Development and Validation of Nutrition Literacy Assessment Instrument for Chinese Pregnant Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Development of NLAI-P
2.2. The Validation of NLAI-P
2.2.1. Data Collection
2.2.2. Validity Test
2.2.3. Reliability
2.3. The Application of NLAI-P
2.4. Statistical Analysis
3. Results
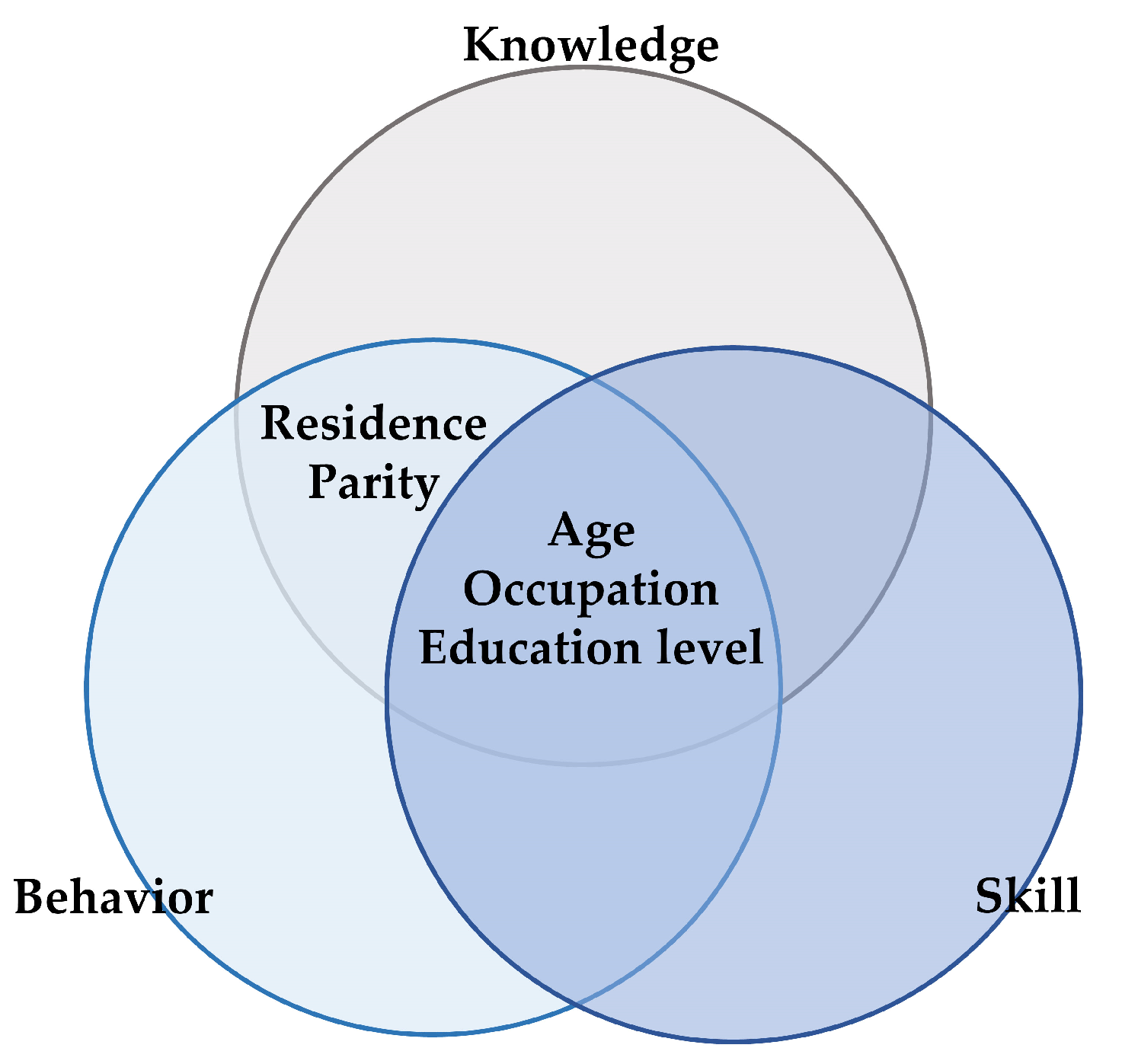
3.1. The Dimension and Components of NLAI-P
3.2. Demographic Characteristics in Confirmatory Study
3.3. Content Validity
3.3.1. I-CVI and CVR
3.3.2. Pearson Correlation Coefficient
3.4. Construct Validity Test
3.4.1. Exploratory Factor Analysis
3.4.2. Confirmatory Factor Analysis
3.5. Reliability and Validity
Internal Consistency and Spilt-Half Reliability
3.6. Assessing Nutrition Literacy for Pregnant Women in China and Its Related Factors
3.6.1. The NLAI-P Scores of Chinese Pregnant Women
3.6.2. The Potential Factors Influencing Nutrition Literacy of Chinese Pregnant Women
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gibbs, H.D.; Ellerbeck, E.F.; Befort, C.; Gajewski, B.; Kennett, A.R.; Yu, Q.; Christifano, D.; Sullivan, D.K. Measuring Nutrition Literacy in Breast Cancer Patients: Development of a Novel Instrument. J. Cancer Educ. 2016, 31, 493–499. [Google Scholar] [CrossRef] [Green Version]
