Motivation and Limiting Factors for Adherence to Weight Loss Interventions among Patients with Obesity in Primary Care
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Sample Size Determination
2.3. Research Variables
2.4. Ethical Considerations
2.5. Data Processing and Statistical Analysis
3. Results
3.1. General Characteristics of the Participants
3.2. Motivation for Adherence to Weight Loss Interventions
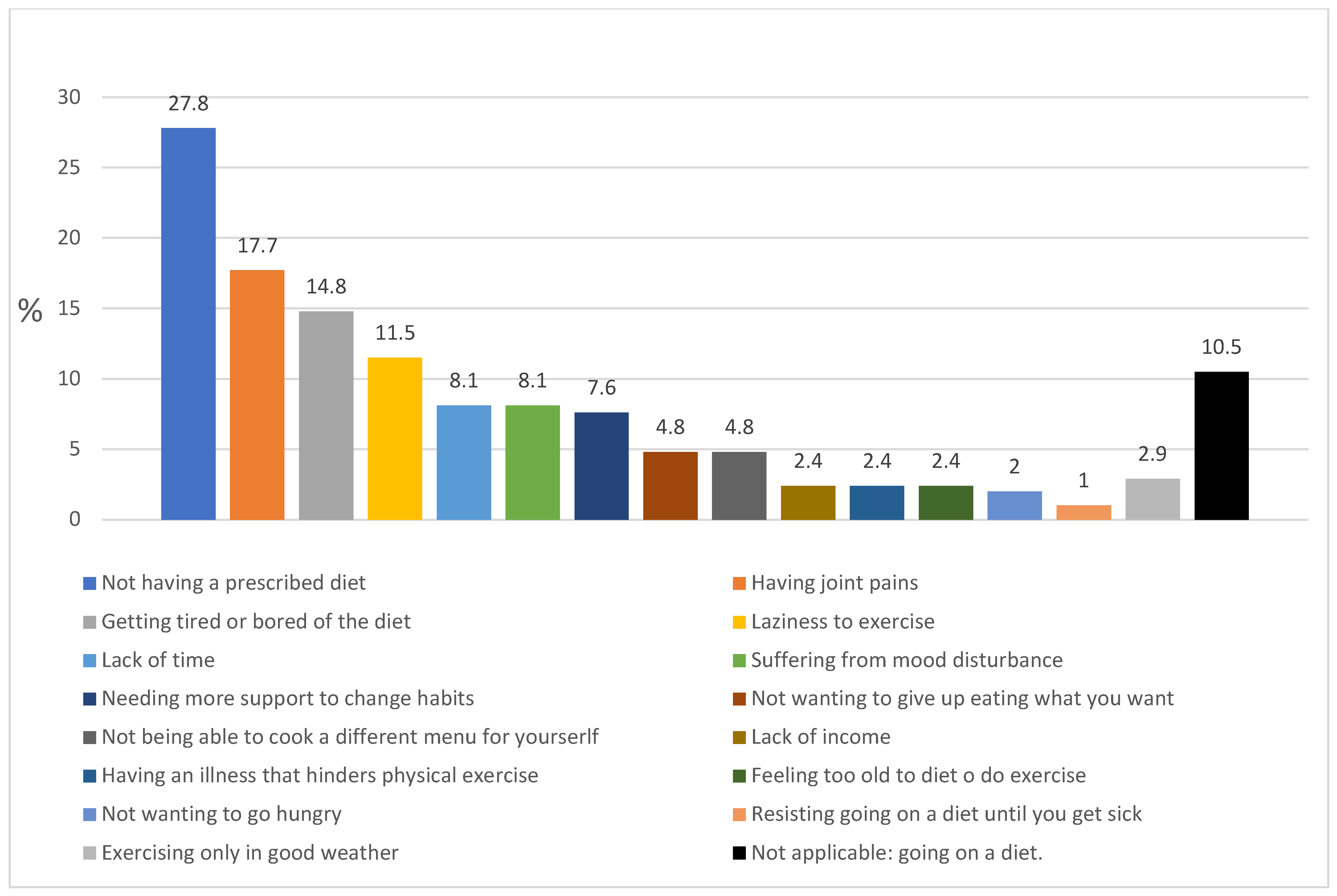
3.3. Limiting Factors for Weight Loss Mentioned by the Patients
3.4. Relationship between Limiting Factors and Motivation to Lose Weight, with Sex, Age and BMI of the Participants
3.5. Relationship between Limiting Factors and Motivation to Lose Weight
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Personal Interview Questions
| Questions aimed at assessing patient motivation to lose weight. | |
| |
| |
| Questions aimed at assessing limiting factors to adhere to a weight loss program. | |
| Close-ended questions: |
|
| |
| Open-ended question:* |
|
| Question aimed at identifying patients who resorted to dieting on their own initiative without the intervention of their primary care physician or endocrinologist. | |
| |
| * The open-ended question was formulated when answers 1 and 2 were affirmative. | |
References
- Flint, S.W.; Colosio, A. Reframing obesity health care from policy to practice: A call for papers. EClinicalMedicine 2022, 43, 101256. [Google Scholar] [CrossRef]
- Schutz, D.D.; Busetto, L.; Dicker, D.; Farpour-Lambert, N.; Pryke, R.; Toplak, H.; Widmer, D.; Yumuk, V.; Schutz, Y. European Practical and Patient-Centred Guidelines for Adult Obesity Management in Primary Care. Obes. Facts 2019, 12, 40–66. [Google Scholar]
- Gallo, S.; Cheskin, L.J. Treatment of Obesity: Beyond the Diet. Gastroenterol. Clin. N. Am. 2021, 50, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Ingersoll, A.B. Current Evidence-Based Treatment of Obesity. Nurs. Clin. N. Am. 2021, 56, 495–509. [Google Scholar] [CrossRef]
- Kheniser, K.; Saxon, D.R.; Kashyap, S.R. Long-Term Weight Loss Strategies for Obesity. J. Clin. Endocrinol. Metab. 2021, 106, 1854–1866. [Google Scholar] [CrossRef]
- Wharton, S.; Lau, D.C.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boulé, N.; et al. Obesity in adults: A clinical practice guideline. Can. Med. Assoc. J. 2020, 192, E875–E891. [Google Scholar] [CrossRef]
- Ryan, D.H.; Kahan, S. Guideline Recommendations for Obesity Management. Med. Clin. N. Am. 2018, 102, 49–63. [Google Scholar] [CrossRef]
- Semlitsch, T.; Stigler, F.L.; Jeitler, K.; Horvath, K.; Siebenhofer-Kroitzsch, A. Management of overweight and obesity in primary care—A systematic overview of international evidence-based guidelines. Obes. Rev. 2019, 20, 1218–1230. [Google Scholar] [CrossRef]
