Effect of Cheese Intake on Cardiovascular Diseases and Cardiovascular Biomarkers
Abstract
:1. Introduction
2. Materials and Methods
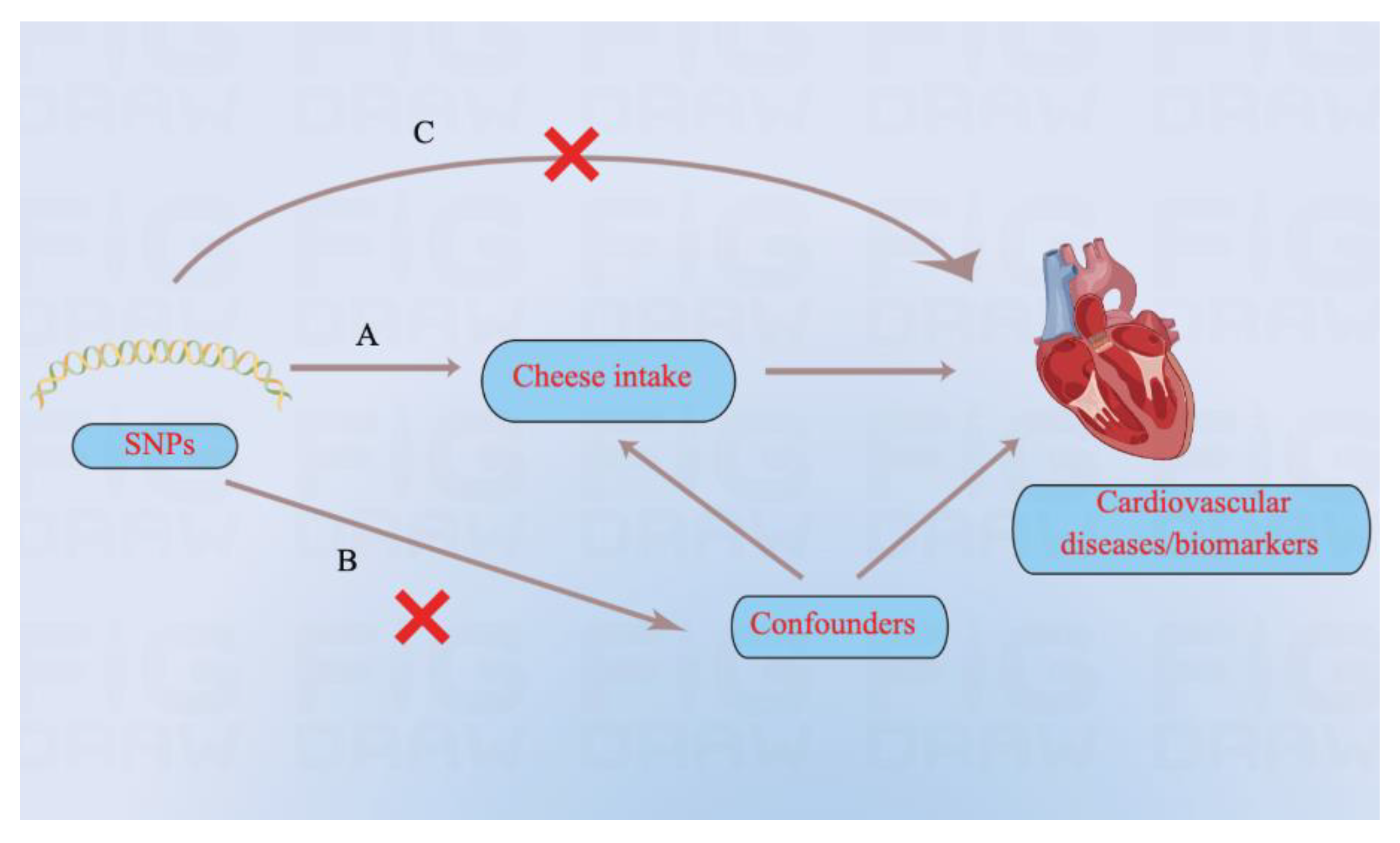
2.1. Study Design
2.2. Data Sources
2.3. Selection and Validation of SNPs
2.4. MR Analysis
3. Results
3.1. SNP Selection and Validation
3.2. Cardiovascular Diseases
3.3. Cardiovascular Biomarkers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviation
| BMI | body mass index |
| CI | confidence interval |
| CRP | C-reactive protein |
| DBP | diastolic blood pressure |
| GWAS | genome-wide association study |
| HDL | high-density lipoprotein |
| IV | instrumental variable |
| IVW | inverse-variance weighted |
| LDL | low-density lipoprotein |
| MR | Mendelian randomization |
| OR | odds ratio |
| RR | relative ratio |
| SBP | systolic blood pressure |
| SNP | single-nucleotide polymorphism |
References
- Tholstrup, T. Dairy products and cardiovascular disease. Curr. Opin. Lipidol. 2006, 17, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, A.H.; Appel, L.J.; Brands, M.; Carnethon, M.; Daniels, S.; Franch, H.A.; Franklin, B.; Kris-Etherton, P.; Harris, W.S.; Howard, B.; et al. Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation 2006, 114, 82–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perk, J.; De Backer, G.; Gohlke, H.; Graham, I.; Reiner, Z.; Verschuren, M.; Albus, C.; Benlian, P.; Boysen, G.; Cifkova, R.; et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur. Heart J. 2012, 33, 1635–1701. [Google Scholar] [CrossRef] [Green Version]
- de Souza, R.J.; Mente, A.; Maroleanu, A.; Cozma, A.I.; Ha, V.; Kishibe, T.; Uleryk, E.; Budylowski, P.; Schünemann, H.; Beyene, J.; et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: Systematic review and meta-analysis of observational studies. BMJ 2015, 351, h3978. [Google Scholar] [CrossRef] [Green Version]
- Siri-Tarino, P.W.; Sun, Q.; Hu, F.B.; Krauss, R.M. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am. J. Clin. Nutr. 2010, 91, 535–546. [Google Scholar] [CrossRef] [Green Version]
- Sluijs, I.; Forouhi, N.G.; Beulens, J.W.; van der Schouw, Y.T.; Agnoli, C.; Arriola, L.; Balkau, B.; Barricarte, A.; Boeing, H.; Bueno-de-Mesquita, H.B.; et al. The amount and type of dairy product intake and incident type 2 diabetes: Results from the EPIC-InterAct Study. Am. J. Clin. Nutr. 2012, 96, 382–390. [Google Scholar] [CrossRef] [Green Version]
