Epicardial Adipose Tissue: A Novel Potential Imaging Marker of Comorbidities Caused by Chronic Inflammation
Abstract
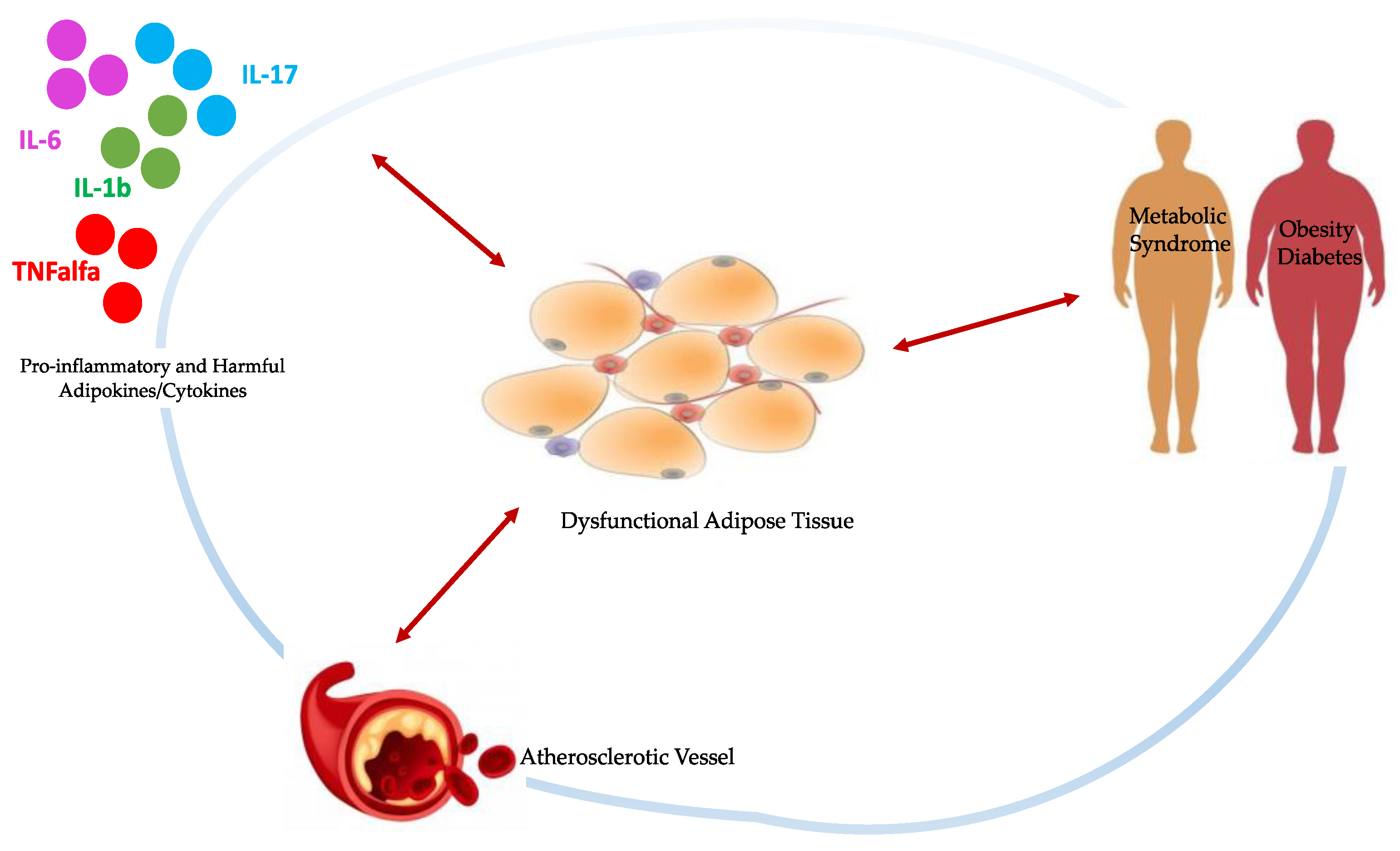
1. Introduction
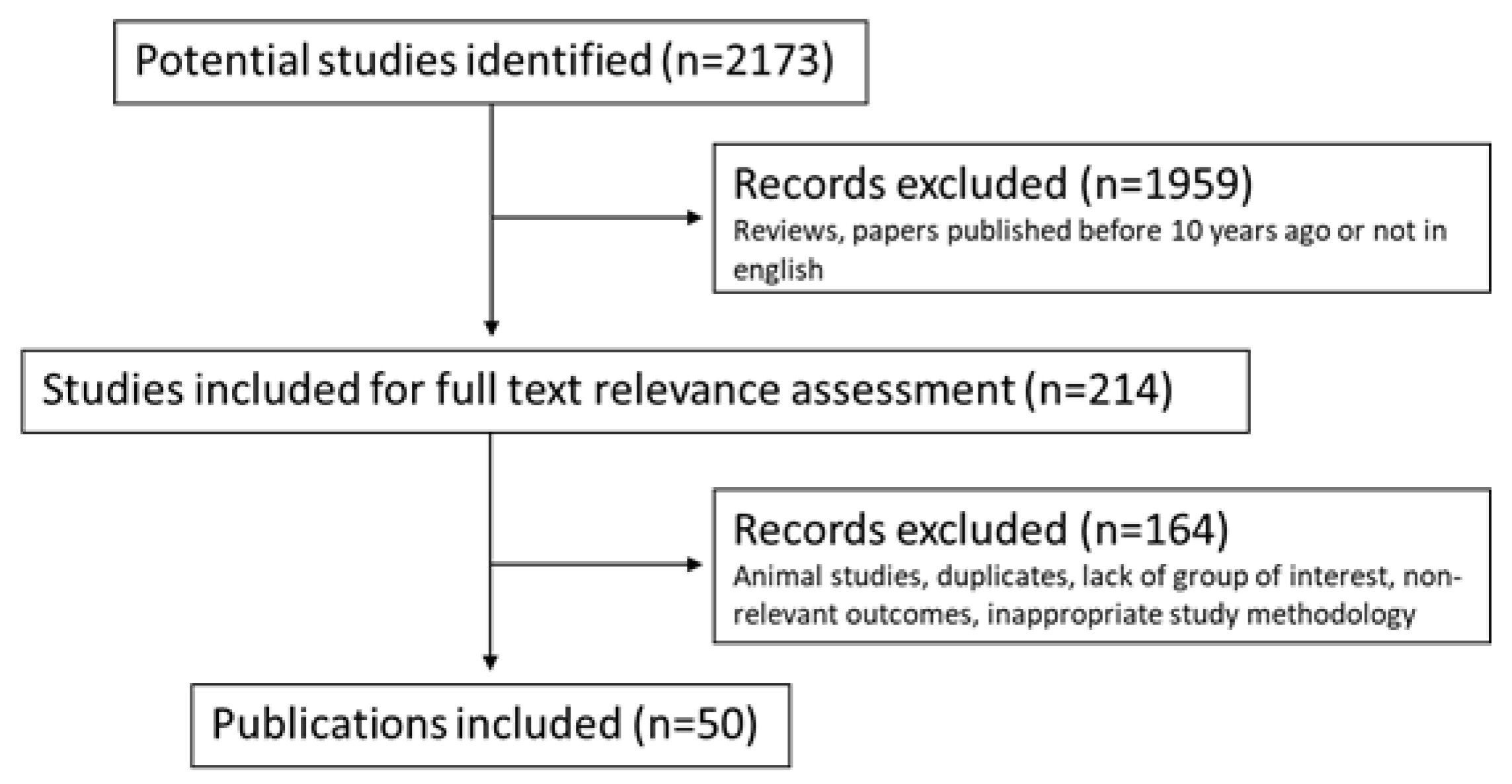
2. Materials and Methods
3. Results
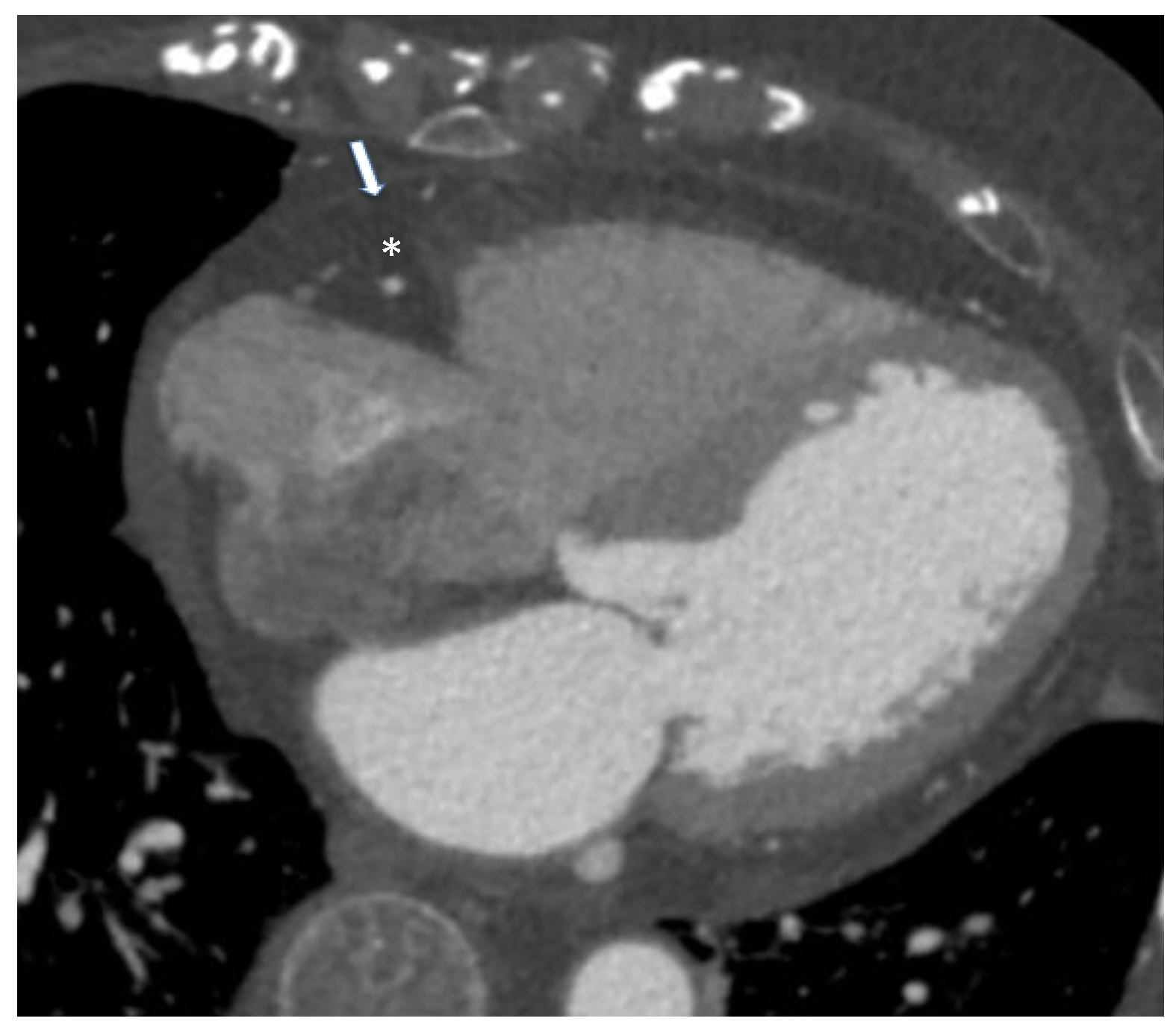
3.1. Epicardial Adipose Tissue and Cardiovascular Diseases
3.2. Epicardial Adipose Tissue and Metabolic Diseases
3.3. Epicardial Adipose Tissue in Other Clinical Conditions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guilherme, A.; Virbasius, J.V.; Puri, V.; Czech, M.P. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat. Rev. Mol. Cell Biol. 2008, 9, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Chouchani, E.T.; Kazak, L.; Spiegelman, B.M. New Advances in Adaptive Thermogenesis: UCP1 and Beyond. Cell Metab. 2019, 29, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Zatterale, F.; Longo, M.; Naderi, J.; Raciti, G.A.; Desiderio, A.; Miele, C.; Beguinot, F. Chronic Adipose Tissue Inflammation Linking Obesity to Insulin Resistance and Type 2 Diabetes. Front. Physiol. 2019, 10, 1607. [Google Scholar] [CrossRef] [PubMed]
- Lumeng, C.N.; Saltiel, A.R. Inflammatory links between obesity and metabolic disease. J. Clin. Investig. 2011, 121, 2111–2117. [Google Scholar] [CrossRef]
- Guglielmo, M.; Lin, A.; Dey, D.; Baggiano, A.; Fusini, L.; Muscogiuri, G.; Pontone, G. Epicardial fat and coronary artery disease: Role of cardiac imaging. Atherosclerosis 2021, 321, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Alzaim, I.; Hammoud, S.H.; Al-Koussa, H.; Ghazi, A.; Eid, A.H.; El-Yazbi, A.F. Adipose Tissue Immunomodulation: A Novel Therapeutic Approach in Cardiovascular and Metabolic Diseases. Front. Cardiovasc. Med. 2020, 7, 602088. [Google Scholar] [CrossRef] [PubMed]
- Pofi, R.; Giannetta, E.; Galea, N.; Francone, M.; Campolo, F.; Barbagallo, F.; Gianfrilli, D.; Venneri, M.A.; Filardi, T.; Cristini, C.; et al. Diabetic Cardiomiopathy Progression is Triggered by miR122-5p and Involves Extracellular Matrix: A 5-Year Prospective Study. JACC Cardiovasc. Imaging 2021, 14, 1130–1142. [Google Scholar] [CrossRef]
- Giannetta, E.; Isidori, A.M.; Galea, N.; Carbone, I.; Mandosi, E.; Vizza, C.D.; Naro, F.; Morano, S.; Fedele, F.; Lenzi, A. Chronic Inhibition of cGMP phosphodiesterase 5A improves diabetic cardiomyopathy: A randomized, controlled clinical trial using magnetic resonance imaging with myocardial tagging. Circulation 2012, 125, 2323–2333. [Google Scholar] [CrossRef]
- Margaritis, M.; Antonopoulos, A.S.; Digby, J.; Lee, R.; Reilly, S.; Coutinho, P.; Shirodaria, C.; Sayeed, R.; Petrou, M.; De Silva, R.; et al. Interactions between vascular wall and perivascular adipose tissue reveal novel roles for adiponectin in the regulation of endothelial nitric oxide synthase function in human vessels. Circulation 2013, 127, 2209–2221. [Google Scholar] [CrossRef]
- Yuvaraj, J.; Cheng, K.; Lin, A.; Psaltis, P.J.; Nicholls, S.J.; Wong, D.T.L. The Emerging Role of CT-Based Imaging in Adipose Tissue and Coronary Inflammation. Cells 2021, 10, 1196. [Google Scholar] [CrossRef]
- Britton, K.A.; Fox, C.S. Perivascular adipose tissue and vascular disease. Clin. Lipidol. 2011, 6, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Ansaldo, A.M.; Montecucco, F.; Sahebkar, A.; Dallegri, F.; Carbone, F. Epicardial adipose tissue and cardiovascular diseases. Int. J. Cardiol. 2019, 278, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, P. The role of adipokines in chronic inflammation. ImmunoTargets Ther. 2016, 5, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Lau, W.B.; Ohashi, K.; Wang, Y.; Ogawa, H.; Murohara, T.; Ma, X.L.; Ouchi, N. Role of Adipokines in Cardiovascular Disease. Circ. J. 2017, 81, 920–928. [Google Scholar] [CrossRef]
- Nishimura, M.; Morioka, T.; Hayashi, M.; Kakutani, Y.; Yamazaki, Y.; Kurajoh, M.; Mori, K.; Fukumoto, S.; Shioi, A.; Shoji, T.; et al. Plasma omentin levels are inversely associated with atherosclerosis in type 2 diabetes patients with increased plasma adiponectin levels: A cross-sectional study. Cardiovasc. Diabetol. 2019, 18, 167. [Google Scholar] [CrossRef]
- Gao, X.; Mi, S.; Zhang, F.; Gong, F.; Lai, Y.; Gao, F.; Zhang, X.; Wang, L.; Tao, H. Association of chemerin mRNA expression in human epicardial adipose tissue with coronary atherosclerosis. Cardiovasc. Diabetol. 2011, 10, 87. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Tarsitano, M.G.; Falcone, C.; Di Renzo, L.; Romano, L.; Macheda, S.; Ferrarelli, A.; Labate, D.; Tescione, M.; Bilotta, F.; et al. Fat mass affects nutritional status of ICU COVID-19 patients. J. Transl. Med. 2020, 18, 299. [Google Scholar] [CrossRef]
- De Lucena, T.M.C.; Da Silva Santos, A.F.; De Lima, B.R.; De Albuquerque Borborema, M.E.; De Azevedo Silva, J. Mechanism of inflammatory response in associated comorbidities in COVID-19. Diabetes Metab. Syndr. 2020, 14, 597–600. [Google Scholar] [CrossRef]
- Falcone, C.; Caracciolo, M.; Correale, P.; Macheda, S.; Vadala, E.G.; La Scala, S.; Tescione, M.; Danieli, R.; Ferrarelli, A.; Tarsitano, M.G.; et al. Can Adenosine Fight COVID-19 Acute Respiratory Distress Syndrome? J. Clin. Med. 2020, 9, 3045. [Google Scholar] [CrossRef]
- Chen, K.Y.; Brychta, R.J.; Abdul Sater, Z.; Cassimatis, T.M.; Cero, C.; Fletcher, L.A.; Israni, N.S.; Johnson, J.W.; Lea, H.J.; Linderman, J.D.; et al. Opportunities and challenges in the therapeutic activation of human energy expenditure and thermogenesis to manage obesity. J. Biol. Chem. 2020, 295, 1926–1942. [Google Scholar] [CrossRef]
- Rafeh, R.; Viveiros, A.; Oudit, G.Y.; El-Yazbi, A.F. Targeting perivascular and epicardial adipose tissue inflammation: Therapeutic opportunities for cardiovascular disease. Clin. Sci. 2020, 134, 827–851. [Google Scholar] [CrossRef] [PubMed]
- Pan, R.; Zhu, X.; Maretich, P.; Chen, Y. Combating Obesity With Thermogenic Fat: Current Challenges and Advancements. Front. Endocrinol. 2020, 11, 185. [Google Scholar] [CrossRef] [PubMed]
