The Effect of a Multifaceted Intervention on Dietary Quality in Schoolchildren and the Mediating Effect of Dietary Quality between Intervention and Changes in Adiposity Indicators: A Cluster Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
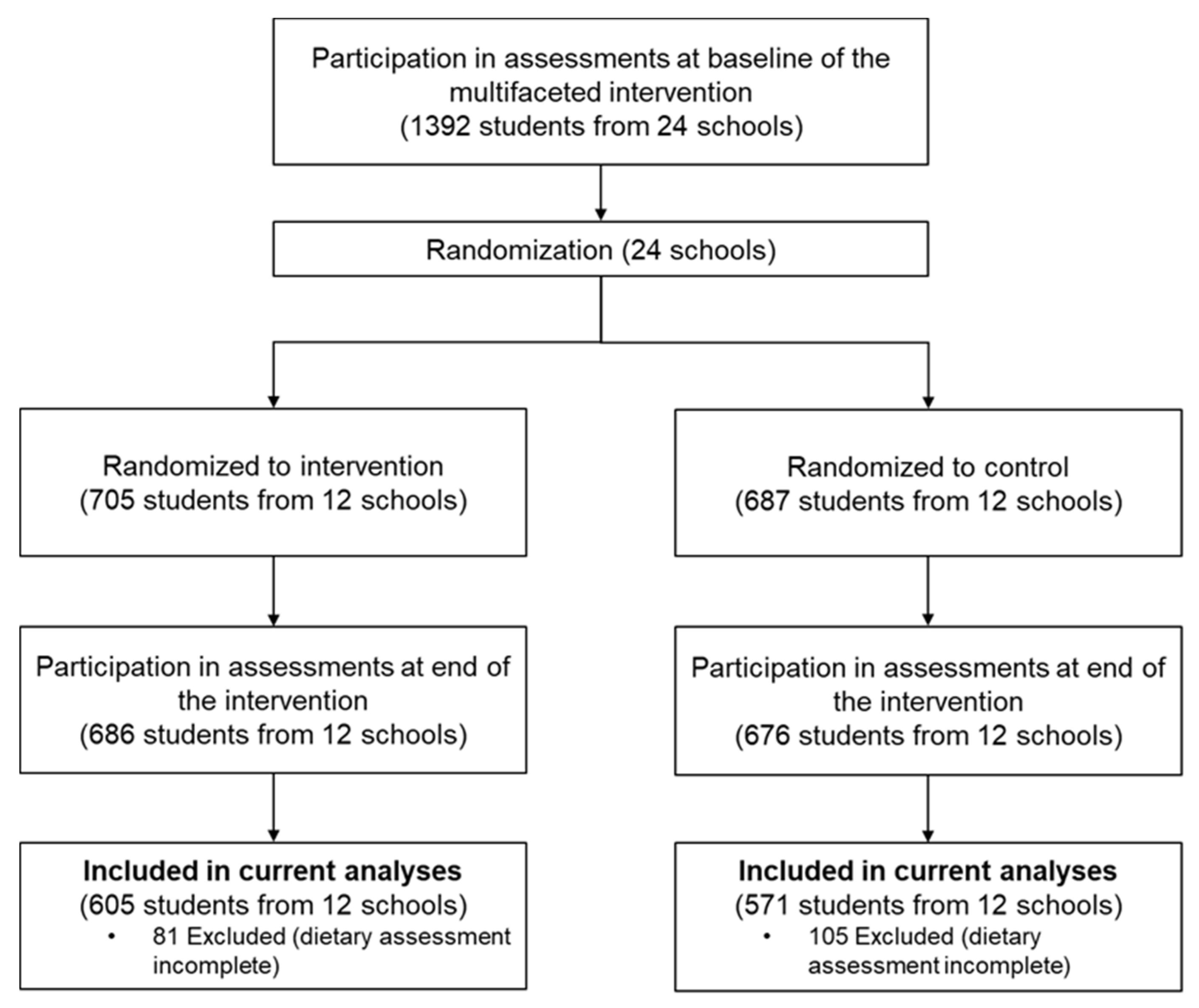
2.1. Study Design and Participants
2.2. Intervention
2.3. Outcome Measures
2.3.1. Assessment of Dietary Intake
2.3.2. Calculation of Dietary Quality
2.3.3. Adiposity Indicators
2.4. Covariates
2.5. Statistical Analyses
3. Results
3.1. Characteristics of Participants
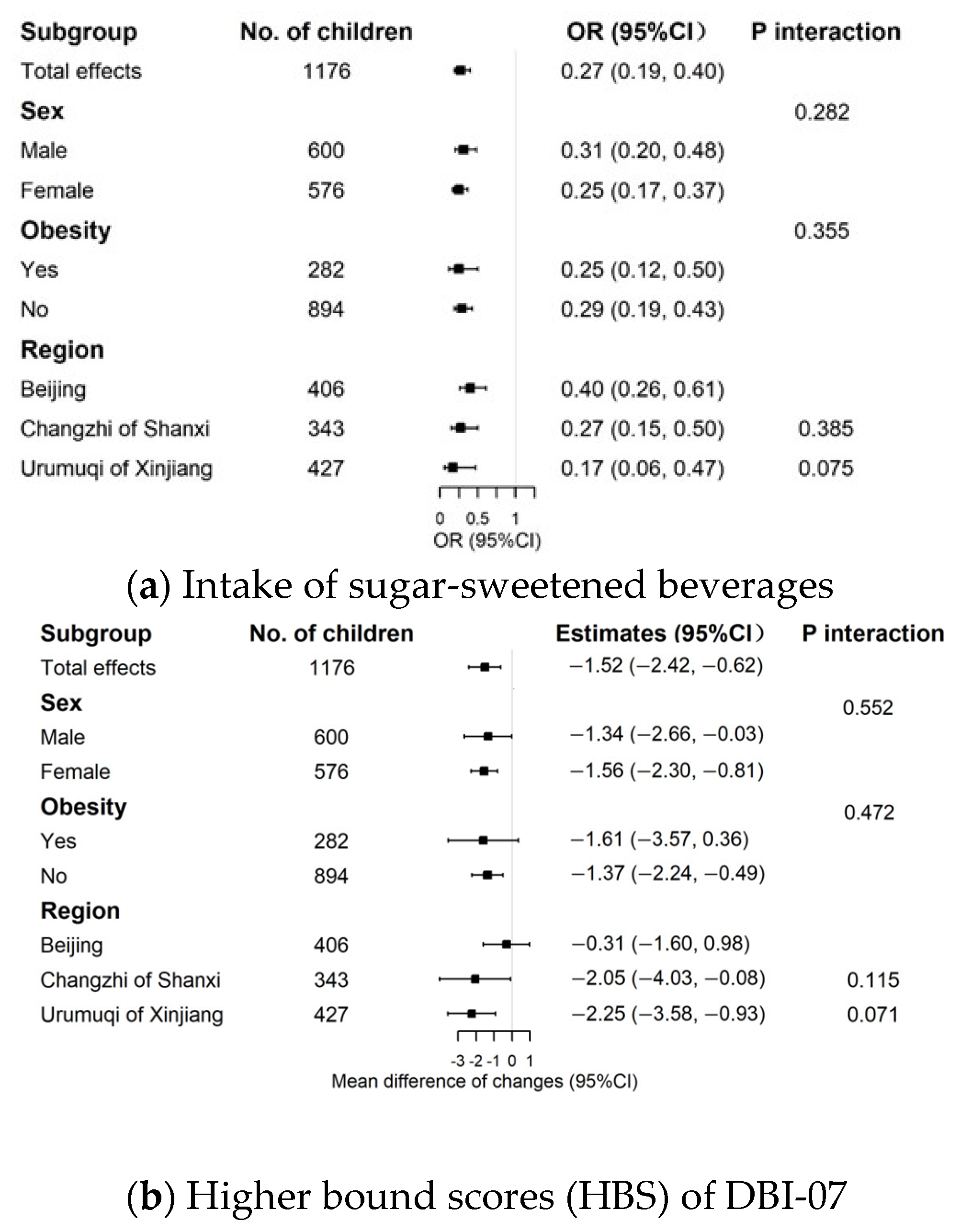
3.2. Effects of the Intervention on Indicators of Food Subgroups and Dietary Quality
3.3. Mediation Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Pan, X.F.; Wang, L.; Pan, A. Epidemiology and determinants of obesity in China. Lancet. Diabetes Endocrinol. 2021, 9, 373–392. [Google Scholar] [CrossRef]
- Han, J.C.; Lawlor, D.A.; Kimm, S.Y.S. Childhood obesity. Lancet 2010, 375, 1737–1748. [Google Scholar] [CrossRef]
- Liu, Z.; Xu, H.-M.; Wen, L.-M.; Peng, Y.-Z.; Lin, L.-Z.; Zhou, S.; Li, W.-H.; Wang, H.-J. A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 95. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 7, Cd001871. [Google Scholar] [CrossRef]
- Norman, G.J.; Kolodziejczyk, J.K.; Adams, M.A.; Patrick, K.; Marshall, S.J. Fruit and vegetable intake and eating behaviors mediate the effect of a randomized text-message based weight loss program. Prev. Med. 2013, 56, 3–7. [Google Scholar] [CrossRef]
- Hammersley, M.L.; Okely, A.D.; Batterham, M.J.; Jones, R.A. Investigating the mediators and moderators of child body mass index change in the Time2bHealthy childhood obesity prevention program for parents of preschool-aged children. Public Health 2019, 173, 50–57. [Google Scholar] [CrossRef]
- Yιldιrιm, M.; Singh, A.S.; Velde, S.J.T.; van Stralen, M.M.; MacKinnon, D.P.; Brug, J.; van Mechelen, W.; Chinapaw, M.J. Mediators of longitudinal changes in measures of adiposity in teenagers using parallel process latent growth modeling. Obesity 2013, 21, 2387–2395. [Google Scholar] [CrossRef]
