Cuffless and Touchless Measurement of Blood Pressure from Ballistocardiogram Based on a Body Weight Scale
Abstract
:1. Introduction
2. Materials and Methods
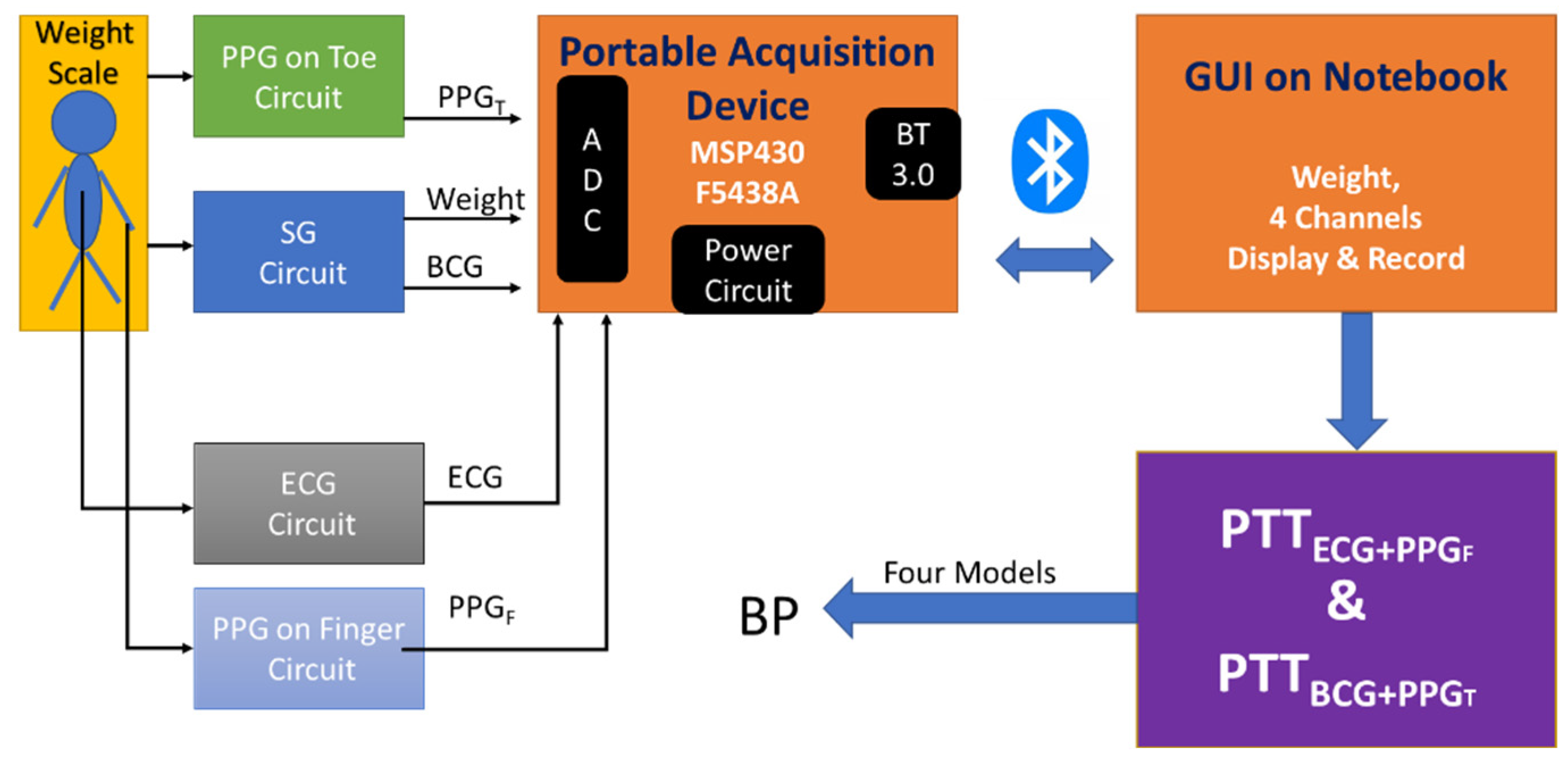
2.1. Portable Acquisition Device
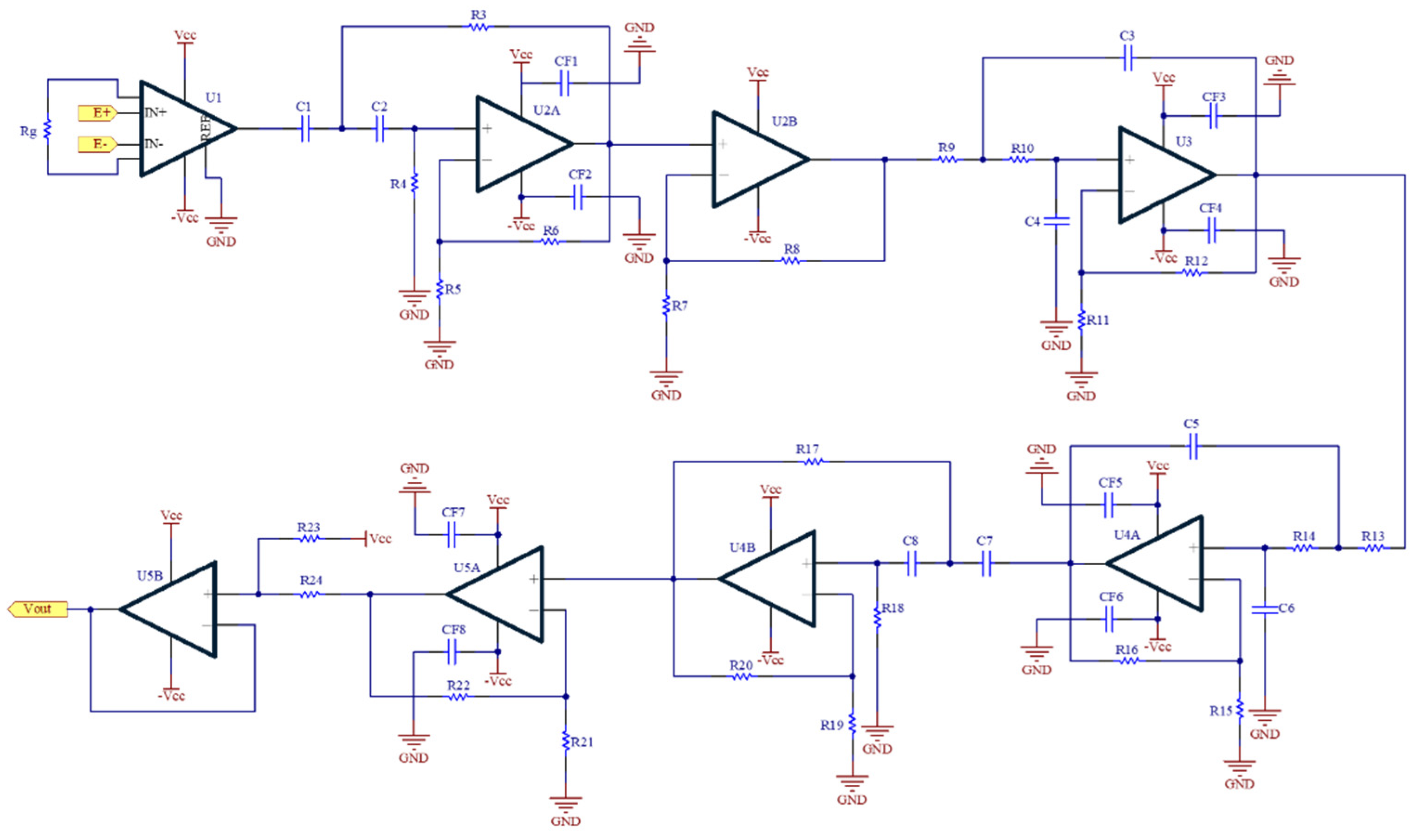
2.2. Ballistocardiograph Circuit
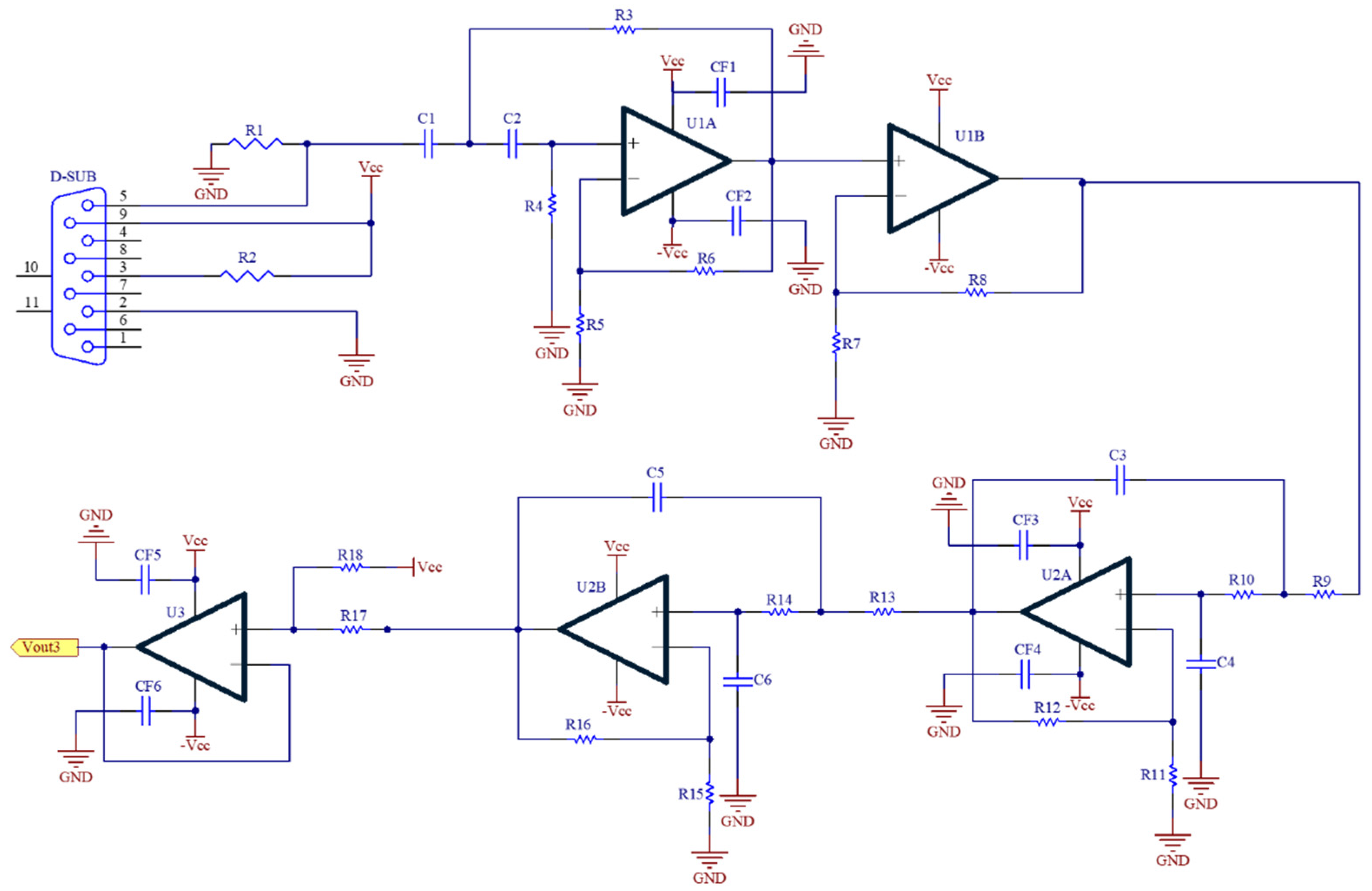
2.3. Photoplethysmograph Circuit
2.4. Electrocardiograph Module
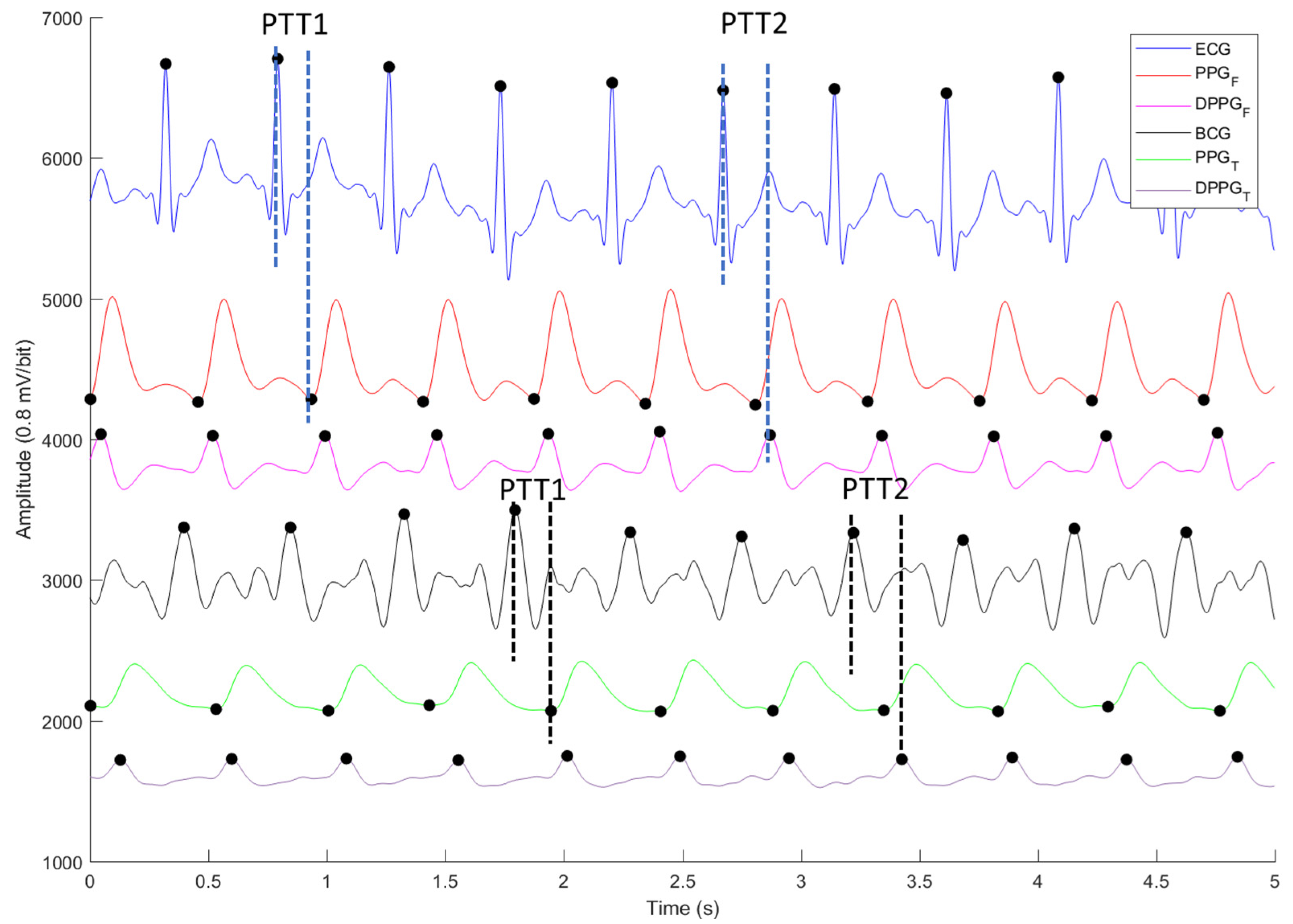
2.5. Digital Signal Processing
2.6. PTT Models for Blood Pressure Estimation
2.7. Statistic Analysis
2.8. Experiment Protocol
- Subjects stood on the weight scale to measure ECG, PPGF, PPGT, and BCG signals for five minutes, as shown in Figure 5. This measurement was used as the baseline of this experiment. At the same time, the blood pressure was measured once; and its finish-time was marked at the PPG signal.
- Subjects ran on the treadmill at a speed of about 6 km/h firstly for at least three minutes, and 8 km/h for the last four minutes.
- Subjects were requested to stand on the weight scale again, to measure ECG, PPGF, PPGT, and BCG signal for six minutes. The blood pressures of subjects were measured repeatedly once a minute within standing on the weight scale.
- One measurement would take about 18 min. Each subject was measured four times. The interval between two measurements was at least one week.
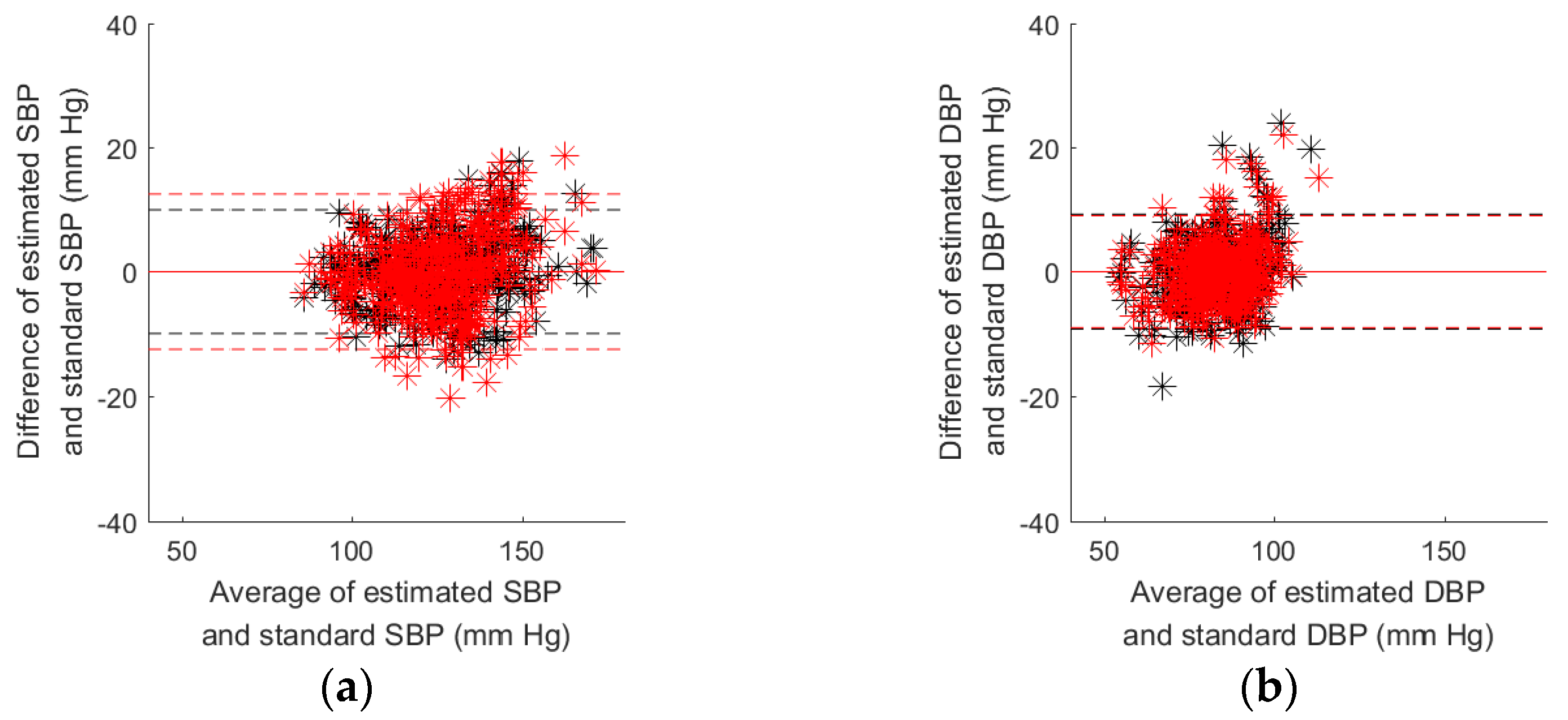
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- De Matos, D.G.; Aidar, F.J.; de Almeida-Neto, P.F.; Moreira, O.S.; de Souza, R.F.; Marcal, A.C.; Marcucci-Barbosa, L.S.; Martins Júnior, F.D.A.; Lobo, L.F.; dos Santos, J.L.; et al. The impact of measures recommended by the government to limit the spread of coronavirus (COVID-19) on physical activity levels, quality of life, and mental health of Brazilians. Sustainability 2020, 12, 9072. [Google Scholar] [CrossRef]
- Röhling, M.; Kempf, K.; Banzer, W.; Braumann, K.M.; Führer-Sakel, D.; Halle, M.; McCarthy, D.; Martin, S.; Scholze, J.; Toplak, H.; et al. A High-Protein and Low-Glycemic formula diet improves blood pressure and other hemodynamic parameters in High-Risk individuals. Nutrients 2022, 14, 1443. [Google Scholar] [CrossRef] [PubMed]
- Hermansen, K. Diet, blood pressure and hypertension. Br. J. Nutr. 2000, 83, 113–119. [Google Scholar] [CrossRef] [Green Version]
- Harsha, D.W.; Bray, G.A. Weight loss and blood pressure control (Pro). Hypertension 2008, 51, 1420–1425. [Google Scholar] [CrossRef] [Green Version]
- Neter, J.E.; Stam, B.E.; Kok, F.J.; Grobbee, D.E.; Geleijnse, J.M. Influence of weight reduction on blood pressure: A meta-analysis of randomized controlled trials. Hypertension 2003, 42, 878–884. [Google Scholar] [CrossRef]