- Michaëlsson, K.; Wolk, A.; Langenskiöld, S.; Basu, S.; Warensjö Lemming, E.; Melhus, H.; Byberg, L. Milk intake and risk of mortality and fractures in women and men: Cohort studies. BMJ 2014, 349, g6015. [Google Scholar] [CrossRef] [Green Version]
- Praagman, J.; Franco, O.H.; Ikram, M.A.; Soedamah-Muthu, S.S.; Engberink, M.F.; van Rooij, F.J.; Hofman, A.; Geleijnse, J.M. Dairy products and the risk of stroke and coronary heart disease: The Rotterdam Study. Eur. J. Nutr. 2015, 54, 981–990. [Google Scholar] [CrossRef]
- Key, T.J.; Appleby, P.N.; Bradbury, K.E.; Sweeting, M.; Wood, A.; Johansson, I.; Kühn, T.; Steur, M.; Weiderpass, E.; Wennberg, M.; et al. Consumption of Meat, Fish, Dairy Products, and Eggs and Risk of Ischemic Heart Disease. Circulation 2019, 139, 2835–2845. [Google Scholar] [CrossRef]
- Frank, A.P.; Clegg, D.J. JAMA PATIENT PAGE. Dietary Guidelines for Americans—Eat Less Sugar. JAMA 2016, 315, 1196. [Google Scholar] [CrossRef]
- Sun, D.; Zhou, T.; Heianza, Y.; Li, X.; Fan, M.; Fonseca, V.A.; Qi, L. Type 2 Diabetes and Hypertension. Circ. Res. 2019, 124, 930–937. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.S.; Hu, M.J.; Yang, Y.M.; Yang, Y.J. Genetic Predisposition to Low-Density Lipoprotein Cholesterol May Increase Risks of Both Individual and Familial Alzheimer’s Disease. Front. Med. 2021, 8, 798334. [Google Scholar] [CrossRef] [PubMed]
- Emdin, C.A.; Khera, A.V.; Kathiresan, S. Mendelian Randomization. JAMA 2017, 318, 1925–1926. [Google Scholar] [CrossRef]
- Sudlow, C.; Gallacher, J.; Allen, N.; Beral, V.; Burton, P.; Danesh, J.; Downey, P.; Elliott, P.; Green, J.; Landray, M.; et al. UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015, 12, e1001779. [Google Scholar] [CrossRef] [Green Version]
- Nikpay, M.; Goel, A.; Won, H.H.; Hall, L.M.; Willenborg, C.; Kanoni, S.; Saleheen, D.; Kyriakou, T.; Nelson, C.P.; Hopewell, J.C.; et al. A comprehensive 1,000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat. Genet. 2015, 47, 1121–1130. [Google Scholar] [CrossRef] [Green Version]
- Shah, S.; Henry, A.; Roselli, C.; Lin, H.; Sveinbjörnsson, G.; Fatemifar, G.; Hedman, Å.K.; Wilk, J.B.; Morley, M.P.; Chaffin, M.D.; et al. Genome-wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat. Commun. 2020, 11, 163. [Google Scholar] [CrossRef]
- Morris, A.P.; Voight, B.F.; Teslovich, T.M.; Ferreira, T.; Segrè, A.V.; Steinthorsdottir, V.; Strawbridge, R.J.; Khan, H.; Grallert, H.; Mahajan, A.; et al. Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat. Genet. 2012, 44, 981–990. [Google Scholar] [CrossRef]