- Gibbs, H.D.; Ellerbeck, E.F.; Gajewski, B.; Zhang, C.; Sullivan, D.K. The Nutrition Literacy Assessment Instrument is a Valid and Reliable Measure of Nutrition Literacy in Adults with Chronic Disease. J. Nutr. Educ. Behav. 2017, 50, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Velardo, S. The Nuances of Health Literacy, Nutrition Literacy, and Food Literacy. J. Nutr. Educ. Behav. 2015, 47, 385–389.e381. [Google Scholar] [CrossRef]
- Yuen, E.Y.N.; Thomson, M.; Gardiner, H. Measuring Nutrition and Food Literacy in Adults: A Systematic Review and Appraisal of Existing Measurement Tools. HLRP Health Lit. Res. Pract. 2018, 2, e134–e160. [Google Scholar] [CrossRef] [Green Version]
- Silk, K.J.; Sherry, J.; Winn, B.; Keesecker, N.; Horodynski, M.A.; Sayir, A. Increasing nutrition literacy: Testing the effectiveness of print, web site, and game modalities. J. Nutr. Educ. Behav. 2008, 40, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Zoellner, J.; Connell, C.; Bounds, W.; Crook, L.; Yadrick, K. Nutrition literacy status and preferred nutrition communication channels among adults in the Lower Mississippi Delta. Prev. Chronic Dis. 2009, 6, A128. [Google Scholar] [PubMed]
- Doustmohammadian, A.; Omidvar, N.; Keshavarz-Mohammadi, N.; Abdollahi, M.; Amini, M.; Eini-Zinab, H. Developing and validating a scale to measure Food and Nutrition Literacy (FNLIT) in elementary school children in Iran. PLoS ONE 2017, 12, e0179196. [Google Scholar] [CrossRef] [Green Version]
- CPC Central Committee; The State Council. The Outline of the Healthy China 2030 Plan. Available online: http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm (accessed on 25 October 2021).