- Nicklas, T.A.; Baranowski, T.; Cullen, K.W.; Berenson, G. Eating Patterns, Dietary Quality and Obesity. J. Am. Coll. Nutr. 2001, 20, 599–608. [Google Scholar] [CrossRef]
- Eloranta, A.M.; Schwab, U.; Venäläinen, T.; Kiiskinen, S.; Lakka, H.M.; Laaksonen, D.E.; Lakka, T.A.; Lindi, V. Dietary quality indices in relation to cardiometabolic risk among Finnish children aged 6–8 years—The PANIC study. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 833–841. [Google Scholar] [CrossRef]
- Marshall, S.; Burrows, T.; Collins, C.E. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2014, 27, 577–598. [Google Scholar] [CrossRef]
- Lioret, S.; McNaughton, S.A.; Cameron, A.J.; Crawford, D.; Campbell, K.J.; Cleland, V.J.; Ball, K. Three-year change in diet quality and associated changes in BMI among schoolchildren living in socio-economically disadvantaged neighbourhoods. Br. J. Nutr. 2014, 112, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Berz, J.P.B.; Singer, M.R.; Guo, X.; Daniels, S.R.; Moore, L.L. Use of a DASH Food Group Score to Predict Excess Weight Gain in Adolescent Girls in the National Growth and Health Study. Arch. Pediatr. Adolesc. Med. 2011, 165, 540–546. [Google Scholar] [CrossRef]
- Okubo, H.; Crozier, S.R.; Harvey, N.C.; Godfrey, K.M.; Inskip, H.M.; Cooper, C.; Robinson, S.M. Diet quality across early childhood and adiposity at 6 years: The Southampton Women’s Survey. Int. J. Obes. 2015, 39, 1456–1462. [Google Scholar] [CrossRef] [PubMed]
- Duan, R.; Liu, Y.; Xue, H.; Yang, M.; Cheng, G. [Cross-sectional association between overall diet quality and overweight/obesity among children and adolescents in Chengdu]. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi 2014, 35, 994–998. [Google Scholar] [PubMed]