- Malik, R.; Chauhan, G.; Traylor, M.; Sargurupremraj, M.; Okada, Y.; Mishra, A.; Rutten-Jacobs, L.; Giese, A.K.; van der Laan, S.W.; Gretarsdottir, S.; et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat. Genet. 2018, 50, 524–537. [Google Scholar] [CrossRef] [Green Version]
- Ligthart, S.; Vaez, A.; Võsa, U.; Stathopoulou, M.G.; de Vries, P.S.; Prins, B.P.; Van der Most, P.J.; Tanaka, T.; Naderi, E.; Rose, L.M.; et al. Genome Analyses of >200,000 Individuals Identify 58 Loci for Chronic Inflammation and Highlight Pathways that Link Inflammation and Complex Disorders. Am. J. Hum. Genet. 2018, 103, 691–706. [Google Scholar] [CrossRef] [Green Version]
- Folkersen, L.; Fauman, E.; Sabater-Lleal, M.; Strawbridge, R.J.; Frånberg, M.; Sennblad, B.; Baldassarre, D.; Veglia, F.; Humphries, S.E.; Rauramaa, R.; et al. Mapping of 79 loci for 83 plasma protein biomarkers in cardiovascular disease. PLoS Genet. 2017, 13, e1006706. [Google Scholar] [CrossRef]
- Dastani, Z.; Hivert, M.F.; Timpson, N.; Perry, J.R.; Yuan, X.; Scott, R.A.; Henneman, P.; Heid, I.M.; Kizer, J.R.; Lyytikäinen, L.P.; et al. Novel loci for adiponectin levels and their influence on type 2 diabetes and metabolic traits: A multi-ethnic meta-analysis of 45,891 individuals. PLoS Genet. 2012, 8, e1002607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machiela, M.J.; Chanock, S.J. LDlink: A web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics 2015, 31, 3555–3557. [Google Scholar] [CrossRef] [PubMed]
- Burgess, S.; Bowden, J.; Fall, T.; Ingelsson, E.; Thompson, S.G. Sensitivity Analyses for Robust Causal Inference from Mendelian Randomization Analyses with Multiple Genetic Variants. Epidemiology 2017, 28, 30–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowden, J.; Davey Smith, G.; Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 2015, 44, 512–525. [Google Scholar] [CrossRef] [Green Version]
- Astrup, A.; Dyerberg, J.; Elwood, P.; Hermansen, K.; Hu, F.B.; Jakobsen, M.U.; Kok, F.J.; Krauss, R.M.; Lecerf, J.M.; LeGrand, P.; et al. The role of reducing intakes of saturated fat in the prevention of cardiovascular disease: Where does the evidence stand in 2010? Am. J. Clin. Nutr. 2011, 93, 684–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, D.D.; Bylsma, L.C.; Vargas, A.J.; Cohen, S.S.; Doucette, A.; Mohamed, M.; Irvin, S.R.; Miller, P.E.; Watson, H.; Fryzek, J.P. Dairy consumption and CVD: A systematic review and meta-analysis. Br. J. Nutr. 2016, 115, 737–750. [Google Scholar] [CrossRef] [Green Version]
