Sex-Dependent Effects of the Intake of NOVA Classified Ultra-Processed Foods on Syndrome Metabolic Components in Brazilian Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Exposure Variable
2.3. Outcome Variable
2.4. Birth Variables
2.5. Socioeconomic, Demographic, and Lifestyle Variables at 23–25 Years
2.6. Data Analysis
2.7. Ethical Aspects
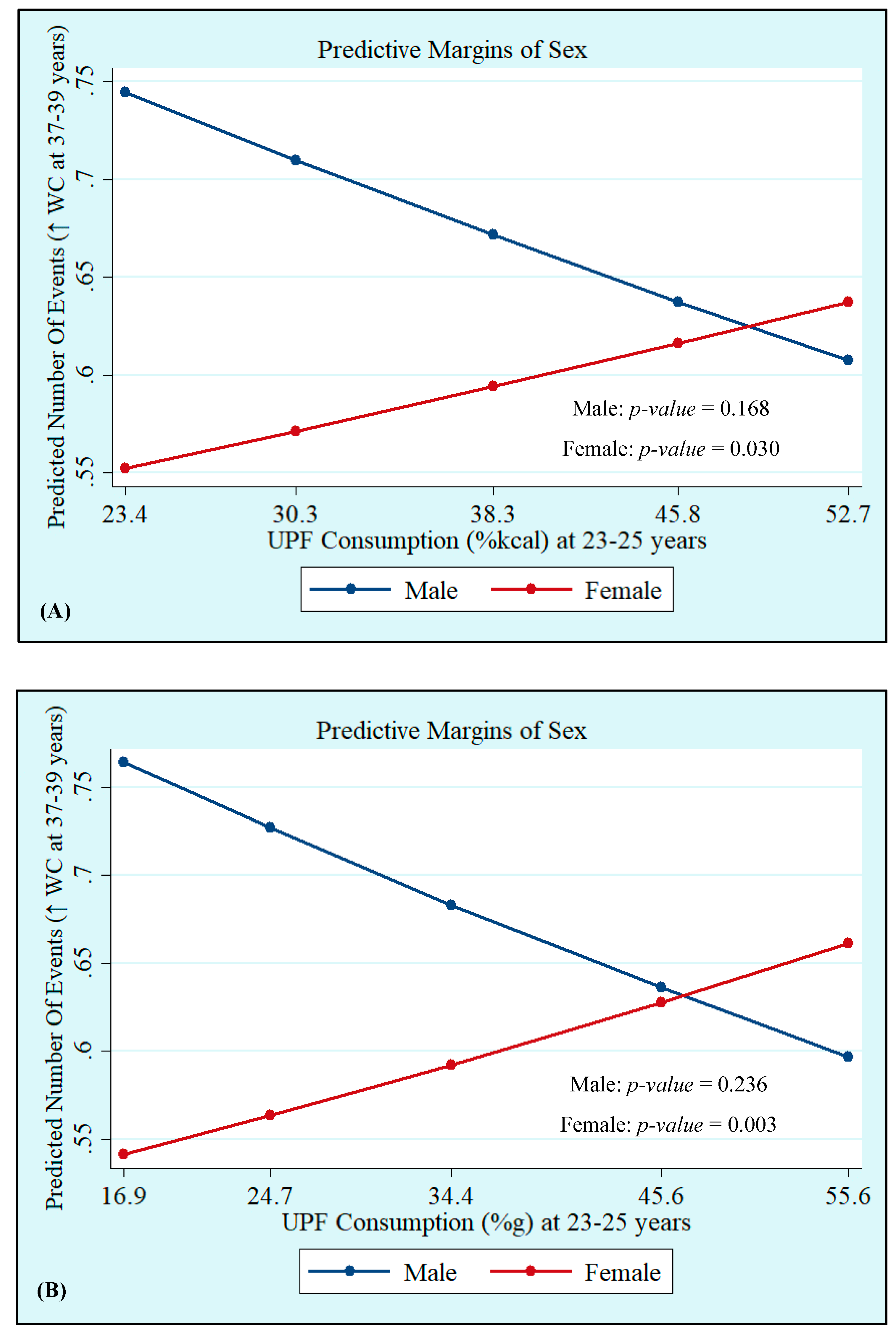
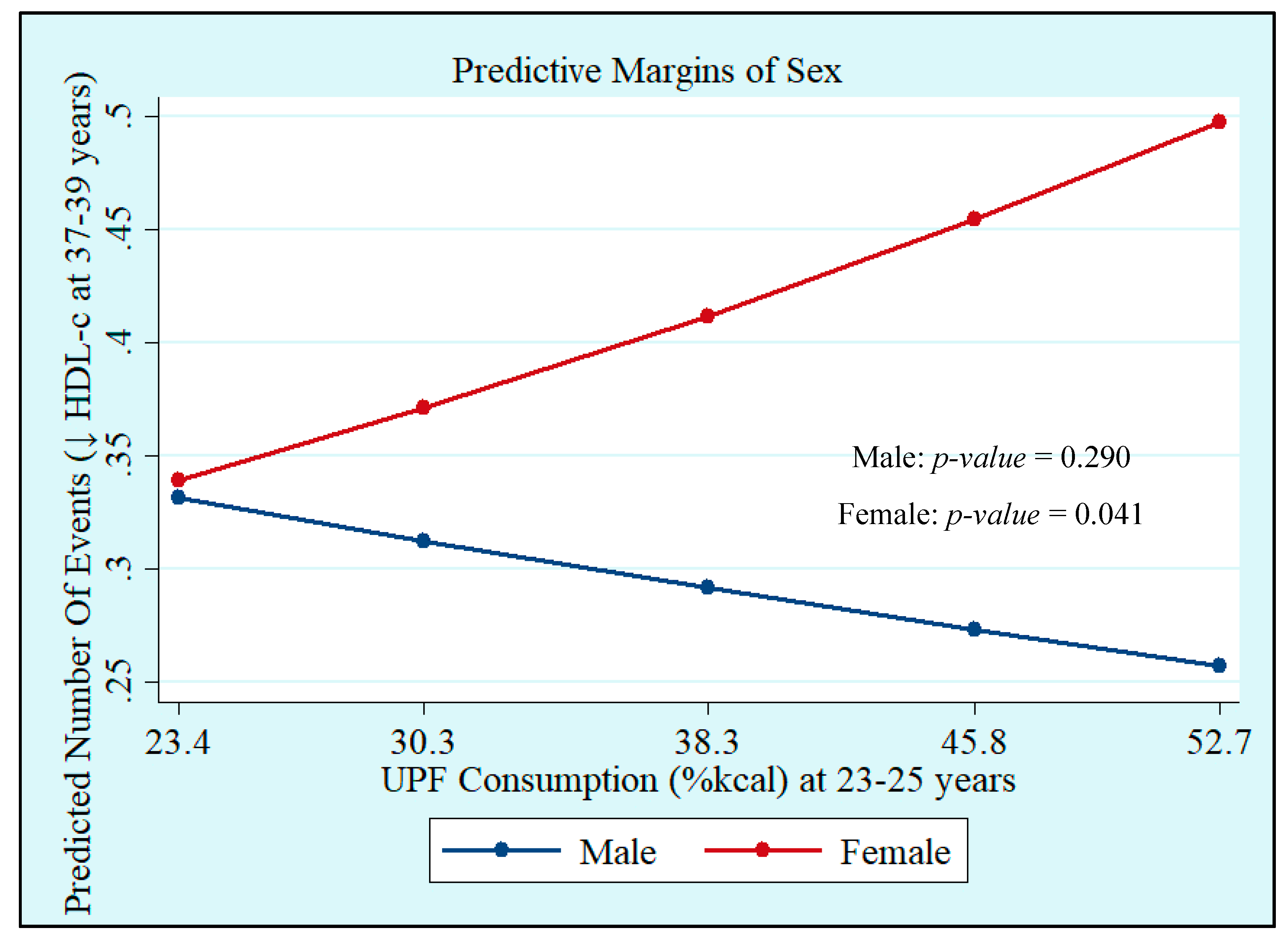
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Monteiro, C.A.; Cannon, G.; Lawrence, M.; Louzada, M.L.d.C.; Machado, P.P. Ultra-Processed Foods, Diet Quality, and Health Using the NOVA Classification System; FAO: Rome, Italy, 2019; p. 48. [Google Scholar]
- Organização Pan-Americana de Saúde (OPAS). Alimentos e Bebidas Ultraprocessados na América Latina: Tendências; Efeito na Obesidade e Implicações para Políticas Públicas: Brasília, Brazil, 2018; ISBN 9789275318645. [Google Scholar]
- Matos, R.A.; Adams, M.; Sabaté, J. Review: The Consumption of Ultra-Processed Foods and Non-communicable Diseases in Latin America. Front. Nutr. 2021, 8, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.X.; Chaudhary, N.; Akinyemiju, T. Metabolic Syndrome Prevalence by Race/ Ethnicity and Sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Prev. Chronic. Dis. 2017, 14, E24. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.H.; Lee, D.K.; Liu, M.; Portincasa, P.; Wang, D.Q.H. Novel insights into the pathogenesis and management of the metabolic syndrome. Pediatr. Gastroenterol. Hepatol. Nutr. 2020, 23, 189–230. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Martínez, P.; Mikhailidis, D.P.; Athyros, V.G.; Bullo, M.; Couture, P.; Covas, M.I.; de Koning, L.; Delgado-Lista, J.; Díaz-López, A.; Drevon, C.A.; et al. Lifestyle recommendations for the prevention and management of metabolic syndrome: An international panel recommendation. Nutr. Rev. 2017, 75, 307–326. [Google Scholar] [CrossRef]