- Mukkamala, R.; Hahn, J.O.; Inan, O.T.; Mestha, L.K.; Kim, C.S.; Töreyin, H.; Kyal, S. Toward ubiquitous blood pressure monitoring via pulse transit time: Theory and practice. IEEE Trans. Bio-Med. Eng. 2015, 62, 1879–1901. [Google Scholar] [CrossRef] [Green Version]
- Buxi, D.; Redouté, J.-M.; Yuce, M.R. A survey on signals and systems in ambulatory blood pressure monitoring using pulse transit time. Physiol. Meas. 2015, 36, R1-26. [Google Scholar] [CrossRef]
- Peter, L.; Noury, N.; Cerny, M. A review of methods for non-invasive and continuous blood pressure monitoring: Pulse transit time method is promising? IRBM 2014, 35, 271–282. [Google Scholar] [CrossRef]
- Ding, X.; Liu, J.; Dai, W.; Carvalho, P.; Magjarevic, R.; Zhang, Y.-T. An attempt to define the pulse transit time. In Proceedings of the International Conference on Biomedical and Health Informatics, Singapore, 9 October 2015. [Google Scholar]
- Huynh, T.H.; Jafari, R.; Chung, W.Y. Noninvasive cuffless blood pressure estimation using pulse transit time and impedance plethysmography. IEEE Trans. Bio-Med. Eng. 2019, 66, 967–976. [Google Scholar] [CrossRef]
- Liu, S.-H.; Cheng, D.-C.; Su, C.-H. A cuffless blood pressure measurement based on the impedance plethysmography technique. Sensors 2017, 17, 1176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buxi, D.; Redout, J.M.; Yuce, M.R. Blood pressure estimation using pulse transit time from bioimpedance and continuous wave radar. IEEE Trans. Bio-Med. Eng. 2017, 64, 917–927. [Google Scholar] [CrossRef] [PubMed]
- Weltman, G.; Sullivan, G.; Bredon, D. The continuous measurement of arterial pulse wave velocity. Med. Electron. Biol. Eng. 1964, 2, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Bramwell, J.C.; Hill, A.V. The velocity of the pulse wave in man. Proc. R. Soc. B Biol. Sci. 1922, 93, 298–306. [Google Scholar]
- Ahlstrom, C.; Johansson, A.; Uhlin, F.; Länne, T.; Ask, P. Noninvasive investigation of blood pressure changes using the pulse wave transit time: A novel approach in the monitoring of hemodialysis patients. J. Artif. Organs 2005, 8, 192–197. [Google Scholar] [CrossRef]
- Liu, S.-H.; Wang, J.-J.; Huang, K.-S. A new Oscillometry-Based Method for estimating the dynamic brachial artery compliance under loaded conditions. IEEE Trans. Biomed. Eng. 2008, 55, 2463–2470. [Google Scholar] [CrossRef]
- Rachim, V.P.; Chung, W.-Y. Multimodal wrist biosensor for wearable Cuff-less blood pressure monitoring system. Sci. Rep. 2019, 9, 7947. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, B.; Jafari, R. Cuffless blood pressure monitoring from an array of wrist Bio-Impedance sensors using Subject-Specific regression models: Proof of concept. IEEE Trans. Biomed. Circuits Syst. 2019, 13, 1723–1735. [Google Scholar] [CrossRef]
