluate Nonresponse in the Current Population Survey Annual Social and Economic Supplement; United States Census Bureau: Sortland, MD, USA, 2021. [Google Scholar]
- De Koning, R.; Egiz, A.; Kotecha, J.; Ciuculete, A.C.; Ooi, S.Z.Y.; Bankole, N.D.A.; Erhabor, J.; Higginbotham, G.; Khan, M.; Dalle, D.U. Survey Fatigue During the COVID-19 Pandemic: An Analysis of Neurosurgery Survey Response Rates. Front. Surg. 2021, 8, 690680. [Google Scholar] [CrossRef]


| Descriptor | N | % |
|---|---|---|
| Reproductive Group | ||
| Preconception | 106 | 42.2 |
| Pregnant | 91 | 36.3 |
| Postpartum | 54 | 21.5 |
| Age, years | ||
| 18–25 | 35 | 13.9 |
| 26–30 | 61 | 24.3 |
| 31–35 | 93 | 37.1 |
| 36–40 | 36 | 14.3 |
| 41 and above | 26 | 10.4 |
| Region | ||
| East of England | 24 | 9.6 |
| East Midlands | 9 | 3.6 |
| London | 25 | 10 |
| Northeast | 9 | 3.6 |
| Northwest | 19 | 7.6 |
| Southeast | 64 | 25.5 |
| Southwest | 32 | 12.7 |
| West Midlands | 17 | 6.8 |
| Yorkshire/Humberside | 18 | 7.2 |
| Northern Ireland | 11 | 4.4 |
| Scotland | 17 | 6.8 |
| Wales | 6 | 2.4 |
| Education | ||
| Primary school or Secondary school up to 16 years | 6 | 2.4 |
| Higher or secondary or further education (A-levels, BTEC, etc.) | 26 | 10.4 |
| College or university | 117 | 46.6 |
| Post-graduate degree | 89 | 35.5 |
| Other | 4 | 1.6 |
| Prefer not to say | 9 | 3.6 |
| Ethnicity | ||
| White | 212 | 84.5 |
| Black/Black British | 6 | 2.4 |
| Asian/Asian British (South Asian) | 18 | 7.2 |
| Asian/Asian British (Chinese) | 4 | 1.6 |
| Mixed/Multiple ethnic groups or Other | 9 | 3.6 |
| Prefer not to say | 2 | 0.8 |
| Index of Multiple Deprivation Quintile * | (N = 147) | (Valid percent) |
| Quintile 1 | 15 | 10.2 |
| Quintile 2 | 28 | 19.0 |
| Quintile 3 | 32 | 21.8 |
| Quintile 4 | 30 | 20.4 |
| Quintile 5 | 42 | 28.6 |
| Descriptor | N | % |
|---|---|---|
| Staff category | ||
| General Practitioner | 3 | 6 |
| OBGYN | 8 | 17 |
| Staff Midwife | 11 | 23 |
| Community Midwife | 9 | 19 |
| Health Visitor | 5 | 11 |
| Dietitian | 8 | 17 |
| Other | 3 | 6 |
| Years of Clinical experience * | ||
| Currently training/less than 2 years | 6 | 13 |
| 2–5 years | 8 | 17 |
| 6–10 years | 6 | 13 |
| More than 10 years | 27 | 57 |
| Region * | ||
| London | 6 | 13 |
| North (East and West) | 9 | 19 |
| South (East and West) | 23 | 49 |
| East of England | 1 | 2 |
| Scotland | 3 | 6 |
| Wales | 4 | 9 |
| Northern Ireland | 1 | 2 |
| Category | Sub-Categories (n) | Sample Quotes |
|---|---|---|
| A. Positive views on routine discussion |
| “When pregnant you have no idea if you’re eating the right things/gaining the right amount of weight and I found I received next to no advice or had any conversations around this.” (ID 1022) |
| B. Negative implications of routine discussion |
| “It doesn’t need to be discussed routinely as it would cause unnecessary stress … Pregnancy sickness and nausea affect dietary habits in the beginning and keeping any food down is a success so regular discussions about nutrition would cause additional pressure.” (ID 1072) |
| C. Information |
| “I’d find it really helpful. I was vegetarian and chose to eat fish pre-pregnancy to help improve my diet. Any discussion around diet would have been immensely helpful and reassuring.” (ID 1113) |
| D. Communication and conversation |