- Lane, M.M.; Davis, J.A.; Beattie, S.; Gómez-Donoso, C.; Loughman, A.; O’Neil, A.; Jacka, F.; Berk, M.; Page, R.; Marx, W.; et al. Ultraprocessed food and chronic noncommunicable diseases: A systematic review and meta-analysis of 43 observational studies. Obes. Rev. 2021, 22, e13146. [Google Scholar] [CrossRef]
- Pagliai, G.; Dinu, M.; Madarena, M.P.; Bonaccio, M.; Iacoviello, L.; Sofi, F. Consumption of ultra-processed foods and health status: A systematic review and meta-Analysis. Br. J. Nutr. 2021, 125, 308–318. [Google Scholar] [CrossRef]
- Martínez Steele, E.; Juul, F.; Neri, D.; Rauber, F.; Monteiro, C.A. Dietary share of ultra-processed foods and metabolic syndrome in the US adult population. Prev. Med. 2019, 125, 40–48. [Google Scholar] [CrossRef]
- Lavigne-Robichaud, M.; Moubarac, J.C.; Lantagne-Lopez, S.; Johnson-Down, L.; Batal, M.; Sidi, E.A.L.; Lucas, M. Diet quality indices in relation to metabolic syndrome in an Indigenous Cree (Eeyouch) population in northern Québec, Canada. Public Health Nutr. 2018, 21, 172–180. [Google Scholar] [CrossRef]
- Ivancovsky-Wajcman, D.; Fliss-Isakov, N.; Webb, M.; Bentov, I.; Shibolet, O.; Kariv, R.; Zelber-Sagi, S. Ultra-processed food is associated with features of metabolic syndrome and non-alcoholic fatty liver disease. Liver Int. 2021, 41, 2635–2645. [Google Scholar] [CrossRef]
- De Miranda, R.C.; Rauber, F.; Levy, R.B. Impact of ultra-processed food consumption on metabolic health. Curr. Opin. Lipidol. 2021, 32, 24–37. [Google Scholar] [CrossRef]
- Barbieri, M.A.; Ferraro, A.A.; Simões, V.M.F.; Goldani, M.Z.; Cardoso, V.C.; Moura da Silva, A.A.; Bettiol, H. Cohort Profile: The 1978–79 Ribeirao Preto (Brazil) birth cohort study. Int. J. Epidemiol. 2022, 51, 27–28. [Google Scholar] [CrossRef]