- Gao, D.; Ning, N.; Wang, C.; Wang, Y.; Li, Q.; Meng, Z.; Liu, Y.; Li, Q. Dairy products consumption and risk of type 2 diabetes: Systematic review and dose-response meta-analysis. PLoS ONE 2013, 8, e73965. [Google Scholar] [CrossRef]
- Guo, J.; Astrup, A.; Lovegrove, J.A.; Gijsbers, L.; Givens, D.I.; Soedamah-Muthu, S.S. Milk and dairy consumption and risk of cardiovascular diseases and all-cause mortality: Dose-response meta-analysis of prospective cohort studies. Eur. J. Epidemiol. 2017, 32, 269–287. [Google Scholar] [CrossRef] [Green Version]
- Ruan, H.; Tang, X.D.; Chen, M.L.; Joiner, M.L.; Sun, G.; Brot, N.; Weissbach, H.; Heinemann, S.H.; Iverson, L.; Wu, C.F.; et al. High-quality life extension by the enzyme peptide methionine sulfoxide reductase. Proc. Natl. Acad. Sci. USA 2002, 99, 2748–2753. [Google Scholar] [CrossRef] [Green Version]
- Hölscher, C.; Hölscher, A.; Rückerl, D.; Yoshimoto, T.; Yoshida, H.; Mak, T.; Saris, C.; Ehlers, S. The IL-27 receptor chain WSX-1 differentially regulates antibacterial immunity and survival during experimental tuberculosis. J. Immunol. 2005, 174, 3534–3544. [Google Scholar] [CrossRef]
- Rehwinkel, J.; Maelfait, J.; Bridgeman, A.; Rigby, R.; Hayward, B.; Liberatore, R.A.; Bieniasz, P.D.; Towers, G.J.; Moita, L.F.; Crow, Y.J.; et al. SAMHD1-dependent retroviral control and escape in mice. EMBO J. 2013, 32, 2454–2462. [Google Scholar] [CrossRef] [Green Version]
- Lüscher, T.F. Ageing, inflammation, and oxidative stress: Final common pathways of cardiovascular disease. Eur. Heart J. 2015, 36, 3381–3383. [Google Scholar] [CrossRef] [Green Version]
- Jacqmain, M.; Doucet, E.; Després, J.P.; Bouchard, C.; Tremblay, A. Calcium intake, body composition, and lipoprotein-lipid concentrations in adults. Am. J. Clin. Nutr. 2003, 77, 1448–1452. [Google Scholar] [CrossRef]
- Engberink, M.F.; Hendriksen, M.A.; Schouten, E.G.; van Rooij, F.J.; Hofman, A.; Witteman, J.C.; Geleijnse, J.M. Inverse association between dairy intake and hypertension: The Rotterdam Study. Am. J. Clin. Nutr. 2009, 89, 1877–1883. [Google Scholar] [CrossRef] [Green Version]
- Adebamowo, S.N.; Spiegelman, D.; Flint, A.J.; Willett, W.C.; Rexrode, K.M. Intakes of magnesium, potassium, and calcium and the risk of stroke among men. Int. J. Stroke 2015, 10, 1093–1100. [Google Scholar] [CrossRef]
- Cifelli, C.J. Looking beyond traditional nutrients: The role of bioactives and the food matrix on health. Nutr. Rev. 2021, 79, 1–3. [Google Scholar] [CrossRef]