- YYoneshiro, T.; Wang, Q.; Tajima, K.; Matsushita, M.; Maki, H.; Igarashi, K.; Dai, Z.; White, P.J.; McGarrah, R.W.; Ilkayeva, O.R.; et al. BCAA catabolism in brown fat controls energy homeostasis through SLC25A44. Nature 2019, 572, 614–619. [Google Scholar] [CrossRef]
- Talman, A.H.; Psaltis, P.J.; Cameron, J.D.; Meredith, I.T.; Seneviratne, S.K.; Wong, D.T. Epicardial adipose tissue: Far more than a fat depot. Cardiovasc. Diagn. Ther. 2014, 4, 416–429. [Google Scholar] [CrossRef] [PubMed]
- Cherian, S.; Lopaschuk, G.D.; Carvalho, E. Cellular cross-talk between epicardial adipose tissue and myocardium in relation to the pathogenesis of cardiovascular disease. Am. J. Physiol. Endocrinol. Metab. 2012, 303, E937–E949. [Google Scholar] [CrossRef] [PubMed]
- Monti, C.B.; Capra, D.; Zanardo, M.; Guarnieri, G.; Schiaffino, S.; Secchi, F.; Sardanelli, F. CT-derived epicardial adipose tissue density: Systematic review and meta-analysis. Eur. J. Radiol. 2021, 143, 109902. [Google Scholar] [CrossRef]
- Sacks, D.; Baxter, B.; Campbell, B.C.V.; Carpenter, J.S.; Cognard, C.; Dippel, D.; Eesa, M.; Fischer, U.; Hausegger, K.; Hirsch, J.A.; et al. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int. J. Stroke 2018, 13, 612–632. [Google Scholar] [CrossRef] [PubMed]
- Song, D.K.; Hong, Y.S.; Lee, H.; Oh, J.Y.; Sung, Y.A.; Kim, Y. Increased Epicardial Adipose Tissue Thickness in Type 2 Diabetes Mellitus and Obesity. Diabetes Metab. J. 2015, 39, 405–413. [Google Scholar] [CrossRef][Green Version]
- Li, X.; Allayee, H.; Xiang, A.H.; Trigo, E.; Hartiala, J.; Lawrence, J.M.; Buchanan, T.A.; Watanabe, R.M. Variation in IGF2BP2 interacts with adiposity to alter insulin sensitivity in Mexican Americans. Obesity 2009, 17, 729–736. [Google Scholar] [CrossRef]
- Tuttle, L.J.; Sinacore, D.R.; Cade, W.T.; Mueller, M.J. Lower physical activity is associated with higher intermuscular adipose tissue in people with type 2 diabetes and peripheral neuropathy. Phys. Ther. 2011, 91, 923–930. [Google Scholar] [CrossRef]
- Iacobellis, G.; Barbaro, G. The double role of epicardial adipose tissue as pro- and anti-inflammatory organ. Horm. Metab. Res. 2008, 40, 442–445. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, B.; Li, Y.; Jing, X.; Deng, S.; Yan, Y.; She, Q. Epicardial fat tissue in patients with diabetes mellitus: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2019, 18, 3. [Google Scholar] [CrossRef] [PubMed]
- Monti, C.B.; Codari, M.; De Cecco, C.N.; Secchi, F.; Sardanelli, F.; Stillman, A.E. Novel imaging biomarkers: Epicardial adipose tissue evaluation. Br. J. Radiol. 2020, 93, 20190770. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Kim, B.S.; Kang, J.H. Echocardiographic epicardial fat thickness is associated with coronary artery calcification—Results from the CAESAR study. Circ. J. 2015, 79, 818–824. [Google Scholar] [CrossRef]
- Iacobellis, G.; Assael, F.; Ribaudo, M.C.; Zappaterreno, A.; Alessi, G.; Di Mario, U.; Leonetti, F. Epicardial fat from echocardiography: A new method for visceral adipose tissue prediction. Obes. Res. 2003, 11, 304–310. [Google Scholar] [CrossRef]
- Tachibana, M.; Miyoshi, T.; Osawa, K.; Toh, N.; Oe, H.; Nakamura, K.; Naito, T.; Sato, S.; Kanazawa, S.; Ito, H. Measurement of epicardial fat thickness by transthoracic echocardiography for predicting high-risk coronary artery plaques. Heart Vessels 2016, 31, 1758–1766. [Google Scholar] [CrossRef]
- Iacobellis, G.; Willens, H.J.; Barbaro, G.; Sharma, A.M. Threshold values of high-risk echocardiographic epicardial fat thickness. Obesity 2008, 16, 887–892. [Google Scholar] [CrossRef]
- Galea, N.; Francone, M.; Fiorelli, A.; Noce, V.; Giannetta, E.; Chimenti, C.; Frustaci, A.; Catalano, C.; Carbone, I. Early myocardial gadolinium enhancement in patients with myocarditis: Validation of “Lake Louise consensus” criteria using a single bolus of 0.1mmol/Kg of a high relaxivity gadolinium-based contrast agent. Eur. J. Radiol. 2017, 95, 89–95. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef]
- Titi, L.; Magnanimi, E.; Mancone, M.; Infusino, F.; Coppola, G.; Del Nonno, F.; Colombo, D.; Nardacci, R.; Falasca, L.; d’Amati, G.; et al. Fatal Takotsubo syndrome in critical COVID-19 related pneumonia. Cardiovasc. Pathol. 2021, 51, 107314. [Google Scholar] [CrossRef]
- Eisenberg, E.; McElhinney, P.A.; Commandeur, F.; Chen, X.; Cadet, S.; Goeller, M.; Razipour, A.; Gransar, H.; Cantu, S.; Miller, R.J.H.; et al. Deep Learning-Based Quantification of Epicardial Adipose Tissue Volume and Attenuation Predicts Major Adverse Cardiovascular Events in Asymptomatic Subjects. Circ. Cardiovasc. Imaging 2020, 13, e009829. [Google Scholar] [CrossRef] [PubMed]
- Nagayama, Y.; Nakamura, N.; Itatani, R.; Oda, S.; Kusunoki, S.; Takahashi, H.; Nakaura, T.; Utsunomiya, D.; Yamashita, Y. Epicardial fat volume measured on nongated chest CT is a predictor of coronary artery disease. Eur. Radiol. 2019, 29, 3638–3646. [Google Scholar] [CrossRef] [PubMed]
- La Grutta, L.; Toia, P.; Farruggia, A.; Albano, D.; Grassedonio, E.; Palmeri, A.; Maffei, E.; Galia, M.; Vitabile, S.; Cademartiri, F.; et al. Quantification of epicardial adipose tissue in coronary calcium score and CT coronary angiography image data sets: Comparison of attenuation values, thickness and volumes. Br. J. Radiol. 2016, 89, 20150773. [Google Scholar] [CrossRef] [PubMed]
- Spearman, J.V.; Renker, M.; Schoepf, U.J.; Krazinski, A.W.; Herbert, T.L.; De Cecco, C.N.; Nietert, P.J.; Meinel, F.G. Prognostic value of epicardial fat volume measurements by computed tomography: A systematic review of the literature. Eur. Radiol. 2015, 25, 3372–3381. [Google Scholar] [CrossRef]
- Raggi, P.; Gadiyaram, V.; Zhang, C.; Chen, Z.; Lopaschuk, G.; Stillman, A.E. Statins Reduce Epicardial Adipose Tissue Attenuation Independent of Lipid Lowering: A Potential Pleiotropic Effect. J. Am. Heart Assoc. 2019, 8, e013104. [Google Scholar] [CrossRef]