- Shin, S.; Yousefian, P.; Mousavi, A.S.; Kim, C.S.; Mukkamala, R.; Jang, D.G.; Ko, B.H.; Lee, J.; Kwon, U.K.; Kim, Y.H.; et al. A unified approach to wearable Ballistocardiogram gating and wave localization. IEEE Trans. Biomed. Eng. 2021, 68, 1115–1122. [Google Scholar] [CrossRef]
- Yousefian, P.; Shin, S.; Mousavi, A.S.; Kim, C.S.; Finegan, B.; McMurtry, M.S.; Mukkamala, R.; Jang, D.G.; Kwon, U.; Kim, Y.H.; et al. Physiological association between limb ballistocardiogram and arterial blood pressure waveforms: A mathematical model-based analysis. Sci. Rep. 2019, 9, 5146. [Google Scholar] [CrossRef] [Green Version]
- Inan, O.T.; Migeotte, P.F.; Park, K.S.; Etemadi, M.; Tavakolian, K.; Casanella, R.; Zanetti, J.; Tank, J.; Funtova, I.; Prisk, G.K.; et al. Ballistocardiography and seismocardiography: A review of recent advances. IEEE J. Biomed. Health Inform. 2015, 19, 1414–1427. [Google Scholar] [CrossRef] [Green Version]
- Martin, S.L.O.; Carek, A.M.; Kim, C.S.; Ashouri, H.; Inan, O.T.; Hahn, J.O.; Mukkamala, R. Weighing scale-based pulse transit time is a superior marker of blood pressure than conventional pulse arrival time. Sci. Rep. 2016, 6, 39273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ding, X.; Zhang, Y.-T. Pulse transit time technique for cuffless unobtrusive blood pressure measurement: From theory to algorithm. Biomed. Eng. Lett. 2019, 9, 37–52. [Google Scholar] [CrossRef]
- Liu, S.-H.; Wang, J.-J.; Tan, T.-H. A portable and wireless multi-channel acquisition system for physiological signal measurements. Sensors 2019, 19, 5314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, M.; Barbosa, K.; Ho, V.; Griggs, D.; Ghirmai, T.; Krishnan, S.K.; Hsiai, T.K.; Chiao, J.C.; Cao, H. Cuff-Less and Continuous Blood Pressure Monitoring: A Methodological Review. Technologies 2017, 5, 21. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.-H.; Wang, J.-J.; Su, C.-H.; Cheng, D.-C. Improvement of left ventricular ejection time measurement in the impedance cardiography combined with the reflection photoplethysmography. Sensors 2018, 18, 3036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.-H.; Wang, J.-J.; Chen, W.; Pan, K.-L.; Su, C.-H. Classification of photoplethysmographic signal quality with fuzzy neural network for improvement of stroke volume measurement. Appl. Sci. 2020, 10, 1476. [Google Scholar] [CrossRef] [Green Version]
- Geddes, L.A.; Voelz, M.H.; Babbs, C.F.; Bourland, J.D.; Tacker, W.A. Pulse transit time as an indicator of arterial blood pressure. Psychophysiology 1981, 18, 71–74. [Google Scholar] [CrossRef]