- Trujillo-Garrido, N.; Bernal-Jiménez, M.; Santi-Cano, M.J. Evaluation of Obesity Management Recorded in Electronic Clinical History: A Cohort Study. J. Clin. Med. 2020, 9, 2345. [Google Scholar] [CrossRef]
- Wadden, T.A.; Butryn, M.L.; Hong, P.S.; Tsai, A.G. Behavioral Treatment of Obesity in Patients Encountered in Primary Care Settings: A Systematic Review. JAMA 2014, 312, 1779–1791. [Google Scholar] [CrossRef]
- Greaney, M.L.; Cohen, S.A.; Xu, F.; Ward-Ritacco, C.L.; Riebe, D. Original research: Healthcare provider counselling for weight management behaviours among adults with overweight or obesity: A cross-sectional analysis of National Health and Nutrition Examination Survey, 2011–2018. BMJ Open 2020, 10, e039295. [Google Scholar] [CrossRef] [PubMed]
- Bailey-Davis, L.; Pinto, A.M.; Hanna, D.J.; Rethorst, C.D.; Still, C.D.; Foster, G.D. Qualitative inquiry with primary care providers and specialists about adult weight management care and referrals. Transl. Behav. Med. 2022, 12, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.A.; Ahern, A.L.; Kasetty, H.; McGowan, B.M.; Parretti, H.M.; Vincent, A.; Halford, J.C.G. Changing the narrative around obesity in the UK: A survey of people with obesity and healthcare professionals from the ACTION-IO study. BMJ Open 2021, 11, e045616. [Google Scholar] [CrossRef] [PubMed]
- Rubino, F.; Puhl, R.M.; Cummings, D.E.; Eckel, R.H.; Ryan, D.H.; Mechanick, J.I.; Nadglowski, J.; Ramos Salas, X.; Schauer, P.R.; Twenefour, D.; et al. Joint international consensus statement for ending stigma of obesity. Nat. Med. 2020, 26, 485–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flint, S.W. Time to end weight stigma in healthcare. EClinicalMedicine 2021, 34, 100810. [Google Scholar] [CrossRef]
- Booth, H.P.; Prevost, A.T.; Gulliford, M.C. Access to weight reduction interventions for overweight and obese patients in UK primary care: Population-based cohort study. BMJ Open 2015, 5, e006642. [Google Scholar] [CrossRef] [Green Version]
- Krippendorff, K. Content Analysis: An Introduction to Its Methodology, 2nd ed.; SAGE Publications: Thousand Oaks, CA, USA, 2004. [Google Scholar]
- Dicker, D.; Alfadda, A.A.; Coutinho, W.; Cuevas, A.; Halford, J.C.; Hughes, C.A.; Iwabu, M.; Kang, J.-H.; Nawar, R.; Reynoso, R.; et al. Patient motivation to lose weight: Importance of healthcare professional support, goals and self-efficacy. Eur. J. Intern. Med. 2021, 91, 10–16. [Google Scholar] [CrossRef]
- Pearl, R.L.; Puhl, R.M. Weight bias internalization and health: A systematic review. Obes. Rev. 2018, 19, 1141–1163. [Google Scholar] [CrossRef] [Green Version]