- Barbieri, M.A.; Bettiol, H.; Silva, A.A.M.; Cardoso, V.C.; Simões, V.M.F.; Gutierrez, M.R.P.; Castro, J.A.S.; Vianna, E.S.O.; Foss, M.C.; Dos Santos, J.E.; et al. Health in early adulthood: The contribution of the 1978/79 Ribeirao Preto birth cohort. Brazilian J. Med. Biol. Res. 2006, 39, 1041–1055. [Google Scholar] [CrossRef]
- Ribeiro, A.B.; Cardoso, M.A. Development of a food frequency questionnaire as a tool for programs of chronic diseases prevention. Rev. Nutr. 2002, 15, 239–245. [Google Scholar] [CrossRef][Green Version]
- Monteiro, J.P.; Pfrimer, K.; Tremeschin, M.H.; Molina, M.C.; Chiarello, P. Consumo Alimentar: Visualizando Porções; Guanabara: Rio de Janeiro, Brasil, 2007. [Google Scholar]
- Zabotto, C.B.; Viana, R.P.T.; Gil, M.F. Registro Fotográfico Para Inquéritos Dietéticos: Utensílios e Porções. Available online: https://www.fcm.unicamp.br/fcm/sites/default/files/2016/page/manual_fotografico.pdf (accessed on 25 October 2021).
- U.S. Department of Agriculture Food Data Central. 2021. Available online: https://www.nal.usda.gov/fnic/food-composition (accessed on 25 October 2021).
- Instituto Brasileiro de Geografia e Estatística—IBGE. Pesquisa de Orçamentos Familiares 2008–2009: Tabela de Composição Nutricional dos Alimentos Consumidos No Brasil; IBGE: Rio de Janeiro, Brasil, 2011.
- Núcleo de Estudos e Pesquisas em Alimentação—NEPA. Tabela Brasileira de Composição de Alimentos; NEPA-UNICAMP: Campinas, Brasil, 2011; p. 161. [Google Scholar]
- Louzada, M.L.d.C.; Canella, D.S.; Jaime, P.C.; Monteiro, C.A. Alimentação e Saúde: A Fundamentação Científica do Guia Alimentar para a População Brasileira; Universidade de, Faculdade de Saude Publica: São Paulo, Brasil, 2019. [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística—IBGE. Pesquisa de Orçamentos Familiares 2002–2003: Primeiros Resultados Brasil e Grandes Regiões; IBGE: Rio de Janeiro, Brasil, 2004.