- Chen, W.; Kobayashi, T.; Ichikawa, S.; Takeuchi, Y.; Togawa, T. Continuous estimation of systolic blood pressure using the pulse arrival time and intermittent calibration. Med. Biol. Eng. Comput. 2000, 38, 569–574. [Google Scholar] [CrossRef]
- Zheng, Y.; Poon, C.C.Y.; Zhang, Y.-T. Investigation of temporal relationship between cardiovascular variables for cuffless blood pressure estimation. In Proceedings of the 2012 IEEE-EMBS International Conference on Biomedical and Health Informatics, Hong Kong, China, 5–7 January 2012. [Google Scholar]
- Allen, R.A.; Schneider, J.A.; Davidson, D.M.; Winchester, M.A.; Taylor, C.B. The covariation of blood pressure and pulse transit time in hypertensive patients. Psychophysiology 1981, 18, 301–306. [Google Scholar] [CrossRef]
- Ma, H.T. A blood pressure monitoring method for stroke management. Biomed Res. Int. 2014, 2014, 571623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García, M.T.G.; Acevedo, M.F.T.; Guzmán, M.R.; de Montaner, R.A.; Fernández, B.F.; del Río Camacho, G.; González-Mangado, N. Puede ser el tiempo de tránsito de pulso útil para detectar hipertensión arterial en pacientes remitidos a la unidad de sueño? Arch. Bronconeumol. 2014, 50, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Forouzanfar, M.; Ahmad, S.; Batkin, I.; Dajani, H.R.; Groza, V.Z.; Bolic, M. Model-based mean arterial pressure estimation using simultaneous electrocardiogram and oscillometric blood pressure measurements. IEEE Trans. Instrum. Meas. 2015, 64, 2443–2452. [Google Scholar] [CrossRef]
- Wong, M.-Y.; Poon, C.-C.; Zhang, Y.-T. An evaluation of the cuffless blood pressure estimation based on pulse transit time technique: A half year study on normotensive subjects. Cardiovasc. Eng. 2009, 9, 32–38. [Google Scholar] [CrossRef]
- Proença, J.; Muehlsteff, J.; Aubert, X.; Carvalho, P. Is pulse transit time a good indicator of blood pressure changes during short physical exercise in a young population? In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology (EMBC), Buenos Aires, Argentina, 31 August–4 September 2010. [Google Scholar]
- Cattivelli, F.S.; Garudadri, H. Noninvasive cuffless estimation of blood pressure from pulse arrival time and heart rate with adaptive calibration. In Proceedings of the 2009 Sixth International Workshop on Wearable and Implantable Body Sensor Networks, Berkeley, CA, USA, 3–5 June 2009. [Google Scholar]
- Heard, S.O.; Lisbon, A.; Toth, I.; Ramasubramanian, R. An evaluation of a new continuous blood pressure monitoring system in critically ill patients. J. Clin. Anesth. 2000, 12, 509–518. [Google Scholar] [CrossRef]