- Zhu, X.; Smith, R.A.; Buteau, E. A meta-analysis of weight stigma and health behaviors. Stigma Health 2022, 7, 1–13. [Google Scholar] [CrossRef]
- Lim, S.; Smith, C.A.; Costello, M.F.; Macmillan, F.; Moran, L.; Ee, C. Barriers and facilitators to weight management in overweight and obese women living in Australia with PCOS: A qualitative study. BMC Endocr. Disord. 2019, 19, 106. [Google Scholar] [CrossRef]
- Yumuk, V.; Tsigos, C.; Fried, M.; Schindler, K.; Busetto, L.; Micic, D.; Toplak, H. European Guidelines for Obesity Management in Adults. Obes. Facts 2015, 8, 402–424. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014, 129, S102–S138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, A.M.; Bélanger, A.; Carson, V.; Krah, J.; Langlois, M.; Lawlor, D.; Lepage, S.; Liu, A.; Macklin, D.A.; MacKay, N.; et al. Perceptions of barriers to effective obesity management in Canada: Results from the ACTION study. Clin. Obes. 2019, 9, e12329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryan, D.; Heaner, M. Guidelines (2013) for managing overweight and obesity in adults. Preface to the full report. Obesity 2014, 22, S1–S3. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, L.J.; Ball, L.E.; Ross, L.J.; Barnes, K.A.; Williams, L.T. Effectiveness of Dietetic Consultations in Primary Health Care: A Systematic Review of Randomized Controlled Trials. J. Acad. Nutr. Diet. 2017, 117, 1941–1962. [Google Scholar] [CrossRef] [Green Version]
- Ang, S.M.; Chen, J.; Liew, J.H.; Johal, J.; Dan, Y.Y.; Allman-Farinelli, M.; Lim, S.L. Efficacy of Interventions That Incorporate Mobile Apps in Facilitating Weight Loss and Health Behavior Change in the Asian Population: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e28185. [Google Scholar] [CrossRef]
- Seward, M.W.; Chen, A.F. Obesity, preoperative weight loss, and telemedicine before total joint arthroplasty: A review. Arthroplasty 2022, 4, 2. [Google Scholar] [CrossRef]
- Lim, K.; Chan, S.-Y.; Lim, S.L.; Tai, B.C.; Tsai, C.; Wong, S.R.; Ang, S.M.; Yew, T.W.; Tai, E.S.; Yong, E.L. A Smartphone App to Restore Optimal Weight (SPAROW) in Women with Recent Gestational Diabetes Mellitus: Randomized Controlled Trial. JMIR MHealth UHealth 2021, 9, e22147. [Google Scholar] [CrossRef]
- Voils, C.I.; Olsen, M.K.; Gierisch, J.M.; McVay, M.A.; Grubber, J.M.; Gaillard, L.; Bolton, J.; Maciejewski, M.L.; Strawbridge, E.; Yancy, W.S., Jr. Maintenance of Weight Loss After Initiation of Nutrition Training: A Randomized Trial. Ann. Intern. Med. 2017, 166, 463–471. [Google Scholar] [CrossRef] [Green Version]