- Alberti, K.G.M.M.; Eckel, R.; Grundy, S.; Zimmet, P.; Cleeman, J.; Donato, K.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- Nordestgaard, B.G.; Langsted, A.; Mora, S.; Kolovou, G.; Baum, H.; Bruckert, E.; Watts, G.F.; Sypniewska, G.; Wiklund, O.; Borén, J.; et al. Fasting is not routinely required for determination of a lipid profile: Clinical and laboratory implications including flagging at desirable concentration cut-points—A joint consensus statement from the European Atherosclerosis Society and European Fede. Eur. Heart J. 2016, 37, 1944–1958. [Google Scholar] [CrossRef]
- Bowen, M.E.; Xuan, L.; Lingvay, I.; Halm, E.A. Doc, I Just Ate: Interpreting Random Blood Glucose Values in Patients with Unknown Glycemic Status. J. Gen. Intern. Med. 2018, 33, 142–144. [Google Scholar] [CrossRef]
- IPAQ Committee. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short and Long Forms; IPAQ Core Gruppetto: Pelotas, Brasil, 2005; pp. 1–15. [Google Scholar]
- Textor, J.; Hardt, J.; Knüppel, S. DAGitty: A graphical tool for analyzing causal diagrams. Epidemiology 2011, 22, 745. [Google Scholar] [CrossRef]
- Canella, D.S.; Louzada, M.L.d.C.; Claro, R.M.; Costa, J.C.; Bandoni, D.H.; Levy, R.B.; Martins, A.P.B. Consumption of vegetables and their relation with ultra-processed foods in Brazil. Rev. Saude Publica 2018, 52, 50. [Google Scholar] [CrossRef]
- Simões, B.d.S.; Barreto, M.S.; Molina, M.d.C.B.; Luft, V.C.; Ducan, B.B.; Schmidt, M.I.; Benseñor, I.J.M.; Cardoso, L.d.O.; Levy, R.B.; Giatti, L. Consumption of ultra-processed foods and socioeconomic position: A cross-sectional analysis of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Cad. Saude Publica 2018, 34, e00019717. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Levy, R.B.; Claro, R.M.; De Castro, I.R.R.; Cannon, G. Increasing consumption of ultra-processed foods and likely impact on human health: Evidence from Brazil. Public Health Nutr. 2010, 14, 5–13. [Google Scholar] [CrossRef]
- Bielemann, R.M.; Santos Motta, J.V.; Minten, G.C.; Horta, B.L.; Gigante, D.P. Consumption of ultra-processed foods and their impact on the diet of young adults. Rev. Saude Publica 2015, 49, 1–10. [Google Scholar] [CrossRef]
- Julia, C.; Martinez, L.; Allès, B.; Touvier, M.; Hercberg, S.; Méjean, C.; Kesse-Guyot, E. Contribution of ultra-processed foods in the diet of adults from the French NutriNet-Santé study. Public Health Nutr. 2018, 21, 27–37. [Google Scholar] [CrossRef]
- Rauber, F.; Louzada, M.L.D.C.; Martinez Steele, E.; De Rezende, L.F.M.; Millett, C.; Monteiro, C.A.; Levy, R.B. Ultra-processed foods and excessive free sugar intake in the UK: A nationally representative cross-sectional study. BMJ Open 2019, 9, 1–11. [Google Scholar] [CrossRef]
- Baraldi, L.G.; Martinez Steele, E.; Canella, D.S.; Monteiro, C.A. Consumption of ultra-processed foods and associated sociodemographic factors in the USA between 2007 and 2012: Evidence from a nationally representative cross-sectional study. BMJ Open 2018, 8, e020574. [Google Scholar] [CrossRef]
- Moubarac, J.-C.; Batal, M.; Louzada, M.L.; Steele, E.M.; Monteiro, C.A. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite 2017, 108, 512–520. [Google Scholar] [CrossRef]
- Shim, J.S.; Shim, S.Y.; Cha, H.J.; Kim, J.; Kim, H.C. Socioeconomic characteristics and trends in the consumption of ultra-processed foods in Korea from 2010 to 2018. Nutrients 2021, 13, 1120. [Google Scholar] [CrossRef]