- Antonopoulos, A.S.; Sanna, F.; Sabharwal, N.; Thomas, S.; Oikonomou, E.K.; Herdman, L.; Margaritis, M.; Shirodaria, C.; Kampoli, A.M.; Akoumianakis, I.; et al. Detecting human coronary inflammation by imaging perivascular fat. Sci. Transl. Med. 2017, 9, eaal2658. [Google Scholar] [CrossRef]
- Gianfrilli, D.; Pofi, R.; Feola, T.; Lenzi, A.; Giannetta, E. The Woman’s Heart: Insights into New Potential Targeted Therapy. Curr. Med. Chem. 2017, 24, 2650–2660. [Google Scholar] [CrossRef]
- Ventura-Clapier, R.; Dworatzek, E.; Seeland, U.; Kararigas, G.; Arnal, J.F.; Brunelleschi, S.; Carpenter, T.C.; Erdmann, J.; Franconi, F.; Giannetta, E.; et al. Sex in basic research: Concepts in the cardiovascular field. Cardiovasc. Res. 2017, 113, 711–724. [Google Scholar] [CrossRef]
- Shimabukuro, M.; Hirata, Y.; Tabata, M.; Dagvasumberel, M.; Sato, H.; Kurobe, H.; Fukuda, D.; Soeki, T.; Kitagawa, T.; Takanashi, S.; et al. Epicardial adipose tissue volume and adipocytokine imbalance are strongly linked to human coronary atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 1077–1084. [Google Scholar] [CrossRef]
- Fantuzzi, G.; Mazzone, T. Adipose tissue and atherosclerosis: Exploring the connection. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 996–1003. [Google Scholar] [CrossRef]
- Oikawa, M.; Owada, T.; Yamauchi, H.; Misaka, T.; Machii, H.; Yamaki, T.; Sugimoto, K.; Kunii, H.; Nakazato, K.; Suzuki, H.; et al. Epicardial adipose tissue reflects the presence of coronary artery disease: Comparison with abdominal visceral adipose tissue. Biomed. Res. Int. 2015, 2015, 483982. [Google Scholar] [CrossRef] [PubMed]
- Commandeur, F.; Slomka, P.J.; Goeller, M.; Chen, X.; Cadet, S.; Razipour, A.; McElhinney, P.; Gransar, H.; Cantu, S.; Miller, R.J.H.; et al. Machine learning to predict the long-term risk of myocardial infarction and cardiac death based on clinical risk, coronary calcium, and epicardial adipose tissue: A prospective study. Cardiovasc. Res. 2020, 116, 2216–2225. [Google Scholar] [CrossRef] [PubMed]
- Nerlekar, N.; Thakur, U.; Lin, A.; Koh, J.Q.S.; Potter, E.; Liu, D.; Muthalaly, R.G.; Rashid, H.N.; Cameron, J.D.; Dey, D.; et al. The Natural history of Epicardial Adipose Tissue Volume and Attenuation: A long-term prospective cohort follow-up study. Sci. Rep. 2020, 10, 7109. [Google Scholar] [CrossRef]
- Forouzandeh, F.; Chang, S.M.; Muhyieddeen, K.; Zaid, R.R.; Trevino, A.R.; Xu, J.; Nabi, F.; Mahmarian, J.J. Does quantifying epicardial and intrathoracic fat with noncontrast computed tomography improve risk stratification beyond calcium scoring alone? Circ. Cardiovasc. Imaging 2013, 6, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Almeida, S.O.; Ram, R.J.; Kinninger, A.; Budoff, M.J. Effect of 5-lipoxygenase inhibitor, VIA-2291 (Atreleuton), on epicardial fat volume in patients with recent acute coronary syndrome. J. Cardiovasc. Comput. Tomogr. 2020, 14, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Soucek, F.; Covassin, N.; Singh, P.; Ruzek, L.; Kara, T.; Suleiman, M.; Lerman, A.; Koestler, C.; Friedman, P.A.; Lopez-Jimenez, F.; et al. Effects of Atorvastatin (80 mg) Therapy on Quantity of Epicardial Adipose Tissue in Patients Undergoing Pulmonary Vein Isolation for Atrial Fibrillation. Am. J. Cardiol. 2015, 116, 1443–1446. [Google Scholar] [CrossRef]
- Gepner, Y.; Shelef, I.; Schwarzfuchs, D.; Zelicha, H.; Tene, L.; Yaskolka Meir, A.; Tsaban, G.; Cohen, N.; Bril, N.; Rein, M.; et al. Effect of Distinct Lifestyle Interventions on Mobilization of Fat Storage Pools: CENTRAL Magnetic Resonance Imaging Randomized Controlled Trial. Circulation 2018, 137, 1143–1157. [Google Scholar] [CrossRef]
- Zeb, I.; Ahmadi, N.; Flores, F.; Budoff, M.J. Randomized trial evaluating the effect of aged garlic extract with supplements versus placebo on adipose tissue surrogates for coronary atherosclerosis progression. Coron. Artery Dis. 2018, 29, 325–328. [Google Scholar] [CrossRef]
- Ahmadi, N.; Nabavi, V.; Hajsadeghi, F.; Zeb, I.; Flores, F.; Ebrahimi, R.; Budoff, M. Aged garlic extract with supplement is associated with increase in brown adipose, decrease in white adipose tissue and predict lack of progression in coronary atherosclerosis. Int. J. Cardiol. 2013, 168, 2310–2314. [Google Scholar] [CrossRef]
- Maimaituxun, G.; Shimabukuro, M.; Fukuda, D.; Yagi, S.; Hirata, Y.; Iwase, T.; Takao, S.; Matsuura, T.; Ise, T.; Kusunose, K.; et al. Local Thickness of Epicardial Adipose Tissue Surrounding the Left Anterior Descending Artery Is a Simple Predictor of Coronary Artery Disease- New Prediction Model in Combination With Framingham Risk Score. Circ. J. 2018, 82, 1369–1378. [Google Scholar] [CrossRef]
- Lu, M.T.; Park, J.; Ghemigian, K.; Mayrhofer, T.; Puchner, S.B.; Liu, T.; Fleg, J.L.; Udelson, J.E.; Truong, Q.A.; Ferencik, M.; et al. Epicardial and paracardial adipose tissue volume and attenuation—Association with high-risk coronary plaque on computed tomographic angiography in the ROMICAT II trial. Atherosclerosis 2016, 251, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Tsushima, H.; Yamamoto, H.; Kitagawa, T.; Urabe, Y.; Tatsugami, F.; Awai, K.; Kihara, Y. Association of epicardial and abdominal visceral adipose tissue with coronary atherosclerosis in patients with a coronary artery calcium score of zero. Circ. J. 2015, 79, 1084–1091. [Google Scholar] [CrossRef] [PubMed]
- Parisi, V.; Rengo, G.; Pagano, G.; D’Esposito, V.; Passaretti, F.; Caruso, A.; Grimaldi, M.G.; Lonobile, T.; Baldascino, F.; De Bellis, A.; et al. Epicardial adipose tissue has an increased thickness and is a source of inflammatory mediators in patients with calcific aortic stenosis. Int. J. Cardiol. 2015, 186, 167–169. [Google Scholar] [CrossRef]
- Tam, W.C.; Lin, Y.K.; Chan, W.P.; Huang, J.H.; Hsieh, M.H.; Chen, S.A.; Chen, Y.J. Pericardial Fat Is Associated With the Risk of Ventricular Arrhythmia in Asian Patients. Circ. J. 2016, 80, 1726–1733. [Google Scholar] [CrossRef] [PubMed]