- Fruh, S.M. Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J. Am. Assoc. Nurse Pract. 2017, 29, S3–S14. [Google Scholar] [CrossRef]
- Messier, S.P.; Beavers, D.P.; Mihalko, S.L.; Miller, G.D.; Lyles, M.F.; Hunter, D.J.; Carr, J.J.; Eckstein, F.; Guermazi, A.; Loeser, R.F.; et al. The effects of intensive dietary weight loss and exercise on gait in overweight and obese adults with knee osteoarthritis. The Intensive Diet and Exercise for Arthritis (IDEA) trial. J. Biomech. 2020, 98, 109477. [Google Scholar] [CrossRef] [PubMed]
- Borazjani, M.; Amini, M.; Faghih, S. Perceived Barriers to Weight Loss: A Qualitative Study of the Lived Experiences of Women with Obesity in Shiraz. J. Nutr. Food Secur. 2022, 7, 60–68. [Google Scholar] [CrossRef]
- Verbanac, D.; Maleš, Ž.; Barišić, K. Nutrition–Facts and myths. Acta Pharm. 2019, 69, 497–510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalra, S.; Arora, S.; Kapoor, N. The motivation-opportunity-capability model of behavioural therapy–The vital component of effective patient centric obesity management. J. Pak. Med. Assoc. 2021, 71, 1900–1901. [Google Scholar] [PubMed]
| Characteristics | Total n = 209 | Men n = 88 (42.1%) | Women n = 121 (57.9%) | p | |
|---|---|---|---|---|---|
| Age (years) Mean (SD) | 65.7 (12.7) | 63.2 (13.6) | 67.6 (11.7) | 0.015 | |
| BMI (kg/m2) a Median (Interquartile range) | 32.9 (31.1–36.4) | 32.2 (30.9–35.0) | 33.4 (31.4–36.9) | 0.178 | |
| Patients’ distribution by BMI classes b % (n) | Overweight | 12.4 (26) | 15.9 (14) | 9.9 (12) | 0.178 |
| Obesity I | 53.6 (112) | 58.0 (51) | 50.4 (61) | ||
| Obesity II | 22.5 (47) | 18.2 (16) | 25.6 (31) | ||
| Obesity III | 11.5 (24) | 8.0 (7) | 14.0 (17) | ||
| Metabolic syndrome b % (n) | 90.4 (189) | 94.3 (83) | 87.6 (106) | 0.085 | |
| Metabolic syndrome diagnosis criteria | Waist circumference Mean (SD) | 111.4 (11.6) | 116.2 (10.1) | 107.9 (11.5) | <0.0001 |
| High blood pressure % (n) | 85.6 (179) | 89.8 (79) | 82.6 (100) | 0.166 | |
| Diabetes Mellitus II % (n) | 38.8 (81) | 38.6 (34) | 38.8 (47) | 1.000 | |
| Hypertrigliceridemia % (n) | 31.7 (66) | 41.4 (36) | 24.8 (30) | 0.009 | |
| Reduced HDL % (n) | 53.5 (112) | 52.8 (46) | 52.5 (62) | 1.000 | |
| Prescription of behavior change recorded % (n) | 2.9 (6) | 3.4 (3) | 2.4 (3) | 0.698 | |
| Type of behavior change recorded % (n) | 1.5 (2) | 1.8 (1) | 1.3 (1) | 1.000 | |
| Total (n = 209) | Men (n = 88) | Women (n = 121) | p | |
|---|---|---|---|---|
| Not having sufficient motivation to adhere to a weight loss program, % (n) | 67.5 (141) | 61.4 (54) | 71.9 (87) | 0.135 |
| Not believe they need to lose weight, % (n) | 20.5 (43) | 20.5 (18) | 20.7 (25) | 0.154 |