- Silva, C.L.; Sousa, A.G.; Borges, L.P.S.L.; da Costa, T.H.M. Usual consumption of ultra-processed foods and its association with sex, age, physical activity, and body mass index in adults living in Brasília city, Brazil. Rev. Bras. Epidemiol. 2021, 24, E210033. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, L.; Kesse-Guyot, E.; Allès, B.; Touvier, M.; Srour, B.; Hercberg, S.; Buscail, C.; Julia, C. Association between Ultraprocessed Food Consumption and Risk of Mortality among Middle-aged Adults in France. JAMA Intern. Med. 2019, 179, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of ultra-processed foods and cancer risk: Results from NutriNet-Santé prospective cohort. Br. Med. J. 2018, 360, k322. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, L.; Buscail, C.; Sabate, J.M.; Bouchoucha, M.; Kesse-Guyot, E.; Allès, B.; Touvier, M.; Monteiro, C.A.; Hercberg, S.; Benamouzig, R.; et al. Association Between Ultra-Processed Food Consumption and Functional Gastrointestinal Disorders: Results From the French NutriNet-Santé Cohort. Am. J. Gastroenterol. 2018, 113, 1217–1228. [Google Scholar] [CrossRef] [PubMed]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed food intake and risk of cardiovascular disease: Prospective cohort study (NutriNet-Santé). Br. Med. J. 2019, 365, l1451. [Google Scholar] [CrossRef]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Debras, C.; Druesne-Pecollo, N.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultraprocessed Food Consumption and Risk of Type 2 Diabetes among Participants of the NutriNet-Santé Prospective Cohort. JAMA Intern. Med. 2019, 180, 283–291. [Google Scholar] [CrossRef]
- Adjibade, M.; Julia, C.; Allès, B.; Touvier, M.; Lemogne, C.; Srour, B.; Hercberg, S.; Galan, P.; Assmann, K.E.; Kesse-Guyot, E. Prospective association between ultra-processed food consumption and incident depressive symptoms in the French NutriNet-Santé cohort. BMC Med. 2019, 17, 78. [Google Scholar] [CrossRef]
- Expert Panel on Detection, E. Executive summary of the Third Report of the National Cholesterol Education Programme. JAMA 2001, 285, 2486–2497. [Google Scholar]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- Haverinen, E.; Paalanen, L.; Palmieri, L.; Padron-Monedero, A.; Noguer-Zambrano, I.; Suárez, R.S.; Tolonen, H. Comparison of metabolic syndrome prevalence using four definitions—A case study from Finland. Eur. J. Public Health 2021, 31, 164–413. [Google Scholar] [CrossRef]
- do Vale Moreira, N.C.; Hussain, A.; Bhowmik, B.; Mdala, I.; Siddiquee, T.; Fernandes, V.O.; Montenegro Júnior, R.M.; Meyer, H.E. Prevalence of Metabolic Syndrome by different definitions, and its association with type 2 diabetes, pre-diabetes, and cardiovascular disease risk in Brazil. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1217–1224. [Google Scholar] [CrossRef]
- Esmailzadehha, N.; Ziaee, A.; Kazemifar, A.M.; Ghorbani, A.; Oveisi, S. Prevalence of metabolic syndrome in Qazvin Metabolic Diseases Study (QMDS), Iran: A comparative analysis of six definitions. Endocr. Regul. 2013, 47, 111–120. [Google Scholar] [CrossRef]
- Ramli, A.S.; Daher, A.M.; Nor-Ashikin, M.N.K.; Mat-Nasir, N.; Ng, K.K.; Miskan, M.; Ambigga, K.S.; Ariffin, F.; Mazapuspavina, M.Y.; Abdul-Razak, S.; et al. JIS definition identified more malaysian adults with metabolic syndrome compared to the NCEP-ATP III and IDF criteria. Biomed. Res. Int. 2013, 2013, 760963. [Google Scholar] [CrossRef]
- Adejumo, E.N.; Ogundahunsi, O.A.; Adejumo, O.A.; Sotunsa, J.; Jagun, O. Prevalence of Metabolic Syndrome in a Rural and Urban Community in South-West Nigeria Using Three Different Definitions. Int. J. Trop. Dis. Health 2017, 24, 1–9. [Google Scholar] [CrossRef][Green Version]
- Mirmiran, P.; Moslehi, N.; Hosseinpanah, F.; Sarbazi, N.; Azizi, F. Dietary determinants of unhealthy metabolic phenotype in normal weight and overweight/obese adults: Results of a prospective study. Int. J. Food Sci. Nutr. 2020, 71, 891–901. [Google Scholar] [CrossRef] [PubMed]