- Canpolat, U.; Aytemir, K.; Yorgun, H.; Asil, S.; Dural, M.; Ozer, N. The Impact of Echocardiographic Epicardial Fat Thickness on Outcomes of Cryoballoon-Based Atrial Fibrillation Ablation. Echocardiography 2016, 33, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Ohyama, K.; Matsumoto, Y.; Nishimiya, K.; Hao, K.; Tsuburaya, R.; Ota, H.; Amamizu, H.; Uzuka, H.; Takahashi, J.; Ito, K.; et al. Increased Coronary Perivascular Adipose Tissue Volume in Patients With Vasospastic Angina. Circ. J. 2016, 80, 1653–1656. [Google Scholar] [CrossRef]
- Gastelurrutia, P.; Galvez-Monton, C.; Camara, M.L.; Bustamante-Munguira, J.; Garcia-Pavia, P.; Avanzas, P.; Alberto San Roman, J.; Pascual-Figal, D.; Teresa, E.; Crespo-Leiro, M.G.; et al. Rationale and design of a multicentre, prospective, randomised, controlled clinical trial to evaluate the efficacy of the adipose graft transposition procedure in patients with a myocardial scar: The AGTP II trial. BMJ Open 2017, 7, e017187. [Google Scholar] [CrossRef]
- Sato, T.; Aizawa, Y.; Yuasa, S.; Kishi, S.; Fuse, K.; Fujita, S.; Ikeda, Y.; Kitazawa, H.; Takahashi, M.; Sato, M.; et al. The effect of dapagliflozin treatment on epicardial adipose tissue volume. Cardiovasc. Diabetol. 2018, 17, 6. [Google Scholar] [CrossRef]
- Iacobellis, G.; Mohseni, M.; Bianco, S.D.; Banga, P.K. Liraglutide causes large and rapid epicardial fat reduction. Obesity 2017, 25, 311–316. [Google Scholar] [CrossRef]
- Christensen, R.H.; Wedell-Neergaard, A.S.; Lehrskov, L.L.; Legaard, G.E.; Dorph, E.; Larsen, M.K.; Launbo, N.; Fagerlind, S.R.; Seide, S.K.; Nymand, S.; et al. Effect of Aerobic and Resistance Exercise on Cardiac Adipose Tissues: Secondary Analyses From a Randomized Clinical Trial: Secondary Analyses From a Randomized Clinical Trial. JAMA Cardiol. 2019, 4, 778–787. [Google Scholar] [CrossRef]
- Fernandez-del-Valle, M.; Gonzales, J.U.; Kloiber, S.; Mitra, S.; Klingensmith, J.; Larumbe-Zabala, E. Effects of resistance training on MRI-derived epicardial fat volume and arterial stiffness in women with obesity: A randomized pilot study. Eur. J. Appl. Physiol. 2018, 118, 1231–1240. [Google Scholar] [CrossRef] [PubMed]
- Rosety, M.A.; Pery, M.T.; Rodriguez-Pareja, M.A.; Diaz, A.; Rosety, J.; Garcia, N.; Brenes-Martin, F.; Rosety-Rodriguez, M.; Toro, R.; Ordonez, F.J.; et al. A Short-Term Circuit Resistance Programme Reduced Epicardial Fat in Obese Aged Women. Nutr. Hosp. 2015, 32, 2193–2197. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, G.; Singh, N.; Wharton, S.; Sharma, A.M. Substantial changes in epicardial fat thickness after weight loss in severely obese subjects. Obesity (Silver Spring) 2008, 16, 1693–1697. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Ferrer, J.; Crendal, E.; Walther, G.; Vinet, A.; Dutheil, F.; Naughton, G.; Lesourd, B.; Chapier, R.; Courteix, D.; Obert, P. Effects of lifestyle intervention on left ventricular regional myocardial function in metabolic syndrome patients from the RESOLVE randomized trial. Metabolism 2016, 65, 1350–1360. [Google Scholar] [CrossRef] [PubMed]
- Jo, E.A.; Cho, K.I.; Park, J.J.; Im, D.S.; Choi, J.H.; Kim, B.J. Effects of High-Intensity Interval Training Versus Moderate-Intensity Continuous Training on Epicardial Fat Thickness and Endothelial Function in Hypertensive Metabolic Syndrome. Metab. Syndr. Relat Disord 2020, 18, 96–102. [Google Scholar] [CrossRef]
- Fornieles Gonzalez, G.; Rosety Rodriguez, M.A.; Rodriguez Pareja, M.A.; Diaz Ordonez, A.; Rosety Rodriguez, J.; Pery Bohorquez, M.T.; Brenes Martin, F.; Escribano Ocon, A.; Rosety Rodriguez, M.; Ordonez Munoz, F.J.; et al. A home-based treadmill training reduced epicardial and abdominal fat in postmenopausal women with metabolic syndrome. Nutr. Hosp. 2014, 30, 609–613. [Google Scholar] [CrossRef]
- Mohar, D.S.; Salcedo, J.; Hoang, K.C.; Kumar, S.; Saremi, F.; Erande, A.S.; Naderi, N.; Nadeswaran, P.; Le, C.; Malik, S. Epicardial adipose tissue volume as a marker of coronary artery disease severity in patients with diabetes independent of coronary artery calcium: Findings from the CTRAD study. Diabetes Res. Clin. Pract. 2014, 106, 228–235. [Google Scholar] [CrossRef]
- Groves, E.M.; Erande, A.S.; Le, C.; Salcedo, J.; Hoang, K.C.; Kumar, S.; Mohar, D.S.; Saremi, F.; Im, J.; Agrawal, Y.; et al. Comparison of epicardial adipose tissue volume and coronary artery disease severity in asymptomatic adults with versus without diabetes mellitus. Am. J. Cardiol. 2014, 114, 686–691. [Google Scholar] [CrossRef]
- Hiruma, S.; Shigiyama, F.; Hisatake, S.; Mizumura, S.; Shiraga, N.; Hori, M.; Ikeda, T.; Hirose, T.; Kumashiro, N. A prospective randomized study comparing effects of empagliflozin to sitagliptin on cardiac fat accumulation, cardiac function, and cardiac metabolism in patients with early-stage type 2 diabetes: The ASSET study. Cardiovasc. Diabetol. 2021, 20, 32. [Google Scholar] [CrossRef]
- Leroux-Stewart, J.; Elisha, B.; Tagougui, S.; Suppere, C.; Bernard, S.; Mircescu, H.; Desjardin, K.; Messier, V.; Iacobellis, G.; Rabasa-Lhoret, R. Effect of caloric restriction with or without physical activity on body composition and epicardial fat in type 2 diabetic patients: A pilot randomized controlled trial. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 921–929. [Google Scholar] [CrossRef]
- Snel, M.; Jonker, J.T.; Hammer, S.; Kerpershoek, G.; Lamb, H.J.; Meinders, A.E.; Pijl, H.; de Roos, A.; Romijn, J.A.; Smit, J.W.; et al. Long-term beneficial effect of a 16-week very low calorie diet on pericardial fat in obese type 2 diabetes mellitus patients. Obesity 2012, 20, 1572–1576. [Google Scholar] [CrossRef] [PubMed]
- Bouchi, R.; Terashima, M.; Sasahara, Y.; Asakawa, M.; Fukuda, T.; Takeuchi, T.; Nakano, Y.; Murakami, M.; Minami, I.; Izumiyama, H.; et al. Luseogliflozin reduces epicardial fat accumulation in patients with type 2 diabetes: A pilot study. Cardiovasc. Diabetol. 2017, 16, 32. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, G.; Gra-Menendez, S. Effects of Dapagliflozin on Epicardial Fat Thickness in Patients with Type 2 Diabetes and Obesity. Obesity 2020, 28, 1068–1074. [Google Scholar] [CrossRef] [PubMed]