- Caixia, D.; Shian, Y. The ten-year retrospect of nutrition and health status of pregnant women in China. Chin. J. Prev. Med. 2018, 52, 94–100. [Google Scholar]
- Ye, B.; Yifan, D.; Jie, W.; Shan, J.; Xuehong, P.; Shian, Y.; Zhenyu, Y.; Jianqiang, L. Status and related factors for gestational weight gain of Chinese pregnant women during 2010–2012. Chin. J. Prev. Med. 2018, 52, 26–30. [Google Scholar]
- Shan, J.; Xuehong, P.; Yifan, D.; Ye, B.; Jie, W.; Shian, Y.; Lichen, Y.; Zhenyu, Y. The influencing factors ofanemia for pregnant women between 2010–2012 in China. Chin. J. Prev. Med. 2018, 52, 21–25. [Google Scholar]
- Diamond, J.J. Development of a reliable and construct valid measure of nutritional literacy in adults. Nutr. J. 2007, 6, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibbs, H.D. Nutrition Literacy: Foundations and Development of an Instrument for Assessment. Ph.D. Thesis, University of Illinois at Urbana, Champaign, IL, USA, 2012. [Google Scholar]
- Aihara, Y.; Minai, J. Barriers and catalysts of nutrition literacy among elderly Japanese people. Health Promot. Int. 2011, 26, 421–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cassar, A.M.; Denyer, G.S.; O’Connor, H.T.; Gifford, J.A. A Qualitative Investigation to Underpin the Development of an Electronic Tool to Assess Nutrition Literacy in Australians Adults. Nutrients 2018, 10, 251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Zhang, Z.; Xu, M.; Aihemaitijiang, S.; Ye, C.; Zhu, W.; Ma, G. Development and Validation of a Food and Nutrition Literacy Questionnaire for Chinese Adults. Nutrients 2022, 14, 1933. [Google Scholar] [CrossRef]
- Aihemaitijiang, S.; Ye, C.; Halimulati, M.; Huang, X.; Wang, R.; Zhang, Z. Development and Validation of Nutrition Literacy Questionnaire for the Chinese Elderly. Nutrients 2022, 14, 1005. [Google Scholar] [CrossRef]
- Liu, T.; Su, X.; Li, N.; Sun, J.; Ma, G.; Zhu, W. Development and validation of a food and nutrition literacy questionnaire for Chinese school-age children. PLoS ONE 2021, 16, e0244197. [Google Scholar] [CrossRef]
- Zhou, Y.L.; Liu, W.; Li, Y.; Qin, Y.; Li, R.J.; Yu, L.L.; Chen, Y.H.; Xu, Y.J. Establishment of nutrition literacy core items for Chinese pregnant women. Chin. J. Prev. Med. 2020, 54, 1081–1086. [Google Scholar]
- Lawshe, C.H. A quantitative approach to content validity. Pers. Psychol. 1975, 28, 563–575. [Google Scholar] [CrossRef]
- Shum, J.W.H.; Lam, W.W.T.; Choy, B.N.K.; Chan, J.C.H.; Ho, W.L.; Lai, J.S.M. Development and pilot-testing of patient decision aid for use among Chinese patients with primary open-angle glaucoma. BMJ Open Ophthalmol. 2017, 2, e000100. [Google Scholar] [CrossRef] [Green Version]
- Souza, A.C.; Alexandre, N.M.C.; Guirardello, E.B. Psychometric properties in instruments evaluation of reliability and validity. Epidemiol. Serv. Saude 2017, 26, 649–659. [Google Scholar] [CrossRef]
- Pronk, T.; Molenaar, D.; Wiers, R.W.; Murre, J. Methods to split cognitive task data for estimating split-half reliability: A comprehensive review and systematic assessment. Psychon. Bull. Rev. 2021, 29, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, H.; Kennett, A.; Sullivan, D.; Kerling, E.; Thodosoff, J. A Pilot Study to Explore the Correlation between Parental Nutrition Literacy, BMI, and Child Healthy Eating Index—2010. J. Nutr. Educ. Behav. 2014, 46, S153. [Google Scholar] [CrossRef]
- Gibbs, H.; Chapman-Novakofski, K. Developing a novel measurement of nutrition literacy. In Proceedings of the 141st APHA Annual Meeting and Exposition 2013, Boston, MA, USA, 2–6 November 2013. [Google Scholar]
- Murimi, M.W. Healthy Literacy, Nutrition Education, and Food Literacy. J. Nutr. Educ. Behav. 2013, 45, 195. [Google Scholar] [CrossRef]
- Carbone, E.T.; Zoellner, J.M. Nutrition and health literacy: A systematic review to inform nutrition research and practice. J. Acad. Nutr. Diet. 2012, 112, 254. [Google Scholar] [CrossRef]
- Institute of Medicine. Health Literacy: A Prescription to End Confusion; National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- Ndahura, N.B. Nutrition literacy status of adolescent students in Kampala district, Uganda. 2012. Available online: https://hdl.handle.net/10642/1200 (accessed on 25 October 2012).