- Cheraghi, Z.; Nedjat, S.; Mirmiran, P.; Moslehi, N.; Mansournia, N.; Etminan, M.; Mansournia, M.A.; McCandless, L.C. Effects of food items and related nutrients on metabolic syndrome using Bayesian multilevel modelling using the Tehran Lipid and Glucose Study (TLGS): A cohort study. BMJ Open 2018, 8, e020642. [Google Scholar] [CrossRef] [PubMed]
- Hosseinpour-Niazi, S.; Hosseini, S.; Mirmiran, P.; Azizi, F. Prospective study of nut consumption and incidence of metabolic syndrome: Tehran Lipid and glucose study. Nutrients 2017, 9, 1056. [Google Scholar] [CrossRef]
- Babio, N.; Becerra-Tomás, N.; Martínez-González, M.Á.; Corella, D.; Estruch, R.; Ros, E.; Sayón-Orea, C.; Fitá, M.; Serra-Majem, L.; Arós, F.; et al. Consumption of Yogurt, Low-FatMilk, and Other Low-Fat Dairy Products Is Associated with Lower Risk of Metabolic Syndrome Incidence in an Elderly Mediterranean Population1-3. J. Nutr. 2015, 145, 2308–2316. [Google Scholar]
- Sayón-Orea, C.; Bes-Rastrollo, M.; Martí, A.; Pimenta, A.M.; Martín-Calvo, N.; Martínez-González, M.A. Association between yogurt consumption and the risk of Metabolic Syndrome over 6 years in the SUN study Disease epidemiology—Chronic. BMC Public Health 2015, 15, 1–10. [Google Scholar] [CrossRef]
- Yoon, H.-J.; Lee, S.-K. The Incidence and Risk Factors of Metabolic Syndrome in Rural Area. J. Korea Acad. Coop. Soc. 2015, 16, 3934–3943. [Google Scholar]
- Mosley, M.A.; Andrade, F.C.D.; Aradillas-Garcia, C.; Teran-Garcia, M. Consumption of Dairy and Metabolic Syndrome Risk in a Convenient Sample of Mexican College Applicants. Food Nutr. Sci. 2013, 4, 56–65. [Google Scholar] [CrossRef]
- Sung, H.; Park, J.M.; Oh, S.U.; Ha, K.; Joung, H. Consumption of ultra-processed foods increases the likelihood of having obesity in Korean women. Nutrients 2021, 13, 698. [Google Scholar] [CrossRef]
- Juul, F.; Martinez-Steele, E.; Parekh, N.; Monteiro, C.A.; Chang, V.W. Ultra-processed food consumption and excess weight among US adults. Br. J. Nutr. 2018, 120, 90–100. [Google Scholar] [CrossRef]
- Mirrahimi, A.; Chiavaroli, L.; Srichaikul, K.; Augustin, L.S.A.; Sievenpiper, J.L.; Kendall, C.W.C.; Jenkins, D.J.A. The role of glycemic index and glycemic load in cardiovascular disease and its risk factors: A review of the recent literature. Curr. Atheroscler. Rep. 2014, 16, 1–10. [Google Scholar] [CrossRef]
- Nasreddine, L.; Tamim, H.; Itani, L.; Nasrallah, M.P.; Isma’eel, H.; Nakhoul, N.F.; Abou-Rizk, J.; Naja, F. A minimally processed dietary pattern is associated with lower odds of metabolic syndrome among Lebanese adults. Public Health Nutr. 2018, 21, 160–171. [Google Scholar] [CrossRef]
- Faludi, A.A.; Izar, M.C.O.; Saraiva, J.F.K.; Chacra, A.P.M.; Bianco, H.T.; Afiune Neto, A.; Bertolami, A.; Pereira, A.C.; Lottenberg, A.M.; Sposito, A.C.; et al. Diagnosis and treatment of rare complication after endomyocardial biopsy. Arq. Bras. Cardiol. 2017, 109, 1–76. [Google Scholar]
- Langsted, A.; Nordestgaard, B.G. Nonfasting versus fasting lipid profile for cardiovascular risk prediction. Pathology 2019, 51, 131–141. [Google Scholar] [CrossRef]
| UPF Consumption (%kcal) | UPF Consumption (%g) | ||||
|---|---|---|---|---|---|
| Variables | N (%) | Mean (SD) | p-Value | Mean (SD) | p-Value |
| Sex | <0.0001 a | 0.2592 a | |||
| Male | 397 (44.3) | 36.2 (10.8) | 35.0 (14.1) | ||
| Female | 499 (55.7) | 39.9 (11.1) | 36.1 (15.8) | ||
| Skin color | 0.0108 b | 0.3339 b | |||
| White | 583 (65.1) | 38.7 (11.1) | 36.0 (15.3) | ||
| Black | 47 (5.3) | 39.4 (10.6) | 36.6 (14.2) | ||
| Mixed Race | 255 (28.5) | 36.3 (11.8) | 34.7 (15.2) | ||
| Asian or Indigenous | 11 (1.2) | 40.9 (8.7) | 41.7 (12.9) | ||
| Age (years) | 0.6337 b | 0.8402 b | |||
| 23 | 273 (30.5) | 37.6 (11.8) | 35.7 (15.9) | ||
| 24 | 447 (49.9) | 38.3 (11.2) | 35.5 (14.7) | ||
| 25 | 176 (19.6) | 38.4 (11.0) | 36.2 (15.2) | ||