- Dutour, A.; Abdesselam, I.; Ancel, P.; Kober, F.; Mrad, G.; Darmon, P.; Ronsin, O.; Pradel, V.; Lesavre, N.; Martin, J.C.; et al. Exenatide decreases liver fat content and epicardial adipose tissue in patients with obesity and type 2 diabetes: A prospective randomized clinical trial using magnetic resonance imaging and spectroscopy. Diabetes Obes. Metab. 2016, 18, 882–891. [Google Scholar] [CrossRef]
- Morano, S.; Romagnoli, E.; Filardi, T.; Nieddu, L.; Mandosi, E.; Fallarino, M.; Turinese, I.; Dagostino, M.P.; Lenzi, A.; Carnevale, V. Short-term effects of glucagon-like peptide 1 (GLP-1) receptor agonists on fat distribution in patients with type 2 diabetes mellitus: An ultrasonography study. Acta Diabetol. 2015, 52, 727–732. [Google Scholar] [CrossRef]
- Elisha, B.; Azar, M.; Taleb, N.; Bernard, S.; Iacobellis, G.; Rabasa-Lhoret, R. Body Composition and Epicardial Fat in Type 2 Diabetes Patients Following Insulin Detemir Versus Insulin Glargine Initiation. Horm. Metab. Res. 2016, 48, 42–47. [Google Scholar] [CrossRef]
- Murai, T.; Takebe, N.; Nagasawa, K.; Todate, Y.; Nakagawa, R.; Nakano, R.; Hangai, M.; Hasegawa, Y.; Takahashi, Y.; Yoshioka, K.; et al. Association of epicardial adipose tissue with serum level of cystatin C in type 2 diabetes. PLoS ONE 2017, 12, e0184723. [Google Scholar] [CrossRef]
- Bayomy, O.; Rao, A.D.; Garg, R.; Vaidya, A.; Kotin, A.R.; Reiber, B.; Nijmeijer, S.; Di Carli, M.F.; Jerosch-Herold, M.; Kwong, R.Y.; et al. Plasminogen Activator Inhibitor-1 and Pericardial Fat in Individuals with Type 2 Diabetes Mellitus. Metab. Syndr. Relat. Disord. 2017, 15, 269–275. [Google Scholar] [CrossRef]
- Nakanishi, K.; Fukuda, S.; Tanaka, A.; Otsuka, K.; Taguchi, H.; Yoshikawa, J.; Shimada, K. Epicardial Adipose Tissue Accumulation Is Associated With Renal Dysfunction and Coronary Plaque Morphology on Multidetector Computed Tomography. Circ. J. 2016, 80, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Yazbek, D.C.; Carvalho, A.B.; Barros, C.S.; Medina Pestana, J.O.; Rochitte, C.E.; Dos Santos Filho, R.D.; Canziani, M.E.F. Is there relationship between epicardial fat and cardiovascular parameters in incident kidney transplant patients? A post-hoc analysis. PLoS ONE 2018, 13, e0191009. [Google Scholar] [CrossRef]
- Altun, B.; Tasolar, H.; Eren, N.; Binnetoglu, E.; Altun, M.; Temiz, A.; Gazi, E.; Barutcu, A.; Altunoren, O.; Colkesen, Y.; et al. Epicardial adipose tissue thickness in hemodialysis patients. Echocardiography 2014, 31, 941–946. [Google Scholar] [CrossRef] [PubMed]
- Ko, S.M.; Zhang, C.; Chen, Z.; D’Marco, L.; Bellasi, A.; Stillman, A.E.; Block, G.; Raggi, P. Epicardial adipose tissue volume increase in hemodialysis patients treated with sevelamer or calcium-based phosphate binders: A substudy of the Renagel in new dialysis trial. J. Nephrol. 2016, 29, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Cetin, S.; Vural, M.G.; Gunduz, H.; Akdemir, R.; Firat, H. Epicardial fat thickness regression with continuous positive airway pressure therapy in patients with obstructive sleep apnea: Assessment by two-dimensional echocardiography. Wien. Klin. Wochenschr. 2016, 128, 187–192. [Google Scholar] [CrossRef] [PubMed]
- El Khoudary, S.R.; Zhao, Q.; Venugopal, V.; Manson, J.E.; Brooks, M.M.; Santoro, N.; Black, D.M.; Harman, S.M.; Cedars, M.I.; Hopkins, P.N.; et al. Effects of Hormone Therapy on Heart Fat and Coronary Artery Calcification Progression: Secondary Analysis From the KEEPS Trial. J. Am. Heart Assoc. 2019, 8, e012763. [Google Scholar] [CrossRef]
- Kahl, K.G.; Kerling, A.; Tegtbur, U.; Gutzlaff, E.; Herrmann, J.; Borchert, L.; Ates, Z.; Westhoff-Bleck, M.; Hueper, K.; Hartung, D. Effects of additional exercise training on epicardial, intra-abdominal and subcutaneous adipose tissue in major depressive disorder: A randomized pilot study. J. Affect. Disord. 2016, 192, 91–97. [Google Scholar] [CrossRef]
- Pacifico, L.; Bonci, E.; Di Martino, M.; Versacci, P.; Andreoli, G.; Silvestri, L.M.; Chiesa, C. A double-blind, placebo-controlled randomized trial to evaluate the efficacy of docosahexaenoic acid supplementation on hepatic fat and associated cardiovascular risk factors in overweight children with nonalcoholic fatty liver disease. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 734–741. [Google Scholar] [CrossRef]
- Farghaly, H.S.; Metwalley, K.A.; Raafat, D.M.; Algowhary, M.; Said, G.M. Epicardial Fat Thickness in Children with Subclinical Hypothyroidism and Its Relationship to Subclinical Atherosclerosis: A Pilot Study. Horm. Res. Paediatr. 2019, 92, 99–105. [Google Scholar] [CrossRef]
- Celik, N.; Alp, H.; Camtosun, E.; Alp, E.; Celik, S.; Berk, E. The Association between Premature Adrenarche and Cardiovascular Risk May Be Greater than Expected. Horm. Res. Paediatr. 2017, 87, 7–14. [Google Scholar] [CrossRef]
- Longenecker, C.T.; Margevicius, S.; Liu, Y.; Schluchter, M.D.; Yun, C.H.; Bezerra, H.G.; McComsey, G.A. Effect of Pericardial Fat Volume and Density on Markers of Insulin Resistance and Inflammation in Patients With Human Immunodeficiency Virus Infection. Am. J. Cardiol. 2017, 120, 1427–1433. [Google Scholar] [CrossRef]
- Hu, H.H.; Chung, S.A.; Nayak, K.S.; Jackson, H.A.; Gilsanz, V. Differential computed tomographic attenuation of metabolically active and inactive adipose tissues: Preliminary findings. J. Comput. Assist. Tomogr. 2011, 35, 65–71. [Google Scholar] [CrossRef]
- Baba, S.; Jacene, H.A.; Engles, J.M.; Honda, H.; Wahl, R.L. CT Hounsfield units of brown adipose tissue increase with activation: Preclinical and clinical studies. J. Nucl. Med. 2010, 51, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Budoff, M.J.; Ahmadi, N.; Gul, K.M.; Liu, S.T.; Flores, F.R.; Tiano, J.; Takasu, J.; Miller, E.; Tsimikas, S. Aged garlic extract supplemented with B vitamins, folic acid and L-arginine retards the progression of subclinical atherosclerosis: A randomized clinical trial. Prev. Med. 2009, 49, 101–107. [Google Scholar] [CrossRef]