- Liao, L.L.; Lai, I.J. Construction of Nutrition Literacy Indicators for College Students in Taiwan: A Delphi Consensus Study. J. Nutr. Educ. Behav. 2017, 49, 734–742.e731. [Google Scholar] [CrossRef]
- Chau, P.H.; Leung, A.Y.; Li, H.L.; Sea, M.; Chan, R.; Woo, J. Development and Validation of Chinese Health Literacy Scale for Low Salt Consumption-Hong Kong Population (CHLSalt-HK). PLoS ONE 2015, 10, e0132303. [Google Scholar] [CrossRef] [Green Version]
- National Health Comission of the People’s Republic of China. Chinese Citizens’ Health Literacy 66 Items—Basic Knowledge and Skills. 2015. Available online: http://www.nhc.gov.cn/xcs/s3582/201601/766ff12e01844a64a80f23949f5d351b.shtml (accessed on 25 October 2021).
- Shan, D.; Qi, Z.; Jing, L.; Rong, X.; Huanling, Y. Investigation of nutritional knowledge, attitude and health behavior of pregnant women and analysis of influencing factors. Matern. Child Health Care China 2016, 31, 345–347. [Google Scholar]
- Qianain, H. The Establishment and Application Research of the Nutrition Knowlegde, Attitude and Practice Questionnaire for Pregnant Women. M.D. Thesis, Anhui Medical University, Hefei, China, 2009. [Google Scholar]
- Monteiro, M.; Fontes, T.; Ferreira-Pêgo, C. Nutrition Literacy of Portuguese Adults—A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 3177. [Google Scholar] [CrossRef]

| Scales | Sub-Scales | Items |
|---|---|---|
| Basic knowledge and ideas | Basic nutrition concept | 1. Reasonable nutrition during pregnancy has crucial impacts on the short-term and long-term health of both mothers and children. |
| 2. Appropriate gestational weight gain contributes to optimal pregnancy outcomes. | ||
| 3. Smoking and drinking during pregnancy are likely to cause miscarriage, premature and fetal malformation. | ||
| Food and nutrition knowledge | 4. Milk is rich in calcium and easily absorbed, making it an ideal food source of calcium. | |
| 5. Animal liver, eggs, legumes, green leafy vegetables, fruits and nuts are good food sources of folic acid. | ||
| Nutrition and disease knowledge | 6. Insufficient dietary iron intake very likely leads to iron deficiency or iron deficiency anemia in pregnant women and infants. | |
| 7. Iodine deficiency during pregnancy can impair the brain and intellectual development of the fetus. | ||
| 8. Increased intake of food rich in dietary fiber during pregnancy can help relieve constipation in pregnant women. | ||
| 9. Insufficient carbohydrate intake in early pregnancy can impair the development of fetal nervous system. | ||
| Lifestyle and dietary behaviors | Lifestyles | 10. At least 30 min of physical activity should be carried out every day during pregnancy if physically able, and vigorous exercise and heavy labor should be avoided. |
| Dietary behaviors | 11. Keep foods diversified and nutrition balanced during pregnancy. | |