- Liu, S.-H.; Liu, L.-J.; Pan, K.-L.; Chen, W.; Tan, T.-H. Using the characteristics of pulse waveform to enhance the accuracy of blood pressure measurement by a multi-dimension regression model. Appl. Sci. 2019, 9, 2922. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.-T.; Liu, S.-H.; Wang, J.-J.; Wen, Z.-C. Reduction of interference in oscillometric arterial blood pressure measurement using fuzzy logic. IEEE Trans. Bio-Med. Eng. 2003, 50, 432–441. [Google Scholar]
- Young, C.C.; Mark, J.B.; White, W.; DeBree, A.; Vender, J.S.; Fleming, A. Clinical evaluation of continuous noninvasive blood pressure monitoring: Accuracy and tracking capabilities. J. Clin. Monit. 1995, 11, 245–252. [Google Scholar] [CrossRef]
- Zong, W.; Moody, G.B.; Mark, R.G. Effects of vasoactive drugs on the relationship between ECG-pulse wave delay time and arterial blood pressure in ICU patients. Comput. Cardiol. 1998, 25, 673–676. [Google Scholar]
- Sharwood-Smith, G.; Bruce, J.; Drummond, G. Assessment of pulse transit time to indicate cardiovascular changes during obstetric spinal anaesthesia. Br. J. Anesth. 2006, 96, 100–105. [Google Scholar] [CrossRef] [Green Version]
- Obrist, P.A.; Light, K.C.; McCubbin, J.A.; Hutcheson, J.; Hoffer, J.L. Pulse transit time: Relationship to blood pressure. Behav. Res. Methods Instrum. 1978, 10, 623–626. [Google Scholar] [CrossRef] [Green Version]
- Inan, O.T.; Park, D.; Giovangrandi, L.; Kovacs, G.T.A. Noninvasive Measurement of Physiological Signals on a Modified Home Bathroom Scale. IEEE Trans. Bio-Med. Eng. 2012, 59, 2137–2143. [Google Scholar] [CrossRef] [PubMed]
- Su, B.Y.; Enayati, M.; Ho, K.C.; Skubic, M.; Despins, L.; Keller, J.; Popescu, M.; Guidoboni, G.; Rantz, M. Monitoring the Relative Blood Pressure Using a Hydraulic Bed Sensor System. IEEE Trans. Bio-Med. Eng. 2019, 66, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Koivistoinen, T.; Junnila, S.; Värri, A.; Kööbi, T. A new method for measuring the ballistocardiogram using EMFi sensors in a normal chair. In Proceedings of the 2004 Annual International Conference of the IEEE Engineering in Medicine and Biology (EMBC), San Francisco, CA, USA, 1–5 September 2004. [Google Scholar]
- Allen, J.; Murray, A. Similarity in bilateral photoplethysmographic peripheral pulse wave characteristics at the ears, thumbs and toes. Physiol. Meas 2000, 21, 369–377. [Google Scholar] [CrossRef] [PubMed]

| Subject (N) | SBP Max.~Min. mmHg | DBP Max.~Min. mmHg | Subject (N) | SBP Max.~Min. mmHg | DBP Max.~Min. mmHg |
|---|---|---|---|---|---|
| 01 (N = 21) | 142~111 | 102~74 | 11 (N = 23) | 150~116 | 106~85 |
| 02 (N = 17) | 121~84 | 81~66 | 12 (N = 24) | 154~116 | 88~58 |
| 03 (N = 24) | 172~124 | 121~85 | 13 (N = 16) | 153~126 | 103~89 |
| 04 (N = 24) | 156~116 | 88~68 | 14 (N = 12) | 146~114 | 77~100 |