- Togawa, J.; Nagase, H.; Tanaka, K.; Inamori, M.; Nakajima, A.; Ueno, N.; Saito, T.; Sekihara, H. Oral administration of lactoferrin reduces colitis in rats via modulation of the immune system and correction of cytokine imbalance. J. Gastroenterol. Hepatol. 2002, 17, 1291–1298. [Google Scholar] [CrossRef]
- Nieman, K.M.; Anderson, B.D.; Cifelli, C.J. The Effects of Dairy Product and Dairy Protein Intake on Inflammation: A Systematic Review of the Literature. J. Am. Coll. Nutr. 2021, 40, 571–582. [Google Scholar] [CrossRef]
- St-Onge, M.P.; Farnworth, E.R.; Jones, P.J. Consumption of fermented and nonfermented dairy products: Effects on cholesterol concentrations and metabolism. Am. J. Clin. Nutr. 2000, 71, 674–681. [Google Scholar] [CrossRef]
- Heller, K.J. Probiotic bacteria in fermented foods: Product characteristics and starter organisms. Am. J. Clin. Nutr. 2001, 73, 374s–379s. [Google Scholar] [CrossRef]
- Plessas, S.; Bosnea, L.; Alexopoulos, A.; Bezirtzoglou, E. Potential effects of probiotics in cheese and yogurt production: A review. Eng. Life Sci. 2012, 12, 433–440. [Google Scholar] [CrossRef]
- Pooyandjoo, M.; Nouhi, M.; Shab-Bidar, S.; Djafarian, K.; Olyaeemanesh, A. The effect of (L-)carnitine on weight loss in adults: A systematic review and meta-analysis of randomized controlled trials. Obes. Rev. 2016, 17, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Y.; Sun, J.; He, J.; Chen, F.; Chen, R.; Chen, H. Effect of Probiotics on Glycemic Control: A Systematic Review and Meta-Analysis of Randomized, Controlled Trials. PLoS ONE 2015, 10, e0132121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toscano, M.; De Grandi, R.; Pastorelli, L.; Vecchi, M.; Drago, L. A consumer’s guide for probiotics: 10 golden rules for a correct use. Dig. Liver Dis. 2017, 49, 1177–1184. [Google Scholar] [CrossRef] [PubMed]
- Nordestgaard, B.G.; Tybjaerg-Hansen, A. IDL, VLDL, chylomicrons and atherosclerosis. Eur. J. Epidemiol. 1992, 8 (Suppl. 1), 92–98. [Google Scholar] [CrossRef]
- St-Pierre, A.C.; Cantin, B.; Dagenais, G.R.; Mauriège, P.; Bernard, P.M.; Després, J.P.; Lamarche, B. Low-density lipoprotein subfractions and the long-term risk of ischemic heart disease in men: 13-year follow-up data from the Québec Cardiovascular Study. Arter. Thromb. Vasc. Biol. 2005, 25, 553–559. [Google Scholar] [CrossRef] [Green Version]
- Sjogren, P.; Rosell, M.; Skoglund-Andersson, C.; Zdravkovic, S.; Vessby, B.; de Faire, U.; Hamsten, A.; Hellenius, M.L.; Fisher, R.M. Milk-derived fatty acids are associated with a more favorable LDL particle size distribution in healthy men. J. Nutr. 2004, 134, 1729–1735. [Google Scholar] [CrossRef] [Green Version]