- Lee, S.Y.; Kim, J.; Oh, S.; Kim, Y.; Woo, S.; Jang, H.B.; Lee, H.-J.; Park, S.I.; Park, K.H.; Lim, H. A 24-week intervention based on nutrition care process improves diet quality, body mass index, and motivation in children and adolescents with obesity. Nutr. Res. 2020, 84, 53–62. [Google Scholar] [CrossRef]
- Wadolowska, L.; Hamulka, J.; Kowalkowska, J.; Ulewicz, N.; Hoffmann, M.; Gornicka, M.; Bronkowska, M.; Leszczynska, T.; Glibowski, P.; Korzeniowska-Ginter, R. Changes in Sedentary and Active Lifestyle, Diet Quality and Body Composition Nine Months after an Education Program in Polish Students Aged 11–12 Years: Report from the ABC of Healthy Eating Study. Nutrients 2019, 11, 331. [Google Scholar] [CrossRef]
- De Miguel-Etayo, P.; Moreno, L.A.; Santabárbara, J.; Martín-Matillas, M.; Azcona-San Julian, M.C.; Marti Del Moral, A.; Campoy, C.; Marcos, A.; Garagorri, J.M. Diet quality index as a predictor of treatment efficacy in overweight and obese adolescents: The EVASYON study. Clin. Nutr. 2019, 38, 782–790. [Google Scholar] [CrossRef]
- Liu, Z.; Gao, P.; Gao, A.Y.; Lin, Y.; Feng, X.X.; Zhang, F.; Xu, L.Q.; Niu, W.Y.; Fang, H.; Zhou, S.; et al. Effectiveness of a Multifaceted Intervention for Prevention of Obesity in Primary School Children in China: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2021, 176, e214375. [Google Scholar] [CrossRef]
- Van Stralen, M.M.; Yildirim, M.; te Velde, S.J.; Brug, J.; van Mechelen, W.; Chinapaw, M.J.M.; on behalf of the ENERGY-consortium. What works in school-based energy balance behaviour interventions and what does not? A systematic review of mediating mechanisms. Int. J. Obes. 2011, 35, 1251–1265. [Google Scholar] [CrossRef]
- Liu, Z.; Wu, Y.; Niu, W.-Y.; Feng, X.; Lin, Y.; Gao, A.; Zhang, F.; Fang, H.; Gao, P.; Li, H.-J.; et al. A school-based, multi-faceted health promotion programme to prevent obesity among children: Protocol of a cluster-randomised controlled trial (the DECIDE-Children study). BMJ Open 2019, 9, e027902. [Google Scholar] [CrossRef]