| Education (years of study) | 0.1742 b | 0.1281 b | |||
| 0 to 8 | 111 (12.4) | 37.5 (12.8) | 37.9 (17.8) | ||
| 9 to 11 | 461 (51.5) | 37.7 (11.6) | 35.7 (15.2) | ||
| ≥12 | 324 (36.2) | 39.0 (10.3) | 34.8 (13.9) | ||
| Marital status | 0.6555 a | 0.1054 a | |||
| With partner | 269 (30.0) | 38.0 (11.6) | 36.9 (15.9) | ||
| Without partner | 627 (70.0) | 38.4 (10.9) | 35.1 (14.6) | ||
| Family income (minimum wages) * | 0.1687 b | 0.8880 b | |||
| <5 | 287 (34.5) | 37.1 (11.2) | 35.3 (15.6) | ||
| 5 to 9.9 | 285 (34.3) | 38.5 (11.6) | 35.8 (14.7) | ||
| ≥10 | 259 (31.2) | 38.9 (10.8) | 35.3 (14.6) | ||
| Alcohol consumption | 0.0682 a | 0.0139 a | |||
| No | 91 (10.2) | 40.3 (12.2) | 39.3 (16.6) | ||
| Yes | 805 (89.8) | 38.1 (11.0) | 35.2 (14.8) | ||
| Smoking | 0.9006 a | 0.1077 a | |||
| No | 763 (85.2) | 38.3 (11.0) | 35.3 (14.8) | ||
| Yes | 133 (14.8) | 38.3 (12.0) | 37.6 (16.4) | ||
| Physical activity level * | 0.0507 b | 0.0004 b | |||
| High | 438 (49.0) | 37.3 (11.3) | 34.2 (14.6) | ||
| Moderate | 278 (31.1) | 38.4 (11.3) | 35.9 (15.7) | ||
| Low | 178 (19.9) | 39.5 (11.2) | 39.1 (15.1) | ||
| Total | 896 (100.0) | 38.3 (11.1) | 35.6 (15.0) | ||
| MetS | ↑ WC | ↑ Triglycerides | ↓ HDL-c | ↑ BP | ↑ Glucose | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | N (%) | p-Value | N (%) | p-Value | N (%) | p-Value | N (%) | p-Value | N (%) | p-Value | N (%) | p-Value |
| Sex | <0.0001 a | 0.074 a | <0.0001 a | 0.001 a | <0.0001 a | 0.013 a | ||||||
| Male | 179 (45.1) | 205 (66.1) | 171 (41.7) | 84 (28.4) | 122 (39.7) | 136 (30.0) | ||||||
| Female | 138 (27.7) | 220 (59.5) | 64 (13.2) | 119 (41.0) | 97 (19.2) | 121 (23.1) | ||||||
| Skin color | 0.961 b | 0.003 b | 0.784 b | 0.334 b | 0.517 b | 0.705 b | ||||||
| White | 204 (35.0) | 250 (58.3) | 149 (25.9) | 123 (32.6) | 136 (25.5) | 167 (25.9) | ||||||
| Black | 18 (38.3) | 26 (76.5) | 13 (28.3) | 9 (29.0) | 12 (28.6) | 16 (33.3) | ||||||
| Mixed race | 91 (35.7) | 145 (70.1) | 72 (27.3) | 68 (40.0) | 3 (37.5) | 71 (25.8) | ||||||
| Asian or Indigenous | 4 (36.4) | 4 (40.0) | 1 (11.1) | 3 (37.5) | 3 (27.3) | |||||||
| Age (years) | 0.845 a | 0.720 a | 0.561 a | 0.106 a | 0.898 a | 0.203 | ||||||
| 23 | 99 (36.3) | 142 (64.3) | 78 (28.7) | 43 (27.7) | 66 (26.2) | 72 (24.3) | ||||||
| 24 | 154 (34.5) | 200 (61.0) | 112 (25.1) | 117 (36.8) | 110 (27.7) | 123 (25.5) | ||||||
| 25 | 64 (36.4) | 83 (63.4) | 45 (25.4) | 43 (38.1) | 43 (26.4) | 62 (31.2) | ||||||
| Education (years of study) | 0.002 a | <0.0001 a | 0.084 a | 0.224 a | 0.109 a | 0.037 a | ||||||
| 0 to 8 | 45 (40.5) | 50 (69.4) | 32 (26.7) | 25 (39.7) | 31 (29.8) | 26 (29.7) | ||||||
| 9 to 11 | 182 (39.5) | 242 (69.3) | 134 (29.1) | 102 (37.0) | 122 (29.3) | 150 (20.8) | ||||||
| ≥12 | 90 (27.8) | 133 (51.4) | 69 (22.0) | 76 (30.8) | 66 (22.6) | 81 (26.3) | ||||||
| Marital status | 0.559 a | 0.034 a | 0.199 a | 0.790 a | 0.693 a | 0.560 a | ||||||
| With partner | 99 (36.8) | 123 (69.1) | 65 (23.5) | 52 (33.8) | 70 (27.9) | 82 (27.5) | ||||||
| Without partner | 218 (34.8) | 302 (60.2) | 170 (27.6) | 151 (35.0) | 149 (26.6) | 175 (25.7) | ||||||
| Family income (minimum wages) * | 0.007 a | <0.0001 a | 0.458 a | 0.037 a | 0.103 a | 0.055 a | ||||||
| <5 | 119 (41.5) | 144 (71.3) | 84 (29.0) | 71 (42.0) | 83 (31.2) | 90 (28.9) | ||||||
| 5 to 9.9 | 105 (36.8) | 146 (65.8) | 71 (24.4) | 61 (35.5) | 75 (28.4) | 91 (28.7) | ||||||
| ≥10 | 74 (28.6) | 104 (49.8) | 67 (27.1) | 61 (29.3) | 50 (22.6) | 59 (21.2) | ||||||
| Alcohol consumption | 0.852 a | 0.818 a | 0.132 a | 0.033 a | 0.592 a | 0.247 a | ||||||
| No | 33 (36.7) | 44 (63.8) | 17 (19.5) | 25 (33.3) | 25 (29.4) | 20 (21.3) | ||||||
| Yes | 284 (35.3) | 381 (62.4) | 218 (27.0) | 178 (48.1) | 194 (26.7) | 237 (26.8) | ||||||
| Smoking | 0.172 a | 0.737 a | 0.009 a | 0.237 a | 0.277 a | 0.949 a | ||||||