- Budoff, M. Aged garlic extract retards progression of coronary artery calcification. J. Nutr. 2006, 136, 741S–744S. [Google Scholar] [CrossRef] [PubMed]
- Steiner, M.; Khan, A.H.; Holbert, D.; Lin, R.I. A double-blind crossover study in moderately hypercholesterolemic men that compared the effect of aged garlic extract and placebo administration on blood lipids. Am. J. Clin. Nutr. 1996, 64, 866–870. [Google Scholar] [CrossRef] [PubMed]
- Rahman, K.; Billington, D. Dietary supplementation with aged garlic extract inhibits ADP-induced platelet aggregation in humans. J. Nutr. 2000, 130, 2662–2665. [Google Scholar] [CrossRef] [PubMed]
- Schlett, C.L.; Ferencik, M.; Kriegel, M.F.; Bamberg, F.; Ghoshhajra, B.B.; Joshi, S.B.; Nagurney, J.T.; Fox, C.S.; Truong, Q.A.; Hoffmann, U. Association of pericardial fat and coronary high-risk lesions as determined by cardiac CT. Atherosclerosis 2012, 222, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Tsao, H.M.; Hu, W.C.; Wu, M.H.; Tai, C.T.; Lin, Y.J.; Chang, S.L.; Lo, L.W.; Hu, Y.F.; Tuan, T.C.; Wu, T.J.; et al. Quantitative analysis of quantity and distribution of epicardial adipose tissue surrounding the left atrium in patients with atrial fibrillation and effect of recurrence after ablation. Am. J. Cardiol. 2011, 107, 1498–1503. [Google Scholar] [CrossRef]
- Nagashima, K.; Okumura, Y.; Watanabe, I.; Nakai, T.; Ohkubo, K.; Kofune, T.; Kofune, M.; Mano, H.; Sonoda, K.; Hirayama, A. Association between epicardial adipose tissue volumes on 3-dimensional reconstructed CT images and recurrence of atrial fibrillation after catheter ablation. Circ. J. 2011, 75, 2559–2565. [Google Scholar] [CrossRef]
- Iacobellis, G.; Ribaudo, M.C.; Assael, F.; Vecci, E.; Tiberti, C.; Zappaterreno, A.; Di Mario, U.; Leonetti, F. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: A new indicator of cardiovascular risk. J. Clin. Endocrinol. Metab. 2003, 88, 5163–5168. [Google Scholar] [CrossRef]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef]
- Marso, S.P.; Daniels, G.H.; Brown-Frandsen, K.; Kristensen, P.; Mann, J.F.; Nauck, M.A.; Nissen, S.E.; Pocock, S.; Poulter, N.R.; Ravn, L.S.; et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Vendrell, J.; El Bekay, R.; Peral, B.; Garcia-Fuentes, E.; Megia, A.; Macias-Gonzalez, M.; Fernandez Real, J.; Jimenez-Gomez, Y.; Escote, X.; Pachon, G.; et al. Study of the potential association of adipose tissue GLP-1 receptor with obesity and insulin resistance. Endocrinology 2011, 152, 4072–4079. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Ren, J.; Song, J.; Liu, F.; Wu, C.; Wang, X.; Gong, L.; Li, W.; Xiao, F.; Yan, F.; et al. Glucagon-like peptide 1 regulates adipogenesis in 3T3-L1 preadipocytes. Int. J. Mol. Med. 2013, 31, 1429–1435. [Google Scholar] [CrossRef]
- Beiroa, D.; Imbernon, M.; Gallego, R.; Senra, A.; Herranz, D.; Villarroya, F.; Serrano, M.; Ferno, J.; Salvador, J.; Escalada, J.; et al. GLP-1 agonism stimulates brown adipose tissue thermogenesis and browning through hypothalamic AMPK. Diabetes 2014, 63, 3346–3358. [Google Scholar] [CrossRef]
- Yagi, S.; Hirata, Y.; Ise, T.; Kusunose, K.; Yamada, H.; Fukuda, D.; Salim, H.M.; Maimaituxun, G.; Nishio, S.; Takagawa, Y.; et al. Canagliflozin reduces epicardial fat in patients with type 2 diabetes mellitus. Diabetol. Metab. Syndr. 2017, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Lima-Martinez, M.M.; Paoli, M.; Rodney, M.; Balladares, N.; Contreras, M.; D’Marco, L.; Iacobellis, G. Effect of sitagliptin on epicardial fat thickness in subjects with type 2 diabetes and obesity: A pilot study. Endocrine 2016, 51, 448–455. [Google Scholar] [CrossRef]
- Dandana, A.; Gammoudi, I.; Chalghoum, A.; Chahed, H.; Addad, F.; Ferchichi, S.; Miled, A. Clinical utility of serum cystatin C in predicting coronary artery disease in patients without chronic kidney disease. J. Clin. Lab. Anal. 2014, 28, 191–197. [Google Scholar] [CrossRef]
- Niccoli, G.; Conte, M.; Della Bona, R.; Altamura, L.; Siviglia, M.; Dato, I.; Ferrante, G.; Leone, A.M.; Porto, I.; Burzotta, F.; et al. Cystatin C is associated with an increased coronary atherosclerotic burden and a stable plaque phenotype in patients with ischemic heart disease and normal glomerular filtration rate. Atherosclerosis 2008, 198, 373–380. [Google Scholar] [CrossRef]
- Ristiniemi, N.; Lund, J.; Tertti, R.; Christensson, A.; Ilva, T.; Porela, P.; Pulkki, K.; Pettersson, K. Cystatin C as a predictor of all-cause mortality and myocardial infarction in patients with non-ST-elevation acute coronary syndrome. Clin. Biochem. 2012, 45, 535–540. [Google Scholar] [CrossRef]
- Schneider, D.J.; Sobel, B.E. PAI-1 and diabetes: A journey from the bench to the bedside. Diabetes Care 2012, 35, 1961–1967. [Google Scholar] [CrossRef]
- Shimomura, I.; Funahashi, T.; Takahashi, M.; Maeda, K.; Kotani, K.; Nakamura, T.; Yamashita, S.; Miura, M.; Fukuda, Y.; Takemura, K.; et al. Enhanced expression of PAI-1 in visceral fat: Possible contributor to vascular disease in obesity. Nat. Med. 1996, 2, 800–803. [Google Scholar] [CrossRef] [PubMed]
- Fain, J.N.; Madan, A.K.; Hiler, M.L.; Cheema, P.; Bahouth, S.W. Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology 2004, 145, 2273–2282. [Google Scholar] [CrossRef] [PubMed]
- Malavazos, A.E.; Ermetici, F.; Cereda, E.; Coman, C.; Locati, M.; Morricone, L.; Corsi, M.M.; Ambrosi, B. Epicardial fat thickness: Relationship with plasma visfatin and plasminogen activator inhibitor-1 levels in visceral obesity. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 523–530. [Google Scholar] [CrossRef] [PubMed]