- Wang, W.P.; Cheng, H.; Zhao, X.Y.; Zhang, M.X.; Chen, F.F.; Hou, D.Q.; Jie, M.I.; Epidemiology, D.O. Reproducibility and validity of a food frequency questionnaire developed for children and adolescents in Beijing. Chin. J. Child Health Care 2016, 24, 8–11. [Google Scholar]
- Yan, Y.; Liu, J.; Zhao, X.; Cheng, H.; Huang, G.; Hou, D.; Mi, J.; China, C.; Adolescent Cardiovascular Health Collaboration Group. Cardiovascular health in urban Chinese children and adolescents. Ann. Med. 2019, 51, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.J.; Zeng, J.; Li, W.F.; Zhao, S.Q.; Liu, H.; Zhang, B.X.; Cheng, G.W. Dietary quality and influencing factors of migrant children in Wuhan in 2016. J. Hyg. Res. 2017, 46, 1008–1012. [Google Scholar]
- Duan, R.N.; Zhou, X.; Liu, Y. Evaluation of dietary balance index among children and adolescents aged 8–16 years old in Longquanyi District of Chengdu. Chin. J. Sch. Health 2014, 35, 979–982. [Google Scholar]
- Chinese Nutrition Society. Dietary Guidelines for Chinese 2007; Chinese Nutrition Society: Beijing, China, 2007. [Google Scholar]
- Yang, S.; Guo, H.W. Application of Diet Balance Index to Preschoolers’ Dietary Structure Evaluation in Beijing, Shanghai and Guangzhou. J. Environ. Occup. Med. 2013, 30, 167–170. [Google Scholar]
- Zheng, J.Q.; Zou, S.R.; Wei-Ying, D.U. Measurement of diet quality of pupils in Pudong new area using diet quality index. Mod. Prev. Med. 2010, 37, 813–817. [Google Scholar]
- Zhang, Q.; Qin, G.; Liu, Z.; Li, Z.; Li, J.; Varma, D.S.; Wan, Q.; Zhao, J.; Min, X.; Han, X.; et al. Dietary Balance Index-07 and the Risk of Anemia in Middle Aged and Elderly People in Southwest China: A Cross Sectional Study. Nutrients 2018, 10, 162. [Google Scholar] [CrossRef]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Screening for Overweight and Obesity Among School-Age Children and Adolescents; WS/T 586-2018; National Health Commission of the People’s Republic of China: Beijing, China, 2018.