| 05 (N = 24) | 154~106 | 83~59 | 15 (N = 12) | 132~100 | 90~76 |
| 06 (N = 19) | 173~134 | 104~85 | 16 (N = 17) | 137~104 | 90~80 |
| 07 (N = 23) | 152~123 | 99~83 | 17 (N = 23) | 148~98 | 90~75 |
| 08 (N = 23) | 154~118 | 114~76 | 18 (N = 16) | 113~91 | 95~67 |
| 09 (N = 12) | 133~108 | 85~74 | 19 (N = 23) | 144~112 | 92~76 |
| 10 (N = 24) | 132~103 | 103~74 | 20 (N = 19) | 141~96 | 74~54 |
| Subjects | Reference Method | Proposed Method | ||||||
|---|---|---|---|---|---|---|---|---|
| SBP | DBP | SBP | DBP | |||||
| ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | |
| 01 | 5.0 | 0.740 | 5.2 | 0.193 | 9.672 | 0.031 | 5.7 | 0.019 |
| 02 | 6.8 | 0.472 | 4.4 | 0.001 | 7.598 | 0.348 | 4.1 | 0.145 |
| 03 | 8.2 | 0.641 | 7.0 | 0.062 | 13.760 | 0.000 | 5.7 | 0.376 |
| 04 | 8.7 | 0.445 | 4.9 | 0.014 | 11.675 | 0.005 | 4.9 | 0.004 |
| 05 | 4.7 | 0.831 | 5.2 | 0.330 | 7.608 | 0.570 | 5.6 | 0.234 |
| 06 | 9.6 | 0.296 | 4.9 | 0.098 | 8.772 | 0.424 | 5.1 | 0.034 |
| 07 | 6.9 | 0.359 | 3.8 | 0.276 | 8.665 | 0.012 | 4.4 | 0.014 |
| 08 | 7.8 | 0.476 | 8.0 | 0.059 | 9.609 | 0.218 | 8.1 | 0.030 |
| 09 | 4.6 | 0.609 | 2.7 | 0.023 | 5.702 | 0.408 | 2.7 | 0.000 |
| 10 | 4.7 | 0.714 | 5.8 | 0.066 | 6.646 | 0.443 | 5.3 | 0.227 |
| 11 | 5.7 | 0.583 | 6.8 | 0.026 | 7.624 | 0.278 | 6.8 | 0.000 |
| 12 | 4.8 | 0.783 | 6.6 | 0.159 | 10.218 | 0.047 | 6.4 | 0.221 |
| 13 | 5.8 | 0.501 | 3.5 | 0.371 | 8.210 | 0.003 | 4.4 | 0.004 |
| 14 | 5.8 | 0.685 | 5.8 | 0.273 | 9.523 | 0.164 | 6.8 | 0.003 |
| 15 | 4.1 | 0.839 | 3.9 | 0.155 | 7.300 | 0.499 | 3.7 | 0.233 |
| 16 | 7.2 | 0.350 | 1.9 | 0.432 | 8.185 | 0.175 | 2.5 | 0.001 |
| 17 | 13.6 | 0.063 | 3.5 | 0.003 | 12.846 | 0.171 | 3.5 | 0.008 |
| 18 | 5.1 | 0.583 | 7.5 | 0.143 | 7.655 | 0.078 | 8.1 | 0.001 |
| 19 | 3.0 | 0.902 | 2.7 | 0.235 | 9.445 | 0.039 | 3.0 | 0.029 |
| 20 | 9.4 | 0.565 | 6.2 | 0.228 | 13.079 | 0.161 | 6.5 | 0.155 |
| Mean ± SD | 6.6 ± 2.40 | 0.572 ± 0.204 | 5.0 ± 1.67 | 0.157 ± 0.128 | 9.2 ± 2.14 | 0.204 ± 0.181 | 5.2 ± 1.61 | 0.087 ± 0.111 |
| Subjects | Reference Method | Proposed Method | ||||||
|---|---|---|---|---|---|---|---|---|
| SBP | DBP | SBP | DBP | |||||
| ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | |
| 01 | 4.8 | 0.761 | 5.2 | 0.178 | 9.6 | 0.026 | 5.8 | 0.001 |
| 02 | 6.7 | 0.486 | 4.4 | 0.001 | 6.9 | 0.458 | 3.8 | 0.229 |
| 03 | 8.1 | 0.650 | 7.1 | 0.039 | 13.2 | 0.070 | 6.2 | 0.256 |
| 04 | 7.9 | 0.534 | 4.8 | 0.029 | 10.8 | 0.149 | 4.8 | 0.045 |
| 05 | 4.4 | 0.851 | 5.0 | 0.382 | 6.5 | 0.684 | 5.5 | 0.270 |
| 06 | 9.2 | 0.354 | 4.9 | 0.108 | 10.8 | 0.114 | 5.1 | 0.016 |
| 07 | 6.9 | 0.369 | 3.8 | 0.276 | 8.4 | 0.059 | 4.3 | 0.041 |
| 08 | 8.0 | 0.446 | 7.7 | 0.120 | 8.9 | 0.326 | 7.5 | 0.165 |