- D’Marco, L.G.; Bellasi, A.; Kim, S.; Chen, Z.; Block, G.A.; Raggi, P. Epicardial adipose tissue predicts mortality in incident hemodialysis patients: A substudy of the Renagel in New Dialysis trial. Nephrol. Dial. Transplant. 2013, 28, 2586–2595. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, A.C.; Amparo, F.C.; Oliveira, M.A.; Amodeo, C.; Smanio, P.; Pinto, I.M.; Lindholm, B.; Stenvinkel, P.; Carrero, J.J. Epicardial fat accumulation, cardiometabolic profile and cardiovascular events in patients with stages 3-5 chronic kidney disease. J. Intern. Med. 2015, 278, 77–87. [Google Scholar] [CrossRef]
- Mariani, S.; Fiore, D.; Barbaro, G.; Basciani, S.; Saponara, M.; D’Arcangelo, E.; Ulisse, S.; Moretti, C.; Fabbri, A.; Gnessi, L. Association of epicardial fat thickness with the severity of obstructive sleep apnea in obese patients. Int. J. Cardiol. 2013, 167, 2244–2249. [Google Scholar] [CrossRef] [PubMed]
- Lubrano, C.; Saponara, M.; Barbaro, G.; Specchia, P.; Addessi, E.; Costantini, D.; Tenuta, M.; Di Lorenzo, G.; Genovesi, G.; Donini, L.M.; et al. Relationships between body fat distribution, epicardial fat and obstructive sleep apnea in obese patients with and without metabolic syndrome. PLoS ONE 2012, 7, e47059. [Google Scholar] [CrossRef]
- El Khoudary, S.R.; Shields, K.J.; Janssen, I.; Hanley, C.; Budoff, M.J.; Barinas-Mitchell, E.; Everson-Rose, S.A.; Powell, L.H.; Matthews, K.A. Cardiovascular Fat, Menopause, and Sex Hormones in Women: The SWAN Cardiovascular Fat Ancillary Study. J. Clin. Endocrinol. Metab. 2015, 100, 3304–3312. [Google Scholar] [CrossRef]


| Study | Design | N. Pts | Population | Imaging Method | EAT Evaluation |
|---|---|---|---|---|---|
| Eisenberg et al. [41] | Prospective (FU over 14 years) | 2068 | Asymptomatic subjects | CT | Increased EAT volume and decreased EAT attenuation were both independently associated with MACE |
| Raggi et al. [45] | RCT (FU 1 year) | 420 | Postmenopausal women with atherosclerosis and hypercholesterolemia | CT | Statins reduced the attenuation of EAT |
| Commandeur et al. [52] | Prospective (FU over 14 years) | 1912 | Asymptomatic subjects | CT | An objective machine learning score evaluating EAT was useful for the prediction of long-term risk of myocardial infarction and cardiac death |
| Nerlekar et al. [53] | Prospective (FU over 4 years) | 90 | Patients with non-obstructive coronary atherosclerosis | CT | EAT demonstrated significant longitudinal changes with an increase in volume and decrease in density |
| Forouzandeh et al. [54] | Prospective (FU over 4 years) | 760 | Patients with acute chest pain | CT | EAT volume was independently associated with MACE |
| Almeida et al. [55] | Prospective (FU 24 weeks) | 54 | Patients with myocardial infarction or unstable angina | CT | A 5-lipoxygenase inhibitor reduced EAT with a correlation between change in EAT and total plaque volume |
| Soucek et al. [56] | Prospective (FU 3 months) | 79 | Atrial fibrillation patients who underwent pulmonary vein isolation | CT | An intensive atorvastatin therapy was associated with a decrease in EAT |
| Gepner et al. [57] | RCT (FU 18 months) | 278 | Sedentary adults with abdominal obesity or dyslipidemia | CMR | Improving nutritional quality and being physically active could decrease cardiometabolic risk through changes in visceral fat depots, like EAT |
| Zeb et al. [58] | RCT (FU 1 year) | 60 | Asymptomatic subjects | CT | Aged garlic extract with supplement could determine a decrease in EAT |
| Ahmadi et al. [59] | RCT (FU 1 year) | 60 | Asymptomatic subjects | CT | Aged garlic extract with supplement could determine a decrease in EAT |
| Maimaituxun et al. [60] | Cross-sectional | 197 | CAD patients vs. non-CAD patients | CT | The local fat thickness surrounding the LAD artery was a marker for estimating the presence, severity and extent of CAD |
| Lu et al. [61] | Cross-sectional | 467 | Patients with suspected acute coronary syndrome | CT | A greater volume of EAT was associated with high-risk coronary plaques |
| Tsushima et al. [62] | Cross-sectional | 352 | Patients with suspected coronary artery disease | CT | A high EAT volume was associated with the presence of non-calcified coronary plaques |
| Parisi et al. [63] | Cross-sectional | 139 | Patients with severe, isolated, calcific aortic stenosis | Echocardiography | EAT could promote degeneration and calcification of the aortic valve |
| Tam et al. [64] | Retrospective | 116 | Patients with suspected coronary artery disease | CT | EAT could promote the occurrence of ventricular premature beats |
| Canpolat et al. [65] | Prospective (FU over 20 months) | 234 | Patients with symptomatic atrial fibrillation subjected to cryoablation | Echocardiography | Preprocedural EAT seemed to predict atrial fibrillation recurrence rate after cryoablation |
| Ohyama et al. [66] | Cross-sectional | 66 | Patients with LAD spasm vs. healthy controls | CT | PVAT had a role in the pathogenesis of coronary spasm |
| Gastelurrutia et al. [67] | RCT (FU 1 year) | 108 | Patients with non-revascularisable myocardial infarction | CMR | A population of human adult mesenchymal-like cells derived from EAT could act as a cellular reservoir for myocardial tissue renewal |
| Study | Design | N. Pts | Population | Imaging Method | EAT Evaluation |
|---|---|---|---|---|---|
| Sato et al. [68] | RCT (FU 6 months) | 35 | Diabetic patients | CT | Greater ↓ EAT volume during dapaglifozin treatment than conventional therapy |
| Iacobellis et al. [69] | RCT (FU 6 months) | 85 | Diabetic patients | Echocardiography | Greater ↓ EAT during liraglutide plus metformin treatment than only metformin |
| Christensen et al. [70] | RCT (FU 12 weeks) | 39 | Patients with abdominal obesity | CMR | Both endurance and resistance training reduced EAT mass |
| Fernandez-del-Valle et al. [71] | RCT (FU 5 weeks) | 11 | Young females with obesity | CMR | Short-term, high-intensity and moderate-volume resistance training reduced EAT |
| Rosety et al. [72] | Prospective (FU 12 weeks) | 48 | Obese aged women | Echocardiography | Resistance training reduced EAT thickness |