- Bel-Serrat, S.; Ojeda-Rodríguez, A.; Heinen, M.M.; Buoncristiano, M.; Abdrakhmanova, S.; Duleva, V.; Sant’Angelo, V.F.; Fijałkowska, A.; Hejgaard, T.; Huidumac, C.; et al. Clustering of Multiple Energy Balance-Related Behaviors in School Children and its Association with Overweight and Obesity-WHO European Childhood Obesity Surveillance Initiative (COSI 2015–2017). Nutrients 2019, 11, 511. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Fairchild, A.J.; MacKinnon, D.P. A general model for testing mediation and moderation effects. Prev. Sci. 2009, 10, 87–99. [Google Scholar] [CrossRef]
- Tingley, D.; Yamamoto, T.; Hirose, K.; Keele, L.; Imai, K. Mediation: R Package for Causal Mediation Analysis. J. Stat. Softw. 2014, 59, 1–38. [Google Scholar] [CrossRef]
- Tofighi, D.; MacKinnon, D.P. RMediation: An R package for mediation analysis confidence intervals. Behav. Res. Methods 2011, 43, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Pallan, M.; Liu, W.J.; Hemming, K.; Frew, E.; Lin, R.; Liu, W.; Martin, J.; Zanganeh, M.; Hurley, K.; et al. The CHIRPY DRAGON intervention in preventing obesity in Chinese primary-school--aged children: A cluster-randomised controlled trial. PLoS Med. 2019, 16, e1002971. [Google Scholar] [CrossRef]
- Mâsse, L.C.; Naiman, D.; Naylor, P.J. From policy to practice: Implementation of physical activity and food policies in schools. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 71. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Guo, L.; Zhang, J.; Zhao, F.; Hu, Y.; Guo, Y.; Du, X.; Zhang, S.; Yang, X.; Lu, C. Effect of School-Based Family Health Education via Social Media on Children’s Myopia and Parents’ Awareness: A Randomized Clinical Trial. JAMA Ophthalmol. 2021, 139, 1165–1172. [Google Scholar] [CrossRef]
- Xu, H.; Ecker, O.; Zhang, Q.; Du, S.; Liu, A.; Li, Y.; Hu, X.; Li, T.; Guo, H.; Li, Y.; et al. The effect of comprehensive intervention for childhood obesity on dietary diversity among younger children: Evidence from a school-based randomized controlled trial in China. PLoS ONE 2020, 15, e0235951. [Google Scholar] [CrossRef]
- Kong, A.; Buscemi, J.; Stolley, M.R.; Schiffer, L.A.; Kim, Y.; Braunschweig, C.L.; Gomez-Perez, S.L.; Blumstein, L.B.; Van Horn, L.; Dyer, A.R.; et al. Hip-Hop to Health Jr. Randomized Effectiveness Trial: 1-Year Follow-up Results. Am. J. Prev. Med. 2016, 50, 136–144. [Google Scholar] [CrossRef]
- Santos, R.G.; Durksen, A.; Rabbanni, R.; Chanoine, J.P.; Lamboo Miln, A.; Mayer, T.; McGavock, J.M. Effectiveness of peer-based healthy living lesson plans on anthropometric measures and physical activity in elementary school students: A cluster randomized trial. JAMA Pediatrics 2014, 168, 330–337. [Google Scholar] [CrossRef]
- Dixon, L.B.; Tershakovec, A.M.; McKenzie, J.; Shannon, B. Diet quality of young children who received nutrition education promoting lower dietary fat. Public Health Nutr. 2000, 3, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Liberali, R.; Kupek, E.; Assis, M.A.A.d. Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child. Obes. 2019, 16, 70–85. [Google Scholar] [CrossRef]