| Report following a diet on their own initiative, % (n) | 22.4 (47) | 19.3 (17) | 24.7 (30) | 0.403 |
| 1. DIFFICULTIES DIETING. |
|
| 2. DIFFICULTIES EXERCISING. |
|
| 3. MOOD THAT MAKES IT DIFFICULT TO FOLLOW A WEIGHT LOSS PLAN. |
|
| 4. DIFFICULTIES CHANGING HABITS. |
|
| Not Having Sufficient Motivation to Adhere to a Weight Loss Program vs. Having Motivation. | p | Difficulties to Dieting vs. * not Having. | p | Difficulties to Exercise vs. not Having. | p | Difficulties Relative to Mood Disturbance vs. not Having. | p | Difficulties to Change Habits vs. not Having. | p | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex a % (n) | Men | 61.4 (54) | 0.135 | 25.0 (22) | 0.874 | 43.2 (38) | 0.887 | 1.1 (1) | 0.001 | 6.8 (6) | 0.617 |
| Women | 71.9 (87) | 26.4 (32) | 41.3 50 | 14.0 (17) | 9.1 11 | ||||||
| Age (years) b Mean (SD) | 67.2.7 vs. 62.7 (11.7)/(14.2) | 0.015 | 62.5 vs. 66.9 (12.7)/(12.5) | 0.027 | 62.6 vs. 68.0 (13.1)/(12.0) | 0.002 | 67.8 vs. 65.5 (13.5)/(12.6) | 0.466 | 62.7 vs. 66.0 (14.4)/(12.5) | 0.299 | |
| BMI (kg/m2) c Median (Interquartile range) | 32.4 vs. 33.26 (31.0–36.2)/(31.1–37.1) | 0.550 | 34.9 vs. 32.2 (32.1–37.8)/(30.9–35.4) | 0.005 | 34.4 vs. 31.8 (32.2–37.7)/(30.5–35.0) | 0.000 | 36.4 vs. 32.6 (32.5–39.7)/(31.0–35.7) | 0.013 | 34.4 vs. 32.5 (32.4–35.0)/(31.0–36.5) | 0.350 | |
| Not Having Sufficient Motivation to Adhere to a Weight Loss Program vs. * Having motivation. | p | |
|---|---|---|
| Difficulties dieting % (n) | 23.4 vs. 30.9 (33)/(21) | 0.311 |
| Difficulties exercising % (n) | 44.0 vs. 38.2 (62)/(26) | 0.458 |
| Mood % (n) | 11.3 vs. 2.9 (16)/(2) | 0.062 |
| Difficulties changing habits % (n) | 9.2 vs. 5.9 (13)/(4) | 0.590 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trujillo-Garrido, N.; Santi-Cano, M.J. Motivation and Limiting Factors for Adherence to Weight Loss Interventions among Patients with Obesity in Primary Care. Nutrients 2022, 14, 2928. https://doi.org/10.3390/nu14142928
Trujillo-Garrido N, Santi-Cano MJ. Motivation and Limiting Factors for Adherence to Weight Loss Interventions among Patients with Obesity in Primary Care. Nutrients. 2022; 14(14):2928. https://doi.org/10.3390/nu14142928
Chicago/Turabian StyleTrujillo-Garrido, Nuria, and María J. Santi-Cano. 2022. "Motivation and Limiting Factors for Adherence to Weight Loss Interventions among Patients with Obesity in Primary Care" Nutrients 14, no. 14: 2928. https://doi.org/10.3390/nu14142928
APA StyleTrujillo-Garrido, N., & Santi-Cano, M. J. (2022). Motivation and Limiting Factors for Adherence to Weight Loss Interventions among Patients with Obesity in Primary Care. Nutrients, 14(14), 2928. https://doi.org/10.3390/nu14142928