| 09 | 5.1 | 0.511 | 2.7 | 0.019 | 5.1 | 0.508 | 2.7 | 0.025 |
| 10 | 4.9 | 0.690 | 5.8 | 0.067 | 7.0 | 0.369 | 5.5 | 0.159 |
| 11 | 4.7 | 0.715 | 6.6 | 0.055 | 8.8 | 0.034 | 6.8 | 0.002 |
| 12 | 6.1 | 0.659 | 6.9 | 0.089 | 7.1 | 0.527 | 5.6 | 0.393 |
| 13 | 5.5 | 0.542 | 3.5 | 0.382 | 8.2 | 0.000 | 4.4 | 0.023 |
| 14 | 6.5 | 0.607 | 5.7 | 0.292 | 9.2 | 0.207 | 5.1 | 0.430 |
| 15 | 3.7 | 0.870 | 3.8 | 0.184 | 10.2 | 0.007 | 4.2 | 0.026 |
| 16 | 7.0 | 0.397 | 1.9 | 0.439 | 4.5 | 0.744 | 2.5 | 0.030 |
| 17 | 8.2 | 0.655 | 3.5 | 0.003 | 8.1 | 0.666 | 3.5 | 0.000 |
| 18 | 5.1 | 0.590 | 7.5 | 0.146 | 7.5 | 0.102 | 8.0 | 0.039 |
| 19 | 2.8 | 0.910 | 2.7 | 0.205 | 9.0 | 0.115 | 3.0 | 0.011 |
| 20 | 8.8 | 0.614 | 5.8 | 0.319 | 12.1 | 0.274 | 6.2 | 0.224 |
| Mean ± SD | 6.2 ± 1.74 | 0.611 ± 0.157 | 5.0 ± 1.65 | 0.167 ± 0.135 | 8.6 ± 2.12 | 0.272 ± 0.241 | 5.0 ± 1.48 | 0.119 ± 0.134 |
| Subjects | Reference Method | Proposed Method | ||||||
|---|---|---|---|---|---|---|---|---|
| SBP | DBP | SBP | DBP | |||||
| ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | |
| 01 | 4.8 | 0.766 | 5.4 | 0.179 | 7.3 | 0.477 | 5.6 | 0.112 |
| 02 | 4.3 | 0.798 | 3.0 | 0.553 | 5.3 | 0.703 | 3.4 | 0.441 |
| 03 | 8.3 | 0.650 | 7.2 | 0.052 | 11.0 | 0.384 | 6.4 | 0.256 |
| 04 | 7.5 | 0.608 | 4.8 | 0.098 | 9.0 | 0.436 | 4.5 | 0.210 |
| 05 | 4.5 | 0.853 | 4.6 | 0.505 | 6.1 | 0.734 | 4.1 | 0.597 |
| 06 | 5.9 | 0.749 | 5.0 | 0.122 | 6.8 | 0.673 | 5.0 | 0.120 |
| 07 | 7.0 | 0.378 | 3.8 | 0.283 | 7.6 | 0.276 | 4.3 | 0.102 |
| 08 | 8.0 | 0.478 | 7.9 | 0.121 | 7.5 | 0.546 | 7.6 | 0.188 |
| 09 | 2.4 | 0.905 | 2.7 | 0.105 | 4.8 | 0.607 | 2.7 | 0.069 |
| 10 | 5.0 | 0.693 | 5.8 | 0.121 | 6.9 | 0.413 | 5.5 | 0.197 |
| 11 | 4.3 | 0.772 | 6.1 | 0.243 | 7.9 | 0.255 | 7.0 | 0.012 |
| 12 | 6.2 | 0.659 | 7.0 | 0.091 | 6.9 | 0.579 | 5.5 | 0.434 |
| 13 | 5.5 | 0.570 | 3.4 | 0.449 | 6.3 | 0.444 | 3.5 | 0.407 |
| 14 | 6.8 | 0.613 | 6.0 | 0.294 | 8.0 | 0.463 | 5.4 | 0.433 |
| 15 | 3.0 | 0.920 | 3.7 | 0.299 | 6.3 | 0.662 | 3.7 | 0.304 |
| 16 | 5.7 | 0.618 | 2.0 | 0.444 | 3.5 | 0.857 | 2.4 | 0.158 |
| 17 | 8.3 | 0.665 | 3.6 | 0.013 | 8.2 | 0.671 | 3.6 | 0.003 |
| 18 | 4.8 | 0.651 | 7.8 | 0.148 | 4.9 | 0.644 | 7.3 | 0.243 |
| 19 | 2.9 | 0.911 | 2.8 | 0.209 | 7.4 | 0.435 | 2.9 | 0.126 |
| 20 | 7.8 | 0.718 | 5.3 | 0.482 | 7.9 | 0.710 | 5.2 | 0.501 |
| Mean ± SD | 5.7 ± 1.76 | 0.699 ± 0.138 | 4.9 ± 1.72 | 0.241 ± 0.162 | 7.0 ± 1.59 | 0.548 ± 0.157 | 4.8 ± 1.48 | 0.246 ± 0.167 |
| Subjects | Reference Method | Proposed Method | ||||||
|---|---|---|---|---|---|---|---|---|
| SBP | DBP | SBP | DBP | |||||
| ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | ERMS (mmHg) | r2 | |
| 01 | 4.9 | 0.770 | 5.4 | 0.203 | 5.8 | 0.684 | 5.5 | 0.192 |