| 12. From 3 months before pregnancy, 400 μg folic acid supplements used can prevent fetal neural tube development deformity. | ||
| 13. In severe cases of morning sickness, it is not necessary to overemphasize balanced diet, but to ensure adequate intake of cereals and tubers. | ||
| 14. Ensure adequate daily intake of water intake and avoid or limit beverages containing sugar, caffeine during pregnancy. | ||
| 15. Eat deep-sea fish 2–3 times per week during pregnancy to provide the fetus with n-3 long-chain polyunsaturated fatty acids that play an important role in retinal development. | ||
| 16. Increase properly the intake of iron-rich animal food in the second and third trimesters and eat animal blood and liver 1–2 times per week. | ||
| 17. Choose iodized salt, often eat iodine-rich seafood such as kelp, laver. | ||
| 18. From the second trimester, increase intake of milk by 200 mL per day in order to make total intake of milk reach 400–500 mL per day. | ||
| Preparation for breastfeeding | 19. Pregnant women should actively prepare for breastfeeding and learn the methods and skills of successful breastfeeding. | |
| Basic skills | Gestational weight management | 20. Monitoring and managing your weight before pregnancy. Measure gestational weight once a month in early pregnancy and once a week in the second and third trimester. |
| Gestational disease management | 21. Pay attention to blood glucose changes and judge the risk factors of diabetes. Pregnant women with gestational diabetes mellitus should strengthen the skill in disease self-management. | |
| 22. Pay attention to blood pressure changes and judge the risk factors of hypertension. Pregnant women with hypertension syndromes should strengthen the skill in disease self-management. | ||
| Judgement of nutrition information, and nutrition decision making | 23. Read and understand food labels and choose packaged food wisely. | |
| Acquisition, understanding and application of nutrition information | 24. Pay attention to nutrition-related information during pregnancy, and be able to obtain, understand, screen and apply nutrition information during pregnancy. |
| Dimension | Components | Questions |
|---|---|---|
| Knowledge | food, nutrition and health | 11 |
| knowledge of balanced diet and healthy lifestyles | 5 | |
| weight management | 5 | |
| risk factors of pregnancy complications | 2 | |
| Behavior | healthy eating behaviors | 3 |
| healthy lifestyles | 4 | |
| Skill | food group and nutrition label analysis | 4 |
| judgement of nutrition information | 2 | |
| nutrition information access and nutrition-related decisions making | 2 | |
| NLAI-P | 38 |
| Variables | n = 699 |
|---|---|
| Age | 31.2 ± 4.1 |
| <25 | 28 (4) |
| 25–30 | 215 (30.8) |
| 30–35 | 346 (49.5) |
| >35 | 104 (14.9) |
| Height (cm) | 162.6 ± 5.1 |