- Fenton, S.; Burrows, T.L.; Collins, C.E.; Holliday, E.G.; Kolt, G.S.; Murawski, B.; Rayward, A.T.; Stamatakis, E.; Vandelanotte, C.; Duncan, M.J. Behavioural mediators of reduced energy intake in a physical activity, diet, and sleep behaviour weight loss intervention in adults. Appetite 2021, 165, 105273. [Google Scholar] [CrossRef] [PubMed]
- Vernarelli, J.A.; Mitchell, D.C.; Hartman, T.J.; Rolls, B.J. Dietary Energy Density Is Associated with Body Weight Status and Vegetable Intake in U.S. Children. J. Nutr. 2011, 141, 2204–2210. [Google Scholar] [CrossRef]
| Control (n = 571) | Intervention (n = 605) | p | |
|---|---|---|---|
| Cluster level | |||
| Number of schools | 12 | 12 | |
| Median (IQR) number of children/school | 37 (10.0) | 35 (9.5) | 0.213 |
| Individual level | |||
| Sex, n (%) | 0.585 | ||
| Male | 296 (51.8) | 304 (50.2) | |
| Female | 275 (48.2) | 301 (49.8) | |
| Region, n (%) | 0.749 | ||
| Beijing | 191 (33.4) | 215 (35.5) | |
| Changzhi of Shanxi | 170 (29.8) | 173 (28.6) | |
| Urumuqi of Xinjiang | 210 (36.8) | 217 (35.9) | |
| Age (years) | 9.61 (0.51) | 9.62 (0.54) | 0.875 |
| Anthropometric measures | |||
| BMI (kg/m2) | 18.19 (5.43) | 17.86 (4.97) | 0.286 |
| BMI z-score | 0.82 (2.24) | 0.74 (2.12) | 0.265 |
| WC (cm) | 63.95 (16.02) | 62.75 (14.00) | 0.336 |
| Body fat percentage (%) | 19.40 (15.85) | 18.70 (13.70) | 0.482 |
| Obesity b, n (%) | 0.406 | ||
| No | 428 (75.0) | 466 (77.0) | |
| Yes | 143 (25.0) | 139 (23.0) |
| Control, n (%) | Intervention, n (%) | Intervention vs. Control | ||||
|---|---|---|---|---|---|---|
| Baseline | End of Trial | Baseline | End of Trial | OR (95% CI) | p | |
| Under-intake | ||||||
| Cereals b | 398 (69.7) | 396 (69.4) | 418 (69.1) | 451 (74.5) | 1.33 (0.94, 1.88) | 0.107 |
| Vegetables | 478 (83.7) | 437 (76.5) | 496 (82.0) | 437 (72.2) | 0.82 (0.54, 1.24) | 0.346 |
| Fruits | 360 (63.0) | 360 (63.0) | 376 (62.1) | 361 (59.7) | 0.88 (0.65, 1.18) | 0.394 |
| Milk and dairy products | 471(82.5) | 422 (73.9) | 490 (81.0) | 461 (76.2) | 1.15 (0.81, 1.63) | 0.448 |
| Soybean and soybean products | 486 (85.1) | 482 (84.4) | 514 (85.0) | 516 (85.3) | 1.05 (0.75, 1.45) | 0.781 |
| Red meat, poultry, and game b | 325 (56.9) | 268 (46.9) | 335 (55.4) | 307 (50.7) | 1.19 (0.90, 1.57) | 0.212 |
| Fish and shrimp | 516 (90.4) | 521 (91.2) | 547 (90.4) | 556 (91.9) | 1.07 (0.67 1.72) | 0.780 |
| Eggs b | 246 (43.1) | 234 (41.0) | 246 (40.7) | 257 (42.5) | 1.08 (0.69, 1.67) | 0.755 |
| Drinking water | 433 (75.8) | 385 (67.4) | 430 (71.1) | 368 (60.8) | 0.73 (0.51, 1.03) | 0.073 |
| Over-intake | ||||||
| Cereals b | 136 (23.8) | 120 (21.0) | 150 (24.8) | 108 (17.9) | 0.80 (0.55, 1.16) | 0.246 |
| Red meat, poultry, and game b | 141 (24.7) | 167 (29.2) | 152 (25.1) | 172 (28.4) | 0.95 (0.69, 1.31) | 0.755 |
| Eggs b | 220 (38.5) | 229 (40.1) | 239 (39.5) | 245 (40.5) | 1.08 (0.69, 1.67) | 0.755 |
| Sugar-sweetened beverages | 207 (36.3) | 276 (48.3) | 249 (41.2) | 138 (22.8) | 0.27 (0.19, 0.40) | <0.001 * |
| Unhealthy snacks | 82 (14.4) | 91 (15.9) | 125 (20.7) | 64 (10.6) | 0.59 (0.37, 0.93) | 0.023 * |
| Dietary diversity | ||||||