- Inoue, N.; Nagao, K.; Hirata, J.; Wang, Y.M.; Yanagita, T. Conjugated linoleic acid prevents the development of essential hypertension in spontaneously hypertensive rats. Biochem. Biophys. Res. Commun. 2004, 323, 679–684. [Google Scholar] [CrossRef]
- Kritchevsky, D.; Tepper, S.A.; Wright, S.; Tso, P.; Czarnecki, S.K. Influence of conjugated linoleic acid (CLA) on establishment and progression of atherosclerosis in rabbits. J. Am. Coll. Nutr. 2000, 19, 472s–477s. [Google Scholar] [CrossRef]
- Kromhout, D.; Spaaij, C.J.; de Goede, J.; Weggemans, R.M. The 2015 Dutch food-based dietary guidelines. Eur. J. Clin. Nutr. 2016, 70, 869–878. [Google Scholar] [CrossRef]
- Fumeron, F.; Lamri, A.; Abi Khalil, C.; Jaziri, R.; Porchay-Baldérelli, I.; Lantieri, O.; Vol, S.; Balkau, B.; Marre, M. Dairy consumption and the incidence of hyperglycemia and the metabolic syndrome: Results from a french prospective study, Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care 2011, 34, 813–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattar, R.; de Campos Mazo, D.F.; Carrilho, F.J. Lactose intolerance: Diagnosis, genetic, and clinical factors. Clin. Exp. Gastroenterol. 2012, 5, 113–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Outcome | Weighted Median | MR-Egger | Pleiotropy | Heterogeneity | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | Intercept | p | Q | p | |
| Coronary heart disease | 0.65 (0.51–0.84) | 0.001 | 1.14 (0.49–2.66) | 0.757 | −0.010 | 0.18 | 84 | 0.02 |
| Hypertension | 0.73 (0.55–0.96) | 0.023 | 1.45 (0.55–3.82) | 0.450 | −0.014 | 0.11 | 107 | <0.01 |
| Atrial fibrillation | 0.83 (0.50–1.39) | 0.483 | 2.59 (0.47–14.15) | 0.277 | −0.021 | 0.15 | 80 | 0.04 |
| Heart failure | 0.85 (0.67–1.08) | 0.172 | 0.85 (0.31–2.34) | 0.750 | −0.005 | 0.54 | 135 | <0.01 |
| Type 2 diabetes | 0.67 (0.51–0.90) | 0.007 | 1.65 (0.39–7.03) | 0.50 | −0.021 | 0.08 | 153 | <0.01 |
| Transient ischemic attack | 0.86 (0.56–1.32) | 0.487 | 1.06 (0.31–3.70) | 0.924 | −0.003 | 0.79 | 51 | 0.77 |
| Ischemic stroke | 0.71 (0.55–0.91) | 0.008 | 1.17 (0.55–2.48) | 0.679 | −0.008 | 0.25 | 80 | 0.04 |
| Pulmonary embolism | 0.81 (0.44–1.48) | 0.497 | 0.45 (0.07–3.04) | 0.417 | 0.010 | 0.55 | 68 | 0.19 |
| Peripheral artery disease | 0.72 (0.43–1.20) | 0.207 | 0.57 (0.11–3.11) | 0.520 | 0.003 | 0.86 | 82 | 0.03 |
| Cardiac death | 0.74 (0.45–1.20) | 0.223 | 1.24 (0.29–5.23) | 0.772 | −0.009 | 0.49 | 52 | 0.73 |
| Outcome | Weighted Median | MR-Egger | Pleiotropy | Heterogeneity | ||||