| Pre-pregnancy body weight (g) | 117.6 ± 20.7 |
| Body weight (g) | 130.7 ± 23.6 |
| Pre-pregnancy BMI (kg/m2) | 22.2 ± 3.6 |
| BMI (kg/m2) | 24.7 ± 4.2 |
| Gestational weight gain (g) | 6.5 ± 5.8 |
| Ethnicity | |
| Han | 658 (94.1) |
| Non-Han | 38 (5.4) |
| Residence | |
| East | 613 (87.7) |
| Middle | 69 (9.9) |
| West | 17 (2.4) |
| Career | |
| Housewife | 151 (21.6) |
| Civil servant | 108 (15.5) |
| Professional | 179 (25.6) |
| Service industry | 121 (17.3) |
| Others | 140 (20) |
| Education | |
| Junior high school or below | 21 (3) |
| Senior high school | 74 (10.6) |
| University | 263 (37.6) |
| Master degree or above | 341 (48.7) |
| Parity | |
| 1 | 344 (49.2) |
| ≥1 | 355 (50.8) |
| Gestational week | |
| 1st TM b | 176 (25.2) |
| 2nd TM | 254 (36.3) |
| 3rd TM | 269 (38.5) |
| Dimension | S-CVI | CVR | I-CVI | ICC (95% CI) |
|---|---|---|---|---|
| Knowledge | 0.99 | 0.98 | 0.85–1.0 | 0.54 (0.28, 0.73) |
| Behavior | 0.98 | 0.96 | 0.71–1.0 | 0.63 (0.24, 0.87) |
| Skill | 0.97 | 0.95 | 0.71–1.0 | 0.74 (0.42, 0.92) |
| NLAI-P | 0.98 | 0.97 | 0.71–1.0 | 0.61 (0.43, 0.76) |
| Dimension | Knowledge | Behavior | Skill |
|---|---|---|---|
| Knowledge | |||
| Behavior | 0.43 | ||
| Skill | 0.54 | 0.44 | |
| NLAI-P | 0.92 | 0.67 | 0.78 |
| Dimension | χ2/df | GFI | AGFI | RMSEA |
|---|---|---|---|---|
| NLAI-P | 1.82 | 0.86 | 0.84 | 0.046 |
| Knowledge | 1.61 | 0.93 | 0.92 | 0.039 |
| Behavior | 1.09 | 0.99 | 0.98 | 0.012 |
| Skill | 1.49 | 0.98 | 0.97 | 0.035 |
| Dimension | Cronbach’s α Coefficient | Spilt-Half Reliability | |
|---|---|---|---|
| Spearman Brown | Guttman Split-Half | ||
| Knowledge | 0.72 | 0.68 | 0.68 |
| Behavior | 0.65 | 0.67 | 0.67 |
| Skill | 0.68 | 0.59 | 0.52 |
| NLAI-P | 0.82 | 0.73 | 0.73 |
| Dimensions | Number of Questions | Total Scores | Scores | Minimum | Maximum | ≥80% n (%) | 60–80% n (%) | <60% n (%) |
|---|---|---|---|---|---|---|---|---|
| Knowledge | 23 | 46 | 28.6 ± 5.67 | 2.00 | 42.00 | 33 (4.7) | 424 (60.7) | 242 (34.6) |
| Behavior | 7 | 14 | 6.4 ± 2.69 | 0.50 | 16.00 | 30 (4.3) | 125 (17.9) | 544 (77.8) |
| Skill | 8 | 16 | 11.59 ± 3.02 | 1.90 | 16.00 | 329 (47.1) | 212 (30.3) | 158 (22.6) |
| NLAI-P | 38 | 76 | 46.59 ± 9.27 | 12.00 | 68.00 | 27 (3.9) | 386 (55.2) | 286 (40.9) |
| Variables | NLAI-P | Knowledge | Behavior | Skill | ||||
|---|---|---|---|---|---|---|---|---|
| Scores | p | Scores | p | Scores | p | Scores | p | |
| Age | 0.003 | 0.004 | 0.019 | 0.126 | ||||
| <25 (reference) | 40.3 ± 10.5 | 25 ± 5.9 | 4.9 ± 2.6 | 10.3 ± 3.3 | ||||
| 25–30 | 46.9 ± 8.7 * | 28.8 ± 5.3 * | 6.3 ± 2.8 * | 11.8 ± 2.8 * | ||||
| 30–35 | 47 ± 9.2 * | 28.9 ± 5.7 * | 6.5 ± 2.6 * | 11.6 ± 3 * | ||||
| >35 | 46.1 ± 9.6 * | 28.1 ± 5.9 * | 6.6 ± 2.6 * | 11.5 ± 3.1 | ||||
| Ethnicity | 0.554 | 0.360 | 0.607 | 0.167 | ||||
| Han (reference) | 46.4 ± 9.3 | 28.5 ± 5.7 | 6.4 ± 2.7 | 11.5 ± 3 | ||||