| No | 263 (34.7) | 364 (62.8) | 189 (24.7) | 179 (35.6) | 190 (27.7) | 217 (26.2) | ||||||
| Yes | 54 (40.6) | 61 (61.0) | 46 (35.7) | 24 (28.9) | 29 (23.0) | 40 (26.5) | ||||||
| Physical activity level * | 0.794 a | 0.164 a | 0.202 a | 0.863 a | 0.492 a | 0.222 a | ||||||
| High | 159 (36.3) | 211 (61.9) | 123 (28.0) | 105 (35.4) | 98 (26.1) | 128 (26.9) | ||||||
| Moderate | 94 (33.8) | 124 (59.1) | 73 (26.7) | 57 (33.0) | 76 (29.6) | 69 (22.9) | ||||||
| Low | 63 (35.4) | 88 (69.3) | 38 (21.1) | 40 (35.1) | 44 (24.9) | 59 (29.7) | ||||||
| Total | 317/896 (35.4) | 425/675 (63.0) | 235/853 (27.5) | 203/565 (35.9) | 219/774 (28.2) | 257/875 (29.4) | ||||||
| Outcomes/Exposures/Interactions | Crude RR (95% CI) | Adjusted RR (95% CI) |
|---|---|---|
| MetS | ||
| UPF (%kcal) | 0.99 (0.98–1.00) | 1.00 (0.99–1.01) a |
| UPF (%g) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) b |
| ↑ WC | ||
| UPF (%kcal) | ||
| UPF | 0.99 (0.98–1.00) | 0.99 (0.98–1.00) a |
| Sex | 0.61 (0.40–0.93) | 0.57 (0.38–0.85) a |
| UPF##Sex | 1.01 (1.00–1.02) | 1.01 (1.00–1.02) a |
| UPF (%g) | ||
| UPF | 1.00 (0.99–1.01) | 0.99 (0.98–1.00) b |
| Sex | 0.60 (0.44–0.81) | 0.57 (0.43–0.77) b |
| UPF##Sex | 1.01 (1.00–1.02) | 1.01 (1.00–1.02) b |
| ↑ Triglycerides | ||
| UPF (%kcal) | 0.99 (0.98–1.00) | 1.00 (0.99–1.01) a |
| UPF (%g) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) b |
| ↓ HDL-c | ||
| UPF (%kcal) | ||
| UPF | 0.99 (0.97–1.00) | 0.99 (0.98–1.01) a |
| Sex | 0.61 (0.27–1.38) | 0.66 (0.30–1.46) a |
| UPF##Sex | 1.02 (1.00–1.04) | 1.02 (1.01–1.04) a |
| UPF (%g) | 0.99 (0.98–1.01) | 0.99 (0.98–1.01) b |
| ↑ BP | ||
| UPF (%kcal) | 1.00 (0.99–1.01) | 1.01 (1.00–1.02) a |
| UPF (%g) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) b |
| ↑ Glucose | ||
| UPF (%kcal) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) a |
| UPF (%g) | 1.00 (0.99–1.01) | 0.99 (0.98–1.00) b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magalhães, E.I.d.S.; de Oliveira, B.R.; Rudakoff, L.C.S.; de Carvalho, V.A.; Viola, P.C.d.A.F.; Arruda, S.P.M.; de Carvalho, C.A.; Coelho, C.C.N.d.S.; Bragança, M.L.B.M.; Bettiol, H.; et al. Sex-Dependent Effects of the Intake of NOVA Classified Ultra-Processed Foods on Syndrome Metabolic Components in Brazilian Adults. Nutrients 2022, 14, 3126. https://doi.org/10.3390/nu14153126
Magalhães EIdS, de Oliveira BR, Rudakoff LCS, de Carvalho VA, Viola PCdAF, Arruda SPM, de Carvalho CA, Coelho CCNdS, Bragança MLBM, Bettiol H, et al. Sex-Dependent Effects of the Intake of NOVA Classified Ultra-Processed Foods on Syndrome Metabolic Components in Brazilian Adults. Nutrients. 2022; 14(15):3126. https://doi.org/10.3390/nu14153126
Chicago/Turabian StyleMagalhães, Elma Izze da Silva, Bianca Rodrigues de Oliveira, Lívia Carolina Sobrinho Rudakoff, Vitória Abreu de Carvalho, Poliana Cristina de Almeida Fonseca Viola, Soraia Pinheiro Machado Arruda, Carolina Abreu de Carvalho, Carla Cristine Nascimento da Silva Coelho, Maylla Luanna Barbosa Martins Bragança, Heloisa Bettiol, and et al. 2022. "Sex-Dependent Effects of the Intake of NOVA Classified Ultra-Processed Foods on Syndrome Metabolic Components in Brazilian Adults" Nutrients 14, no. 15: 3126. https://doi.org/10.3390/nu14153126
APA StyleMagalhães, E. I. d. S., de Oliveira, B. R., Rudakoff, L. C. S., de Carvalho, V. A., Viola, P. C. d. A. F., Arruda, S. P. M., de Carvalho, C. A., Coelho, C. C. N. d. S., Bragança, M. L. B. M., Bettiol, H., Barbieri, M. A., Cardoso, V. C., dos Santos, A. M., Levy, R. B., & da Silva, A. A. M. (2022). Sex-Dependent Effects of the Intake of NOVA Classified Ultra-Processed Foods on Syndrome Metabolic Components in Brazilian Adults. Nutrients, 14(15), 3126. https://doi.org/10.3390/nu14153126