|---|---|---|---|---|---|---|---|---|
| Effect Estimate (95% CI) | p | Effect Estimate (95% CI) | p | Intercept | p | Q | p | |
| Systolic blood pressure | −1.14 (from −2.17 to −0.11) | 0.030 | 0.09 (from −7.17 to 7.35) | 0.981 | −0.026 | 0.68 | 593 | <0.01 |
| Diastolic blood pressure | −0.52 (from −1.12 to 0.09) | 0.094 | 1.34 (from −3.37 to 6.06) | 0.579 | −0.032 | 0.43 | 765 | <0.01 |
| Body mass index | −0.30 (from −0.48 to −0.12) | 0.001 | −0.65 (from −2.20 to 0.89) | 0.416 | 0.001 | 0.92 | 250 | <0.01 |
| Waist circumference | −0.39 (from −0.59 to −0.19) | <0.001 | −0.45 (from −1.76 to 0.86) | 0.508 | −0.001 | 0.95 | 136 | <0.01 |
| C-Reactive protein | −0.25 (from −0.43 to −0.06) | 0.009 | −0.27 (from −1.58 to 1.03) | 0.688 | 0.001 | 0.94 | 135 | <0.01 |
| Interleukin 6 | −0.23 (from −1.02 to 0.55) | 0.564 | −0.40 (from −2.88 to 2.07) | 0.750 | 0.006 | 0.79 | 42 | 0.77 |
| Adiponectin | −0.04 (from −0.23 to 0.14) | 0.639 | −0.51 (from −1.33 to 0.30) | 0.228 | 0.007 | 0.26 | 41 | 0.02 |
| Total cholesterol | −0.13 (from −0.35 to 0.09) | 0.245 | 0.82 (from −0.20 to 1.84) | 0.130 | −0.014 | 0.10 | 62 | <0.01 |
| Triglycerides | −0.40 (from −0.59 to −0.21) | <0.001 | −0.71 (from −1.49 to 0.07) | 0.087 | 0.006 | 0.34 | 38 | 0.02 |
| HDL | 0.21 (from 0 to 0.43) | 0.054 | 2.04 (from 0.56 to 3.51) | 0.013 | −0.027 | 0.03 | 157 | <0.01 |
| LDL | −0.16 (from −0.37 to 0.05) | 0.133 | 0.18 (from −0.71 to 1.08) | 0.690 | −0.006 | 0.44 | 40 | 0.01 |
| Fasting glucose | −0.30 (from −0.46 to −0.14) | <0.001 | −0.05 (from −0.68 to 0.59) | 0.881 | −0.002 | 0.64 | 37 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, M.-J.; Tan, J.-S.; Gao, X.-J.; Yang, J.-G.; Yang, Y.-J. Effect of Cheese Intake on Cardiovascular Diseases and Cardiovascular Biomarkers. Nutrients 2022, 14, 2936. https://doi.org/10.3390/nu14142936
Hu M-J, Tan J-S, Gao X-J, Yang J-G, Yang Y-J. Effect of Cheese Intake on Cardiovascular Diseases and Cardiovascular Biomarkers. Nutrients. 2022; 14(14):2936. https://doi.org/10.3390/nu14142936
Chicago/Turabian StyleHu, Meng-Jin, Jiang-Shan Tan, Xiao-Jin Gao, Jin-Gang Yang, and Yue-Jin Yang. 2022. "Effect of Cheese Intake on Cardiovascular Diseases and Cardiovascular Biomarkers" Nutrients 14, no. 14: 2936. https://doi.org/10.3390/nu14142936
APA StyleHu, M.-J., Tan, J.-S., Gao, X.-J., Yang, J.-G., & Yang, Y.-J. (2022). Effect of Cheese Intake on Cardiovascular Diseases and Cardiovascular Biomarkers. Nutrients, 14(14), 2936. https://doi.org/10.3390/nu14142936