| Non-Han | 48.8 ± 8.2 | 29.7 ± 5.1 | 7 ± 2.9 | 12.2 ± 2.5 | ||||
| Residence | 0.016 | 0.045 | 0.410 | 0.010 | ||||
| East (reference) | 46.9 ± 8.9 | 28.8 ± 5.6 | 6.5 ± 2.6 | 11.7 ± 2.9 | ||||
| Middle | 43.6 ± 11.3 * | 27 ± 6.6 * | 6 ± 3.1 | 10.6 ± 3.4 * | ||||
| West | 46.7 ± 10.2 | 29.1 ± 4.9 | 6.3 ± 3 | 11.3 ± 3.8 | ||||
| Career | 0.000 | 0.000 | 0.003 | 0.000 | ||||
| Housewife (reference) | 43 ± 9.7 | 26.5 ± 6.2 | 5.8 ± 2.5 | 10.7 ± 3.3 | ||||
| Civil servant | 47.6 ± 9.5 * | 29 ± 5.7 * | 6.8 ± 3 * | 11.9 ± 3.1 * | ||||
| Professional | 49.7 ± 8.5 * | 30.5 ± 5.1 * | 6.9 ± 2.7 * | 12.3 ± 2.5 * | ||||
| Service industry | 45.2 ± 9.4 * | 27.6 ± 5.4 | 6.3 ± 2.9 | 11.2 ± 3.3 | ||||
| Others | 46.9 ± 7.9 * | 29 ± 5.1 * | 6.2 ± 2.4 | 11.6 ± 2.8 * | ||||
| Education | 0.000 | 0.000 | 0.000 | 0.000 | ||||
| Junior high school or below (reference) | 39.1 ± 10.4 | 24.4 ± 7 | 4.8 ± 2.3 | 9.8 ± 3 | ||||
| Senior high school | 40.3 ± 10.7 | 25.3 ± 6.2 | 5.4 ± 2.5 | 9.7 ± 3.7 | ||||
| University | 46 ± 8.8 * | 28.3 ± 5.5 | 6.3 ± 2.7 | 11.5 ± 3 | ||||
| Graduate or up | 48.9 ± 8.3 * | 29.8 ± 5.2 * | 6.8 ± 2.6 * | 12.2 ± 2.6 * | ||||
| Parity | 0.012 | 0.011 | 0.618 | 0.013 | ||||
| 1 (reference) | 47.5 ± 8.8 | 29.2 ± 5.4 | 6.5 ± 2.7 | 11.9 ± 2.9 | ||||
| ≥1 | 45.7 ± 9.6 | 28.1 ± 5.9 | 6.4 ± 2.6 | 11.3 ± 3.1 | ||||
| Gestational week | 0.900 | 0.307 | 0.070 | 0.648 | ||||
| 1st TM(reference) | 46.5 ± 9.7 | 28 ± 6.1 | 6.7 ± 2.7 | 11.8 ± 3.1 | ||||
| 2nd TM | 46.4 ± 9.6 | 28.8 ± 5.8 | 6.1 ± 2.7 | 11.5 ± 3 | ||||
| 3rd TM | 46.8 ± 8.7 | 28.8 ± 5.2 | 6.5 ± 2.7 | 11.5 ± 2.9 | ||||
| Variable | NLAI-P | Knowledge | Behavior | Skill | ||||
|---|---|---|---|---|---|---|---|---|
| β | p | β | p | β | p | β | p | |
| Education level | 3.67 * | 0.000 | 1.98 * | 0.000 | 0.69 * | 0.000 | 0.99 * | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, Y.; Lyu, Y.; Zhao, R.; Shi, H.; Ye, W.; Wen, Z.; Li, R.; Xu, Y. Development and Validation of Nutrition Literacy Assessment Instrument for Chinese Pregnant Women. Nutrients 2022, 14, 2863. https://doi.org/10.3390/nu14142863
Zhou Y, Lyu Y, Zhao R, Shi H, Ye W, Wen Z, Li R, Xu Y. Development and Validation of Nutrition Literacy Assessment Instrument for Chinese Pregnant Women. Nutrients. 2022; 14(14):2863. https://doi.org/10.3390/nu14142863
Chicago/Turabian StyleZhou, Yalin, Ying Lyu, Runlong Zhao, Hanxu Shi, Wanyun Ye, Zhang Wen, Rui Li, and Yajun Xu. 2022. "Development and Validation of Nutrition Literacy Assessment Instrument for Chinese Pregnant Women" Nutrients 14, no. 14: 2863. https://doi.org/10.3390/nu14142863
APA StyleZhou, Y., Lyu, Y., Zhao, R., Shi, H., Ye, W., Wen, Z., Li, R., & Xu, Y. (2022). Development and Validation of Nutrition Literacy Assessment Instrument for Chinese Pregnant Women. Nutrients, 14(14), 2863. https://doi.org/10.3390/nu14142863