| Inadequate dietary diversity | 559 (97.9) | 560 (98.1) | 592 (97.9) | 593 (98.0) | 0.97 (0.39, 2.42) | 0.943 |
| Control, Mean (SD) | Intervention, Mean (SD) | Changes from Baseline (Intervention vs. Control) | ||||
|---|---|---|---|---|---|---|
| Baseline | End of Trial | Baseline | End of Trial | Adjusted Mean Difference (95% CI) | p | |
| Higher bound scores (HBS) | 5.28 (5.70) | 5.89 (5.86) | 6.03 (6.04) | 4.51 (5.37) | −1.52 (−2.42, −0.62) | 0.005 * |
| Lower bound scores (LBS) | 34.61 (13.45) | 30.71 (12.25) | 32.66 (12.62) | 30.38 (12.45) | 0.01 (−2.27, 2.28) | 0.996 |
| Diet quality distance (DQD) | 39.90 (11.88) | 36.60 (10.49) | 38.68 (10.74) | 34.88 (11.43) | −1.50 (−3.72, 0.70) | 0.219 |
| BMI Change | BMI Z-Score Change | WC Change | BF% Change | |||||
|---|---|---|---|---|---|---|---|---|
| Estimates (95% CI) | p | Estimates (95% CI) | p | Estimates (95% CI) | p | Estimates (95% CI) | p | |
| HBS a,b | ||||||||
| Direct effect | −0.37 (−0.59, −0.16) | <0.001 * | −0.14 (−0.22, −0.06) | 0.002 * | −1.40 (−2.48, −0.33) | 0.010 * | −0.85 (−1.45, −0.26) | 0.008 * |
| Indirect effect | −0.02 (−0.04, 0.00) | 0.026 * | −0.01 (−0.01, 0.00) | 0.070 | −0.07 (−0.16, 0.00) | 0.030 * | −0.05 (−0.12, 0.00) | 0.026 * |
| Total effect | −0.39 (−0.61, −0.18) | <0.001 * | −0.15 (−0.24, −0.06) | <0.001 * | −1.47 (−2.54, −0.42) | 0.010 * | −0.90 (−1.50, −0.32) | 0.006 * |
| Proportion of mediation, % | 4.01 (0.31, 12.29) | 0.028 * | 3.46 (−0.15, 14.36) | 0.070 | 4.51 (0.21, 17.10) | 0.036 * | 5.67 (0.43, 19.41) | 0.028 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lyu, J.-L.; Liu, Z.; Zhou, S.; Feng, X.-X.; Lin, Y.; Gao, A.-Y.; Zhang, F.; Li, L.; Hebestreit, A.; Wang, H.-J. The Effect of a Multifaceted Intervention on Dietary Quality in Schoolchildren and the Mediating Effect of Dietary Quality between Intervention and Changes in Adiposity Indicators: A Cluster Randomized Controlled Trial. Nutrients 2022, 14, 3272. https://doi.org/10.3390/nu14163272
Lyu J-L, Liu Z, Zhou S, Feng X-X, Lin Y, Gao A-Y, Zhang F, Li L, Hebestreit A, Wang H-J. The Effect of a Multifaceted Intervention on Dietary Quality in Schoolchildren and the Mediating Effect of Dietary Quality between Intervention and Changes in Adiposity Indicators: A Cluster Randomized Controlled Trial. Nutrients. 2022; 14(16):3272. https://doi.org/10.3390/nu14163272
Chicago/Turabian StyleLyu, Jin-Lang, Zheng Liu, Shuang Zhou, Xiang-Xian Feng, Yi Lin, Ai-Yu Gao, Fang Zhang, Li Li, Antje Hebestreit, and Hai-Jun Wang. 2022. "The Effect of a Multifaceted Intervention on Dietary Quality in Schoolchildren and the Mediating Effect of Dietary Quality between Intervention and Changes in Adiposity Indicators: A Cluster Randomized Controlled Trial" Nutrients 14, no. 16: 3272. https://doi.org/10.3390/nu14163272
APA StyleLyu, J.-L., Liu, Z., Zhou, S., Feng, X.-X., Lin, Y., Gao, A.-Y., Zhang, F., Li, L., Hebestreit, A., & Wang, H.-J. (2022). The Effect of a Multifaceted Intervention on Dietary Quality in Schoolchildren and the Mediating Effect of Dietary Quality between Intervention and Changes in Adiposity Indicators: A Cluster Randomized Controlled Trial. Nutrients, 14(16), 3272. https://doi.org/10.3390/nu14163272