| “I would be happy with this as long as it was framed positively, not in a way that makes mums feel they are damaging their baby or being shamed. E.g., statements like eating fatty acids are good for baby’s brain development” (ID 1027) |
| E. Other (19) (This separate category looks at reasons to refuse routine discussion for oneself but accept it for other women or for the health of the baby.) |
| “I didn’t gain much weight during/after my pregnancy and already back to my pre pregnancy healthy weight. Nutrition was never mentioned to me, but I already live a healthy lifestyle. I think it would be very beneficial to others though.” (ID 1026) |
| Category | Sub-Categories (n) | Sample Quotes |
|---|---|---|
| A. Practical issues relating to discussion of nutrition |
| “Often other priority areas e.g., communicating info about gestational diabetes and hypertension. As always obesity gets underprioritized” (GP 101) |
| B. Concerns around communication relating to nutrition and the checklist |
| “… By changing the focus of the dietary changes from being all about weight, to being about making sure mother is having the right nutrition for her and baby, then we can still achieve the same healthy dietary changes (and therefore outcomes) but without the negative connotations and stigma of discussing weight all the time.” (Dietitian, 144) |
| C. Support for routine discussion and recommendations |
| “Questionnaires promote self-questioning behaviour rather than “being told” by a midwife”. (Midwife, 108)“I feel nutrition is so important and we should all be focusing on it more…Also as GPs we are not always well informed as not taught much about nutrition” (GP, 120). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jacob, C.M.; Inskip, H.M.; Lawrence, W.; McGrath, C.; McAuliffe, F.M.; Killeen, S.L.; Divakar, H.; Hanson, M. Acceptability of the FIGO Nutrition Checklist in Preconception and Early Pregnancy to Assess Nutritional Status and Prevent Excess Gestational Weight Gain: A Study of Women and Healthcare Practitioners in the UK. Nutrients 2022, 14, 3623. https://doi.org/10.3390/nu14173623
Jacob CM, Inskip HM, Lawrence W, McGrath C, McAuliffe FM, Killeen SL, Divakar H, Hanson M. Acceptability of the FIGO Nutrition Checklist in Preconception and Early Pregnancy to Assess Nutritional Status and Prevent Excess Gestational Weight Gain: A Study of Women and Healthcare Practitioners in the UK. Nutrients. 2022; 14(17):3623. https://doi.org/10.3390/nu14173623
Chicago/Turabian StyleJacob, Chandni Maria, Hazel M. Inskip, Wendy Lawrence, Carmel McGrath, Fionnuala M. McAuliffe, Sarah Louise Killeen, Hema Divakar, and Mark Hanson. 2022. "Acceptability of the FIGO Nutrition Checklist in Preconception and Early Pregnancy to Assess Nutritional Status and Prevent Excess Gestational Weight Gain: A Study of Women and Healthcare Practitioners in the UK" Nutrients 14, no. 17: 3623. https://doi.org/10.3390/nu14173623
APA StyleJacob, C. M., Inskip, H. M., Lawrence, W., McGrath, C., McAuliffe, F. M., Killeen, S. L., Divakar, H., & Hanson, M. (2022). Acceptability of the FIGO Nutrition Checklist in Preconception and Early Pregnancy to Assess Nutritional Status and Prevent Excess Gestational Weight Gain: A Study of Women and Healthcare Practitioners in the UK. Nutrients, 14(17), 3623. https://doi.org/10.3390/nu14173623