| Iacobellis et al. [73] | Prospective (FU 6 months) | 20 | Severely obese patients | Echocardiography | Significant weight loss could be associated with a reduction in the EAT thickness, involving cardiac morphological and functional changes |
| Serrano-Ferrer et al. [74] | Prospective (FU 6 months) | 131 | Metabolic syndrome patients vs. healthy controls | Echocardiography | EAT decreased following lifestyle intervention (partly explaining myocardial function improvements) |
| Jo et al. [75] | Prospective (FU 8 weeks) | 34 | Hypertensive metabolic syndrome patients | Echocardiography | Greater ↓ EAT with high-intensity interval training than moderate-intensity continuous training |
| Fornieles Gonzalez et al. [76] | Prospective (FU 16 weeks) | 60 | Menopausal women with metabolic syndrome | Echocardiography | EAT decreased with a supervised home-based 16-week treadmill training program |
| Mohar et al. [77] | Cross-sectional | 39 | Diabetic patients | CT | Increased EAT volume was associated with the presence of severe CAD |
| Groves et al. [78] | Cross-sectional | 362 | Diabetic patients vs. healthy controls | CT | Increased EAT volume was associated with greater severity of CAD in patients with and without diabetes |
| Hiruma et al. [79] | RCT (FU 12 weeks) | 42 | Diabetic patients | CMR | Empaglifozin had similar effects as sitagliptin on EAT accumulation |
| Leroux-Stewart et al. [80] | RCT (FU 16 weeks) | 73 | Diabetic patients | Echocardiography | Greater ↓ EAT thickness during caloric restriction diet associated with physical activity |
| Snel et al. [81] | Prospective (FU 14 months) | 14 | Diabetic obese patients | CMR | EAT decreased after a 16-week low-calorie diet (reduction maintained also after 14 months on a regular diet) |
| Bouchi et al. [82] | Prospective (FU 12 weeks) | 19 | Diabetic overweight/obese patients | CMR | Luseoglifozin may impact cardiovascular risk partly by reducing the EAT volume |
| Iacobellis et al. [83] | RCT (FU 24 weeks) | 84 | Diabetic overweight/obese patients | Echocardiography | Dapagliflozin caused EAT reduction |
| Dutour et al. [84] | RCT (FU 26 weeks) | 38 | Diabetic obese patients | CMR | Exenatide caused EAT reduction |
| Morano et al. [85] | Prospective (FU 3 months) | 25 | Diabetic patients | Echocardiography | A short course of GLP-1 RA treatment induced a redistribution of EAT deposits |
| Elisha et al. [86] | RCT (FU 6 months) | 56 | Diabetic patients | Echocardiography | Greater ↓ EAT thickness with insulin detemir than insulin glargine |
| Murai et al. [87] | Cross-sectional | 208 | Diabetic patients | CT | A close relationship existed between EAT accumulation and cystatin C level |
| Bayomy et al. [88] | Cross-sectional | 51 | Diabetic patients | CMR | PAI-1 levels positively correlated with EAT volume |
| Study | Design | N. Pts | Population | Imaging Method | EAT Evaluation |
|---|---|---|---|---|---|
| Nakanishi et al. [89] | Cross-sectional | 275 | CKD patients vs. non-CDK patients | CT | Greater EAT volume and high-risk coronary plaques in CKD patients |
| Yazbek et al. [90] | Prospective (FU 1 year) | 98 | Kidney transplant patients | CT | No relationship between the presence/progression of coronary calcification and EAT |
| Altun et al. [91] | Cross-sectional | 102 | Hemodialysis patients vs. healthy controls | Echocardiography | EAT thickness may be a useful indicator of early atherosclerosis |
| Ko et al. [92] | Prospective (FU 18 months) | 109 | Hemodialysis patients | CT | Lower EAT progression with Sevelamer than another calcium-based phosphate binder |
| Cetin et al. [93] | Prospective (FU 24 weeks) | 162 | Obstructive sleep apnea patients | Echocardiography | Greater EAT with AHI > 15. CPAP therapy may induce EAT regression |
| El Khoudary et al. [94] | RCT (FU 48 months) | 474 | Menopausal women | CT | Oral conjugated equine estrogens may slow EAT accumulation |
| Kahl et al. [95] | RCT (FU 6 weeks) | 30 | Depressed patients | CMR | Exercise training decreased the amount of visceral fat, in particular, EAT |
| Pacifico et al. [96] | RCT (FU 6 months) | 51 | Overweight children with NAFLD | Echocardiography | Docosahexaenoic acid supplementation decreased EAT |
| Farghaly et al. [97] | Cross-sectional | 32 | Subclinical hypothyroidism children vs. healthy children | Echocardiography | Greater EAT in children with subclinical hypothyroidism |
| Celik et al. [98] | Cross-sectional | 75 | Children with premature adrenarche vs. healthy children | Echocardiography | Greater EAT in children with premature adrenarche (positively correlated with DHEA-SO4 level) |
| Longenecker et al. [99] | Cross-sectional | 118 | HIV patients | CT | EAT volume and density were related to insulin resistance at baseline |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tarsitano, M.G.; Pandozzi, C.; Muscogiuri, G.; Sironi, S.; Pujia, A.; Lenzi, A.; Giannetta, E. Epicardial Adipose Tissue: A Novel Potential Imaging Marker of Comorbidities Caused by Chronic Inflammation. Nutrients 2022, 14, 2926. https://doi.org/10.3390/nu14142926
Tarsitano MG, Pandozzi C, Muscogiuri G, Sironi S, Pujia A, Lenzi A, Giannetta E. Epicardial Adipose Tissue: A Novel Potential Imaging Marker of Comorbidities Caused by Chronic Inflammation. Nutrients. 2022; 14(14):2926. https://doi.org/10.3390/nu14142926
Chicago/Turabian StyleTarsitano, Maria Grazia, Carla Pandozzi, Giuseppe Muscogiuri, Sandro Sironi, Arturo Pujia, Andrea Lenzi, and Elisa Giannetta. 2022. "Epicardial Adipose Tissue: A Novel Potential Imaging Marker of Comorbidities Caused by Chronic Inflammation" Nutrients 14, no. 14: 2926. https://doi.org/10.3390/nu14142926
APA StyleTarsitano, M. G., Pandozzi, C., Muscogiuri, G., Sironi, S., Pujia, A., Lenzi, A., & Giannetta, E. (2022). Epicardial Adipose Tissue: A Novel Potential Imaging Marker of Comorbidities Caused by Chronic Inflammation. Nutrients, 14(14), 2926. https://doi.org/10.3390/nu14142926