| 02 | 4.4 | 0.807 | 2.8 | 0.639 | 5.2 | 0.734 | 3.5 | 0.447 |
| 03 | 8.3 | 0.664 | 6.7 | 0.219 | 10.7 | 0.446 | 5.7 | 0.435 |
| 04 | 7.2 | 0.654 | 4.8 | 0.138 | 8.8 | 0.483 | 4.5 | 0.231 |
| 05 | 4.3 | 0.871 | 4.7 | 0.505 | 5.8 | 0.767 | 4.2 | 0.615 |
| 06 | 5.9 | 0.770 | 5.2 | 0.121 | 6.7 | 0.702 | 5.2 | 0.123 |
| 07 | 7.3 | 0.365 | 4.0 | 0.277 | 7.6 | 0.305 | 4.4 | 0.112 |
| 08 | 7.8 | 0.534 | 7.7 | 0.213 | 7.6 | 0.548 | 7.5 | 0.255 |
| 09 | 2.6 | 0.897 | 2.8 | 0.107 | 4.7 | 0.670 | 2.9 | 0.098 |
| 10 | 4.8 | 0.730 | 5.9 | 0.139 | 6.6 | 0.491 | 5.4 | 0.264 |
| 11 | 4.5 | 0.772 | 6.2 | 0.259 | 7.3 | 0.390 | 7.1 | 0.014 |
| 12 | 4.8 | 0.802 | 6.6 | 0.247 | 5.9 | 0.704 | 5.8 | 0.417 |
| 13 | 5.0 | 0.679 | 3.4 | 0.493 | 5.9 | 0.548 | 3.6 | 0.449 |
| 14 | 4.8 | 0.830 | 6.2 | 0.327 | 7.8 | 0.544 | 5.6 | 0.449 |
| 15 | 3.1 | 0.926 | 3.7 | 0.386 | 5.6 | 0.761 | 3.9 | 0.327 |
| 16 | 5.9 | 0.621 | 1.9 | 0.515 | 3.7 | 0.851 | 2.5 | 0.166 |
| 17 | 7.8 | 0.722 | 3.7 | 0.018 | 8.4 | 0.679 | 3.7 | 0.008 |
| 18 | 4.1 | 0.766 | 8.0 | 0.173 | 5.0 | 0.663 | 7.5 | 0.268 |
| 19 | 2.7 | 0.925 | 2.7 | 0.301 | 7.5 | 0.441 | 2.7 | 0.309 |
| 20 | 7.7 | 0.738 | 4.9 | 0.579 | 8.0 | 0.716 | 5.3 | 0.508 |
| Mean ± SD | 5.4 ± 1.71 | 0.742 ± 0.131 | 4.9 ± 1.68 | 0.293 ± 0.169 | 6.7 ± 1.60 | 0.606 ± 0.142 | 4.8 ± 1.47 | 0.284 ± 0.166 |
| PTT1ECG (ms) | PTT1BCG (ms) | PTT2ECG (ms) | PTT2BCG (ms) | |
|---|---|---|---|---|
| Mean | 164.8 | 142.2 | 227.4 | 212.0 |
| SD | 21.46 | 17.57 | 24.29 | 18.81 |
| p-value | 2.76 × 10−51 | 5.23 × 10−22 | ||
| DTECG-BCG (ms) | DTPPGF-PPGT (ms) | |
|---|---|---|
| Mean | 82.8 | 61.6 |
| SD | 22.73 | 17.47 |
| p-value | 0.000 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, S.-H.; Zhang, B.-H.; Chen, W.; Su, C.-H.; Chin, C.-L. Cuffless and Touchless Measurement of Blood Pressure from Ballistocardiogram Based on a Body Weight Scale. Nutrients 2022, 14, 2552. https://doi.org/10.3390/nu14122552
Liu S-H, Zhang B-H, Chen W, Su C-H, Chin C-L. Cuffless and Touchless Measurement of Blood Pressure from Ballistocardiogram Based on a Body Weight Scale. Nutrients. 2022; 14(12):2552. https://doi.org/10.3390/nu14122552
Chicago/Turabian StyleLiu, Shing-Hong, Bing-Hao Zhang, Wenxi Chen, Chun-Hung Su, and Chiun-Li Chin. 2022. "Cuffless and Touchless Measurement of Blood Pressure from Ballistocardiogram Based on a Body Weight Scale" Nutrients 14, no. 12: 2552. https://doi.org/10.3390/nu14122552
APA StyleLiu, S.-H., Zhang, B.-H., Chen, W., Su, C.-H., & Chin, C.-L. (2022). Cuffless and Touchless Measurement of Blood Pressure from Ballistocardiogram Based on a Body Weight Scale. Nutrients, 14(12), 2552. https://doi.org/10.3390/nu14122552









